Abstract
Aim:
Intramedullary spinal cord tumors (IMSCT) are rare neoplasms of central nervous system but require proper evaluation and management to ensure a good outcome. This study was carried out to evaluate the functional outcome of IMSCT following surgery and to decipher the factors affecting optimal outcome of these cases.
Materials and Methods:
A prospective clinical study was carried out at a tertiary care center from 2003 to 2012. Forty three patients with intramedullary tumors diagnosed on magnetic resonance imaging were included. Their clinical details, neurological findings and demographic data were recorded. The patients were then subjected to surgery and adjuvant radiotherapy. The patients were followedup clinically and radiologically, and all parameters examined and recorded.
Results:
Sensory and motor impairment was present preoperatively in majority of patients (n = 39 and n = 38, 90.7% and 88.4%, respectively). Gross total excision was performed in 30 cases (69.76%). The most common histological diagnosis was ependymoma (n = 21, 48.8%). Postoperatively 32 patients (74.4%) were in McCormick functional Grade I or II improving from 13 cases (30.2%) in Grade I or II preoperatively. Fifteen of 17 patients in Medical Research Council (MRC) Grade III and 10 out of 12 patients in Grade MRC IV improved. No mortality was recorded during the entire period of follow-up (mean: 22, range: 3-96 months). Eight patients (18.6%) had recurrence till the last follow-up visit.
Conclusions:
Preoperative neurological grade was the most important predictor of functional outcome. Gross tumor excision was the best surgical modality to improve event free survival. High-grade tumors had higher rates of recurrence but no effect on functional outcome.
Keywords: Ependymoma, functional outcome, intramedullary tumor, radical excision
Introduction
Intramedullary spinal cord tumors (IMSCT) are rare accounting for about 6% of all central nervous system tumors. They arise from the neural tissue of the spinal cord with propensity for the variable degree of neurological compromise. Intramedullary position poses complications in the surgical excision of these tumors because of their intricate origin. The clinical signs and symptoms of these tumors are due to mass effect and neurological dysfunction.[1] The lack of any specific clinical characteristic often precludes early diagnosis of the lesion and results in most patients being diagnosed with advanced neurological impairments such as paralysis and bladder incontinence.[2] Radiological evaluation with magnetic resonance imaging (MRI) has however led to decreased lag time in the diagnosis of such lesions.[3] The management of IMSCTs is mainly surgical, however, the proximity and intimate involvement of neural tracts in the tumor makes surgery difficult and increases the surgical morbidity. The aggressive surgical procedures result in deterioration of the neurological status and hence a more conservative excision of the tumor with adjuvant radiotherapy may be an available alternative.[4,5] Multiple studies have proven that optimum surgical excision of the tumor provides the best outcome.[6,7,8] In tumors which have definite plane there is a general consensus toward total excision but controversy still exists between radical tumor excision and near total excisions with adjuvant therapy particularly in tumors with ill-defined margins/planes. The role of adjuvant therapy is also variable in different histotypes and depends on the totality of excision of tumors. The role of chemotherapy is still questionable in spinal tumors.
With these points in mind we studied the clinical presentation, histological diagnosis, management and functional outcome of patients presenting with IMSCTs.
Materials and Methods
The study was a prospective clinical study carried out at a tertiary care center from 2003 to 2012. All patients presenting with neurological clinical features were evaluated thoroughly by academic residents of neurosurgery. They were subjected to systematic physical and neurological evaluation, and radio-diagnostic studies were performed and any doubtful features were checked by an academic faculty. The standard diagnostic tool was MRI (with or without contrast). Fifty-one patients with suspected intramedullary spinal mass were further evaluated on MRI of which 48 had spinal intramedullary tumors, three patients with recurrence were excluded. These three patients had been treated elsewhere, and the exact nature and details of their treatment were not available.
The clinical details and demographic data of each case were recorded. Their motor and sensory functions were documented. The motor power grading was done using the Medical Research Council (MRC) grading. The sensory compromises were recorded quantitatively. Sphincter functions were assessed and recorded. The level of lesion was recorded.
