Abstract
Background
The degree to which outcomes following hospitalization for acute heart failure (HF) vary by racial and ethnic groups is poorly characterized. We sought to compare 30‐day and 1‐year rehospitalization and mortality rates for HF among 4 race/ethnic groups.
Methods and Results
Using the Get With The Guidelines–HF registry linked with Medicare data, we compared 30‐day and 1‐year outcomes between racial/ethnic groups by using a multivariable Cox proportional hazards model adjusting for clinical, hospital, and socioeconomic status characteristics. We analyzed 47 149 Medicare patients aged ≥65 years who had been discharged for HF between 2005 and 2011: there were 39 213 whites (83.2%), 4946 blacks (10.5%), 2347 Hispanics (5.0%), and 643 Asians/Pacific Islanders (1.4%). Relative to whites, blacks and Hispanics had higher 30‐day and 1‐year unadjusted readmission rates but lower 30‐day and 1‐year mortality; Asians had similar 30‐day readmission rates but lower 1‐year mortality. After risk adjustment, blacks had higher 30‐day and 1‐year CV readmission than whites but modestly lower short‐ and long‐term mortality; Hispanics had higher 30‐day and 1‐year readmission rates and similar 1‐year mortality than whites, while Asians had similar outcomes. When socioeconomic status data were added to the model, the majority of associations persisted, but the difference in 30‐day and 1‐year readmission rates between white and Hispanic patients became nonsignificant.
Conclusions
Among Medicare patients hospitalized with HF, short‐ and long‐term readmission rates and mortality differed among the 4 major racial/ethnic populations and persisted even after controlling for clinical, hospital, and socioeconomic status variables.
Keywords: health policy and outcome research, heart failure, race/ethnicity, rehospitalization
Introduction
Public reporting of hospital readmissions for heart failure (HF) underscores its importance as a measure of quality of care and as a metric for Medicare reimbursements.1 Among different racial/ethnic groups, older black and Hispanic patients have been reported to have higher 30‐day readmission rates compared with whites, in part related to the hospitals where care was provided.2–3 Although these data indicate racial/ethnic disparities in HF readmissions, lack of longer follow‐up data has limited the evaluation of how short‐term rehospitalizations may impact long‐term outcomes. A statewide study documented that minorities were more likely to be rehospitalized and were paradoxically less likely to die within 1 year, yet it remains unknown if these results are similar across the United States.4 A postulated explanation for these observations is that HF hospitalization in minority populations may not necessarily imply more severe disease but rather may result from poorer access to follow‐up care and/or poorer understanding of outpatient management of their symptoms and medications.
Understanding racial/ethnic differences in HF rehospitalizations and mortality may be crucial in helping to guide initiatives aimed at promoting health equity, reducing the financial burden of readmissions, and improving outcomes. We sought to evaluate the hypothesis that in contrast to white patients, black, Hispanic, and Asian patients have more comorbid diseases and higher rates of short‐ and long‐term readmissions but better short‐ and long‐term survival.5–7 Our 2 main objectives were to (1) compare 30‐day readmission and 1‐year mortality rates for HF among these 4 race/ethnic groups and (2) examine the impact of clinical profile and socioeconomic status (SES) variables on HF outcomes stratified by race/ethnicity.
Methods
Data Sources
Data for this analysis were derived from the Get With The Guidelines (GWTG)‐HF registry linked with Medicare inpatient data. The GWTG‐HF registry is an ongoing national, voluntary program formed to improve quality of care for patients hospitalized with HF. Its design and data variables have been previously reported.8–9 Data elements, including patient characteristics, medical history, medications, laboratory data, contraindications to treatment, inpatient care, outcomes, and hospital characteristics, were entered into an online interactive case report form and patient management tool (Outcome Sciences, Inc, a Quintiles Company). Using standardized definitions, trained personnel abstracted the data. Race/ethnicity data were recorded by patient self‐reporting by admissions or medical staff during registration. Race was recorded as part of a multiple‐choice data entry tool (ie, white, black, Asian, American Indian/Alaska native, and Native Hawaiian/Pacific Islander). A separate data element for Hispanic ethnicity (ie, yes versus no/not documented) was also implemented. All participating institutions were required to comply with local regulatory and privacy guidelines and, if required, to secure institutional review board approval. Because data were used primarily at the local site for quality improvement, sites were granted a waiver of informed consent under the common rule. Through an Internet‐based system, data quality was monitored for completeness and accuracy. Outcome Sciences, Inc served as the data collection and coordinating center for GWTG. The Duke Clinical Research Institute served as the data analysis center and examined the aggregate deidentified data for research purposes.
The Medicare data included Part A (inpatient) claims and the associated denominator file. Medicare inpatient claims data from January 1, 2005, through December 31, 2011, were linked with data from the GWTG‐HF registry, matching by admission and discharge dates, hospital, date of birth, and sex.10
Study Population
The study population for this analysis was based on those patients who (1) came from hospitals in GWTG‐HF registry that were fully participating, (2) had a principal HF diagnosis, (3) were ≥65 years old with a GWTG‐HF registry hospitalization linked to Medicare, (4) were discharged between January 1, 2005, and December 31, 2011, (5) were enrolled in fee‐for‐service Medicare at discharge, and (6) whose race/ethnicity were recorded as white (non‐Hispanic white), black (non‐Hispanic black), Hispanic, or Asian (non‐Hispanic Asian/Pacific Islander). If multiple hospitalizations exist for a patient, the first hospitalization was selected as the index hospitalization for this study.
Outcome Measures
For outcomes (ie, length of hospital stay and mortality) assessed post index admission, all patients after the aforementioned exclusions were analyzed. For outcomes (ie, readmission, hospital stay, mortality, and composite of mortality/readmission) post index discharge, the analysis was further limited to those who were discharged alive but did not leave against medical advice and were not discharged/transferred to either another short‐term hospital or hospice or had discharge destination missing.
The primary outcome measures were 30‐day and 1‐year rehospitalization, length of hospital stay, and mortality. More specifically, we examined all‐cause readmission post index discharge (30‐day and 1‐year), cardiovascular readmission post index discharge (30‐day and 1‐year), all‐cause mortality post index admission (30‐day and 1‐year), all‐cause mortality post index discharge (30‐day and 1‐year), and composite of mortality and all‐cause readmission post index discharge (30‐day and 1‐year). In addition, we assessed days in hospital for index admission and hospital stay within 30 days or 1 year post index discharge. Readmissions excluded the index hospitalization claim, transfers to or from another hospital, and admissions for rehabilitation.
Statistical Analysis
There are 2 study subpopulations: 1 for mortality and hospital stay post index admission and the other for mortality, readmission, composite of mortality/readmission, and total hospital days post index discharge.
