Abstract
Background
Cerebrospinal fluid (CSF) flow dynamics play critical roles in both the immature and adult brain, with implications for neurodevelopment and disease processes such as hydrocephalus and neurodegeneration. Remarkably, the only reported method to date for measuring CSF formation in laboratory rats is the indirect tracer dilution method (a.k.a., ventriculocisternal perfusion), which has limitations.
New Method
Anesthetized rats were mounted in a stereotaxic apparatus, both lateral ventricles were cannulated, and the Sylvian aqueduct was occluded. Fluid exited one ventricle at a rate equal to the rate of CSF formation plus the rate of infusion (if any) into the contralateral ventricle. Pharmacological agents infused at a constant known rate into the contralateral ventricle were tested for their effect on CSF formation in real-time.
Results
The measured rate of CSF formation was increased by blockade of the Sylvian aqueduct but was not changed by increasing the outflow pressure (0–3 cm of H2O). In male Wistar rats, CSF formation was age-dependent: 0.39±0.06, 0.74±0.05, 1.02±0.04 and 1.40±0.06 µL/min at 8, 9, 10 and 12 weeks, respectively. CSF formation was reduced 57% by intraventricular infusion of the carbonic anhydrase inhibitor, acetazolamide.
Comparison with existing methods
Tracer dilution methods do not permit ongoing real-time determination of the rate of CSF formation, are not readily amenable to pharmacological manipulations, and require critical assumptions. Direct measurement of CSF formation overcomes these limitations.
Conclusions
Direct measurement of CSF formation in rats is feasible. Our method should prove useful for studying CSF dynamics in normal physiology and disease models.
Keywords: CSF formation, method, acetazolamide
1. Introduction
Cerebrospinal fluid (CSF) is a clear fluid found in the ventricular system and in the cranial and spinal subarachnoid spaces. CSF plays critical roles in health and disease (Johanson et al., 2008). Among its many functions, CSF imparts buoyancy to the brain that prevents its weight from distorting its structure or impeding venous outflow; it circulates growth factors critical for brain development; and it clears metabolic waste products produced during physiological activity (Redzic et al., 2005). There is a growing recognition of the important role of CSF dynamics in the maturation of the developing central nervous system (CNS), and the function of the mature CNS. For example, impaired CSF dynamics can result in disrupted corticogenesis in the developing brain (Feliciano et al., 2014) and may contribute to neurodegeneration in older adults (Iliff et al., 2012; Chikly and Quaghebeur, 2013; Iliff et al., 2013). In all age groups, disrupted CSF dynamics can manifest as hydrocephalus (Redzic et al., 2005).
The classical view of the CSF “circulatory system” is that CSF is formed by the choroid plexus (CP), circulates through the ventricular system, enters the subarachnoid space, and is reabsorbed into the venous system at the arachnoid granulations and villi (Cushing, 1914). However, recent investigations, as well as reassessments of published data, have called into question many of these concepts (Chikly and Quaghebeur, 2013; Brinker et al., 2014). While the CP is still considered an important source of CSF formation, its relative contribution compared to the cerebral endothelium and other pathways is currently being re-evaluated (Chikly and Quaghebeur, 2013; Brinker et al., 2014).
Many of the individual ion channels and transporters involved in the end-stages of ion and water transport required for CSF formation are known (Praetorius, 2007; Christensen et al., 2013; Damkier et al., 2013). Less well known are the upstream mechanisms that regulate these ion transport molecules to influence the rate of production and the composition of CSF. An important impediment to progress in this field is the lack of a suitable method for quantifying real-time CSF formation in laboratory rodents in vivo under near-physiological conditions.
Oreskovic and Klarica (2010) recently reviewed the most common methods that have been used to measure CSF formation. They identified important shortcomings with almost all of these methods, many of which provide indirect measures of CSF formation that require assumptions that may be difficult to justify. Other methods that provide direct measures of CSF formation require the use of non-physiological conditions or have been implemented only in larger animals such as sheep and cats. Here, we describe a simple method that permits the real-time measurement of the rate of formation of CSF in laboratory rats in vivo under near-physiological conditions.
2. Materials and methods
2.1. Animals
Animal experiments were performed under a protocol approved by the Institutional Animal Care and Use Committee (IACUC) of the University of Maryland, and in accordance with the guidelines and regulations in the NIH Guide for the Care and Use of Laboratory Animals. Male Wistar rats, ages 8–12 weeks (Harlan, Indianapolis, IN, USA), were anesthetized (60 mg/kg ketamine plus 7.5 mg/kg xylazine, IP) and allowed to breathe room air spontaneously. Body temperature was maintained at 37±1° C (Harvard Apparatus, Holliston, MA, USA) throughout the course of the experiments.
2.2. Procedure for measuring CSF formation
Anesthetized rats were mounted in a stereotactic apparatus (Stoelting Co., Wood Dale, IL) in the usual manner with an incisor-bar and ear-bars (Fig. 1). A midline scalp incision was made to expose the skull. A 1.3-mm burr hole, centered over the left lateral ventricle (x, −0.8 mm; y, +1.7 mm relative to bregma), was made using a high-speed drill. The dura and underlying arachnoid and pia were opened using a cruciate incision made with the tip of a #11 scalpel blade. The wound was irrigated with sterile normal saline (NS) to clear any blood.