The patients were then subjected to surgery after obtaining anesthetic clearance following requisite investigations for anesthetic and other considerations. All patients were operated upon by a single senior neuro-surgeon. All efforts were made to remove the tumor intoto Gross total excision was defined as no visual evidence of tumor on the surgical field on operating microscope. Near total excision was defined as <10% residual tumor mass following surgery. Sub-total excision involved removal of 50-90% of tumor tissue by the end of surgical procedure. The surgeries were carried out under an operating microscope. The surgeon decided on his clinical experience and visual confirmation the extent of dissection and resection required.
The excised tumor mass was then examined by two senior pathologists concurrently to arrive at a histological diagnosis.
Postoperatively patients were subjected to adjuvant radiotherapy. The patients were then followed-up clinically and radiologically at 6 weeks, 3, 6, and 12 months and thereafter depending on neurological progression. Only those patients having a follow-up of more than 3 months were included in the present series. Neurological examination was carried out at each follow-up and recorded in terms of improvement, deterioration or stabilization. Any evidence of recurrence was duly noted and diligently followed-up with further diagnostic work-up. All complications were noted and treated as required. McCormick's functional classification was used to assess the functional outcome of the patients postsurgery.[9] The data generated was subjected to statistical analysis using IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp and two-tailed Fisher's t-test was used to calculate significance.
Observations
Of the total 48 patients presenting with intramedullary tumors, intraoperatively and following the histo-pathological diagnosis one case with tuberculoma and two cases with benign growths (lipoma) were excluded. Two patients were lost to follow-up and were not included in the analysis. The remaining 43 patients were assessed for the study. Male patients constituted a majority of the study group (72%, n = 31). The patients ranged from pediatric age group (3 years) to geriatric population (63 years) with a mean age of 27.4 years.
Being a tertiary care center and a referral hospital most patients presented to us with long duration of symptoms, (mean = 25.6 months, range - 1-45 months). The most common clinical presentation was back pain (upper and lower) which was documented in 82% patients (n = 34). On detailed neurological examination, nearly all patients had some degree of impairment [Table 1]. Sensory derangement was present in 39 patients (90.7%) but dissociated sensory loss was seen in only 19 cases (44.1%). Sphincteric functions were impaired in 22 cases (51.2%). While motor deterioration was seen in 38 patients (88.4%) with most common preoperative power grade being MRC Grade III (n = 17, 39.5%). Dorsal spine was most commonly affected region with 22 cases (51.6%) followed by cervical spine (n = 12, 27.9%) [Figure 1].
Table 1.
Preoperative neurological status
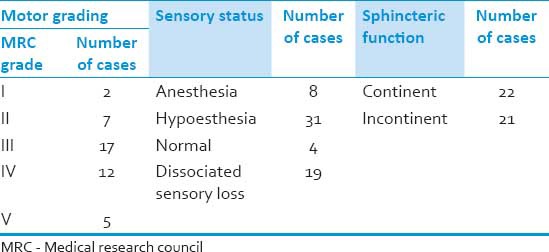
Figure 1.