Baseline characteristics of study population were described by race/ethnic groups, by using proportions for categorical variables and means with SD values for normally distributed continuous variables and medians with 25th and 75th percentiles for continuous variables with skewed distribution. Differences between the 4 race groups were tested by using χ2 tests for categorical variables and Wilcoxon tests for continuous variables. Characteristics of the study population were based on GWTG‐HF Registry data and included demographics (age, sex), clinical characteristics, including medical history, vital signs at admission (systolic blood pressure, heart rate, respiratory rate), lab work at admission (blood urea nitrogen, creatinine, hemoglobin, and sodium), ejection fraction, medications at discharge (angiotensin‐converting enzyme inhibitor, angiotensin II receptor blocker, β‐blocker, digoxin, diuretic, aldosterone antagonist, aspirin, and anticoagulants), length of stay >7 days for the index hospitalization, and year of index hospitalization, and hospital characteristics, namely geographic region, number of beds, teaching status, and rural location. Most variables had <5% missing except brain natriuretic peptide and missing on continuous variables were imputed to median and missing on categorical variables were imputed to dominant level.
Additionally, observed event rates were described for each race/ethnic group. For mortality, incidence at 30 days and 1 year were calculated by using Kaplan–Meier estimates. The mortality and composite of mortality/readmission were compared between race groups by using log‐rank tests. For readmissions, incidence at 30 days and 1 year were calculated by using estimates from the cumulative incidence function to account for the competing risk of mortality. The readmission outcomes were compared by using Gray tests. The hospital stay days were reported as a continuous variable and compared between the 4 race groups by using Wilcoxon tests.
Finally, the association of race/ethnicity with each outcome was assessed by using adjusted regression modeling for patient and hospital characteristics. For time‐to‐event outcomes, the adjusted association of race/ethnicity with outcome was assessed by using multivariable Cox proportional hazards models, where robust standard errors were used to account for the clustering of patients by hospital. The variables described here, except ejection fraction and discharge medications, were included in addition to the main variable of interest race groups with white as the referent. The adjustment was performed in 3 steps: adjustment for patient characteristics only, adjustment for patient and hospital characteristics together, followed by additional adjustment for SES data. SES variables included mean household income estimate, percentage of persons aged ≥25 years with ≥4 years of college (2006–2010 Census), and percentage of persons aged ≥25 years with high school diploma or greater (2006–2010 Census). Negative binomial regression model with individual specific offset was performed to examine the association of race/ethnicity and total days rehospitalized. GEE approach was used to account for within hospital clustering. In the model, the individual specific offset was determined by logarithm of length of follow‐up until censoring and the hospital stay days outcome was capped by the number of follow‐up days. Therefore, the individual specific offset allows model to account for the fact that patients had different length of follow‐up days. Other covariates in the model are same as those we used in the analyses of mortality and readmission outcomes. Race/ethnic group and geographic region interactions were also explored.
All tests were evaluated at a 2‐sided significance level of P<0.05. All statistical analyses were performed by using SAS 9.2 (SAS Institute).
Results
Patient and Hospital Characteristics
The linked GWTG‐HF and Medicare data included 175 693 patients. After further excluding 358 hospitals with limited participation and data capture (n=110 656 patients); 68 hospitals with <25 patients in the cohort (n=844 patients); patients with no fee‐for‐service eligibility at index discharge (n=2473); patients with race missing (n=1768), unable to determine (n=1332), or American Indian/Alaska native (n=210); patients without ≥1 documented admission vital signs (eg, systolic blood pressure, heart rate, or respiratory rate) (n=3979); and patients without at least 1 documented admission laboratory data result (eg, serum creatinine, blood urea nitrogen, or sodium) (n=7282), the final study population was composed of 47 149 patients from 213 hospitals across the United States. The composition by race/ethnicity was as follows: white (83.2%; n=39 213), black (10.5%; n=4946), Hispanic (5.0%; n=2347), and Asian/Pacific Islander patients (1.4%; n=643). From the study population of 47 149 patients, we excluded those who left against medical advice (n=135), were transferred out (n=685), were discharged to hospice (n=1220), died during the index admission (n=1413), and had ndocumented or undetermined discharge destination (n=551), and the analysis sample for the outcomes of interest post index discharge included 43 145 patients.
Baseline patient characteristics are summarized in Table 1. More than half (54.5%) of the population were women. Overall, white patients were older and had the highest proportion of octogenarians. Asian patients had the highest household income and were most likely to have a college degree; Hispanic patients were least likely to have a high school diploma. Compared with other racial/ethnic groups, white patients were more likely to have a history of atrial fibrillation, chronic obstructive pulmonary disease, ischemic etiology of HF, and peripheral vascular disease, whereas non‐Hispanic black patients were more likely to have anemia, hypertension, renal insufficiency, smoking, and a history of stroke. Hispanic patients were more likely to have diabetes, while Asian patients had a stronger history of valvular heart disease. On admission, black and Asian patients were more likely to have higher brain natriuretic peptide levels; black and Hispanic patients were more likely to have lower left ventricular systolic ejection fraction. At discharge, β‐blockers and angiotensin‐converting enzyme inhibitors were more likely to be prescribed to black patients, while angiotensin II receptor blockers and aldosterone antagonists were more likely to be prescribed to Asian and white patients, respectively. Black patients were more likely to be treated at higher‐volume, teaching hospitals. Geographically, more black and Hispanic patients were discharged from hospitals in the south, whereas more Asian patients were treated at centers in the western region.
Table 1.
