Abstract
Chronic subdural hematomas (SDHs) associated with non-operated moyamoya disease are extremely rare. A 68-year-old woman underwent burr-hole surgery for a right SDH, which resolved completely. On day 3, however, the patient suffered cerebral infarction in the right parietal lobe. Cerebral angiography demonstrated total occlusion of the bilateral internal carotid arteries with transdural anastomoses via branches of the right occipital artery and middle meningeal artery, feeding the left parietal cortex. A branch of the right middle meningeal artery passed near the burr hole, but was preserved. The patient was diagnosed of moyamoya disease. We thought that the main cause of chronic SDH might be the disruption of transdural anastomoses. Furthermore, we also hypothesized that we might have coagulated the small vessels of the transdural anastomoses which were undetectable by postoperative angiography, and that cerebral infarction might occur.
Keywords: Burr-hole surgery, cerebral infarction, chronic subdural hematoma, moyamoya disease, transdural anastomosis
Introduction
Moyamoya disease is a progressive occlusive disease of the cerebral vasculature, with particular involvement of the internal carotid artery or its terminal branches, accompanied by the formation of abnormal extensive collateral networks in the basal ganglia, leptomeningeal anastomoses, and multiple transdural anastomoses.[1]
The common onsets are ischemic attacks in children and intracranial hemorrhages in adults. Intracranial hemorrhages associated with moyamoya disease are commonly intracerebral, intraventricular, or subarachnoid.[1,2] Subdural hematomas (SDHs) have also recently been described in moyamoya disease, mostly in acute or subacute cases.[3,4,5,6,7] Several authors have reported chronic SDHs following bypass surgery, including surgery for moyamoya disease,[8,9,10] but only two cases of chronic SDHs associated with non-operated moyamoya disease have previously been reported.[11,12] We present a rare case of chronic SDH associated with moyamoya disease.
Case Report
A 68-year-old woman was admitted to our hospital with dysesthesia of her left upper extremity. She had a past history of mild hypertrophic cardiomyopathy. There was no history of trauma and no family history of hereditary disease, including moyamoya disease or ischemic stroke. Physical examinations on admission were normal. Neurologic examinations revealed an alert consciousness, no motor weakness, and mild dysesthesia of her left upper extremity. A head computed tomography (CT) scan revealed a chronic SDH in the right frontoparietal region [Figure 1a]. Burr-hole surgery was performed under local anesthesia. We decided on a regular burr hole at the point of maximal SDH thickness, at the parietal bone, approximately 3 cm behind the coronal suture. A burr hole was made with a hand drill, following a small linear skin incision. The dura was coagulated and a cross-shaped incision was made. No major branches of the superficial temporal artery, middle meningeal artery, or occipital artery were detected. After incision of the outer SDH membrane, a drainage catheter was placed into the subdural space. No aspiration with negative pressure or flushing with normal saline was performed. Vital signs were normal during surgery. Dysesthesia resolved completely after surgery, and the drainage catheter was removed the day after surgery. On day 3, however, the patient presented with left-sided hemiparesis. A head CT scan showed no postoperative hemorrhage, and cerebral infarction was suspected. A free-radical scavenger was administered for 2 weeks. On day 11, diffusion-weighted magnetic resonance imaging revealed elevated diffusion coefficients with high signal intensity in the right parietal cortex [Figure 1b]. Laboratory tests were normal. Cardiac ultrasonography showed good wall motion and an ejection fraction rate of 91%. No intracardiac thrombus was detected. Cerebral angiography on day 19 demonstrated total occlusion of bilateral internal carotid arteries, with ethmoidal moyamoya vessels [Figure 2], and significant collateral flow from the posterior cerebral arteries. Right external carotid angiography revealed transdural anastomoses via branches of the right occipital artery and middle meningeal artery, feeding the left parietal cortex [Figure 3]. A branch of the right middle meningeal artery passed near the burr hole, but was preserved [Figure 4]. The patient was diagnosed of moyamoya disease. Brain single photon emission CT revealed no abnormal cerebral blood flow. The patient made a full recovery and was discharged on day 39.
Figure 1.

(a) Head computed tomography scan on admission showing a chronic SDH in the right frontoparietal region; (b) Diffusion-weighted magnetic resonance imaging on day 11 showing elevated diffusion coefficients with high signal intensity in the right parietal cortex
Figure 2.

Left (a); and right (b) carotid angiography (lateral view) on day 19 showing occlusion of the top of the bilateral internal carotid arteries, with ethmoidal moyamoya vessels
Figure 3.