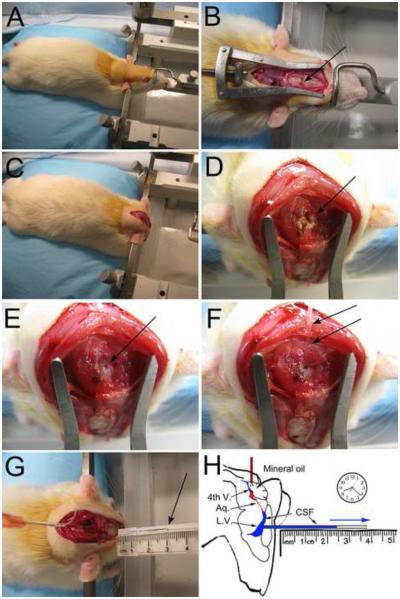
Figure 1. The experimental procedure for measuring CSF formation.
A–H: Photographs (A–G) and artistic depiction (H) of the procedure for measuring CSF formation. An anesthetized rat is mounted in a stereotactic apparatus in the usual manner with an incisor-bar and ear-bars (A); a midline scalp incision is made to expose the skull, and a 1.3-mm burr hole, centered over the left lateral ventricle (x, −0.8 mm; y, +1.7 mm relative to bregma), is made (B, arrow); the hind end of the animal is elevated ~2 cm, the incisor-bar is removed, the rat’s head is rotated on the ear-bars 90°, nose-down, and is held in this vertical position using an improvised plastic device pressing against the dorsum of the snout (C); the suboccipital muscles are bluntly dissected to expose the atlanto-occiptal ligament (D, arrow); the ligament is partially resected and the underlying dura is punctured in the midline (E, arrow); a 23 gauge flexible catheter (PE-20) loaded with sterile, molecular grade mineral oil pre-warmed to 37° C is advanced gently 5 mm through the foramen of Magendie into the 4th ventricle for infusion of mineral oil (100 µl) into the 4th ventricle to occlude the aqueduct of Sylvius (F, arrows); the left lateral ventricle is cannulated using a pre-marked glass capillary tube held horizontally in the correct “x” and “y” planes (now rotated 90°), and is carefully advanced by hand horizontally through the burr hole to a “z” coordinate of 4 mm to enter the frontal horn of the lateral ventricle, allowing CSF to exit (G, arrow); the distance traveled by the advancing front of fluid is used to calculate the rate of CSF formation (H).
After completing the burr hole and opening the membranes, the hind end of the animal was elevated ~2 cm, the incisor-bar was removed, the rat’s head was rotated on the ear-bars 90°, nose-down, and was held in this vertical position using an improvised plastic device pressing against the dorsum of the snout. The cisterna magna was exposed by dissecting the suboccipital muscles from the occipital bones and exposing the atlanto-occiptal ligament. The ligament was partially resected and the underlying dura was punctured in the midline to enter the cisterna magna, with the size of the dural puncture being ~1 mm2. A 23 gauge flexible catheter (PE-20) loaded with sterile, molecular grade mineral oil (Sigma Aldrich, St. Louis MO) pre-warmed to 37° C was advanced gently 5 mm through the foramen of Magendie into the 4th ventricle. Mineral oil (100 µl) was infused into the 4th ventricle to occlude the aqueduct of Sylvius.
Following occlusion of the aqueduct, with the long axis of the head still positioned vertically, the left lateral ventricle was cannulated using a pre-marked glass capillary tube (cat # CV8010-300; borosilicate; OD, 1 mm; ID, 0.8 mm; length, 30 cm; VitroCom, Mountain Lakes NJ). The capillary tube was held horizontally in the correct “x” and “y” planes (now rotated 90°), and was carefully advanced by hand horizontally through the burr hole to a “z” coordinate of 4 mm to enter the frontal horn of the lateral ventricle. The capillary tube, which often contained brain matter, was withdrawn and was replaced by a new capillary tube that was reintroduced into the ventricle.
After entering the ventricle, the capillary tube began to fill with CSF, with the front of fluid advancing steadily in the capillary tube as CSF was formed. We measured the distance that the front travelled within the capillary tube at precise intervals (5 or 10 min). The volume of CSF that formed was calculated as: volume = π × radius2 × distance. The rate of CSF formation (µL/min) was calculated as the slope of the volume-time relationship.
In a separate series of experiments, we examined the effect of collecting CSF at elevated outflow pressures (1.5 and 3 cm of H2O). For these experiments, we modified the outflow capillary tube by introducing two right-angle bends, 3 cm apart, to create a “Z” shape. Rotating the Z-shaped outflow capillary tube allowed measurements at different outflow pressures to be made in the same rat – when the plane of the “Z” was oriented horizontally, the outflow pressure was 0 cm of H2O; when the plane of the “Z” was rotated 45° from horizontal, the outflow pressure was 1.5 cm of H2O; when the plane of the “Z” was rotated 90° from horizontal, the outflow pressure was 3 cm of H2O.
