Abstract
We report two cases with giant intramedullary epidermoid cysts in the thoracolumbosacral and lumbosacral regions with varied presentations. Magnetic resonance (MR) imaging of the thoraco lumbar spine in case 1revealed an intramedullary elongated mass extending from T10 to S2 level causing significant widening of the spinal canal while MR imaging of lumbosacral spine in case 2 showed straightening of the lumbar spine and spina bifida at L5 level with conus at L3 and a lobulated long segment intramedullary solid cystic lesion extending from L2 to S2 veterbrae. The lesion was surgically resected and the pathology revealed an epidermoid cyst. Epidermoid cysts of the spinal cord are rare tumours in the adult population which may be congenital or acquired. Symptoms arising from epidermoid cysts vary with the level of involvement. The treatment of epidermoid cysts is surgical and if possible, complete removal is the goal.
Keywords: Epidermoid cyst, intramedullary lesion, pearly tumour
Introduction
Spinal epidermoid tumors are rare, ≤1% of all spinal tumors. Most of them are intradural and extramedullary and are frequently present in association with spinal dysraphism or as a consequence of repeated lumbar punctures. True intramedullary epidermoid cysts are very uncommon, with ≤60 cases published till 2009.[1] Whether congenital or iatrogenically caused, they form as the result of epidermal cells implanted within the spinal channel. Such implantation can occur during a variety of procedures and events such as bullet wounds, surgery, myelography or punctures for diagnosis, anesthesia or treatment.[2] Intramedullary dermoid cyst is common in the lumbosacral and thoracic regions; two frequent localizations are T4-T6 and T11-T12, while only three cases have been reported with cervical cord involvement.[3] We report two cases of intramedullary epidermoid cyst with different presentations.
Case Report
Case 1
A 23-year-old female patient presented with 2 months history of post-partum progressive bilateral lower extremity numbness and weakness, spasticity and fecal incontinence. At the time of presentation, she was ambulatory with only maximal assistance. She denied any back or leg pain. She had no history of back injury and had never undergone lumbar puncture. Her past medical history was insignificant.
Physical examination on admission revealed no cutaneous lesions on her back. Motor examination revealed a Grade I power in all group of lower limb muscles. No fasciculation's or muscle atrophy was noted. Diminution to light touch and pinprick was noted in both the lower extremities. Deep tendon reflexes were hyperactive in the lower limbs without any clonus. Perianal sensations were absent with absent bulbocavernous reflex. Babinski's sign was present bilaterally.
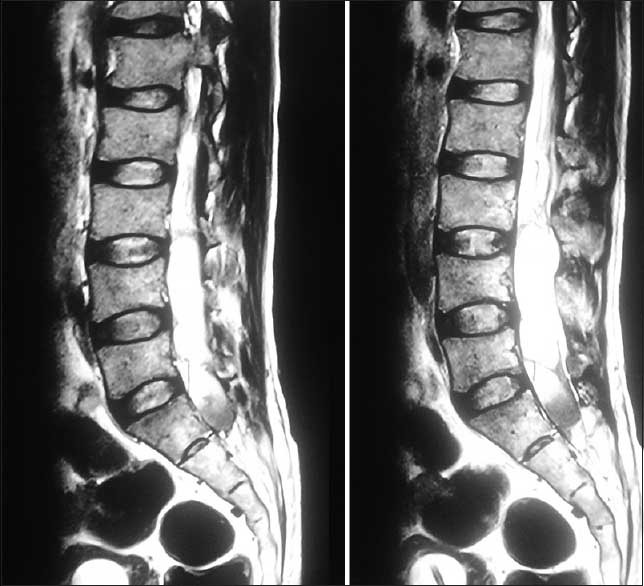
Magnetic resonance imaging (MRI) of the thoraco lumbar spine revealed an intramedullary elongated mass extending from T10 to S2 level causing significant widening of the spinal canal. This mass shows hyperintense signal on T1 and T2 images. There is a marked scalloping of the lumbar vertebral bodies posteriorly. The study did not demonstrate spinal dysraphism. Complete neural axis imaging demonstrated no other lesions [Figure 1].
Figure 1.
Preoperative sagittal T2-weighted magnetic resonance imaging MRI showing an intramedullary elongated mass extending from T10 to S2 level causing significant widening of the spinal canal
Case 2
A 35-year-old male patient presented with 6 months history of urinary incontinence. The patient had no complaints of weakness in the lower limbs.
Physical examination on admission revealed no cutaneous lesions on his back. No fasciculation's or muscle atrophy was noted. Patient had no motor or sensory deficit. Deep tendon reflexes and perianal sensations were normal [Figure 2].