Baseline Characteristics
| Variable | Non‐Hispanic White (n=39 213) | Non‐Hispanic Black (n=4946) | Hispanic (n=2347) | Non‐Hispanic Asian/Pacific Islander (n=643) | P Value* | |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age, y | Median (IQR) | 81 (75 to 87) | 76 (70 to 83) | 78 (71 to 84) | 80 (74 to 86) | <0.001 |
| Age (grouped), % | ≥80 | 7.1 | 5.5 | 2.1 | 54.9 | <0.001 |
| 75 to 79 | 18.1 | 20.1 | 20.1 | 19.1 | ||
| 70 to 74 | 13.9 | 20.7 | 19.0 | 16.0 | ||
| 65 to 69 | 11.0 | 23.7 | 18.9 | 10.0 | ||
| Female, % | 53.9 | 59.9 | 53.1 | 55.2 | <0.001 | |
| Social economic status | ||||||
| Median household income estimate, US$ | Median (IQR) | 45 798 (40 780 to 53 577) | 45 359 (41 087 to 53 363) | 46 566 (38 740 to 53 547) | 53 494 (49 284 to 66 476) | <0.001 |
| Persons aged ≥25 years with high school diploma, % | Median (IQR) | 86.2 (83.1 to 89.0) | 84.3 (81.4 to 87.1) | 80.3 (75.5 to 84.9) | 85.4 (75.9 to 89.9) | <0.001 |
| Persons aged ≥25 years with ≥4 years of college education, % | Median (IQR) | 25.2 (17.8 to 29.2) | 27.9 (21.3 to 33.2) | 26.7 (16.9 to 30.7) | 29.0 (27.7 to 33.2) | <0.001 |
| Medical history, % | ||||||
| Anemia | 19.6 | 21.8 | 16.4 | 16.2 | <0.001 | |
| Atrial fibrillation/flutter | 41.5 | 22.8 | 22.5 | 31.4 | <0.001 | |
| COPD or asthma | 29.5 | 28.8 | 25.5 | 21.2 | <0.001 | |
| Depression | 10.9 | 5.3 | 6.7 | 5.4 | <0.001 | |
| Diabetes | 37.6 | 49.0 | 54.6 | 43.2 | <0.001 | |
| Heart failure | 52.5 | 55.3 | 54.5 | 46.7 | <0.001 | |
| Hypertension | 74.9 | 85.6 | 84.8 | 81.2 | <0.001 | |
| ICD or CRT‐D | 9.2 | 9.4 | 8.7 | 6.8 | 0.155 | |
| Ischemic cause: Med Hx of CAD, MI, prior PCI or CABG | 60.0 | 46.1 | 57.9 | 54.4 | <0.001 | |
| Peripheral arterial disease | 14.6 | 12.1 | 11.8 | 7.9 | <0.001 | |
| Renal insufficiency | 18.7 | 25.8 | 19.4 | 22.6 | <0.001 | |
| Smoking | 8.5 | 13.7 | 8.5 | 5.3 | <0.001 | |
| CVA/TIA | 16.5 | 18.9 | 13.2 | 17.7 | <0.001 | |
| Valvular heart disease | 14.9 | 9.4 | 9.5 | 15.9 | <0.001 | |
| Vital signs at admission | ||||||
| Heart rate, bpm | Median (IQR) | 80.0 (70.0 to 94.0) | 80.0 (71.0 to 95.0) | 80.0 (70.0 to 95.0) | 82.0 (70.0 to 98.0) | <0.001 |
| Systolic blood pressure, mm Hg | Median (IQR) | 137.0 (119.0 to 157.0) | 146.0 (126.0 to 170.0) | 143.0 (123.0 to 165.0) | 142.0 (122.0 to 164.0) | <0.001 |
| Lab work at admission | ||||||
| Sodium, mEq/L | Median (IQR) | 138 (136 to 140) | 139 (137 to 141) | 138 (135 to 140) | 138 (134 to 140) | <0.001 |
| BNP, pg/mL | Median (IQR) | 766 (391 to 1485) | 832 (329 to 1850) | 763 (348 to 1642) | 1000 (481 to 2099) | <0.001 |
| Creatinine, mg/dL | Median (IQR) | 1.3 (1.0 to 1.8) | 1.4 (1.1 to 2.1) | 1.3 (1.0 to 1.9) | 1.3 (1.0 to 2.0) | <0.001 |
| BUN, mg/dL | Median (IQR) | 26 (19 to 37) | 26 (17 to 35) | 26 (19 to 37) | 27 (19 to 42) | <0.001 |
| Hemoglobin, g/dL | Median (IQR) | 11.8 (10.6 to 13.1) | 11.8 (10.4 to 12.6) | 11.8 (10.6 to 12.8) | 11.8 (10.5 to 12.9) | <0.001 |
| Ejection fraction | ||||||
| LVEF <40% (combined quantitative and qualitative), % | 36.5 | 41.6 | 41.8 | 31.6 | <0.001 | |
| LVEF value, % | Median (IQR) | 45 (30 to 57) | 43 (25 to 57) | 40 (27 to 55) | 49.5 (34 to 60) | <0.001 |
| Hospital stay | ||||||
| Length of stay (transfer out and in excluded), days | Median (IQR) | 4.0 (3 to 7) | 4.0 (3 to 7) | 5.0 (3 to 7) | 4.0 (3 to 7) | <0.001 |
| Medications at discharge, % | ||||||
| ARB | 12.2 | 14.0 | 18.5 | 20.1 | <0.001 | |
| ACE‐I | 42.1 | 47.8 | 46.1 | 32.5 | <0.001 | |
| β‐Blocker | 71.0 | 74.6 | 72.6 | 66.6 | <0.001 | |
| Aldosterone antagonist | 13.4 | 12.7 | 12.7 | 9.6 | 0.012 | |
| Anticoagulants | 30.7 | 19.4 | 19.4 | 17.9 | <0.001 | |
| Hospital characteristics | ||||||
| Geographic region, % | West | 10.7 | 3.0 | 14.9 | 51.3 | <0.001 |
| South | 32.1 | 38.4 | 42.6 | 20.1 | ||
| Midwest | 29.9 | 24.8 | 8.4 | 13.4 | ||
| Northeast | 27.4 | 33.9 | 34.1 | 15.2 | ||
| Teaching hospital, % | 58.1 | 73.2 | 52.1 | 51.0 | <0.001 | |
| Number of beds | Median (IQR) | 400.0 (238 to 593) | 438.0 (317 to 610) | 346.00 (280 to 483) | 400.00 (238 to 501) | <0.001 |
| Rural location, % | 8.2 | 2.3 | 1.5 | 1.4 | <0.001 | |
ACE‐I indicates angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; BNP, brain natriuretic peptide; BUN, blood urea nitrogen; CABG, coronary artery bypass graft surgery; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; CRT‐D, cardiac resynchronization therapy‐defibrillator; CVA, cerebrovascular accident; ICD, implantable cardiac defibrillator; LVEF, left ventricular ejection fraction; Med Hx, Past Medical History; MI, myocardial infarction; PCI, percutaneous coronary intervention; TIA, transient ischemic attack.
P value tests the difference across the 4 race groups.
Unadjusted Outcomes
Thirty‐day outcomes
The unadjusted 30‐day mortality post index admission and all‐cause readmission post index discharge ranged from 5.6% to 9.7% and 22.9% to 26.3%, respectively (Table 2). In contrast to white patients, black and Hispanic patients had lower short‐term mortality (mortality postdischarge: white 6.3%, black 4.3%, Hispanic 4.4%; P<0.001), higher short‐term all‐cause (non‐Hispanic white 23%, black 25.1%, Hispanic 26.3%; P=0.003) and cardiovascular readmissions. Compared with white patients, Asian patients had similar short‐term mortality and all‐cause readmission but slightly higher short‐term cardiovascular readmission.
Table 2.
Cumulative Incidence of Outcomes Overall and by Race/Ethnicity
| Outcomes | Non‐Hispanic White | Non‐Hispanic Black | Hispanic | Non‐Hispanic Asian/Pacific Islander | P Value* |
|---|---|---|---|---|---|
| 30‐Day outcomes | |||||
| Mortality post index admission, n | 3790 (9.7%) | 274 (5.6%) | 168 (7.2%) | 61 (9.6%) | <0.001 |
| Mortality post index discharge, n | 2227 (6.3%) | 199 (4.3%) | 94 (4.4%) | 35 (6.0%) | <0.001 |
| All‐cause readmission post index discharge, n | 8109 (23.0%) | 1157 (25.1%) | 565 (26.3%) | 133 (22.9%) | 0.003 |
| Cardiovascular readmission post index discharge, n | 4146 (11.7%) | 612 (13.3%) | 304 (14.2%) | 80 (13.8%) | <0.001 |
| Mortality/readmission post index discharge, n | 9251 (26.2%) | 1260 (27.4%) | 608 (28.3%) | 150 (25.8%) | 0.360 |
| 1‐Year outcomes | |||||
| Mortality post index admission, n | 13 940 (37.8%) | 1367 (29.5%) | 701 (32.2%) | 206 (35.1%) | <0.001 |
| Mortality post index discharge, n | 11 323 (34.1%) | 1203 (27.7%) | 585 (29.2%) | 165 (31.2%) | <0.001 |
| All‐cause readmission post index discharge, n | 22 390 (66.9%) | 3144 (72.9%) | 1440 (71.3%) | 359 (66.5%) | <0.001 |
| Cardiovascular readmission post index discharge, n | 13 642 (41.0%) | 2097 (49.0%) | 950 (47.5%) | 223 (41.5%) | <0.001 |
| Mortality/readmission post index discharge, n | 25 068 (74.8%) | 3366 (78.0%) | 1531 (75.7%) | 391 (72.3%) | 0.007 |
P value tests the difference across the 4 race groups.