2.3. Procedure for infusing drugs
In some rats, before rotating the head to a vertical orientation, a second burr hole was made over the right lateral ventricle (x: −0.8 mm, y: −1.7 mm relative to bregma) and the 28 gauge cannula from an Alzet brain infusion kit (#1; Durect, Cupertino, CA), with a single spacer to adjust the depth to 4.5 mm, was stereotactically placed in the ventricle and secured to the skull using cyanoacrylate adhesive. The cannula was connected via a PE-20 catheter to a 1 mL syringe containing an infusion solution (see below). The syringe was loaded into a syringe infusion apparatus (Pump elite 11, Harvard Apparatus) and maintained at 37° C. Intraventricular infusions were performed at a nominal pump rate of 2 µL/min. The actual rate of fluid delivery by the pump was determined empirically in a separate experiment, performed in triplicate, in which we measured the volume of fluid delivered over the course of 30 min. The actual rate was 1.93±0.03 µL/min. When measuring CSF formation during intraventricular drug infusion, the “actual infusion rate” of 1.93 µL/min was subtracted from the “measured outflow rate” to obtain the “calculated rate of CSF formation”. When measuring the effect of a drug (acetazolamide or mannitol, see below), first the baseline rate of CSF formation was determined during spontaneous CSF formation (no infusion), then the calculated rate of formation was determined after switching to the test drug. The infusion then was stopped, to check for reversibility of the drug effect.
Intraventricular infusion solutions were made using artificial CSF (aCSF), composed as follows (in mM): Na 150; K 3.0; Ca 1.4; Mg 0.8; P 1.0; Cl 155, pH 7.19 (Tocris, Bristol UK), with a calculated osmolarity of 311.2 mOsmC/L. Two drugs were studied, acetazolamide (45 mM; Sigma Aldrich, St. Louis MO) and mannitol (88.2 mM; Sigma Aldrich). Since acetazolamide is a weak acid, the high concentration was solubilized in aCSF titrated to pH 9.0 (no additional buffer). Acetazolamide (45 mM; pKa, 7.2; 98% ionized at pH 9.0) added an excess of 89.1 mOsmC/L; for pH 9.0, the solution of acetazolamide required 70 μL/mL of 0.5 N NaOH, which contributed an additional 70 mOsmC/L. Because of the high osmolarity of the acetazolamide infusion solution, we studied the effect of a solution of mannitol (88.2 mM, pH 9.0) in aCSF which, for pH 9.0, required 0.66 μL/mL of 0.5 N NaOH.
2.4. Procedure for validating aqueduct occlusion
We used an intraventricular infusion of hematoxylin and eosin (H&E) to check the integrity of the block of the aqueduct by mineral oil. In 3 rats, the aqueduct was occluded using mineral oil, as described above. In another 3 rats, nothing was placed in the 4th ventricle, allowing for CSF outflow from both the cannulated lateral ventricle and from the 4th ventricle. In both groups, CSF exiting the lateral ventricle was measured as above, and in both groups, H&E-containing aCSF was infused into the contralateral ventricle as described above. H&E-containing aCSF was infused at a nominal rate of 2 µL/min for 30 min. The rat then was euthanized by pentobarbital overdose, and was transcardially perfused with saline followed by 10% paraformaldehyde. In these cases, transcardial perfusion was performed with the rat’s head still held in the vertical orientation, to prevent loss of aqueductal occlusion and inadvertent spread of the H&E. These brains were embedded in OCT and frozen. The frozen block was photographed in the cryostat as it was cryosectioned to document the extent of H&E staining.
2.6. Data analysis
Numerical data are given as mean ± standard error of the mean (SE). Rates (µL/min) were calculated as the slope of the volume-time relationship, usually based on data collected over 30 min or more. Rates were determined for individual animals and were averaged across individuals of the same age. Calculations were performed using OriginPro (OriginLab Corporation, Northampton, MA).
3. Results
3.1. Aqueduct occlusion
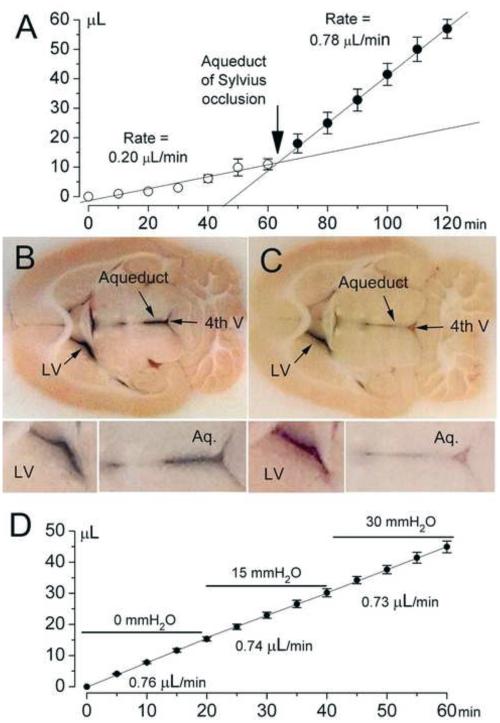
We compared CSF outflow from the cannulated lateral ventricle, without and with block of the aqueduct. In the absence of block, the average rate of CSF outflow in 3 rats over the course of 1 hr was 0.20 μL/min (Fig. 2A). In the same rats, blocking the aqueduct with mineral oil resulted in a 4-fold increase in the rate of outflow to 0.78 μL/min (9 weeks of age) (Fig. 2A).
Figure 2. The measured rate of CSF formation is increased by blockade of the Sylvian aqueduct but is not altered by increasing the outflow pressure.
