Abstract
Background
Ten‐year and lifetime cardiovascular risk assessment algorithms have been adopted into atherosclerotic cardiovascular disease (ASCVD) prevention guidelines, but these prediction models are not based on South Asian populations and may underestimate the risk in Indians, Pakistanis, Bangladeshis, Nepali, and Sri Lankans in the United States. Little is known about ASCVD risk prediction and intermediate endpoints such as subclinical atherosclerosis in US individuals of South Asian ancestry.
Methods and Results
South Asians (n=893) from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study who were 40 to 79 years and free of ASCVD were included. Ten‐year ASCVD predicted risk was calculated using the 2013 Pooled Cohort Equations. Lifetime predicted risk was based on risk factor burden. Baseline levels of subclinical atherosclerosis (coronary artery calcium [CAC] and carotid intima media thickness [CIMT]) were compared across 10‐year and lifetime risk strata: (1) high (≥7.5%) 10‐year and low (<7.5%) 10‐year risk; (2) high (≥39%) lifetime and low (<39%) lifetime risk. South Asian men and women with high 10‐year predicted risk had a significantly greater CAC burden than those with low 10‐year risk. South Asians with high lifetime predicted risk had a significantly increased odds for CAC higher than 0 (odds ratio: men 1.97; 95% CI, 1.2 to 3.2; women 3.14; 95% CI, 1.5, 6.6). Associations between risk strata and CIMT were also present.
Conclusion
This study is the first to provide evidence that contemporary ASCVD risk assessment algorithms derived from non‐Hispanic white and African‐American samples can successfully identify substantial differences in atherosclerotic burden in US South Asians.
Keywords: cardiovascular risk stratification, epidemiology, subclinical atherosclerosis
Introduction
Individuals of South Asian ancestry (from India, Pakistan, Bangladesh, Nepal, and Sri Lanka) represent a quarter of the world's population; at 3.4 million, they are the sixth largest ethnic minority group in the United States, and the second fastest growing group.1 South Asians have a high incidence of cardiovascular disease (CVD); for example, in California, South Asians have the highest ischemic heart disease mortality rate among the top 6 racial/ethnic groups.2
One strategy to reduce the high CVD risk of South Asians includes screening for and treating CVD risk factors. The 2013 American Heart Association/American College of Cardiology Pooled Risk Calculator for estimating 10‐year and lifetime predicted risk of atherosclerotic cardiovascular disease (ASCVD) has been developed and validated for risk estimation among Americans aged 40 to 79 by pooling non‐Hispanic white and African‐American groups.3–4 However, like other risk calculators,5–6 the Pooled Risk Calculator may underestimate observed ASCVD risk in South Asians in the United States, an ethnic group with high rates of CVD at standard risk thresholds.7
Berry and colleagues demonstrated an association between levels of 10‐year and lifetime ASCVD risks and subclinical atherosclerosis prevalence and progression among young and middle‐aged adults from the Coronary Artery Risk Development in Young Adults (CARDIA) and Multi‐Ethnic Study of Atherosclerosis (MESA).8 Risk stratification models have focused on lifetime cardiovascular disease risk because a large proportion of ASCVD events ultimately occur among individuals with a relatively low 10‐year predicted risk.9 Lifetime ASCVD risk estimation, which measures the cumulative risk of developing the disease during the remainder of an individual's lifespan, may provide a more appropriate assessment of future ASCVD risk than shorter‐term 10‐year risk estimates, especially in younger individuals in whom 10‐year ASCVD risk is nearly always low.
Our objective was to apply previously published 10‐year and lifetime predicted risk algorithms to data from participants in the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study and to evaluate the association between the ASCVD predicted risk (both 10‐year and lifetime) and measures of subclinical atherosclerosis (coronary artery calcium and carotid intima media thickness) in US South Asians. Although these data are cross‐sectional and cannot be used to assess the performance of the risk prediction algorithms, coronary artery calcium has been shown to be a powerful predictor of risk and CVD events in healthy people;10–11 in this paper, we describe the distribution of cardiovascular risk in US South Asians and the relationship between the new Pooled Cohort Risk Equation and established surrogate markers of ASCVD.
Methods
The MASALA study methods are modeled after the MESA study,12 as previously described.13 The MASALA study is a community‐based cohort of South Asian men and women from 2 clinical sites (San Francisco Bay Area at the University of California, San Francisco [UCSF] and the greater Chicago area at Northwestern University [NU]). The baseline examination was conducted from October 2010 through March 2013. The institutional review boards of UCSF and NU approved the MASALA study protocol.
Participants
To be eligible for the MASALA study, participants had to self‐identify as South Asian ethnicity (at least 3 grandparents born in any South Asian country), speak English, Hindi, or Urdu, and be between the ages of 40 and 84 years at baseline. As in the MESA study, we excluded those with clinically evident CVD from the MASALA study.13 Participants undergoing active treatment for cancer and those residing in a nursing home were also excluded. MASALA employed community‐based recruitment methods that were similar to the MESA study.12–13 The baseline cohort included 906 participants; the present analysis only includes the 893 who had complete risk factor measurements and who were between ages of 40 and 79 years. We restricted the analysis to include participants who were between the ages of 40 and 79 years to match the ages of cohorts used in the development of the Pooled Cohort risk equations.