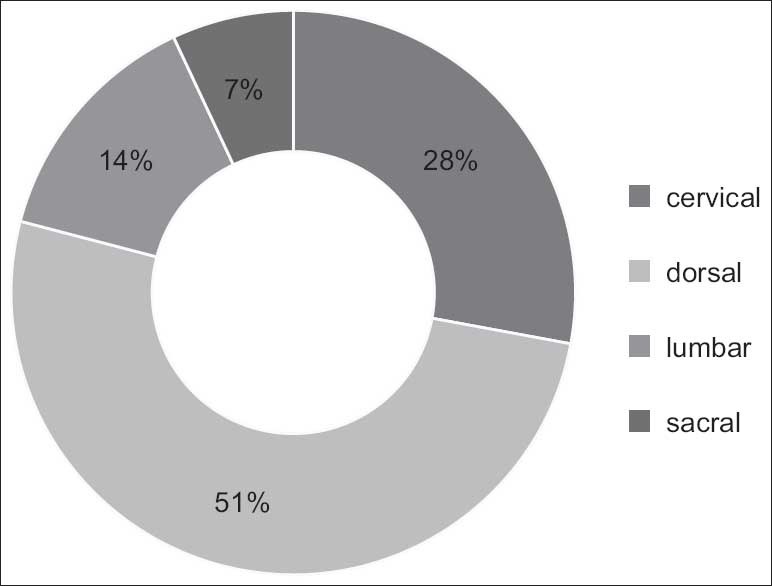
Spinal region of involvement
Gross total excision was performed in 30 cases (69.76%) the rest being near total excisions (n = 13, 30.2%). Fourteen patients (32.5%) were subjected to adjuvant radio-therapy in addition to surgery. On histopathological diagnosis the most common tumor type was ependymoma (n = 21, 48.8%) followed by astrocytoma (n = 12) cases [Figure 2]. The rest were hemangioblastomas (n = 5, 11%), scwannomas (n = 3) and gangliogliomas (n = 2). Of the astrocytomas, eight were anaplastic/high grade; similarly seven ependymomas were high grade on histopathological examination.
Figure 2.
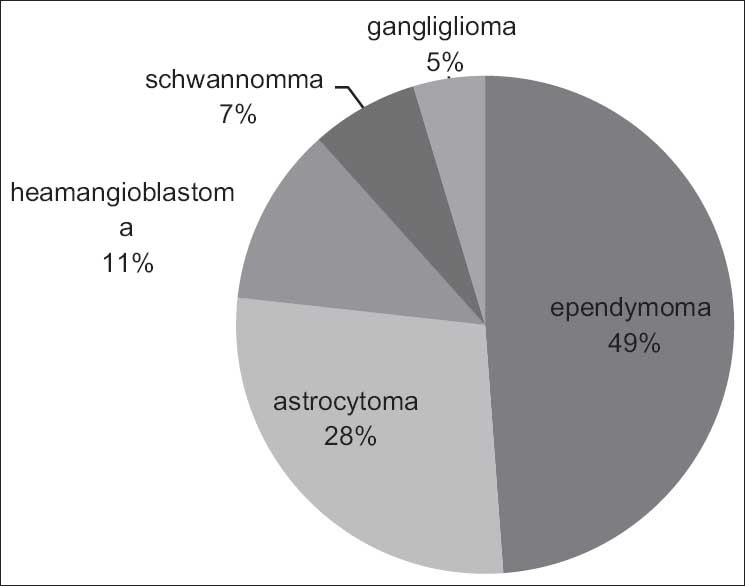
Histopathological diagnosis
Immediately after surgery 65% of cases (n = 28) showed a transient decline in the neurological status due to cord handling and edema, which stabilized over the recovery period. Neurological evaluation was then carried out at discharge and subsequently at every follow-up visit. Treatment led to an improvement in muscle power in 28 cases (65.1%) with only five cases showing deterioration while 10 cases remained stable, similarly 27 cases (62.8%) showed sensory improvement and four patients showed deterioration at average follow-up shown in Figure 3. Bladder incontinence persisted in five cases, pressure sore occurred in two cases and impotence was complained postoperatively by one case.
Figure 3.
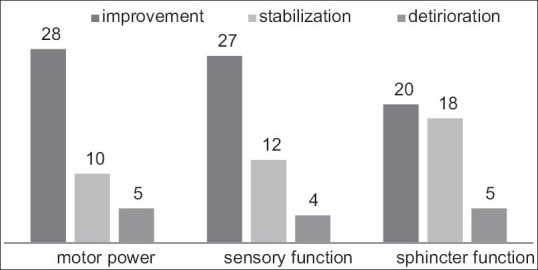
Effect of surgery on neurological status
The mean follow-up period was 22 months (range: 3-96 months). By the last follow-up only 8 patients (18.6%) had tumor recurrence proven in MRI.