One‐year outcomes
The unadjusted 1‐year mortality post index admission ranged from 29.5% to 37.8%, while all‐cause readmission post index discharge ranged from 66.5% to 72.9% (Table 2). In comparison to white patients, all other groups had lower long‐term mortality (mortality postdischarge: white 34.1%, black 27.7%, Hispanic 29.2%, Asian 31.2%; P<0.001). However, black and Hispanic patients had higher long‐term all‐cause (white 66.9%, black 72.9%, Hispanic 71.3%; P<0.001) and cardiovascular readmission and slightly higher combined mortality and readmission than non‐Hispanic white patients. Asian patients had similar long‐term readmission rates as white patients (Figures 1 through 5).
Figure 5.
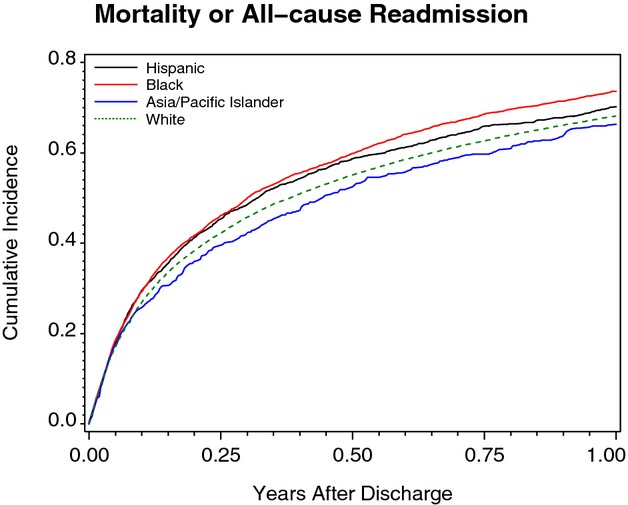
One‐year composite of mortality or all‐cause readmission stratified by race/ethnicity.
Figure 1.
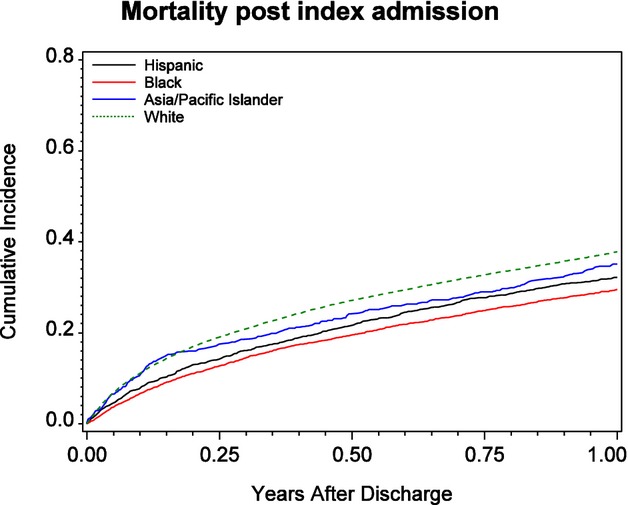
One‐year mortality after index heart failure admission stratified by race/ethnicity.
Figure 2.
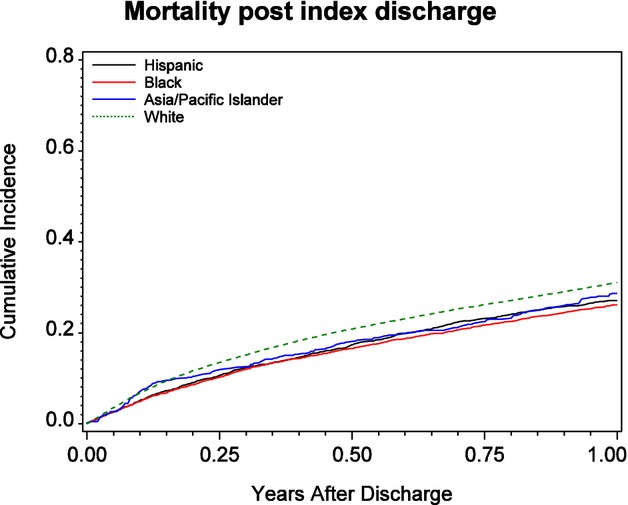
One‐year mortality after index hospital discharge stratified by race/ethnicity.
Figure 3.
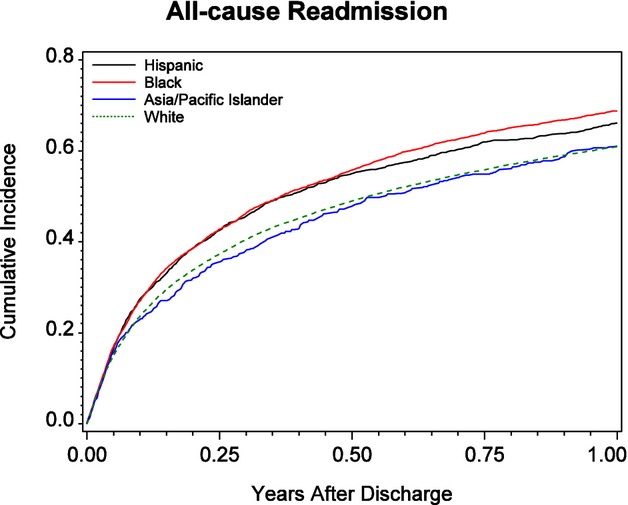
One‐year all‐cause readmission stratified by race/ethnicity.
Figure 4.
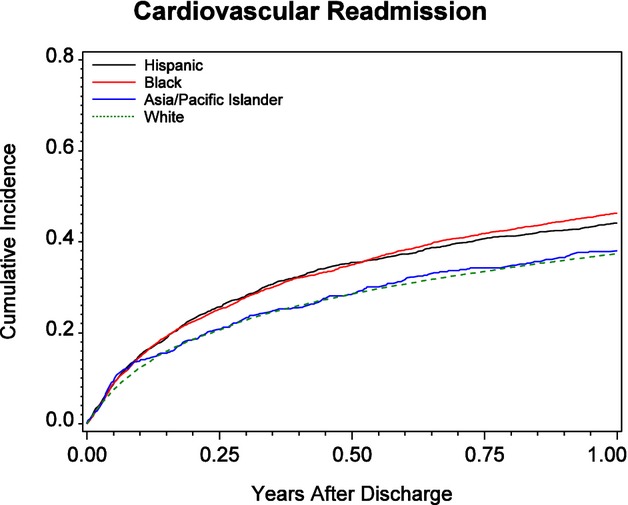
One‐year cardiovascular readmission stratified by race/ethnicity.