Clinical Measurements
Trained multilingual study staff conducted all visits, and all consent forms and questionnaires were also translated into Hindi and Urdu. We gathered information on participants’ demographics, habits including tobacco use, medical history, and medication use.
We measured seated resting blood pressure 3 times using an automated blood pressure monitor (V100 Vital sign monitor; GE Medical Systems, Fairfield, CT) and used the mean of the last 2 readings for analyses.13 We collected blood after a 12‐hour fast, and measured fasting and 2‐hour plasma glucose by the glucose oxidase method and fasting total cholesterol, triglycerides, and high‐density lipoprotein (HDL) cholesterol y enzymatic methods (Quest Diagnostics, San Jose, CA), from which we calculated low‐density lipoprotein (LDL) cholesterol.14
Risk Factor Definitions
We defined dyslipidemia as total cholesterol ≥240 mg/dL, LDL cholesterol ≥160 mg/dL, or HDL cholesterol <40 mg/dL (for persons with and without diabetes) or use of a cholesterol‐lowering medication.9 We defined hypertension as a systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or use of an antihypertensive medication. We defined diabetes mellitus as a fasting plasma glucose ≥126 mg/dL, 2‐hour post‐load plasma glucose ≥200 mg/dL, HbA1c ≥6.5%, or use of antihyperglycemic medications. We defined cigarette smoking as currently smoking cigarettes. Use of an HMG‐coA reductase inhibitor, fibrate, or niacin was categorized as cholesterol medication use. The study PI adjudicated the use of antihypertensive medicines and diabetes medicines. Antihypertensive use was classified as a medication from any class (angiotensin‐converting enzyme inhibitor, angiotensin‐receptor blocker, beta‐blocker, calcium channel blocker, or diuretic) that was inventoried at the clinical examination.
Ten‐Year and Lifetime Risk Factor Stratification
We estimated the 10‐year predicted risk for ASCVD events (myocardial infarction or coronary death, and fatal or non‐fatal stroke) using the new Pooled Cohort Equations.15–16 These allowed us to stratify the study samples into 2 groups: those with low predicted 10‐year risk (10‐year risk <7.5%) and those with high predicted 10‐year risk (10‐year risk ≥7.5% or diabetes mellitus). The lifetime predicted risk for ASCVD (myocardial infarction, coronary insufficiency, angina, atherothrombotic stroke, intermittent claudication, or CVD death) was estimated using a previously published algorithm based on the aggregate risk factor burden (Table 1).9 This method of classification resulted in the formation of 2 lifetime risk different groups: low (<39%) lifetime and high (≥39%) lifetime predicted risk. The cut point of 39% was derived initially from data from the Framingham Heart Study whereby individuals with ≥1 clinically elevated CVD risk factors (eligible for treatment based on clinical practice guidelines) had a lifetime risk for CVD of 39% to 70%.9 Berry and colleagues evaluated this threshold of 39% a priori in their demonstration of the association between short‐term/lifetime risk categories and baseline and changes in subclinical measures of cardiovascular disease using data from CARDIA and MESA longitudinal cohorts.8 This cut point has also previously been shown to be associated with CVD events and mortality.17
Table 1.
Estimation of Predicted Lifetime Risks for Atherosclerotic Cardiovascular Disease (ASCVD) and Risk Factor (RF) Stratification*
| CVD Risk Factors | All Optimal RFs | Borderline RFs | High RFs | Very High RFs |
|---|---|---|---|---|
| SBP and DBP, mm Hg | SBP <120 and DBP <80 | SBP 120 to 139 and/or DBP 80 to 89 | SBP 140 to 159 or DBP 90 to 99 | SBP ≥160 or DBP ≥100 or treated |
| AND | OR | OR | OR | |
| Total cholesterol, mg/dL | <180 | 180 to 199 | 200 to 239 | ≥240 or treated |
| AND | AND | AND | OR | |
| Diabetes mellitus* | No | No | No | Yes |
| AND | AND | AND | OR | |
| Current smoking | No | No | No | Yes |
| Lifetime risk stratification | Low predicted lifetime risk: all risk factors are either optimal or borderline | High predicted lifetime risk: at least 1 high or very high risk factor | ||
DBP indicates diastolic blood pressure; SBP, systolic blood pressure.