Results
Functional outcome
It was one of the most important facets of the study. Postoperatively patients improved by an average of one MRC grade. Fifteen of 17 patients in Grade III and 10 out of 12 patients in Grade IV improved and had near-normal functional muscle power [Table 2]. Only three patients out of nine (33%) with Grade I or Grade II showed improvement in functional muscle power. Bowel and bladder continence improved or was stabilized in 38 cases (88.4%). Similarly, protective sensation was restored in eight cases and maintained in 31 patients. The ability to walk with/without support and carryout activities of personal hygiene and daily living was improved in 19 out of 30 patients with impairment (63.3%). Preoperaive McCormick classification showed 13 cases (30.2%) in Grade I or II, which improved to 32 cases (74.4%) postoperatively [Figure 4].
Table 2.
Pre and postoperative McCormick functional grade
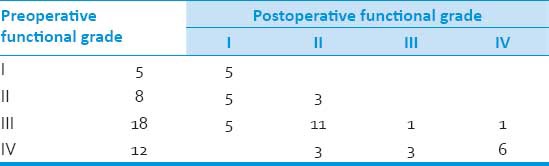
Figure 4.
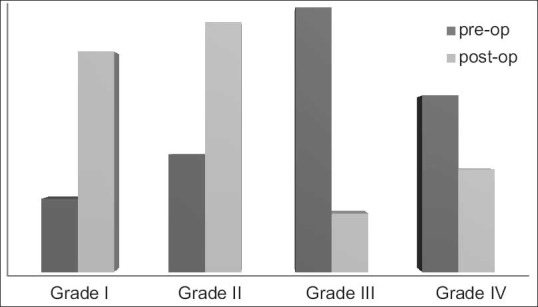
McCormick functional grade
Survival and recurrence
No mortality was recorded during the entire period of study. More important was maintenance of the improvement in the status of the patient during the follow-up. We measured the survival outcomes in terms of event free survival, that is, the absence of deterioration of functional results, absence of new sign and symptom or radiological evidence of tumor recurrence. Thirty-five patients (81.4%) had an event free survival till their last follow-up visit. Of the eight patients with recurrence three had clinical deterioration rest were diagnosed on radiology during follow-up visits. The average duration between surgery and detection of recurrence in this study was 34.4 months (range: 9-84 months).
Of the eight cases with recurrence three had undergone gross total excision, the remaining five had undergone near total excision followed by radiotherapy. Thus, the percentage of patients who had a recurrence following gross total excision (GTE) was 10% as compared to 38.5% (5 out of 13) in cases with near total excision (NTE) plus radiotherapy. Thus, GTE was significantly better than NTE plus radiotherapy for management of IMSCTs (P = 0.0415). With respect to tumor type anaplastic astrocytoma had the most recurrences (n = 3) but was not statistically significant (P = 0.68)
Discussion
Spinal tumors have always been a challenge for the treating surgeon. The rarity of IMSCTs notwithstanding,[2,6] they have always posed a question regarding their optimum management. Most authors have reported a delayed presentation and diagnosis of IMSCTs because they have no specific symptoms, and the patient is often treated symptomatically initially and the full radiological and clinical examination is frequently not performed.[2,7] the most common symptom in this study, as well as others in literature, is low back ache. Radiating low-back ache is not characteristic of intramedullary tumors and is more associated with extramedullary pathologies such as, disc disease, spondylitis, etc., However, it is seen in a number of cases of intramedullary tumors and hence the need for an exhaustive clinical examination and radiological work-up in cases of radicular back pain. MRI is the preferred method of diagnosis[1,3] and we found it quite useful not just for diagnosis, but also for preoperative planning and early detection of recurrent lesions.
Any procedure or surgical management in neurosurgical oncology is judged by the improvement in functional status after surgery, the overall improvement in survival and the incidence of recurrence. With these parameters in mind, the results of the study were deciphered. Surgery on spinal cord tumors is fraught with the risk of postoperative morbidity, and the surgeon is always in a dilemma between aggressive radical resection and preserving functional neural mass. Conservative surgical excision coupled with radiotherapy was once promulgated as a viable alternative to radical surgery and consequent neurological morbidity.[10,11] Nowadays, the standard protocol is for gross total excision as it has been proven by many authors to be superior, in this study also, it was significantly better (P = 0.0415) in terms of rate of recurrence. The developments in neurosurgical techniques, particularly micro dissection and use of somatosensory evoked potential and motor evoked potential intraoperatively have vastly reduced the incidence of iatrogenic damage.[12,13] We routinely used the operating microscope. The experience of the surgeon is an important factor in reducing intraoperative damage and in experienced hands the surgical morbidity is minimal.