Right external carotid angiography (anterolateral views) demonstrating transdural anastomoses via branches of the right occipital artery and middle meningeal artery, feeding the left parietal cortex. (a) Early phase; (b) Late phase. Note the branch of the middle meningeal artery (arrow), occipital artery (arrow head), and the transdural anastomosis feeding the left parietal cortex (large arrow)
Figure 4.
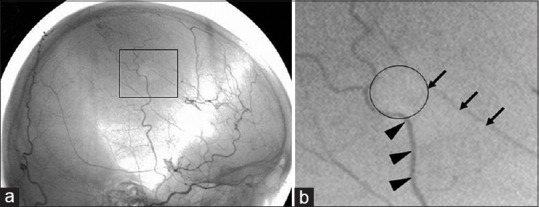
(a) Right external carotid angiography (lateral view) demonstrating that a branch of the right middle meningeal artery passes near a point of the burr hole, but is preserved; (b) Enlargement of the square area. Note the margin of the burr hole (circle), branch of the middle meningeal artery (arrow), and branch of the superficial temporal artery (arrow head)
Discussion
Chronic SDHs associated with non-operated moyamoya disease are extremely rare, with only two reported cases.[11,12] Ito et al. reported a case of acute carotid arterial occlusion after burr-hole surgery for chronic SDH associated with moyamoya disease.[11] Matsumura and Nojiri reported a case of resolved chronic SDH associated with acute SDH in moyamoya disease, and suggested that the chronic SDH might have been caused by antiplatelet agents, which the patient had been prescribed for ischemic attack, and by minor bleeding caused by disruption of transdural anastomoses.[12]
In our case, the patient received no antiplatelet agents and had no history of head trauma. We thought that the main cause of chronic SDH might be the disruption of transdural anastomoses. Our patient had a history of mild hypertrophic cardiomyopathy. Cardiac ultrasonography showed good wall motion and a high ejection fraction, without intracardiac thrombus, but we were unable to exclude cardiogenic factors as the cause of the cerebral infarction. It is also possible that cerebral infarction might have been caused by disruption of the inner membrane by the drain catheter, suggested by Nakaguchi et al.[13] Furthermore, we can also hypothesize that we might have coagulated the small vessels of the transdural anastomoses which were undetectable by postoperative angiography, and that cerebral infarction might occur.
Chronic SDH is a very common neurosurgical entity, whereas chronic SDH associated with moyamoya disease is rare. Therefore, we cannot suggest the investigation on the presence of vascular abnormalities in every patient with chronic SDH. This case suggests that more attention should be paid to the presence of vascular abnormalities including moyamoya disease, especially when cerebral ischemia occurs after surgery for acute or chronic SDH.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Scott RM, Smith ER. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009;360:1226–37. doi: 10.1056/NEJMra0804622. [DOI] [PubMed] [Google Scholar]
- 2.Aoki N, Mizutani H. Does moyamoya disease cause subarachnoid hemorrhage? Review of 54 cases with intracranial hemorrhage confirmed by computerized tomography. J Neurosurg. 1984;60:348–53. doi: 10.3171/jns.1984.60.2.0348. [DOI] [PubMed] [Google Scholar]
- 3.Kawakami K, Takahashi S, Sonobe M, Koshu K, Hirota S, Kusunose M. Subacute subdural hematoma associated with moyamoya phenomenon-a case report. No Shinkei Geka. 1988;16:205–9. [PubMed] [Google Scholar]
- 4.Nakakita K, Tanaka S, Fukuda A, Fujii C, Kohama A, Miyasato H. Nontraumatic acute subdural hematoma caused by the rupture of transdural anastomotic vessels in moyamoya disease. No Shinkei Geka. 1984;22:561–5. [PubMed] [Google Scholar]
- 5.Oppenheim JS, Gennuso R, Sacher M, Hollis P. Acute atraumatic subdural hematoma associated with moyamoya disease in an African-American. Neurosurgery. 1991;28:616–8. doi: 10.1097/00006123-199104000-00026. [DOI] [PubMed] [Google Scholar]
- 6.Shen WC, Lee WY. Moyamoya disease causes acute subdural hematomas and sudden death: A case report. Zhonghua Yi Xue Za Zhi (Taipei) 1998;61:619–23. [PubMed] [Google Scholar]
- 7.Takeuchi S, Ichikawa A, Koike T, Tanaka R, Arai H. Acute subdural hematoma in young patient with moyamoya disease-case report. Neurol Med Chir (Tokyo) 1992;32:80–3. doi: 10.2176/nmc.32.80. [DOI] [PubMed] [Google Scholar]
- 8.Andoh T, Sakai N, Yamada H, Yano H, Hirayama H, Imao Y, et al. Chronic subdural hematoma following bypass surgery-report of three cases. Neurol Med Chir (Tokyo) 1992;32:684–9. doi: 10.2176/nmc.32.684. [DOI] [PubMed] [Google Scholar]
- 9.Nakagawa Y, Shimoyama M, Kashiwaba T, Suzuki Y, Gotoh S, Miyasaka K, et al. Reconstructive operation of Moyamoya disease and its problems. No Shinkei Geka. 1981;9:305–14. [PubMed] [Google Scholar]
- 10.Sonobe M, Takahashi S, Kubota Y, Shirane R. Chronic subdural hematoma developing after EMS for moyamoya disease. No Shinkei Geka. 1982;10:857–9. [PubMed] [Google Scholar]
- 11.Ito S, Miyazaki H, Iino N, Shiokawa Y, Saito I. Acute carotid arterial occlusion after burr hole surgery for chronic subdural haematoma in moyamoya disease. J Clin Neurosci. 2004;11:778–80. doi: 10.1016/j.jocn.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 12.Matsumura M, Nojiri K. Resolved chronic subdural hematoma associated with acute subdural hematoma in moyamoya disease. Neurol Med Chir (Tokyo) 1984;24:622–7. doi: 10.2176/nmc.24.622. [DOI] [PubMed] [Google Scholar]
- 13.Nakaguchi H, Yoshimasu N, Tanishima T. Relationship between the natural history of chronic subdural hematoma and enhancement of the inner membrane on post-contrast CT scan. No Shinkei Geka. 2003;31:157–64. [PubMed] [Google Scholar]