Lifetime risk refers to risk of all ASCVD (myocardial infarction, coronary insufficiency, angina, atherothrombotic stroke, intermittent claudication or ASCVD death). Risk factor (RF) stratification derived from Lloyd‐Jones et al.9
Subclinical Disease Measures
Cardiac CT scans were performed using a gated‐cardiac electron‐beam CT scanner. At UCSF, the system was either the 16D scanner (Philips Medical Systems, Andover, MA) or the MSD Aquilion 64 model (Toshiba Medical Systems, Tustin, CA). At NU, the technicians used the Sensation Cardiac 64 Scanner (Siemens Medical Solutions, Malvern, PA).13 All CT scans were sent in batches to the centralized reading center at Harbor‐UCLA Medical Center, where they were interpreted with Rephot Imaging software according to the MESA study methods. The prevalence of coronary calcium was defined using the Agatston score and was treated as a categorical variable (CAC=0 or CAC >0) and as a continuous variable for participants with CAC >0.18
We conducted high‐resolution B‐mode ultrasonography for measurement of right and left internal and common carotid arty intima media thickness (millimeters). Carotid IMT (CIMT) was measured in 12 predefined segments (6 per side) including 1 transverse scan sequence of the common carotid through the bulb and 5 longitudinal images taken from both the right and left carotid arteries for each participant.12 These digitized data were batched and mailed on magneto‐optical disks to the central reading center at Wake Forest University, where they were read by a single reader, for wall‐thickness measurements using the MESA protocol for CIMT measurement, which only uses the far wall measures, not an average of the maximum thickness of the near and far wall (which MESA used for the baseline MESA CIMT protocol). For quality control, the single reader completed 25 repeat CIMT measures, and we calculated the correlation among ultrasound repeated readings. The intraclass correlation coefficient (ICC) for the internal carotid IMT was 0.96 and was 0.78 for the common carotid IMT. All CT scans and ultrasounds were read by trained individuals who were blinded to clinical and demographic characteristics of participants.
Statistical Analysis
In all analyses, the predicted risk group functioned as the independent variable and the measure of atherosclerosis (ie, CAC or CIMT) functioned as the dependent variable. Because of potentially large differences in associations of CAC and carotid IMT with the risk groups by gender, all analyses were conducted separately for women and men. We calculated mean and standard deviation for continuous variables and proportions for categorical variables for the baseline characteristics. We computed the prevalence (percentage) rates of CAC >0 and the odds ratios with 95% confidence intervals (CIs) across the 10‐year and lifetime risk groups using logistic models with the binary variable of CAC >0 as the outcome adjusting for the age distribution within each risk group. We also used age‐adjusted logistic regression to test differences between the reference group (low 10‐year and low lifetime risk) and high 10‐year and high lifetime predicted risk groups. We computed means for common and internal CIMT by use of general linear models with adjustment for age. We used linear regression to test associations between each CIMT outcome variable and the different risk groups with adjustment for age. We conducted all analyses with SAS statistical software (version 9.3; SAS Institute, Inc.).
The authors had full access to and take full responsibility for the integrity of the data. All authors have read and agree to the manuscript as written.
Results
Participant Characteristics
Detailed socio‐demographic characteristics of the MASALA cohort have been published previously.13 Participants had a mean (SD) age of 55 (9) years, 46% were women, 98% were born outside the United States, and overall, the cohort had a high socioeconomic status (Table 2). The most common ASCVD risk factors in men and women were hyperlipidemia and hypertension. The prevalence of diabetes was 28% in men and 22% in women, respectively. Smoking prevalence was low.
Table 2.
Demographic Characteristics and Age‐Adjusted Prevalence of ASCVD Risk Factors in the MASALA Study Cohort, 2010–2013
| Men (n=485) | Women (n=418) | |
|---|---|---|
| Age, mean (SD) | 56 (10) | 54 (9) |
| Foreign‐born, % | 98 | 98 |
| Years in the US, mean (SD) | 28 (11) | 27 (11) |
| Education‐Bachelor's or higher, % | 90 | 85 |
| Annual family income, ≥$75 000, % | 73 | 74 |
| Hypertension, age‐adjusted % | 43 | 35 |
| Hyperlipidemia, age‐adjusted % | 62 | 39 |
| Diabetes, age‐adjusted % | 28 | 22 |
| Smoking, age‐adjusted % | 5 | 1 |
ASCVD indicates atherosclerotic cardiovascular disease; MASALA, Mediators of Atherosclerosis in South Asians Living in America.
Distribution of Risk Strata and Risk Factor Profiles
Nearly half (49%) of the men in MASALA and only 14% of women were classified as having a high 10‐year predicted risk (Figure A). The majority of South Asian men (79%) and women (70%) had a high lifetime predicted risk of ASCVD (Figure B).
Figure 1.