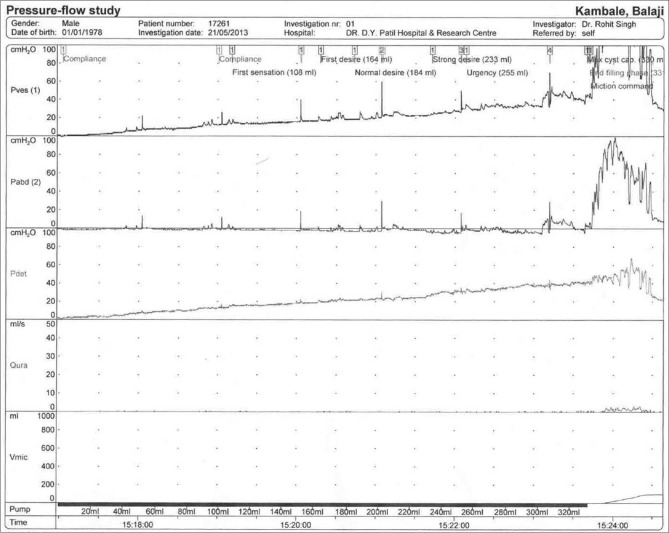
Figure 2.
Urodynamic studies of case 2 suggestive of acontractile detrusor with poor bladder compliance. Bladder capacity and sensation are normal
The first diagnostic evaluation had included renal ultrasonography and voiding cystoureterography that were normal. Urodynamic studies were also done which were suggestive of acontractile detrusor with poor bladder compliance. Bladder capacity and sensation were normal.
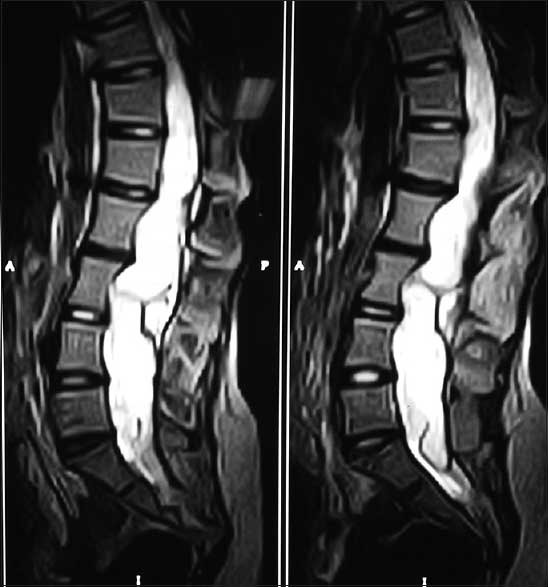
Magnetic resonance imaging of the lumbosacral spine showed straightening of the lumbar spine and spina bifida at L5 level. It also showed a conus at L3 with lobulated long segment intramedullary solid cystic lesion extending from L2 to S2 veterbrae and causing significant widening of the spinal canal. The upper one-third of the lesion is hyperintense on T1- and T2-weighted images and shows loss of signal in fat suppressed images suggestive of fatty component. Middle one-third and lower third are predominantly cystic which appear hyperintense on T2-weighted and hypointense on T1-weighted with foci of calcification in the lower one-third of the lesion [Figure 3].
Figure 3.
Preoperative sagittal T2-weighted magnetic resonance imaging MRI showing conus at L3 with lobulated long segment intramedullary solid cystic lesion extending from L2 to S2 veterbrae and causing significant widening of the spinal canal
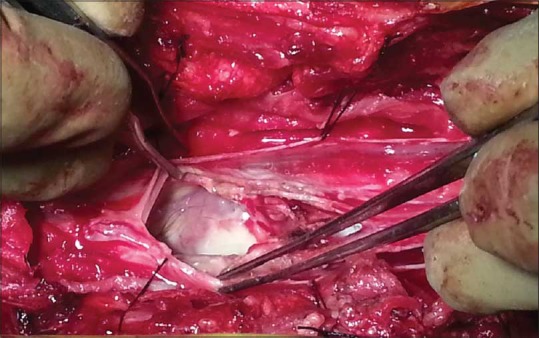
Operation
The patient underwent T10-S1 laminectomies in case 1 and L2-S2 laminectomies in case 2. After dural opening, the lower tract of the spinal cord and the conus medullaris appeared over distended by an intrinsic lesion. By performing a limited dorsal slit, the whitish tumor capsule was immediately reached. The capsule was dissected free from neural tissue and then opened to allow removal of the soft, pearly content. Thereafter, a progressive careful dissection of the cyst wall was accomplished until its complete removal [Figures 4 and 5].