A: CSF outflow from the left lateral ventricle was measured before and after occluding the 4th ventricle with mineral oil; before occlusion, the CSF outflow rate was 0.20 μL/min; after occlusion, the rate was 0.78 μL/min (3 rats; 9 weeks of age). B,C: Hematoxylin and eosin (H&E) staining of the ventricular system without (B) and with (C) occlusion of the 4th ventricle with mineral oil; H&E dye was infused into the right lateral ventricle; the lateral ventricles (LV) were stained in both cases, but the aqueduct (Aq.) and 4th ventricle (4th V) were stained only in (B), not in (C); the data shown are representative of findings in 3 rats per condition. D: CSF formation was measured at different outflow pressures; successive rates of 0.76, 0.74 and 0.73 μL/min (3 rats; 9 weeks of age) were observed with outflow pressures of 0, 1.5 and 3 cm of H2O, respectively.
We compared H&E staining of the ventricular system following intraventricular infusion of H&E, without and with block of the aqueduct. In the absence of block, prominent staining was observed in the lateral ventricles, the aqueduct and 4th ventricle (Fig. 2B). By contrast, in rats with mineral oil block of the aqueduct, staining was observed in the lateral ventricles, as expected, but the 4th ventricle was unstained (Fig. 2C). This experiment confirmed that mineral oil placed in the vertically oriented 4th ventricle was highly effective in blocking the aqueduct. All subsequent experiments were carried out with mineral oil occlusion of the aqueduct.
We next examined whether the outflow pressure at which CSF was collected would impact the measured rate of CSF formation. For each rat, we compared the effect of collecting CSF at 0, 1.5 and 3 cm of H2O. Rates of 0.76, 0.74 and 0.73 μL/min (9 weeks of age) were observed with outflow pressures of 0, 1.5 and 3 cm of H2O, respectively (Fig. 2D). All subsequent experiments were carried out using outflow pressures of 0 cm H2O.
3.2. Pharmacological inhibition of CSF formation
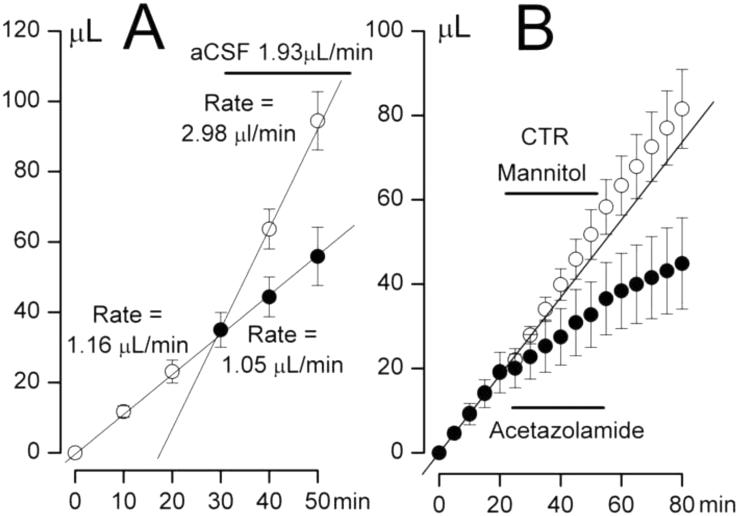
Studying CSF formation in real time during pharmacological inhibition requires intraventricular infusion of a drug solution at a known constant rate. We first evaluated this method by infusing aCSF. After cannulating the ventricle, the spontaneous rate of CSF formation was measured to be 1.16 μL/min (n=3; 11 weeks of age) (Fig. 3A). Infusion of aCSF at the rate of 1.93 μL/min yielded a measured outflow rate of 2.98 μL/min, or a calculated rate of CSF formation 1.05 μL/min, which was within 10% of the baseline rate.
Figure 3. Pharmacological inhibition of CSF formation by acetazolamide.
A: CSF outflow at baseline was 1.16 μL/min; infusion of aCSF (1.93 μL/min) yielded a measured outflow rate of 2.98 μL/min, or a calculated rate of CSF formation of 1.05 μL/min, within 10% of baseline (3 rats; 11 weeks of age). B: In two different experiments, CSF outflow at baseline was 0.95±0.23 μL/min (filled circles) or 0.96±0.03 μL/min (empty circles); infusion of acetazolamide (45 mM in aCSF; pH 9.0; 1.93 μL/min) or of mannitol (88.2 mM in aCSF; pH 9.0; 1.93 μL/min) yielded calculated rates of CSF formation 0.48±0.12 μL/min (filled circles) or of 1.12±0.17 μL/min (empty circles); based on these 2 experiments, inhibition by acetazolamide was calculated to be 57%; note that inhibition by acetazolamide was not reversible, with a rate of 0.38±0.10 μL/min observed after stopping infusion (3 rats/experiment; 10 weeks of age).
CSF formation is dependent on carbonic anhydrase (Praetorius, 2007; Christensen et al., 2013; Damkier et al., 2013). We thus sought to inhibit CSF formation pharmacologically using acetazolamide. Preliminary experiments showed that high concentrations of drug would have to be infused intraventricularly, likely due to the fact that active formation of CSF not only dilutes the infusate, but more importantly, it continuously washes drug away. Since acetazolamide is a weak acid, and since high concentrations of weak acids in aqueous solution are best obtained using basic pH, our drug infusion solution was titrated to pH 9.0.
Infusion of acetazolamide (45 mM in aCSF; pH 9.0) decreased the calculated rate of CSF formation from 0.95±0.23 to 0.48±0.12 µL/min (n=3; 10 weeks of age) (Fig. 3B). Inhibition of CSF formation by acetazolamide was not reversible, with a rate of 0.38±0.10 μL/min measured during 30 min after cessation of drug infusion.
