Abstract
Arnold-Chiari malformations (ACM) of the brain result from aberrations in the development of the posterior fossa resulting in its smaller volume leading to tonsillar herniation. The most common type includes Type I ACM where tonsillar descent reaches up to either C1 or C2 along with cervico-dorsal syringomyelia. The surgery (foramen magnum decompression, [FMD]) is usually straight forward and includes sub-occipital craniectomy and cervical laminectomy based on the level of descent. Rarely inadequate cervical laminectomy of C1 arch may result in residual compression at the level of obex even after “lax” duraplasty. A cervico-dural angle (angle between the neo-dura and cervical dura) at level foramen magnum can be observed in these patients. This angle is usually obtuse in imaging of cranio-vertebral junction (CVJ) of normal people and in postoperative patients of Chiari malformations where normal anatomy is restored. Inadequate C1 laminectomy may result in an acute cervico-dural angle with residual compression at the level of CVJ. Therefore, C1 laminectomy becomes a key step in FMD surgery that is often underemphasized, and neurosurgeons should be careful in doing it adequately.
Keywords: Chiari malformations, duraplasty, failed foramen magnum decompression
Introduction
Chiari malformations characterize the descent of tonsils at least >5 mm below the level of foramen magnum. This results from occipital hypoplasia resulting in small posterior fossa volume (PFV) and hence crowding of rhombencephalic structures leading to tonsillar ectopia. Foramen magnum decompression (FMD) results in an increase in the PFV and restores the cerebro-spinal fluid (CSF) flow dynamics at the cranio-vertebral junction. However, inadequate C1 laminectomy may result in persistent tonsillar impaction even though sufficient CSF flow in the cisterna magna could be visualized in the postoperative imaging.
Case Report
A 22-year-old male presented to us with chief complaints of paraesthesiae in the right half of the body since 2 years. On examination, there were no deficits apart from 80% reduction in the sensations on the right half of the body to pin prick and temperature. The posterior column functions were intact. The reflexes were exaggerated and plantars are down going. He had similar complaints 2 years back for which he was investigated thoroughly. Magnetic resonance imaging (MRI) of the brain showed Type I Chiari malformation with extensive cervico-dorsal syrinx [Figure 1]. He had undergone FMD then, but his symptoms were not relieved. Recent MRI showed lax duraplasty with adequate retro-cerebellar CSF signal [Figure 2]. However, the tonsils were still impacted at the FM due to persistent C1 arch. Re-exploration was done and intra-operatively, the C1 arch was found to be only partially removed causing significant compression at the cranio-spinal junction [Figure 3]. The arch was removed up to 3 cm and re-duraplasty was performed after sub-pial resection of tonsils. Adequate CSF flow was seen through the obex. The postoperative course was uneventful, and the patient was discharged later. He is clinically stable in the follow-up and follow-up MRI after 6 months is showing resolving syrinx and re-establishment of an obtuse cervico-dural angle
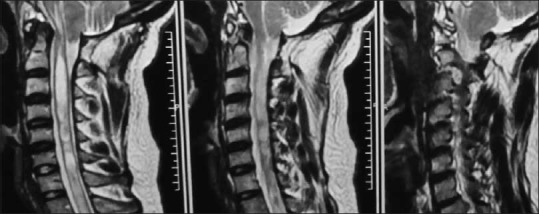
Figure 1.

Initial magnetic resonance imaging showing crowded posterior fossa with tonsillar descent and cervico-dorsal syrinx prior to first surgery
Figure 2.
Postoperative magnetic resonance imaging after 2 years showing residual tonsillar descent with persistent syrinx. However the retrocerebellar cerebro spinal fluid signal seems to be adequate
Figure 3.