The role of radiotherapy as adjuvant is also under debate. Most centers continue to advice adjuvant radiotherapy in cases of IMSCT, and there have been reports in the past suggesting its role in improving long-term outcome.[5] Latest studies however lay emphasis on gross tumor excision and relegate the role of adjuvant radiotherapy in inoperable tumors, high-grade/malignant tumors and inadequately resected tumors.[2,7,14] In this study too we found that radiotherapy didn’t affect the rate of recurrence postresection, and the eventual outcome was inferior to those with GTE. However, we do support the use of adjuvant radiotherapy in high-grade astrocytomas and ependymomas.
The recurrence rate in this study was 18.6% at the last follow-up, this is in agreement with the data published in the literature with recurrence rates ranging from 10% to 22%.[6,10,13] The association of tumor type with recurrence is not that consistent. Most intramedullary tumors of spinal cord are either benign or low-grade and hence the rate of recurrence is more dependent upon the extent of surgical resection as micro-residual tumors (which are frequently left even after GTE) probably didn’t recur frequently. On the other hand high grade astrocytomas and malignant tumors are associated with an increased risk of recurrence.[6,15] In this study too high-grade astrocytomas had the highest number of recurrence (3 out of 8, 37.5%) though not statistically significant and were associated with an inferior eventual outcome.
There has been consistency in the literature regarding the importance of preoperative neurological status and its bearing on the eventual functional outcome.[6,7,13] In this study, too patients with Grade III and IV muscle power showed significant improvement and far exceeded the improvement in patients with lower MRC grading. This could be because a good preoperative status collaborates with less infiltration of tumor mass into neural tracts and recent tumor effect which can be reversed with surgery. Furthermore, the fact that even a single-grade improvement in muscle power for Grade III results in significant functional improvement is instrumental in the improved outcome in these patients. This again emphasizes the role of early diagnosis and timely, aggressive surgical management in IMSCTs. A pertinent point in this regard is that our being tertiary center patients presented to us late which led to a deterioration in their neurological status, thus the importance of an effective referral system.
Conclusions
Intramedullary spinal cord tumors are rare neuroaxial neoplasms but require aggressive diagnostic and surgical management duly to ensure the best outcome. Even malignant lesions such as anaplastic astrocytomas and high-grade ependymomas occupy this location. The most important predictor of functional outcome is preoperative neurological status and hence referral system and other efforts must be made to ensure early diagnosis and prompt surgical management. Most IMSCTs are histologically of low-grade. Tumor type seemingly has no effect on functional outcome; however high-grade tumors are associated with a higher rate of recurrence. Gross total excision of the tumor offers the best chance for an improved event free survival and is definitely superior to sub-total excision and adjuvant radiotherapy. The role of radiotherapy is limited to high-grade tumors and in cases where radical excision is not achieved or in inoperable cases. Meticulous clinical and radiological follow-up is needed to ensure early detection and timely treatment of recurrence ensures prolonged survival and reduces morbidity in patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kane PJ, el-Mahdy W, Singh A, Powell MP, Crockard HA. Spinal intradural tumours: Part II - Intramedullary. Br J Neurosurg. 1999;13:558–63. doi: 10.1080/02688699943051. [DOI] [PubMed] [Google Scholar]