The addition to aCSF of acetazolamide (45 mM) plus NaOH for pH 9.0 resulted in a large excess of osmols over that in aCSF alone. Because CSF formation depends on the osmolarity of the compartment into which CSF is secreted, we used an infusion of mannitol (88.2 mM in aCSF; pH 9.0) as a control. Infusion of the mannitol control solution increased the calculated rate of CSF formation from 0.96±0.03 to 1.12±0.17 µL/min (n=3; 10 weeks of age) (Fig. 3B). The rate of CSF formation returned to 1.00±0.12 µL/min, within 4% of the baseline value, after stopping the infusion. The observed increase in rate with mannitol likely reflected the increase in osmolarity due to the infusate (Krishnamurthy et al., 2009; Krishnamurthy et al., 2012), although additional experiments would be required to determine whether pH also had an effect. However, using this mannitol control infusion as baseline indicated that acetazolamide inhibited CSF formation by 57%, consistent with the overall process of CSF formation being highly dependent on HCO3− (Vogh et al., 1987).
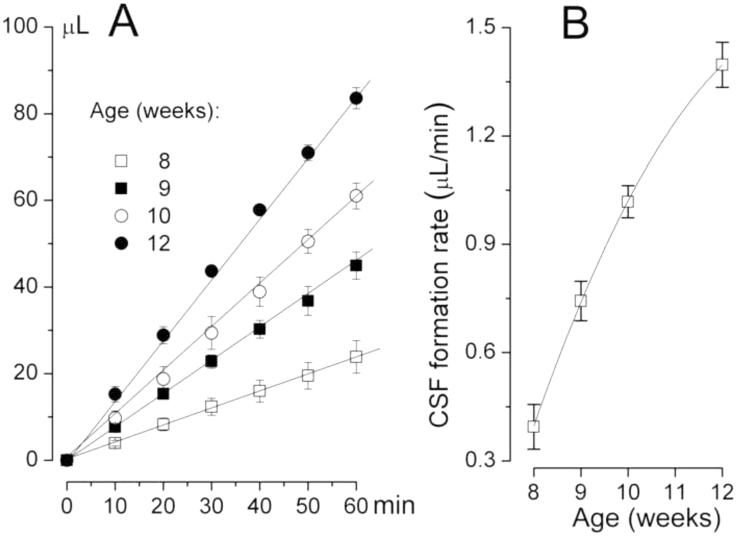
3.3. CSF formation is age-dependent
In the forgoing experiments, baseline rates of CSF formation were occasionally different between groups, likely due to differences in age (Preston, 2001; Chiu et al., 2012). We measured spontaneous CSF formation over the course of 60 min in rats of different ages. The rates measured were 0.39±0.06, 0.74±0.05, 1.02±0.04 and 1.40±0.06 µL/min at 8, 9, 10 and 12 weeks, respectively (3 rats/group) (Fig. 4A,B).
Figure 4. The effect of age on CSF formation.
A: CSF outflow at baseline was 0.39±0.06, 0.74±0.05, 1.02±0.04 and 1.40±0.06 µL/min at 8, 9, 10 and 12 weeks, respectively (3 rats/group). B: Plot of the rate of CSF formation by the choroid plexus of the lateral ventricles as a function of age; data from (A).
4. Discussion
The major finding of the present study is that we have developed a novel technique to perform direct real-time measurements of ongoing CSF formation by the brain of the rat in vivo. With this technique, it is feasible to study the effect of pharmacological manipulations on ongoing CSF formation. Our method is superior to the only other existing method in rodents, the tracer dilution method, which does not permit ongoing real-time determination of the rate of CSF formation, is not readily amenable to the study of pharmacological manipulations, and requires potentially confounding assumptions.
Many studies on CSF formation are carried out on cultured epithelial cells in vitro (Angelow et al., 2004; Hosoya et al., 2004; Baehr et al., 2006). As many as 8 methods have been described for measuring CSF formation in vivo (Oreskovic and Klarica, 2010). The indirect methods for measuring CSF formation in vivo include tracer dilution, MRI and others. All indirect methods require one or more assumption that may be difficult to justify. Some of the direct methods require the use of highly non-physiological conditions, such as removing brain tissues overlying the choroid plexus and collecting CSF under oil, removing CSF from the ventricle and observing the time needed to refill the ventricle, or extracorporeal perfusion of the choroid plexus. None of the 8 methods described to date is readily suited for directly quantifying CSF formation in laboratory rodents in vivo, in real-time, under near-physiological conditions. Notably, all of the direct methods described have been implemented only in large species such as sheep and cats.
The only method that has been used previously in rats to measure CSF formation is the indirect tracer dilution method (a.k.a., ventriculocisternal perfusion). In this method, blue dextran 2000 dye is infused into the lateral ventricle, samples of CSF are collected from the cisterna magna at fixed time intervals, and the concentration of dye is colorimetrically determined. Tracer dilution measurements in rats have yielded values for CSF formation rates of 1.2–1.8 μL/min at 3 months of age (Preston, 2001; Chiu et al., 2012). Reported values obtained by tracer dilution compare favorably to the value of 1.40±0.06 μL/min at 3 months of age that we obtained using our direct method.