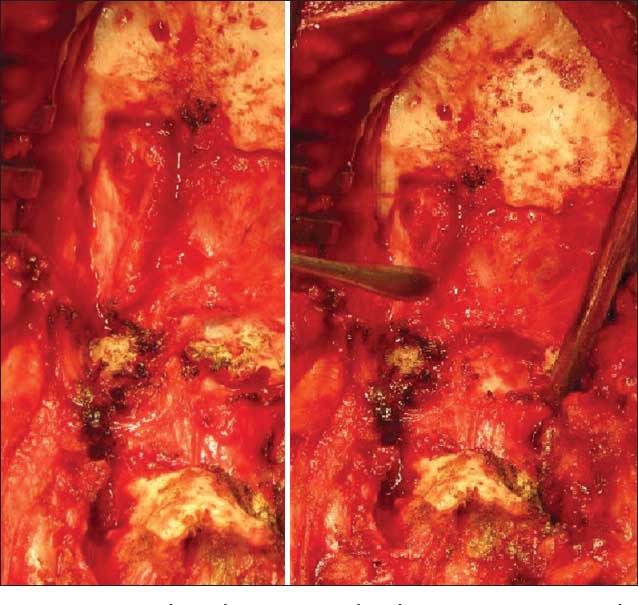
Intra-operative picture showing inadequate C1 laminectomy and imprinted dura due to bony compression after its removal
Discussion
The standard surgery for Type 1 Chiari malformation is FMD with Cervical Laminectomy (CL) with or without autologous duraplasty with or without arachnoid sparing. There is sparse evidence on the extent of bony decompression in FMD as far as cervical laminectomies are concerned. Furtado et al. have described successful outcome in 20 patients over a period of 9 years where they did a C1 laminectomy and a condyle to condyle FMD in all patients.[1] C2 laminectomy was done if the tonsillar ectopia reached up to C2. Hoffman and Souweidane have shown 91.8% clinical improvement in a series of 40 patients where they did the laminectomy according to the tonsillar descent.[2] Aghakhani et al. did C1 laminectomy in all cases of FMD in their series of 157 patients showing almost 90% clinico-radiological improvements.[3] Our patient did not improve after surgery due to incomplete removal of C1 arch forming a constriction in an otherwise lax dura with adequate CSF intensity in the cisterna magna. This resulted in an ACUTE cervico-dural angle that is, the angle formed by the neo-dura after duraplasty and the cervical dura [Figure 4]. Retrospectively, we reviewed the postoperative MRI images from our database and observed that this angle is rather OBTUSE in normal persons and in cases where a liberal “lax” duraplasty has been done after an adequate bony decompression (sub-occipital craniectomy of 3 cm × 3 cm and C1/C2 laminectomy) [Figure 5]. This cervico-dural angle may get altered by variety of factors such as residual bony spurs, bony-regrowth at C1 and incising only outer layer of dura.[4] Rarely, authors further advocate against opening of dura in these surgeries and suggest bony decompression only.[5] There may be higher chances of compression by the fibrous bands at the level of foramen magnum in all such cases, and the cervico-dural angle may remain acute on post-operative images. Similarly, inadequate extension of the vertical limb of the Y shaped durotomy on to the cervical part of dura in spite of adequate bony removal and duraplasty may result in an acute angulation of this angle and may lead to nonresolution of the syrinx.
Figure 4.
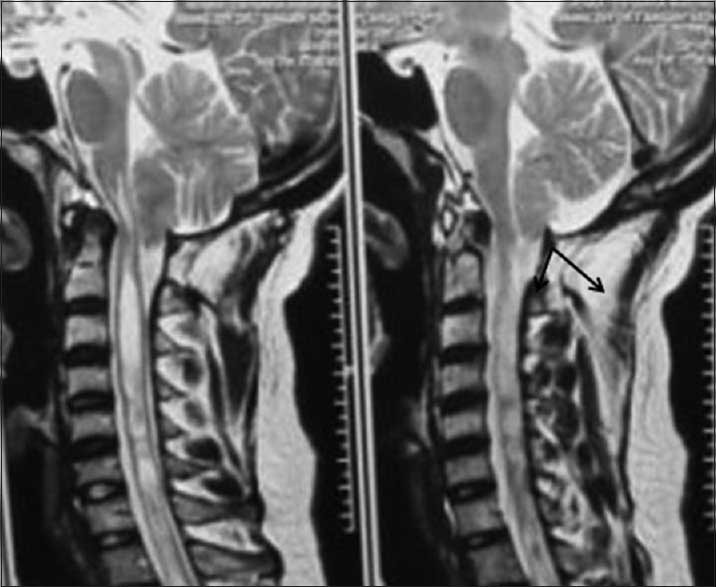
Acute cervicodural angle shown on the postoperative magnetic resonance imaging in the same patient (arrows)
Figure 5.