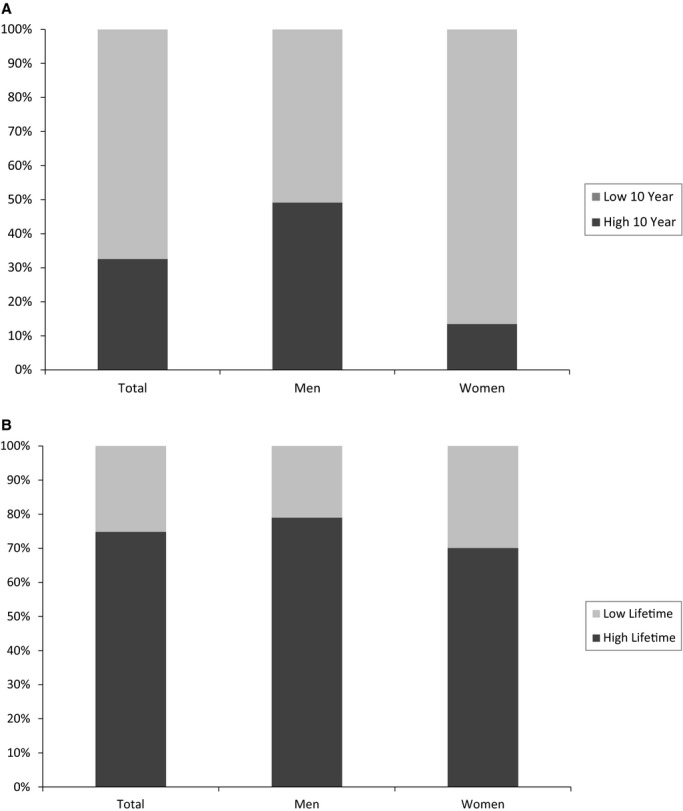
A, Distribution of 10‐year predicted risk groups among 893 MASALA participants. B, Distribution of lifetime predicted risk groups among 893 MASALA participants. MASALA indicates mediators of atherosclerosis in South Asians living in America.
Not surprisingly, risk factor profiles were more adverse in those classified as high risk compared with low risk (Table 3). The 10‐year predicted risk of ASCVD in the high lifetime predicted risk groups, using the Pooled cohort equation from the 2013 ACC/AHA Guidelines,3 was 12.6% in men and 5.1% in women.
Table 3.
Baseline Characteristics of the MASALA Study Participants by Risk Strata
| Men (n=485) | Women (n=418) | |||||||
|---|---|---|---|---|---|---|---|---|
| 10‐Year Risk* | Lifetime Risk | 10‐Year Risk* | Lifetime Risk | |||||
| Low (n=243) | High (n=235) | Low (n=102) | High (n=383) | Low (n=359) | High (n=56) | Low (n=125) | High (n=293) | |
| Age in years, mean (SD) | 48 (5.5) | 64 (7.0) | 53 (8.9) | 57 (10.0) | 52 (7.0) | 68. (4.8) | 50 (7.5) | 56 (8.5) |
| Systolic blood pressure, mm Hg, (SD) | 121 (11.5) | 132 (15.1) | 122 (10.8) | 128 (15.2) | 120 (14.8) | 139 (18.3) | 117 (14.4) | 125 (17.1) |
| Total cholesterol, mg/dL (SD) | 186 (36.6) | 178 (37.3) | 173 (20.1) | 185 (39.9) | 193 (34.6) | 195 (43.0) | 177 (16.9) | 201 (39.1) |
| HDL cholesterol, mg/dL (SD) | 44 (9.5) | 47 (12.2) | 44 (10.4) | 46 (11.1) | 56 (13.9) | 55 (13.3) | 56 (13.6) | 55 (13.9) |
| BMI, kg/m2 (SD) | 25.9 (3.9) | 25.9 (4.8) | 25.8 (6.1) | 25.9 (3.8) | 26.0 (4.3) | 26.6 (4.0) | 25.1 (3.8) | 26.5 (4.3) |
| Waist circumference, cm (SD) | 95.1 (9.4) | 96.7 (9.5) | 93.5 (10.2) | 96.5 (9.2) | 88.7 (9.8) | 92.2 (10.9) | 86.6 (9.4) | 90.2 (10.1) |
| Current smokers, % | 5 (2.1) | 21 (8.9) | 0 (0) | 26 (6.8) | 4 (1.1) | 1 (1.8) | 0 (0) | 5 (1.7) |
| Diabetes mellitus, % | 41 (16.9) | 98 (41.7) | 0 (0) | 139 (36.3) | 58 (16.2) | 32 (57.2) | 0 (0) | 90 (30.7) |
| Antihypertensive therapy, % | 46 (18.9) | 128 (54.5) | 0 (0) | 175 (45.7) | 69 (19.2) | 38 (67.9) | 0 (0) | 107 (36.5) |
| Lipid‐lowering therapy, % | 73 (30.0) | 97 (41.3) | 0 (0) | 174 (45.4) | 77 (21.5) | 24 (42.9) | 0 (0) | 101 (34.5) |
| Pooled cohort equation ASCVD 10‐year risk, % mean (SD) | 3.7 (1.9) | 18.9 (10.5) | 5.6 (5.2) | 12.6 (11.3) | 2.1 (1.7) | 16.2 (9.1) | 1.6 (2.0) | 5.1 (6.9) |
ASCVD indicates atherosclerotic cardiovascular disease; HDL, high‐density lipoprotein; MASALA, Mediators of Atherosclerosis in South Asians Living in America.
Participants who were missing HDL cholesterol (n=10) could not have 10‐year risk calculated and are not included in 10‐year risk strata.