Multivariable Analysis
After multivariable adjustment for patient and hospital characteristics, black patients had lower odds of death but showed slightly higher risk of readmission and combined mortality/readmission than did white patients in both short‐ and long‐term follow‐up (Table 3). Compared with white patients, Hispanic patients had similar 30‐day mortality postadmission, modestly lower 30‐day mortality postdischarge, similar 1‐year mortality, and higher short‐ and long‐term readmission and combined mortality/readmission. In reference to white patients, Asian patients had similar outcomes, except for marginally higher risk of short‐term cardiovascular readmission.
Table 3.
Associations Between Race/Ethnicity and Outcomes
| Outcome | Comparison | Unadjusted | Adjusted for Patient and Hospital Characteristics | Adjusted for Patient, Hospital, and SES Characteristics | |||
|---|---|---|---|---|---|---|---|
| HR (95% CI) | P Value | HR (95% CI) | P Value | HR (95% CI) | P Value | ||
| 30‐Day outcomes | |||||||
| Mortality post index admission | Black (vs white) | 0.56 (0.49 to 0.64) | <0.001 | 0.73 (0.64 to 0.83) | <0.001 | 0.73 (0.65 to 0.83) | <0.001 |
| Hispanic (vs white) | 0.73 (0.59 to 0.91) | 0.005 | 0.88 (0.73 to 1.07) | 0.192 | 0.87 (0.71 to 1.06) | 0.165 | |
| Asian (vs white) | 0.98 (0.76 to 1.27) | 0.897 | 0.95 (0.74 to 1.21) | 0.662 | 0.99 (0.78 to 1.26) | 0.941 | |
| Mortality post index discharge | Black (vs white) | 0.67 (0.56 to 0.81) | <0.001 | 0.88 (0.74 to 1.04) | 0.123 | 0.90 (0.76 to 1.06) | 0.209 |
| Hispanic (vs white) | 0.69 (0.56 to 0.84) | <0.001 | 0.81 (0.6 to 0.99) | 0.034 | 0.84 (0.67 to 1.05) | 0.124 | |
| Asian (vs white) | 0.95 (0.60 to 1.50) | 0.830 | 0.97 (0.64 to 1.48) | 0.888 | 1.03 (0.67 to 1.57) | 0.905 | |
| All‐cause readmission post index discharge | Black (vs white) | 1.10 (1.02 to 1.18) | 0.013 | 1.08 (1.00 to 1.17) | 0.057 | 1.05 (0.98 to 1.13) | 0.166 |
| Hispanic (vs white) | 1.15 (1.03 to 1.28) | 0.011 | 1.16 (1.04 to 1.29) | 0.008 | 1.08 (0.98 to 1.19) | 0.142 | |
| Asian (vs white) | 1.00 (0.81 to 1.22) | 0.975 | 1.07 (0.84 to 1.35) | 0.591 | 1.03 (0.81 to 1.30) | 0.833 | |
| Cardiovascular readmission post index discharge | Black (vs white) | 1.13 (1.02 to 1.26) | 0.021 | 1.12 (1.01 to 1.24) | 0.029 | 1.09 (0.99 to 1.19) | 0.083 |
| Hispanic (vs white) | 1.21 (1.08 to 1.35) | 0.001 | 1.22 (1.08 to 1.37) | 0.001 | 1.11 (0.99 to 1.24) | 0.081 | |
| Asian (vs white) | 1.18 (0.96 to 1.45) | 0.110 | 1.29 (1.00 to 1.68) | 0.053 | 1.23 (0.95 to 1.59) | 0.112 | |
| Mortality/readmission post index discharge | Black (vs white) | 1.05 (0.98 to 1.12) | 0.172 | 1.07 (1.00 to 1.15) | 0.059 | 1.05 (0.98 to 1.13) | 0.130 |
| Hispanic (vs white) | 1.08 (0.99 to 1.19) | 0.085 | 1.12 (1.02 to 1.23) | 0.014 | 1.06 (0.97 to 1.16) | 0.178 | |
| Asian (vs white) | 0.99 (0.81 to 1.20) | 0.883 | 1.05 (0.85 to 1.30) | 0.658 | 1.02 (0.83 to 1.27) | 0.826 | |
| 1‐Year outcomes | |||||||
| Mortality post index admission | Black (vs white) | 0.72 (0.67 to 0.78) | <0.001 | 0.88 (0.83 to 0.93) | <0.001 | 0.88 (0.83 to 0.93) | <0.001 |
| Hispanic (vs white) | 0.81 (0.72 to 0.90) | <0.001 | 0.94 (0.86 to 1.03) | 0.199 | 0.94 (0.86 to 1.02) | 0.113 | |
| Asian (vs white) | 0.90 (0.80 to 1.02) | 0.109 | 0.91 (0.80 to 1.04) | 0.185 | 0.92 (0.80 to 1.06) | 0.233 | |
| Mortality post index discharge | Black (vs white) | 0.77 (0.71 to 0.84) | <0.001 | 0.93 (0.87 to 0.99) | 0.030 | 0.93 (0.87 to 1.00) | 0.040 |
| Hispanic (vs white) | 0.82 (0.73 to 0.93) | 0.001 | 0.96 (0.87 to 1.05) | 0.374 | 0.96 (0.87 to 1.05) | 0.353 | |
| Asian (vs white) | 0.88 (0.76 to 1.02) | 0.098 | 0.92 (0.79 to 1.07) | 0.279 | 0.92 (0.78 to 1.08) | 0.308 | |
| All‐cause readmission post index discharge | Black (vs white) | 1.14 (1.07 to 1.20) | <0.001 | 1.13 (1.06 to 1.20) | 0.001 | 1.10 (1.04 to 1.16) | <0.001 |
| Hispanic (vs white) | 1.10 (1.02 to 1.19) | 0.012 | 1.13 (1.04 to 1.22) | 0.002 | 1.06 (0.99 to 1.14) | 0.094 | |
| Asian (vs white) | 0.95 (0.86 to 1.04) | 0.267 | 1.03 (0.92 to 1.15) | 0.636 | 0.99 (0.89 to 1.11) | 0.878 | |
| Cardiovascular readmission post index discharge | Black (vs white) | 1.22 (1.14 to 1.31) | <0.001 | 1.23 (1.15 to 1.33) | <0.001 | 1.20 (1.13 to 1.28) | <0.001 |
| Hispanic (vs white) | 1.19 (1.11 to 1.29) | <0.001 | 1.23 (1.13 to 1.34) | <0.001 | 1.15 (1.06 to 1.24) | 0.001 | |
| Asian (vs white) | 1.01 (0.91 to 1.12) | 0.885 | 1.11 (0.98 to 1.27) | 0.094 | 1.07 (0.94 to 1.21) | 0.286 | |
| Mortality/readmission post index discharge | Black (vs white) | 1.09 (1.03 to 1.14) | 0.001 | 1.12 (1.06 to 1.18) | 0.001 | 1.10 (1.04 to 1.15) | <0.001 |
| Hispanic (vs white) | 1.05 (0.98 to 1.12) | 0.202 | 1.09 (1.02 to 1.17) | 0.013 | 1.04 (0.98 to 1.11) | 0.192 | |
| Asian (vs white) | 0.92 (0.85 to 1.00) | 0.064 | 0.99 (0.89 to 1.09) | 0.820 | 0.96 (0.87 to 1.06) | 0.446 | |
Adjustment variables in the multivariable models are patient characteristics including age; sex; past medical history of atrial fibrillation/flutter, anemia, chronic obstructive pulmonary disease, depression, diabetes mellitus, heart failure, hypertension, implantable cardiac defibrillator, ischemic cause, dyslipidemia, pacemaker, peripheral vascular disease, renal insufficiency, cerebrovascular accident/transient ischemic attack, valvular heart disease, smoker; systolic blood pressure, heart rate, and respiratory rate; sodium, serum creatinine, blood urea nitrogen, and hemoglobin; year of index hospitalization; and hospital characteristics including region (Midwest, West, South vs Northeast), number of beds, teaching status, and rural (vs urban). Socioeconomic status characteristics adjustment included mean household income estimate, percentage persons aged ≥25 years with ≥4 years of college, and percentage of persons aged ≥25 years with a high school diploma or greater.