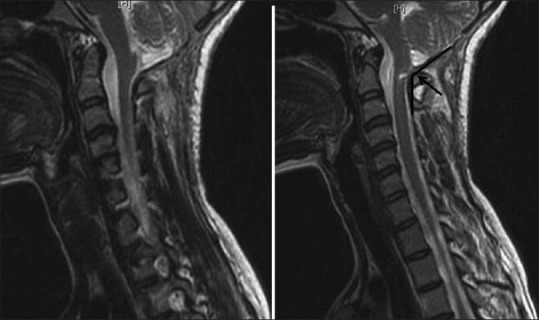
Obtuse cervico-dural angle seen in a different patient after adequate surgery (arrow)
We also came across numerous case reports in the literature regarding increase in the posterior fossa volume following FMD and subsequent favourable clinico-radiological outcome.[6] However, strangely the posterior fossa morphometry never accounted for or included the C1 arch as the lowest level while calculating the volume. Hence, as C1 laminectomy significantly contributes to the increased PFV, more anatomical studies with a larger number of patients should be performed in order to correctly estimate the posterior fossa morphometry.
Conclusions
C1 laminectomy has never gained importance in literature as far as FMD surgery is concerned. Incomplete bony removal doesn’t help the outcome and may not relieve the symptoms. Therefore, surgeons should make sure that the C1 arch is removed completely (3 cm wide), and they are not focussing just on the foramen magnum per se.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Furtado SV, Thakar S, Hegde AS. Correlation of functional outcome and natural history with clinicoradiological factors in surgically managed pediatric Chiari I malformation. Neurosurgery. 2011;68:319–27. doi: 10.1227/NEU.0b013e31820206e5. [DOI] [PubMed] [Google Scholar]
- 2.Hoffman CE, Souweidane MM. Cerebrospinal fluid-related complications with autologous duraplasty and arachnoid sparing in type I Chiari malformation. Neurosurgery. 2008;62(3 Suppl 1):156–60. doi: 10.1227/01.neu.0000317387.76185.ac. [DOI] [PubMed] [Google Scholar]
- 3.Aghakhani N, Parker F, David P, Morar S, Lacroix C, Benoudiba F, et al. Long-term follow-up of Chiari-related syringomyelia in adults: Analysis of 157 surgically treated cases. Neurosurgery. 2009;64:308–15. doi: 10.1227/01.NEU.0000336768.95044.80. [DOI] [PubMed] [Google Scholar]
- 4.Yoshifuji K, Imaizumi T, Iihoshi S, Miyata K, Toyama K. Chiari malformation (type 1) with regeneration of removed C1 lamina after foramen magnum decompression: A case report. No Shinkei Geka. 2005;33:257–60. [PubMed] [Google Scholar]
- 5.Isu T, Tanaka T, Nakamura T, Yamauchi T, Kobayashi N. A case of a young infant with Chiari II malformation treated by only bony foramen magnum decompression. No Shinkei Geka. 1995;23:435–7. [PubMed] [Google Scholar]
- 6.Attenello FJ, McGirt MJ, Gathinji M, Datoo G, Atiba A, Weingart J, et al. Outcome of Chiari-associated syringomyelia after hindbrain decompression in children: Analysis of 49 consecutive cases. Neurosurgery. 2008;62:1307–13. doi: 10.1227/01.neu.0000333302.72307.3b. [DOI] [PubMed] [Google Scholar]