Subclinical Atherosclerosis
In men, high 10‐year predicted risk was associated with higher CAC prevalence (68%) and greater adjusted odds ratio of CAC (OR [95% CI]=1.81 [1.0, 3.3]) compared with low 10‐year risk (Table 4). Women in the high 10‐year predicted risk group also had a greater CAC burden than women in the low 10‐year risk group, however the confidence intervals were larger and did not reach statistical significance. In men and women, CAC prevalence was significantly higher in the high lifetime predicted risk group compared with the low lifetime predicted risk group (64% versus 48% in men [P<0.01] and 23% versus 9% in women [P<0.01], Table 4). When CAC was analyzed as a continuous score (Agatston score in those with CAC >0), we observed significantly higher CAC scores in men with high lifetime predicted risk compared with men with low lifetime risk. The odds ratio for age‐adjusted CAC prevalence was also higher among for men and women with high lifetime risk (men: OR [95% CI]=1.97 [1.2, 3.2]); women (OR [95% CI]=3.1 [1.5, 6.6]) compared with individuals with low lifetime risk.
Table 4.
Age‐Adjusted Coronary Artery Calcium (CAC) Among MASALA Participants by Gender and Risk Group Strata
| Men (n=485) | Women (n=418) | |||||||
|---|---|---|---|---|---|---|---|---|
| 10‐Year Risk* | Lifetime Risk | 10‐Year Risk* | Lifetime Risk | |||||
| Low (n=243) | High (n=235) | Low (n=102) | High (n=383) | Low (n=359) | High (n=56) | Low (n=125) | High (n=293) | |
| Age‐adjusted CAC prevalence, % | 46.2 | 67.9* | 47.9 | 64.4* | 18.5 | 26.2 | 8.9 | 23.3* |
| Age‐adjusted CAC score, mean (SE) | 73.5 (0.7) | 97.4 (0.9) | 52.0 (0.6) | 95.3 (0.6)* | 44.7(1.5) | 82.1 (1.8) | 45.6 (1.2) | 56.3 (1.2) |
| Presence of CAC, OR (95% CI) | Referent | 1.81 (1.0, 3.3)* |
Referent | 1.97 (1.2, 3.2)* |
Referent | 1.56 (0.7, 3.4) |
Referent | 3.14 (1.5, 6.6)* |
HDL indicates high‐density lipoprotein; MASALA, Mediators of Atherosclerosis in South Asians Living in America.
Participants who were missing HDL cholesterol (n=10) could not have 10‐year risk calculated and are not included in 10‐year risk strata.
P<0.01.
P<0.05.
In age‐adjusted regression models (Table 5), women in the high 10‐year predicted risk group had a significantly greater common CIMT (0.89 mm [SD=0.09]) and internal CIMT (1.27 mm [SD=0.18]) than those in the low 10‐year risk strata (common CIMT=0.83 mm [0.06] and internal CIMT=1.12 mm [0.18]). In men, a significantly greater internal CIMT was found among men in the high lifetime predicted risk group compared with low lifetime risk, but no significant associations between 10‐year risk strata and CIMT were observed in men.
Table 5.
Age‐Adjusted Carotid Intima‐Media Thickness (IMT) Among MASALA Participants by Gender and Risk Group Strata
| Men (n=485) | Women (n=418) | |||||||
|---|---|---|---|---|---|---|---|---|
| 10‐Year Risk* | Lifetime Risk | 10‐Year Risk* | Lifetime Risk | |||||
| Low (n=243) | High (n=235) | Low (n=102) | High (n=383) | Low (n=359) | High (n=56) | Low (n=125) | High (n=293) | |
| Common carotid IMT, n | 242 | 234 | 101 | 382 | 359 | 56 | 125 | 293 |
| Adjusted mean (SE), mm | 0.90 (0.08) | 0.92 (0.11) | 0.90 (0.06) | 0.92 (0.06) | 0.83 (0.07) | 0.89 (0.09)* | 0.82 (0.06) | 0.84 (0.06) |
| Internal carotid IMT, n | 242 | 233 | 101 | 381 | 359 | 56 | 125 | 293 |
| Adjusted mean (SE), mm | 1.26 (0.16) | 1.28 (0.19) | 1.20 (0.11) | 1.30 (0.12)* | 1.12 (0.14) | 1.27 (0.18)* | 1.10 (0.11) | 1.16 (0.12) |
HDL indicates high‐density lipoprotein; MASALA, Mediators of Atherosclerosis in South Asians Living in America.
Participants who were missing HDL cholesterol (n=10) could not have 10‐year risk calculated and are not included in 10‐year risk strata.
P<0.01.
P<0.05.
Discussion
This study yielded several important insights about cardiovascular risk stratification, the new Pooled Cohort Equation, and subclinical atherosclerosis among middle‐aged US South Asian men and women. Using the new Pooled Cohort Equation for risk stratification, we found that 49% of South Asian men and 13% of women had a high 10‐year predicted risk. In addition, almost three‐quarters of South Asians were identified as having high lifetime predicted ASCVD risk. Importantly, the relationship between risk factor levels and CAC that has been demonstrated in other race/ethnic groups was also demonstrated in US South Asians. Although associations between IMT and lifetime and 10‐year predicted risk were present, these were not consistent.