Central to the classical view of CSF circulation is that CSF is secreted from the CP in the lateral ventricles and exits the brain after passing through the aqueduct of Sylvius. With our measurements, outflow from the cannulated lateral ventricle was 0.20 μL/min before blocking the aqueduct, and was 4-fold greater, 0.78 μL/min (9 weeks of age), after blocking the aqueduct, consistent with CSF traversing the aqueduct before occlusion. Most of our measurements were made at outflow pressures of 0 cm H2O, but we found that measurements of CSF formation differed <5% when made at outflow pressures of 3 cm H2O, which approaches the intraventricular pressure of 4–6 cm H2O at which CSF normally forms in the rat (Roy et al., 2013). This finding is consistent with the observation that CSF formation occurs by way of osmotic forces that are not influenced by the hydrostatic pressure of the compartment into which formation occurs (Damkier et al., 2013). Measurements of CSF formation at lower than normal intraventricular hydrostatic pressures obscure the potential for CSF absorption from within the ventricle, as shown by the work of Oreskovic and colleagues (Oreskovic et al., 2002; Klarica et al., 2009; Oreskovic and Klarica, 2010).
The method of blocking the aqueduct of Sylvius is important. Flexner and Winters (Flexner and Winters, 1932) blocked the aqueduct by inflating a balloon in the 4th ventricle. Oreskovic and Klarica (2010) criticized this as follows: “The pressure within the balloon was two times higher than the physiological one (about 160 mm H2O) and this non-physiological pressure, by influencing the sensitive adjacent tissue, probably caused a significant disturbance in CSF hydrodynamics and brain blood flow surrounding the balloon”. In their work on the cat, Oreskovic and colleagues did not block the aqueduct but instead cannulated it using a 1.2 mm O.D. tube plus cyanoacrylate glue on the outside of the tube to prevent CSF from leaking around it (Oreskovic et al., 2002). Dilation of the aqueduct by the tube plus exposure of the tissues to irritants in the glue also could harm delicate midbrain tissues. In our method, we blocked the aqueduct by placing 100 μL of mineral oil, pre-warmed to 37° C, into the 4th ventricle while the long axis of the head of the rat was positioned vertically, nose-down. The mineral oil was effective in blocking outflow from the aqueduct, as shown by the lack of staining of the 4th ventricle when H&E dye was infused into the lateral ventricle (Fig. 2). Importantly, blocking the aqueduct with mineral oil precluded anatomical distortion of delicate brainstem tissues by a balloon or by a catheter, produced no obvious physical injury to the tissues surrounding the 4th ventricle, and produced no obvious physiological disturbance to brainstem structures. Recordings of CSF formation could be performed over the course of several hours without disturbances in brainstem-controlled vital signs.
Pharmacological studies of CSF formation are complicated due to the effects of osmolarity and dilution. First, the increase in osmolarity that arises from adding study drug to aCSF can itself increase the production of CSF, since CSF formation is increased by increasing osmolarity (Krishnamurthy et al., 2009; Krishnamurthy et al., 2012). We observed a 17% increase in the rate of CSF formation when ventricular infusion of aCSH was changed to aCSF plus mannitol. Secondly, active CSF formation dilutes intraventricular infusate and continuously washes drug away, with both effects reducing the apparent efficacy of the drug under study. In our experiments, the concentration of acetazolamide that we used was appreciably greater than the EC50 value reported for inhibition of carbonic anhydrase (Ho et al., 2003). Given that the mannitol solution was infused at a rate of 1.93 μL/min and mixed with CSF that was being formed at a rate of 1.12 μL/min implies a dilution of the infusate to 63% of its starting concentration. Also, given that the mannitol infusate was at pH 9.0 (unbuffered) running at 1.93 μL/min, the dilution of OH− ions that occurs when it is mixed with a solution of pH 7.2 formed at 1.12 μL/min would yield a pH of 7.6. We found empirically that 28 mM acetazolamide (63% dilution) remains in solution at pH 7.6 at 37° C, suggesting that the apparent low efficacy of acetazolamide was not due to precipitation of drug within the ventricle. Importantly, these calculations involving dilution represent the “worst case scenario”, and ignore the fact that the rate of CSF formation is actually reduced by the drug – it is evident that, as inhibition takes hold, the degree of dilution is reduced accordingly.
Pharmacological manipulation of CSF formation in vivo remains challenging. At present, interventions in humans are extremely limited, due in part to the lack of organ specificity of candidate drugs that also affect renal function, and to the lack of molecular knowledge about the regulation of CSF formation. Parenteral administration of the carbonic anhydrase inhibitor, acetazolamide, is commonly used to reduce CSF formation in patients with idiopathic intracranial hypertension (pseudotumor cerebri), acute mountain sickness and other conditions associated with raised intracranial pressure (Fraser and Plant, 2011; Biousse, 2012; Ritchie et al., 2012). In our experiments, intraventricular infusion of acetazolamide reduced CSF formation by 57%. Intraventricular infusions of some drugs are used in humans, but usually only in an intensive care setting. Our data suggest that intraventricular infusion of acetazolamide or other inhibitors of CSF formation may be highly effective and may avoid the lack of organ specificity that limits current treatments.
Having a reliable, assumption-free method to measure the rate of CSF formation in laboratory rats will be important for studies on different disease states. For example, dysfunction of the CP and of the blood-cerebrospinal fluid barrier are believed to contribute to age-related cognitive decline and neurodegenerative disease (Chen et al., 2009). Abnormally low rates of CSF formation have been linked to the accumulation of neurotoxic substances, including amyloid-β, in aging and in Alzheimer's disease (Serot et al., 2011; Serot et al., 2012; Arbel-Ornath et al., 2013). Our data showing age-dependent rates of CSF formation accorded with previous work performed in rats studied using ventriculocisternal perfusion (Preston, 2001; Chiu et al., 2012), in sheep studied using an in situ perfused choroid plexus technique (Chen et al., 2009; Chen et al., 2010), and in humans studied using MRI (Bouzerar et al., 2013). The marked age-related changes in the rates of CSF formation observed by us and others point to important upstream mechanisms in CSF regulation that are only beginning to be explored (Johanson et al., 2008).