When SES data were added to the multivariable model, we observed that the majority of mortality end points did not change after adjusting for SES variables. Black patients remained at higher risk for rehospitalization compared with white patients, even after accounting for SES. However, the difference in rehospitalization risk, including 30‐day all‐cause and cardiovascular readmission and 1‐year all‐cause readmission, between white and Hispanic patients diminished and became statistically nonsignificant.
Analysis of total readmission days in the first 30 days postdischarge revealed that there was no difference in this end point across racial/ethnic groups after adjusting for patient, hospital, and SES characteristics (Table 4). For the first 1 year postdischarge, black patients had more rehospitalization stay days within 1 year after patient, hospital, and SES adjustments. Hispanics and Asians also had more rehospitalization stay days after adjusting for patient and hospital characteristics, but the difference became marginally insignificant after further SES adjustment.
Table 4.
Analysis of Total Number of Hospital Stay Days in First 30 Days and 1 Year After Index Hospital Admission or Index Hospital Discharge by Race/Ethnicity
| Outcome | Comparison | Unadjusted | Adjusted for Patient and Hospital Variables | Adjusted for Patient, Hospital, and SES Variables | |||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | ||
| Hospital stay days within 30 days post index discharge | Hispanic (2.1 days) (vs white, 1.8 days) | 0.99 (0.88 to 1.11) | 0.848 | 0.95 (0.85 to 1.06) | 0.347 | 0.91 (0.82 to 1.01) | 0.076 |
| Black (2.0 days) (vs white) | 0.99 (0.91 to 1.08) | 0.834 | 0.95 (0.88 to 1.03) | 0.189 | 0.93 (0.87 to 1.01) | 0.075 | |
| Asian (2.1 days) (vs white) | 1.16 (0.90 to 1.50) | 0.258 | 1.14 (0.87 to 1.49) | 0.347 | 1.11 (0.85 to 1.45) | 0.435 | |
| Hospital stay days within 1 year post index discharge | Hispanic (13.3 days) (vs white 9.7 days) | 1.09 (0.96 to 1.23) | 0.183 | 1.25 (1.10 to 1.42) | 0.001 | 1.09 (0.99 to 1.21) | 0.086 |
| Black (13.6 days) (vs white) | 1.12 (1.04 to 1.21) | 0.002 | 1.19 (1.09 to 1.30) | 0.001 | 1.13 (1.04 to 1.23) | 0.004 | |
| Asian (11.0 days) (vs white) | 1.18 (0.90 to 1.54) | 0.226 | 1.33 (1.04 to 1.71) | 0.024 | 1.24 (0.99 to 1.53) | 0.057 | |
Patient characteristics adjustment included age, gender, PMHX (Past medical history), atrial fibrillation/flutter, anemia, chronic obstructive pulmonary disease, depression, diabetes mellitus, heart failure, hypertension, implantable cardiac defibrillator, ischemic cause, dyslipidemia, pacemaker, peripheral vascular disease, renal insufficiency, cerebrovascular accident/transient ischemic attack, valvular heart disease, and smoker, vital signs: systolic blood pressure, heart rate, and respiratory rate, labs: sodium, serum creatinine, blood urea nitrogen, hemoglobin, year of index hospitalization. Hospital characteristics adjustment included region (Midwest, West, South vs Northeast), no. of beds, teaching status, rural (vs urban). Socioeconomic status characteristics adjustment included mean household income estimate, percentage persons aged ≥25 years with ≥4 years of college, and percentage of persons aged ≥25 years with a high school diploma or greater.
Moreover, we examined the interaction by race/ethnicity × region and found that compared with white patients, Hispanics in the West had lower 1‐year mortality risk relative to the other regions (Table 5).
Table 5.
Analysis of Interaction Between Race/Ethnicity and Geographic Region
| Outcome | Interaction P Value | Variable | Hazard Ratio (95% CI) | P Value |
|---|---|---|---|---|
| 30‐Day mortality post index admission | 0.155 | |||
| 30‐Day mortality post index discharge | 0.884 | |||
| 30‐Day all‐cause readmission | 0.110 | |||
| 1‐Year mortality post index admission | <0.001 | |||
| Hispanic (vs white) in Midwest | 0.84 (0.66 to 1.08) | 0.168 | ||
| Hispanic (vs white) in Northeast | 0.93 (0.84 to 1.03) | 0.150 | ||
| Hispanic (vs white) in South | 1.06 (0.94 to 1.20) | 0.319 | ||
| Hispanic (vs white) in West | 0.66 (0.57 to 0.76) | <0.001 | ||
| Black (vs white) in Midwest | 0.86 (0.78 to 0.95) | 0.003 | ||
| Black (vs white) in Northeast | 0.89 (0.80 to 0.99) | 0.040 | ||
| Black (vs white) in South | 0.89 (0.81 to 0.97) | 0.011 | ||
| Black (vs white) in West | 0.90 (0.62 to 1.31) | 0.581 | ||
| Asian (vs white) in Midwest | 0.91 (0.68 to 1.21) | 0.522 | ||
| Asian (vs white) in Northeast | 0.85 (0.52 to 1.37) | 0.498 | ||
| Asian (vs white) in South | 1.05 (0.72 to 1.51) | 0.812 | ||
| Asian (vs white) in West | 0.88 (0.75 to 1.03) | 0.120 | ||
| 1‐Year mortality post index discharge | 0.003 | |||
| Hispanic (vs white) in Midwest | 0.89 (0.66 to 1.18) | 0.414 | ||
| Hispanic (vs white) in Northeast | 0.96 (0.86 to 1.08) | 0.531 | ||
| Hispanic (vs white) in South | 1.09 (0.95 to 1.24) | 0.219 | ||
| Hispanic (vs white) in West | 0.62 (0.52 to 0.76) | <0.001 | ||
| Black (vs white) in Midwest | 0.94 (0.83 to 1.06) | 0.309 | ||
| Black (vs white) in Northeast | 0.92 (0.82 to 1.02) | 0.123 | ||
| Black (vs white) in South | 0.94 (0.85 to 1.05) | 0.290 | ||
| Black (vs white) in West | 0.95 (0.68 to 1.33) | 0.786 | ||
| Asian (vs white) in Midwest | 1.04 (0.78 to 1.40) | 0.788 | ||
| Asian (vs white) in Northeast | 0.70 (0.41 to 1.21) | 0.200 | ||
| Asian (vs white) in South | 1.00 (0.71 to 1.43) | 0.985 | ||
| Asian (vs white) in West | 0.90 (0.72 to 1.11) | 0.327 | ||
| 1‐Year all‐cause readmission | 0.111 |
Model adjusted for patient, hospital characteristics, and socioeconomic status variables as displayed in Table 3 footnote.