Until now, there have been no data on 10‐year and lifetime risk strata and subclinical atherosclerosis in US South Asians. Similar to findings from the Cardiovascular Lifetime Risk Pooling Project,8–9,8–20 South Asian individuals with high lifetime predicted ASCVD risk had a greater burden of CAC, which in other studies has been associated with higher ASCVD event rates.10,21 In both the MESA and CARDIA cohorts, elevated lifetime predicted risk was associated with increased CAC score and progression of subclinical atherosclerosis in men and women from diverse racial/ethnic backgrounds.8 In this community‐based cohort of US South Asians we studied, an elevated lifetime ASCVD predicted risk was associated with greater likelihood of having CAC. Others have shown that exposure to elevated risk factors is associated with subclinical atherosclerosis in young adults,21 and that as these individuals age, greater baseline subclinical atherosclerosis predicts more CVD events. Not surprisingly, participants with a high 10‐year risk also had a greater CAC burden compared with those with low 10‐year risk. It is interesting to note that the risk factor distribution in South Asians is somewhat different than in MESA and CARDIA participants8; MASALA participants have a higher prevalence of diabetes and much lower prevalence of smoking.22–23 The MASALA study participants had much higher education and income levels compared with MESA study participants, which is consistent with US Census data on the South Asian population compared with other racial/ethnic groups.1 However, we have found that similar to other racial/ethnic groups, a higher prevalence of abnormal, established risk factors is associated with pathogenesis of CAC in South Asians. Therefore, risk factor prevention and control remain cornerstones for decreasing ASCVD incidence and mortality in South Asians.
Prior studies examining lifetime predicted risk and CIMT have not been as consistent as data on risk strata and CAC; high lifetime predicted risk was associated with greater CIMT in CARDIA participants, but the association in MESA cohort participants was not significant.8 In the MASALA study cohort, we found that high lifetime predicted risk was only associated with greater internal CIMT among men. In US South Asian women, high 10‐year predicted risk was associated with greater common and internal CIMT. The uniformly high CIMT across all MASALA study participants may have precluded the ability to detect differences across risk strata. Alternatively, the higher prevalence of statin use in the MASALA cohort compared to CARDIA and MESA could have caused stabilization of carotid plaques and potentially could have attenuated potential associations between predicted risk strata and CIMT.24–25 It should also be noted that we observed much higher CIMT in MASALA participants than what has been reported in CARDIA and MESA participants8 and in South Asians cohorts from Canada and the United Kingdom.26–27 Compared with data from the New Delhi Birth Cohort, however, our estimates of CIMT are similar (0.91 for men and 0.86 for women at mean age of 36 years).28 There are several possible explanations for the higher CIMT observed in MASALA study participants. The South Asians in this study were older than the MESA and CARDIA participants who were included in the lifetime predicted risk paper by Berry et al.8 Another possible explanation for the higher CIMT in the MASALA participants compared to other studies is the high prevalence of diabetes, impaired glucose tolerance, and impaired fasting glucose observed in the MASALA cohort.22 In addition to diabetes, impaired glucose tolerance and impaired fasting glucose are independently associated with greater CIMT.29” Because the MASALA study used the MESA Exam 5 protocol for CIMT measurement,13 and not the MESA baseline CIMT measurement protocol, it is difficult to directly compare the baseline CIMT measures in MASALA to MESA baseline CIMT measures.
The present study uses cross‐sectional data and cannot assess the performance of the risk prediction models. Future data on CVD incidence from the MASALA study will allow for further validation of the Pooled Cohort Equation in US South Asians. However, several other studies have suggested that standard risk prediction algorithms, which were developed largely in non‐Hispanic white and African‐American populations, underestimate ASCVD risk among South Asians.3,6,30 A study by Bhopal et al of South Asians in the United Kingdom found that the Framingham and FINRISK risk prediction models predicted CHD and stroke mortality equally well.6 More recently, 2 separate studies in Britain, one using cross‐sectional data and the other using prospective CVD event data, found that different risk prediction algorithms produce significantly different estimates of CVD risk within South Asians.5,31 For example, the QRISK2 algorithm and the Joint British Societies algorithm produces significantly different median risk scores in South Asian men compared with white men31 because QRISK2 counts South Asian ethnicity as an additional risk factor.30–31 Studies also show that the QRISK2 and Framingham risk scores consistently underestimated CVD event risk in South Asian women.5 The conflicting evidence to date underscores the need for longitudinal data on cardiovascular risk estimates and ASCVD events derived from diverse populations, including US South Asians.
Strengths and Limitations
Our study is the first to report on associations between risk strata using the new Pooled Cohort Equations3 and subclinical atherosclerosis in a largely immigrant South Asian population. As the MASALA study cohort matures, we will be able to describe the relationship between ASCVD risk assessment scores, including the Pooled Cohort Equation, and the occurrence of ASCVD events.