- 2.Malhotra N, BHowmick D, Whitfield P. Intramedullary spinal cord tumours: Diagnosis, treatment, and outcomes. Adv Clin Neurosci Rehabil. 2010;10:21–5. [Google Scholar]
- 3.Jallo GI, Freed D, Epstein F. Intramedullary spinal cord tumors in children. Childs Nerv Syst. 2003;19:641–9. doi: 10.1007/s00381-003-0820-3. [DOI] [PubMed] [Google Scholar]
- 4.Chun HC, Schmidt-Ullrich RK, Wolfson A, Tercilla OF, Sagerman RH, King GA. External beam radiotherapy for primary spinal cord tumors. J Neurooncol. 1990;9:211–7. doi: 10.1007/BF02341151. [DOI] [PubMed] [Google Scholar]
- 5.Linstadt DE, Wara WM, Leibel SA, Gutin PH, Wilson CB, Sheline GE. Postoperative radiotherapy of primary spinal cord tumors. Int J Radiat Oncol Biol Phys. 1989;16:1397–403. doi: 10.1016/0360-3016(89)90940-1. [DOI] [PubMed] [Google Scholar]
- 6.Constantini S, Miller DC, Allen JC, Rorke LB, Freed D, Epstein FJ. Radical excision of intramedullary spinal cord tumors: Surgical morbidity and long-term follow-up evaluation in 164 children and young adults. J Neurosurg. 2000;93:183–93. doi: 10.3171/spi.2000.93.2.0183. [DOI] [PubMed] [Google Scholar]
- 7.Sandalcioglu IE, Gasser T, Asgari S, Lazorisak A, Engelhorn T, Egelhof T, et al. Functional outcome after surgical treatment of intramedullary spinal cord tumors: Experience with 78 patients. Spinal Cord. 2005;43:34–41. doi: 10.1038/sj.sc.3101668. [DOI] [PubMed] [Google Scholar]
- 8.Hoshimaru M, Koyama T, Hashimoto N, Kikuchi H. Results of microsurgical treatment for intramedullary spinal cord ependymomas: Analysis of 36 cases. Neurosurgery. 1999;44:264–9. doi: 10.1097/00006123-199902000-00012. [DOI] [PubMed] [Google Scholar]
- 9.McCormick PC, Stein BM. Intramedullary tumors in adults. In: Stein BM, McCormick PC, editors. Neurosurgery Clinics in North America: Intradural Spinal Surgery. Vol. 1. Philadelphia: WB Saunders Co; 1990. pp. 609–30. [PubMed] [Google Scholar]
- 10.Houten JK, Cooper PR. Spinal cord astrocytomas: Presentation, management and outcome. J Neurooncol. 2000;47:219–24. doi: 10.1023/a:1006466422143. [DOI] [PubMed] [Google Scholar]
- 11.Wood EH, Berne AS, Taveras JM. The value of radiation therapy in the management of intrinsic tumors of the spinal cord. Radiology. 1954;63:11–24. doi: 10.1148/63.1.11. [DOI] [PubMed] [Google Scholar]
- 12.Wiedemayer H, Fauser B, Sandalcioglu IE, Schäfer H, Stolke D. The impact of neurophysiological intraoperative monitoring on surgical decisions: A critical analysis of 423 cases. J Neurosurg. 2002;96:255–62. doi: 10.3171/jns.2002.96.2.0255. [DOI] [PubMed] [Google Scholar]
- 13.Garcés-Ambrossi GL, McGirt MJ, Mehta VA, Sciubba DM, Witham TF, Bydon A, et al. Factors associated with progression-free survival and long-term neurological outcome after resection of intramedullary spinal cord tumors: Analysis of 101 consecutive cases. J Neurosurg Spine. 2009;11:591–9. doi: 10.3171/2009.4.SPINE08159. [DOI] [PubMed] [Google Scholar]
- 14.Jallo GI, Danish S, Velasquez L, Epstein F. Intramedullary low-grade astrocytomas: Long-term outcome following radical surgery. J Neurooncol. 2001;53:61–6. doi: 10.1023/a:1011886516506. [DOI] [PubMed] [Google Scholar]
- 15.Cohen AR, Wisoff JH, Allen JC, Epstein F. Malignant astrocytomas of the spinal cord. J Neurosurg. 1989;70:50–4. doi: 10.3171/jns.1989.70.1.0050. [DOI] [PubMed] [Google Scholar]