Figure 4.

Intraoperative image of case 1 showing intramedullary dermoid cyst
Figure 5.
Intraoperative image of case 2 showing intramedullary cystic material
Post-operative histology demonstrated that the cyst wall contained an abundant keratin with foci of calcification and cholesterol clefts, consistent with an epidermoid cyst [Figure 6].
Figure 6.
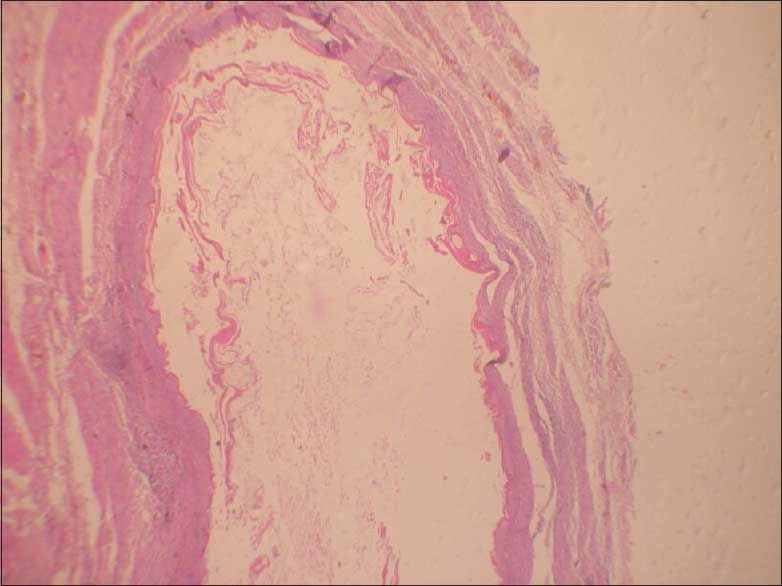
Histopathological image of a dermoid cyst
Immediate postoperative event was uneventful without any deterioration of neurological symptoms in both the patients.
Post-operative follow-up after 3 months in case 1, patients weakness, and fecal incontinence improved whereas in case 2 there was no improvement in the urinary incontinence of the patient.
Discussion
Epidermoid tumors were first described by Cruveilhier in 1835, who called them “tumor perlees” (pearly tumors).[4] The first description of an intramedullary epidermoid cyst belongs to Hans Chiari in 1883. Between 1883 and 1992 there were only 47 reported of pure intramedullary epidermoid cysts.[5]
Epidermoid cysts of the spinal cord are rare tumors in the adult population. Intraspinal epidermoid cysts may be congenital or acquired. Congenital spinal epidermoids are related to inclusion of the ectoderm at the time of inclusion of the ectoderm at the time of closure of the neural tube between 3rd and 4th weeks of fetal life.[6] This accounts for the midline location of most cysts, and their possible association with defects of the overlying bone and skin.[7] The congenital epidermoid cysts are more frequently associated with other congenital abnormalities, such as dermal sinus, spina bifida and hemivertebrae.[3] Acquired epidermoid cysts are thought to result from iatrogenic penetration of skin fragments, especially after single or multiple lumbar punctures or after meningomyelocele repairs.[8]
Symptoms arising from epidermoid cysts vary with the level of involvement but do not differ from other space occupying lesions in the spinal column. Signs and symptoms at presentation are usually neurological such as progressive paraparesis, sensory loss, urological manifestations and back/leg pain. The slow growth of epidermoid cysts often leads to a delay in their diagnosis: Duration of symptoms before diagnostic recognition may extend for many years. Due to this the symptoms may often arise in early or middle-adult life.[9]
The peculiarity of the history of case 2 is that the patient presented only with urological symptoms as initial manifestations, consisting mainly as incontinence leading to diagnostic delay. The absence of neurological deficit is remarkable in this case.
Radiographic characteristics of epidermoids typically how a displacement of nerve roots and the spinal cord in the subdural space.[10] T1- and T2- weighted signal on MRI usually varies from hypo to isointense, but may occasionally have increased intensity on T2- weighted images.[11,12] This variation in signal characteristics makes the preoperative diagnosis in the spinal lesions difficult.