Discussion
Our results highlight several important racial/ethnic differences in HF outcomes. First, black and Hispanic HF patients had higher 30‐day and 1‐year readmission rates but lower 30‐day and 1‐year mortality, whereas Asian patients had similar 30‐day readmission rates but lower 1‐year mortality relative to white patients. Second, adjustment for patient and hospital characteristics resulted in similar outcomes for black patients but significantly diminished the mortality difference between Hispanic and white patients. Third, after additional adjustment for SES variables, the majority of associations between race/ethnicity group and outcomes persisted, with the exception that there was further reduction in the difference in 30‐day and 1‐year readmission rates between white and Hispanic patients.
A previous analysis of the GWTG‐HF database revealed that black and Hispanic patients hospitalized with HF, despite having more cardiovascular risk factors, had lower in‐hospital mortality rates than white patients.5 By linking with Medicare data for postdischarge outcomes, our results extend these observations by demonstrating that better survival among black patients persists during the 30‐day and 1‐year follow‐up periods, although they were more likely to be readmitted during the same follow‐up intervals. These findings are consistent with data from the OPTIMIZE‐HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure) Registry comparing 60‐ to 90‐day outcomes between African Americans and non‐African Americans.11 Other reports using Medicare data described higher 30‐day readmission for HF in black and Hispanic patients, even after controlling for patient and hospital characteristics.2–3 A multiethnic population study using a California database found that age‐adjusted hospitalization rates were highest in black patients; similar between white and Hispanic patients; and lowest among Asian men. Conversely, black and Hispanic patients were found to be more likely than white and Asian patients to survive for 12 months after the index HF hospitalization.4 Data from other recent studies support the observation of lower adjusted in‐hospital and short‐term mortality in black and Hispanic patients than whites.6,12–14
Racial/ethnic differences in HF outcomes have been previously explained on the basis of comorbid conditions and quality of care. Consistent with prior registry data, our findings show lower left ventricular ejection fraction, higher brain natriuretic peptide levels, and higher comorbidity burden in black (ie, hypertension and renal insufficiency) and Hispanic patients (ie, diabetes) than in white patients.5,11,15 In reference to quality of HF care, results from both the OPTIMIZE‐HF and GWTG databases demonstrate comparable to better delivery of guideline‐recommended measures of care in blacks and Hispanics relative to white patients.5,11,15 Apart from these differences, another plausible explanation for the seemingly paradoxical observation of higher HF readmission frequency and lower mortality among minorities is poorer socioeconomic resources. A prior analysis of a national sample of Medicare beneficiaries hospitalized with HF between 1998 and 1999 reported that lower‐SES patients had a higher risk of 1‐year readmission and 1‐year mortality compared with higher‐SES patients. Patient SES factors, determined based on the sociodemographic characteristics of the patient's ZIP code of residence, were not significantly associated with 30‐day death but were strongly associated with longer‐term outcomes in that population.6 In our study, multivariable adjustment for several SES variables such as household income and markers of higher education reduced intergroup differences in rehospitalization risk (ie, between white and Hispanic patients) but did not significantly impact most of the mortality end points.
How race/ethnicity, as a social determinant, could influence HF outcomes has not been adequately evaluated in prior studies. In this study, black HF patients had lower risk‐adjusted mortality than white patients. Our results suggest that when the analyses are limited to fee‐for‐service Medicare patients (aged >65 years, have insurance and Social Security), the impact of SES parameters on HF outcomes, mortality in particular, may be blunted. Relative to its effect on HF outcomes, income may be more important among younger patients and less indicative of SES in older, retired individuals.16 Whereas our multivariable model adjusts for patients' educational level, conventional definitions of education may not completely correlate with health literacy. Race/ethnicity may also be a surrogate for other factors that may account for health disparities. In our and other analyses, collection of SES variables do not incorporate access to care, acculturation, language barrier, health‐related behaviors and cultural beliefs, patient–provider trust, and provider issues of bias and cultural insensitivity.17–21
Our study has a number of other limitations. As a retrospective observational study, residual measured and unmeasured confounding variables may account for some or all of the findings despite adjustment for multiple variables. Because the study population was composed of patients who were fee‐for‐service Medicare beneficiaries and who were from hospitals participating in the GWTG‐HF program, our results may not be applicable to other HF populations. In this context, our study population is not reflective of the racial/ethnic distribution of the national US population. The method of recording race and ethnicity by patient self‐designation as recorded by administrative staff or admitting providers may be less reliable than direct patient reporting. Moreover, the existing data entry tool for race/ethnicity recording limited our ability to examine differences at the level of white, black, Hispanic, and Asian subpopulations. SES was derived from environment level (ie, residence ZIP code) household income rather than individual attributes. Direct patient‐level measures of SES were not available. Findings for readmission may be influenced by competing risks from mortality.
Conclusions
Among Medicare patients hospitalized with HF, there were important differences in patient characteristics as well as short‐ and long‐term outcomes among 4 racial/ethnic populations. Compared with white patients, black and Hispanic patients had lower 30‐day and 1‐year mortality but higher 30‐day and 1‐year readmission rates. The 30‐day and 1‐year outcomes for Asian and white patients were similar. After controlling for patient clinical characteristics, SES, and hospital‐related variables, black patients had higher 1‐year readmission rates but lower 30‐day and 1‐year mortality; while Hispanic and Asian patients had largely similar risk‐adjusted outcomes, compared with white patients. This study provides evidence of contemporary racial and ethnic‐based differences in HF outcomes and highlights the need for further studies to identify underlying causes for these racial and ethnic differences in care and outcomes of HF patients.
Sources of Funding
The GWTG‐HF program is provided by the American Heart Association. GWTG‐HF has been funded in the past through support from Medtronic, GlaxoSmithKline, Ortho‐McNeil, and the American Heart Association (AHA) Pharmaceutical Roundtable.