HIGHLIGHTS.
CSF formation is critical for normal brain health
Abnormalities are implicated in brain maldevelopment, degeneration, hydrocephalus
In rats, CSF formation has only been measured indirectly
We describe a novel method for direct measurement of CSF formation in rats
Our method will advance studies on development, aging and hydrocephalus
Acknowledgments
Funding
This work was supported by grants to JMS from the Department of Veterans Affairs (Baltimore) (BX001629), the National Institute of Neurological Disorders and Stroke (NINDS) (NS060801; NS061808), the National Heart, Lung and Blood Institute (HL082517); to VG from NINDS (NS061934; NS072501); and by a AANS/CNS Dempsey Cerebrovascular Research Award to KTK.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Angelow S, Zeni P, Galla HJ. Usefulness and limitation of primary cultured porcine choroid plexus epithelial cells as an in vitro model to study drug transport at the blood-CSF barrier. Adv. Drug Deliv. Rev. 2004;56:1859–73. doi: 10.1016/j.addr.2004.07.012. [DOI] [PubMed] [Google Scholar]
- Arbel-Ornath M, Hudry E, Eikermann-Haerter K, Hou S, Gregory JL, Zhao L, Betensky RA, Frosch MP, Greenberg SM, Bacskai BJ. Interstitial fluid drainage is impaired in ischemic stroke and Alzheimer's disease mouse models. Acta Neuropathol. 2013;126:353–64. doi: 10.1007/s00401-013-1145-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baehr C, Reichel V, Fricker G. Choroid plexus epithelial monolayers--a cell culture model from porcine brain. Cerebrospinal. Fluid Res. 2006;3:13. doi: 10.1186/1743-8454-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biousse V. Idiopathic intracranial hypertension: Diagnosis, monitoring and treatment. Rev. Neurol. (Paris) 2012;168:673–83. doi: 10.1016/j.neurol.2012.07.018. [DOI] [PubMed] [Google Scholar]
- Bouzerar R, Chaarani B, Gondry-Jouet C, Zmudka J, Baledent O. Measurement of choroid plexus perfusion using dynamic susceptibility MR imaging: capillary permeability and age-related changes. Neuroradiology. 2013;55:1447–54. doi: 10.1007/s00234-013-1290-2. [DOI] [PubMed] [Google Scholar]
- Brinker T, Stopa E, Morrison J, Klinge P. A new look at cerebrospinal fluid circulation. Fluids Barriers. CNS. 2014;11:10. doi: 10.1186/2045-8118-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen RL, Chen CP, Preston JE. Elevation of CSF albumin in old sheep: relations to CSF turnover and albumin extraction at blood-CSF barrier. J. Neurochem. 2010;113:1230–9. doi: 10.1111/j.1471-4159.2010.06689.x. [DOI] [PubMed] [Google Scholar]
- Chen RL, Kassem NA, Redzic ZB, Chen CP, Segal MB, Preston JE. Age-related changes in choroid plexus and blood-cerebrospinal fluid barrier function in the sheep. Exp. Gerontol. 2009;44:289–96. doi: 10.1016/j.exger.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Chikly B, Quaghebeur J. Reassessing cerebrospinal fluid (CSF) hydrodynamics: a literature review presenting a novel hypothesis for CSF physiology. J. Bodyw. Mov Ther. 2013;17:344–54. doi: 10.1016/j.jbmt.2013.02.002. [DOI] [PubMed] [Google Scholar]
- Chiu C, Miller MC, Caralopoulos IN, Worden MS, Brinker T, Gordon ZN, Johanson CE, Silverberg GD. Temporal course of cerebrospinal fluid dynamics and amyloid accumulation in the aging rat brain from three to thirty months. Fluids Barriers. CNS. 2012;9:3. doi: 10.1186/2045-8118-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen HL, Nguyen AT, Pedersen FD, Damkier HH. Na(+) dependent acid-base transporters in the choroid plexus; insights from slc4 and slc9 gene deletion studies. Front Physiol. 2013;4:304. doi: 10.3389/fphys.2013.00304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cushing H. Studies on the Cerebro-Spinal Fluid : I. Introduction. J. Med. Res. 1914;31:1–19. [PMC free article] [PubMed] [Google Scholar]
- Damkier HH, Brown PD, Praetorius J. Cerebrospinal fluid secretion by the choroid plexus. Physiol Rev. 2013;93:1847–92. doi: 10.1152/physrev.00004.2013. [DOI] [PubMed] [Google Scholar]
- Feliciano DM, Zhang S, Nasrallah CM, Lisgo SN, Bordey A. Embryonic cerebrospinal fluid nanovesicles carry evolutionarily conserved molecules and promote neural stem cell amplification. PLoS. One. 2014;9:e88810. doi: 10.1371/journal.pone.0088810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flexner IB, Winters H. The rate of formation of cerebrospinal fluid in etherized cats. Am. J. Physiol. 1932;101:697–710. [Google Scholar]
- Fraser C, Plant GT. The syndrome of pseudotumour cerebri and idiopathic intracranial hypertension. Curr. Opin. Neurol. 2011;24:12–7. doi: 10.1097/WCO.0b013e328341f94a. [DOI] [PubMed] [Google Scholar]