The MASALA sample is limited to participants from 2 specific geographic regions, the San Francisco Bay and greater Chicago areas, which may not represent all South Asians in the United States. However, we have previously reported the similarity of the MASALA population to the US Census 2010 South Asian data.13 We also excluded all persons with known cardiovascular disease or any cardiovascular symptoms from the study population so the estimates reported represent a relatively healthier population of South Asians. The MASALA sample is largely comprised of immigrants from India and their descendants, and CVD risk prediction models may not be consistent across South Asians from countries other than India.6 The MASALA data presented here are cross‐sectional, which limits the ability to study the progression of subclinical atherosclerosis or incident ASCVD events, both of which are targets of future research within our group.
Conclusions
CVD risk prediction is increasingly being incorporated into prevention guidelines; however, current risk estimation methods have been limited by a lack of data on some ethnic minority groups, including South Asians. This study provides important new information on associations between the new Pooled Cohort Risk Equation, lifetime and 10‐year predicted risk, and subclinical atherosclerosis in US South Asians. Longitudinal follow‐up of the MASALA cohort will allow further study of the relationship between cardiovascular risk stratification and progression of subclinical atherosclerosis, incident CVD events, and mortality in US South Asians.
Sources of Funding
The MASALA study was supported by the NIH grant no. 1R01 HL093009. Data collection at UCSF was also supported by NIH/NCRR UCSF‐CTSI grant number UL1 RR024131. The sponsors did not play a significant role in the analysis, interpretation, and presentation of these results.
Disclosures
None.
References
- 1.Hoeffel EM, Rastogi S, Kim MO, Shahid H. The Asian Population: 2010. US Department of Commerce, Economics and Statistics Administration. US Census Bureau: Washington, DC; 2012. [Google Scholar]
- 2.Palaniappan L, Wang Y, Fortmann SP. Coronary heart disease mortality for six ethnic groups in California, 1990–2000. Ann Epidemiol. 2004; 14:499-506. [DOI] [PubMed] [Google Scholar]
- 3.Goff DC, Jr, Lloyd‐Jones DM, Bennett G, Coady S, D'Agostino RB, Sr, Gibbons R, Greenland P, Lackland DT, Levy D, O'Donnell CJ, Robinson J, Schwartz JS, Shero ST, Smith SC, Jr, Sorlie P, Stone NJ, Wilson PW. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014; 129:S49-S73. [DOI] [PubMed] [Google Scholar]
- 4.Safford MM, Brown TM, Muntner PM, Durant RW, Glasser S, Halanych JH, Shikany JM, Prineas RJ, Samdarshi T, Bittner VA, Lewis CE, Gamboa C, Cushman M, Howard V, Howard GInvestigators R. Association of race and sex with risk of incident acute coronary heart disease events. JAMA. 2012; 308:1768-1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dalton AR, Bottle A, Soljak M, Majeed A, Millett C. Ethnic group differences in cardiovascular risk assessment scores: national cross‐sectional study. Ethn Health. 2014; 19:367-384. [DOI] [PubMed] [Google Scholar]
- 6.Bhopal R, Fischbacher C, Vartiainen E, Unwin N, White M, Alberti G. Predicted and observed cardiovascular disease in South Asians: Application of FINRISK, Framingham and SCORE models to Newcastle Heart Project data. J Public Health (Oxf). 2005; 27:93-100. [DOI] [PubMed] [Google Scholar]
- 7.Kanjilal S, Rao VS, Mukherjee M, Natesha BK, Renuka KS, Sibi K, Iyengar SS, Kakkar VV. Application of cardiovascular disease risk prediction models and the relevance of novel biomarkers to risk stratification in Asian Indians. Vasc Health Risk Manag. 2008; 4:199-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berry JD, Liu K, Folsom AR, Lewis CE, Carr JJ, Polak JF, Shea S, Sidney S, O'Leary DH, Chan C, Lloyd‐Jones DM. Prevalence and progression of subclinical atherosclerosis in younger adults with low short‐term but high lifetime estimated risk for cardiovascular disease: the coronary artery risk development in young adults study and multi‐ethnic study of atherosclerosis. Circulation. 2009; 119:382-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lloyd‐Jones DM, Leip EP, Larson MG, D'Agostino RB, Beiser A, Wilson PW, Wolf PA, Levy D. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006; 113:791-798. [DOI] [PubMed] [Google Scholar]
- 10.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004; 291:210-215. [DOI] [PubMed] [Google Scholar]
- 11.Polonsky TS, McClelland RL, Jorgensen NW, Bild DE, Burke GL, Guerci AD, Greenland P. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010; 303:1610-1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacobs DR, Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi‐ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002; 156:871-881. [DOI] [PubMed] [Google Scholar]