Disclosures
Dr Hernandez reports receiving research grants from Johnson & Johnson and honoraria from Medtronic, Amgen, and Astra Zeneca. Dr Peterson serves as the principal investigator of the Data Analytic Center for the GWTG of the AHA. He reports receiving research support from Bristol‐Meyers Squibb, Sanofi, Merck, Schering‐Plough, Lilly, and Johnson & Johnson. Dr Deepak L. Bhatt discloses the following relationships—Advisory Board: Elsevier Practice Update Cardiology, Medscape Cardiology, Regado Biosciences; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care; chair: AHA GWTG Steering Committee; Data Monitoring Committees: Duke Clinical Research Institute; Harvard Clinical Research Institute; Mayo Clinic; Population Health Research Institute; honoraria: American College of Cardiology (editor, Clinical Trials, Cardiosource), Belvoir Publications (editor in chief, harvard heart letter), Duke Clinical Research Institute (clinical trial steering committees), Harvard Clinical Research Institute (clinical trial steering committee), HMP Communications (editor in chief, Journal of Invasive Cardiology); Population Health Research Institute (Clinical Trial Steering Committee), Slack Publications (chief medical editor, Cardiology Today's Intervention), WebMD (CME steering committees); other: Clinical Cardiology (associate editor); Journal of the American College of Cardiology (section editor, pharmacology); research grants: Amarin, AstraZeneca, Bristol‐Myers Squibb, Eisai, Ethicon, Medtronic, Roche, Sanofi Aventis, The Medicines Company; Unfunded Research: FlowCo, PLx Pharma, Takeda. Dr Schwamm serves as chair of the GWTG Steering Committee of the AHA. Dr Fonarow served as former chair of the AHA GWTG Steering Committee. He reports receiving research grants from National Heart, Lung, and Blood Institute (significant); receiving honoraria from Medtronic (modest), and serving as a consultant for Novartis (significant). The remaining authors report no conflicts of interest. The authors are solely responsible for the design and conduct of this study, all analyses, and the drafting and editing of the paper and its final contents.
References
- 1. Hospital Compare. Department of Health and Human Services; Available at: http://www.hospitalcompare.hhs.gov. Accessed 18 November 2013. [Google Scholar]
- 2.Joynt KE, Orav EJ, Jha AK. Thirty‐day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011; 305:675-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodriguez F, Joynt KE, López L, Saldaña F, Jha AK. Readmission rates for Hispanic Medicare beneficiaries with heart failure and acute myocardial infarction. Am Heart J. 2011; 162:254-261. [DOI] [PubMed] [Google Scholar]
- 4.Alexander M, Grumbach K, Remy L, Rowell R, Massie BM. Congestive heart failure hospitalizations and survival in California: patterns according to race/ethnicity. Am Heart J. 1999; 137:919-927. [DOI] [PubMed] [Google Scholar]
- 5.Thomas KL, Hernandez AF, Dai D, Heidenreich P, Fonarow GC, Peterson ED, Yancy CW. Association of race/ethnicity with clinical risk factors, quality of care, and acute outcomes in patients hospitalized with heart failure. Am Heart J. 2011; 161:746-754. [DOI] [PubMed] [Google Scholar]
- 6.Rathore SS, Masoudi FA, Wang Y, Curtis JP, Foody JM, Havranek EP, Krumholz HM. Socioeconomic status, treatment, and outcomes among elderly patients hospitalized with heart failure: findings from the National Heart Failure Project. Am Heart J. 2006; 152:371-378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greiner MA, Hammill BG, Fonarow GC, Whellan DJ, Eapen ZJ, Hernandez AF, Curtis LH. Predicting costs among Medicare beneficiaries with heart failure. Am J Cardiol. 2012; 109:705-711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hernandez AF, Fonarow GC, Liang L, Al‐Khatib SM, Curtis LH, LaBresh KA, Yancy CW, Albert NM, Peterson ED. Sex and racial differences in the use of implantable cardioverter‐defibrillators among patients hospitalized with heart failure. JAMA. 2007; 298:1525-1532. [DOI] [PubMed] [Google Scholar]
- 9.Peterson PN, Rumsfeld JS, Liang L, Hernandez AF, Peterson ED, Fonarow GC, Masoudi FA. Treatment and risk in heart failure: gaps in evidence or quality? Circ Cardiovasc Qual Outcomes. 2010; 3:309-315. [DOI] [PubMed] [Google Scholar]
- 10.Hammill BG, Hernandez AF, Peterson ED, Fonarow GC, Schulman KA, Curtis LH. Linking inpatient clinical registry data to Medicare claims data using indirect identifiers. Am Heart J. 2009; 157:995-1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yancy CW, Abraham WT, Albert NM, Clare R, Stough WG, Gheorghiade M, Greenberg BH, O'Connor CM, She L, Sun JL, Young JB, Fonarow GC. Quality of care of and outcomes for African Americans hospitalized with heart failure: findings from the OPTIMIZE‐HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure) registry. J Am Coll Cardiol. 2008; 51:1675-1684. [DOI] [PubMed] [Google Scholar]
- 12.Deswal A, Petersen NJ, Souchek J, Ashton CM, Wray NP. Impact of race on health care utilization and outcomes in veterans with congestive heart failure. J Am Coll Cardiol. 2004; 43:778-784. [DOI] [PubMed] [Google Scholar]
- 13.Brown DW, Haldeman GA, Croft JB, Giles WH, Mensah GA. Racial or ethnic differences in hospitalization for heart failure among elderly adults: Medicare, 1990–2000. Am Heart J. 2005; 150:448-454. [DOI] [PubMed] [Google Scholar]
- 14.Kamath SA, Drazner MH, Wynne J, Fonarow GC, Yancy CW. Characteristics and outcomes in African American patients with decompensated heart failure. Arch Intern Med. 2008; 168:1152-1158. [DOI] [PubMed] [Google Scholar]
- 15.Vivo RP, Krim SR, Krim NR, Zhao X, Hernandez AF, Peterson ED, Piña IL, Bhatt DL, Schwamm LH, Fonarow GC. Care and outcomes of Hispanic patients admitted with heart failure with preserved or reduced ejection fraction: findings from get with the guidelines‐heart failure. Circ Heart Fail. 2012; 5:167-175. [DOI] [PubMed] [Google Scholar]
- 16.Borne Y, Engstrom G, Essen B, Sundquist J, Hedblad B. Country of birth and risk of hospitalization due to heart failure: a Swedish population‐based cohort study. Eur J Epidemiol. 2011; 26:275-283. [DOI] [PubMed] [Google Scholar]
- 17.Evangelista LS, Dracup K, Doering LV. Racial differences in treatment‐seeking delays among heart failure patients. J Card Fail. 2002; 8:381-386. [DOI] [PubMed] [Google Scholar]
- 18.Peterson PN, Shetterly SM, Clarke CL, Bekelman DB, Chan PS, Allen LA, Matlock DD, Magid DJ, Masoudi FA. Health literacy and outcomes among patients with heart failure. JAMA. 2011; 305:1695-1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chaudhry SI, Herrin J, Phillips C, Butler J, Mukerjhee S, Murillo J, Onwuanyi A, Seto TB, Spertus J, Krumholz HM. Racial disparities in health literacy and access to care among patients with heart failure. J Card Fail. 2011; 17:122-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peterson PN, Campagna EJ, Maravi M, Allen LA, Bull S, Steiner JF, Havranek EP, Dickinson LM, Masoudi FA. Acculturation and outcomes among patients with heart failure. Circ Heart Fail. 2012; 5:160-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yancy CW, Wang TY, Ventura HO, Piña IL, Vijayaraghavan K, Ferdinand KC, Hall LLcredo Advisory Group. The coalition to reduce racial and ethnic disparities in cardiovascular disease outcomes (credo): why credo matters to cardiologists. J Am Coll Cardiol. 2011; 57:245-252. [DOI] [PubMed] [Google Scholar]