- Ho YT, Purohit A, Vicker N, Newman SP, Robinson JJ, Leese MP, Ganeshapillai D, Woo LW, Potter BV, Reed MJ. Inhibition of carbonic anhydrase II by steroidal and non-steroidal sulphamates. Biochem. Biophys. Res. Commun. 2003;305:909–14. doi: 10.1016/s0006-291x(03)00865-9. [DOI] [PubMed] [Google Scholar]
- Hosoya K, Hori S, Ohtsuki S, Terasaki T. A new in vitro model for blood-cerebrospinal fluid barrier transport studies: an immortalized choroid plexus epithelial cell line derived from the tsA58 SV40 large T-antigen gene transgenic rat. Adv. Drug Deliv. Rev. 2004;56:1875–85. doi: 10.1016/j.addr.2004.07.013. [DOI] [PubMed] [Google Scholar]
- Iliff JJ, Lee H, Yu M, Feng T, Logan J, Nedergaard M, Benveniste H. Brain-wide pathway for waste clearance captured by contrast-enhanced MRI. J. Clin. Invest. 2013;123:1299–309. doi: 10.1172/JCI67677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, Benveniste H, Vates GE, Deane R, Goldman SA, Nagelhus EA, Nedergaard M. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid beta. Sci. Transl. Med. 2012;4:147ra111. doi: 10.1126/scitranslmed.3003748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johanson CE, Duncan JA, III, Klinge PM, Brinker T, Stopa EG, Silverberg GD. Multiplicity of cerebrospinal fluid functions: New challenges in health and disease. Cerebrospinal. Fluid Res. 2008;5:10. doi: 10.1186/1743-8454-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klarica M, Oreskovic D, Bozic B, Vukic M, Butkovic V, Bulat M. New experimental model of acute aqueductal blockage in cats: effects on cerebrospinal fluid pressure and the size of brain ventricles. Neuroscience. 2009;158:1397–405. doi: 10.1016/j.neuroscience.2008.11.041. [DOI] [PubMed] [Google Scholar]
- Krishnamurthy S, Li J, Schultz L, Jenrow KA. Increased CSF osmolarity reversibly induces hydrocephalus in the normal rat brain. Fluids Barriers. CNS. 2012;9:13. doi: 10.1186/2045-8118-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnamurthy S, Li J, Schultz L, McAllister JP. Intraventricular infusion of hyperosmolar dextran induces hydrocephalus: a novel animal model of hydrocephalus. Cerebrospinal. Fluid Res. 2009;6:16. doi: 10.1186/1743-8454-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oreskovic D, Klarica M. The formation of cerebrospinal fluid: nearly a hundred years of interpretations and misinterpretations. Brain Res. Rev. 2010;64:241–62. doi: 10.1016/j.brainresrev.2010.04.006. [DOI] [PubMed] [Google Scholar]
- Oreskovic D, Klarica M, Vukic M. The formation and circulation of cerebrospinal fluid inside the cat brain ventricles: a fact or an illusion? Neurosci. Lett. 2002;327:103–6. doi: 10.1016/s0304-3940(02)00395-6. [DOI] [PubMed] [Google Scholar]
- Praetorius J. Water and solute secretion by the choroid plexus. Pflugers Arch. 2007;454:1–18. doi: 10.1007/s00424-006-0170-6. [DOI] [PubMed] [Google Scholar]
- Preston JE. Ageing choroid plexus-cerebrospinal fluid system. Microsc. Res. Tech. 2001;52:31–7. doi: 10.1002/1097-0029(20010101)52:1<31::AID-JEMT5>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- Redzic ZB, Preston JE, Duncan JA, Chodobski A, Szmydynger-Chodobska J. The choroid plexus-cerebrospinal fluid system: from development to aging. Curr. Top. Dev. Biol. 2005;71:1–52. doi: 10.1016/S0070-2153(05)71001-2. [DOI] [PubMed] [Google Scholar]
- Ritchie ND, Baggott AV, Andrew Todd WT. Acetazolamide for the prevention of acute mountain sickness--a systematic review and meta-analysis. J. Travel. Med. 2012;19:298–307. doi: 10.1111/j.1708-8305.2012.00629.x. [DOI] [PubMed] [Google Scholar]
- Roy CU, Holman BH, Fautsch MP. A novel rat model to study the role of intracranial pressure modulation on optic neuropathies. PLoS. One. 2013;8:e82151. doi: 10.1371/journal.pone.0082151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serot JM, Peltier J, Fichten A, Ledeme N, Bourgeois AM, Jouanny P, Toussaint P, Legars D, Godefroy O, Maziere JC. Reduced CSF turnover and decreased ventricular Abeta42 levels are related. BMC. Neurosci. 2011;12:42. doi: 10.1186/1471-2202-12-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serot JM, Zmudka J, Jouanny P. A possible role for CSF turnover and choroid plexus in the pathogenesis of late onset Alzheimer's disease. J. Alzheimers. Dis. 2012;30:17–26. doi: 10.3233/JAD-2012-111964. [DOI] [PubMed] [Google Scholar]
- Vogh BP, Godman DR, Maren TH. Effect of AlCl3 and other acids on cerebrospinal fluid production: a correction. J. Pharmacol. Exp. Ther. 1987;243:35–9. [PubMed] [Google Scholar]