- 13.Kanaya AM, Kandula N, Herrington D, Budoff MJ, Hulley S, Vittinghoff E, Liu K. Mediators of Atherosclerosis in South Asians Living in America (MASALA) study: objectives, methods, and cohort description. Clin Cardiol. 2013; 36:713-720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low‐density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18:499-502. [PubMed] [Google Scholar]
- 15.Grundy SM, Bazzarre T, Cleeman J, D'Agostino RB, Sr, Hill M, Houston‐Miller N, Kannel WB, Krauss R, Krumholz HM, Lauer RM, Ockene IS, Pasternak RC, Pearson T, Ridker PM, Wood D. Prevention Conference V: Beyond secondary prevention: identifying the high‐risk patient for primary prevention: medical office assessment: Writing Group I. Circulation. 2000; 101:E3-E11. [DOI] [PubMed] [Google Scholar]
- 16.National Heart Lung and Blood Institute. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002; 106:3143-3421. [PubMed] [Google Scholar]
- 17.Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, Greenland P, Van Horn L, Tracy RP, Lloyd‐Jones DM. Lifetime risks of cardiovascular disease. N Engl J Med. 2012; 366:321-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Detrano R. Quantification of coronary‐artery calcium using ultrafast computed‐tomography. J Am Coll Cardiol. 1990; 15:827-832. [DOI] [PubMed] [Google Scholar]
- 19.Marma AK, Berry JD, Ning H, Persell SD, Lloyd‐Jones DM. Distribution of 10‐year and lifetime predicted risks for cardiovascular disease in US adults: findings from the National Health and Nutrition Examination Survey 2003 to 2006. Circ Cardiovasc Qual Outcomes. 2010; 3:8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gawron A, Hou L, Ning H, Berry JD, Lloyd‐Jones DM. Lifetime risk for cancer death by sex and smoking status: the lifetime risk pooling project. Cancer Causes Control. 2012; 23:1729-1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Loria CM, Liu K, Lewis CE, Hulley SB, Sidney S, Schreiner PJ, Williams OD, Bild DE, Detrano R. Early adult risk factor levels and subsequent coronary artery calcification: The CARDIA study. J Am Coll Cardiol. 2007; 49:2013-2020. [DOI] [PubMed] [Google Scholar]
- 22.Kanaya AM, Herrington D, Vittinghoff E, Ewing SK, Liu K, Blaha MJ, Dave SS, Qureshi F, Kandula NR. Understanding the high prevalence of diabetes in US South Asians compared with four racial/ethnic groups: The MASALA and MESA studies. Diabetes Care. 2014; 37:1621-1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kanaya AM, Kandula NR, Ewing SK, Herrington D, Liu K, Blaha MJ, Srivastava S, Dave SS, Budoff MJ. Comparing coronary artery calcium among U.S. South Asians with four racial/ethnic groups: The MASALA and MESA studies. Atherosclerosis. 2014; 234:102-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taylor AJ, Kent SM, Flaherty PJ, Coyle LC, Markwood TT, Vernalis MN. ARBITER: Arterial Biology for the Investigation of the Treatment Effects of Reducing Cholesterol: a randomized trial comparing the effects of atorvastatin and pravastatin on carotid intima medial thickness. Circulation. 2002; 106:2055-2060. [DOI] [PubMed] [Google Scholar]
- 25.Crouse JR, III, Raichlen JS, Riley WA, Evans GW, Palmer MK, O'Leary DH, Grobbee DE, Bots ML, Group MS. Effect of rosuvastatin on progression of carotid intima‐media thickness in low‐risk individuals with subclinical atherosclerosis: The METEOR Trial. JAMA. 2007; 297:1344-1353. [DOI] [PubMed] [Google Scholar]
- 26.Anand SS, Yusuf S, Vuksan V, Devanesen S, Teo KK, Montague PA, Kelemen L, Yi C, Lonn E, Gerstein H, Hegele RA, McQueen M. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the study of health assessment and risk in ethnic groups (share). Lancet. 2000; 356:279-284. [DOI] [PubMed] [Google Scholar]
- 27.Chaturvedi N, Coady E, Mayet J, Wright AR, Shore AC, Byrd S, McG Thom SA, Kooner JS, Schalkwijk CG, Hughes AD. Indian Asian men have less peripheral arterial disease than European men for equivalent levels of coronary disease. Atherosclerosis. 2007; 193:204-212. [DOI] [PubMed] [Google Scholar]
- 28.Khalil A, Huffman MD, Prabhakaran D, Osmond C, Fall CH, Tandon N, Lakshmy R, Prabhakaran P, Biswas SK, Ramji S, Sachdev HS, Bhargava SKNew Delhi Birth C. Predictors of carotid intima‐media thickness and carotid plaque in young Indian adults: the New Delhi birth cohort. Int J Cardiol. 2013; 167:1322-1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Faeh D, William J, Yerly P, Paccaud F, Bovet P. Diabetes and pre‐diabetes are associated with cardiovascular risk factors and carotid/femoral intima‐media thickness independently of markers of insulin resistance and adiposity. Cardiovasc Diabetol. 2007; 6:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hippisley‐Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, Brindle P. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ. 2008; 336:1475-1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tillin T, Hughes AD, Whincup P, Mayet J, Sattar N, McKeigue PM, Chaturvedi N. Ethnicity and prediction of cardiovascular disease: performance of QRISK2 and Framingham scores in a U.K. tri‐ethnic prospective cohort study (SABRE–Southall and Brent REvisited). Heart. 2014; 100:60-67. [DOI] [PMC free article] [PubMed] [Google Scholar]