Diagnosis of epidermoid, as well as dermoid cysts, is usually based on inspection due to typical aspect of their content. Histologically, epidermoid and dermoid cysts are lined by stratified squamous epithelium supported by an outer layer of collagenous tissue, progressive desquamation of keratin from epithelial lining toward the interior of the cyst produces a soft white material. Differentiation between the two forms is based on the presence of skin adnexa present only in a dermoid cyst.[3]
The treatment of epidermoid cysts is surgical, and if possible, complete removal is the goal. Sometimes the capsule is tightly adherent to the surrounding cord tissue, in which case an attempt to perform complete removal may result in neurological deficit and should be avoided. Following resection, preoperative symptoms may resolve completely, even after partial resection of the cyst. Recurrence is rare after a complete removal of the tumor, and the rate of recurrence seems to be inversely proportional to the magnitude of the resection.[1]
The prognosis for epidermoid tumors of the spine is good, since they have histologically benign nature. Because long-standing neurological deficits may become irreversible, patients with neurological findings should undergo surgery when the diagnosis is made.[6]
Epidermoid cysts are rare tumors without specific clinical presentations. Because of these atypical presentations and delay in the onset of symptoms, patients presenting with neurological deficits or patients presenting with clinical and urodynamic features suggestive of neuropathic bladder with urological symptoms, a detailed neurological examination followed by MRI of the spinal cord should be done at the earliest to decrease the time to diagnosis. This will help in immediate surgical intervention and will improve prognosis of the patient.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gonzalvo A, Hall N, McMahon JH, Fabinyi GC. Intramedullary spinal epidermoid cyst of the upper thoracic region. J Clin Neurosci. 2009;16:142–4. doi: 10.1016/j.jocn.2008.04.017. [DOI] [PubMed] [Google Scholar]
- 2.Gardner DJ, O’Gorman AM, Blundell JE. Intraspinal epidermoid tumour: Late complication of lumbar puncture. CMAJ. 1989;141:223–5. [PMC free article] [PubMed] [Google Scholar]
- 3.Ferrara P, Costa S, Rigante D, Mule A, D’Aleo C, Pulitanò S, et al. Intramedullary epidermoid cyst presenting with abnormal urologic manifestations. Spinal Cord. 2003;4:645–8. doi: 10.1038/sj.sc.3101482. [DOI] [PubMed] [Google Scholar]
- 4.Chandra PS, Manjari T, Devi BI, Chandramouli BA, Srikanth SG, Shankar SK. Intramedullary spinal epidermiod cyst. Neurol India. 2000;48:75–7. [PubMed] [Google Scholar]
- 5.Roux A, Mercier C, Larbrisseau A, Dube LJ, Dupuis C, Del Carpio R. Intramedullary epidermoid cysts of the spinal cord. Case report. J Neurosurg. 1992;76:528–33. doi: 10.3171/jns.1992.76.3.0528. [DOI] [PubMed] [Google Scholar]
- 6.Ozaras N, Sariyildiz M, Demir S, Guzey F, Aycan A, Esenyel M. A neglected case admitted with paraplegia: An intradural extramedullary epidermoid cyst. J ClinExp Invest. 2012;3:270. [Google Scholar]
- 7.Teksam M, Casey SO, Michel E, Benson M, Truwit CL. Intraspinal epidermoid cyst: Diffusion-weighted MRI. Neuroradiology. 2001;43:572–4. doi: 10.1007/s002340000526. [DOI] [PubMed] [Google Scholar]
- 8.Cataltepe O, Berker M, Akalan N. A giant intramedullary spinal epidermoid cyst of the cervicothoracic region. Pediatr Neurosurg. 2004;40:1220–3. doi: 10.1159/000079853. [DOI] [PubMed] [Google Scholar]
- 9.Scarrow AM, Levy EI, Gerszten PC, Kulich SM, Chu CT, Welch WC. Epidermoid cyst of the thoracic spine: Case history. Clin Neurol Neurosurg. 2001;103:220–2. doi: 10.1016/s0303-8467(01)00156-1. [DOI] [PubMed] [Google Scholar]
- 10.Tabaddor K, Lamorgese JR. Lumbar epidermoid cyst following single spinal puncture. Case report. J Bone Joint Surg Am. 1975;57:1168–9. [PubMed] [Google Scholar]
- 11.Gupta S, Gupta RK, Gujral RB, Mittal P, Kuriyal M, Krishnani N. Signal intensity patterns in intraspinal dermoids and epidermoids on MR imaging. Clin Radiol. 1993;48:405–13. doi: 10.1016/s0009-9260(05)81110-9. [DOI] [PubMed] [Google Scholar]
- 12.Visciani A, Savoiardo M, Balestrini MR, Solero CL. Iatrogenic intraspinal epidermoid tumor: Myelo-CT and MRI diagnosis. Neuroradiology. 1989;31:273–5. doi: 10.1007/BF00344358. [DOI] [PubMed] [Google Scholar]