Abstract
Acute inflammatory responses are protective, yet without timely resolution can lead to chronic inflammation and organ fibrosis. A systems approach to investigate self-limited (self-resolving) inflammatory exudates in mice and structural elucidation uncovered novel resolution phase mediators in vivo that stimulate endogenous resolution mechanisms in inflammation. Resolving inflammatory exudates and human leukocytes utilize DHA and other n-3 EFA to produce three structurally distinct families of potent di- and trihydroxy-containing products, with several stereospecific potent mediators in each family. Given their potent and stereoselective picogram actions, specific members of these new families of mediators from the DHA metabolome were named D-series resolvins (Resolvin D1 to Resolvin D6), protectins (including protectin D1-neuroprotectin D1), and maresins (MaR1 and MaR2). In this review, we focus on a) biosynthesis of protectins and maresins as anti-inflammatory - pro-resolving mediators; b) their complete stereochemical assignments and actions in vivo in disease models. Each pathway involves the biosynthesis of epoxide-containing intermediates produced from hydroperoxy-containing precursors from human leukocytes and within exudates. Also, aspirin triggers an endogenous DHA metabolome that biosynthesizes potent products in inflammatory exudates and human leukocytes, namely aspirin-triggered Neuroprotectin D1/Protectin D1 [AT-(NPD1/PD1)]. Identification and structural elucidation of these new families of bioactive mediators in resolution has opened the possibility of diverse pathophysiologic actions in several processes including infection, inflammatory pain, tissue regeneration, neuroprotection-neurodegenerative disorders, wound healing, and others.
Keywords: Resolvins, leukocytes, LC-MS-MS-based targeted lipid mediator metabolomics, lipid mediators, eicosanoids
Introduction
Docosahexaenoic acid (DHA) is a highly conserved structure, an essential fatty acid in humans, and has physical properties that evolved to impact cellular membrane and neural function [1-4]. Recent results from this laboratory indicate that DHA is also a precursor to potent local autacoids. These includes the D-series resolvins, protectins and maresins that are produced in self-resolving inflammatory exudates in mice [reviewed in ref. 5]. Neutrophils (PMN) are first to arrive at the site of inflammation during the acute inflammatory response and play an important protective role in innate immunity and host defense. However, excessive accumulation of PMN within tissues can lead to tissue damage, amplification of the inflammatory response, injury from within and prolongation of the signs of inflammation [6]. The control of neutrophil infiltration is of wide interest, as new anti-inflammatory agents are needed to control excess neutrophil responses within tissues that can give rise to chronic inflammatory diseases [7]. Along these lines, evidence was sought for the endogenous mechanism(s) controlling PMN infiltration and natural tissue resolution, since protective PMN (i.e. acute inflammatory responses) are programmed to be self-limited and tightly controlled [8-10]. Lipid mediators such as prostaglandins and leukotrienes play pivotal roles in the initiation of acute inflammation [11], whereas resolvins and protectins promote and stimulate active resolution [8, 9, 12]. In excess, prostaglandins and leukotrienes are generally pro-inflammatory [11] and involved in the classic initiation phase of the acute inflammatory response in humans.
Studies in this laboratory uncovered potent new families of n-3 essential fatty acid (EFA)-derived mediators generated during resolution that are antiinflammatory, neuroprotective, and activate novel resolution pathways [9, 10, 13, 14]. Resolution of acute inflammation is a central component of host defense and the return of tissue to homeostasis [15]. It is now well recognized that inflammation plays a key role in many prevalent human diseases including cardiovascular diseases, atherosclerosis, Alzheimer's disease, and cancer [16-18]. Although much is known about the molecular basis of initiating signals and proinflammatory chemical mediators in inflammation [19], it has only recently become apparent that endogenous stop signals are critical at early checkpoints within the temporal events of inflammation [20-22]. In this context, lipid mediators are of considerable interest. The arachidonic acid-derived prostaglandins and leukotrienes are potent pro-inflammatory mediators [23], whereas the lipoxins, biosynthesized from arachidonic acid, are potent anti-inflammatory and proresolving molecules [for reviews see 24, 25, 26]. During the course of inflammation, arachidonatederived eicosanoids switch from prostaglandins and leukotrienes within inflammatory exudates to lipoxins that in turn stop the recruitment of neutrophils to the site. This switch in eicosanoid profiles and biosynthesis is driven, in part, by cyclooxygenase-derived prostaglandin E2 and prostaglandin D2, which instruct the transcriptional regulation of enzymes involved in lipoxin biosynthesis [22]. Hence, the appearance of lipoxins within inflammatory exudates is concomitant with self-limited, or also described in the literature as spontaneous, resolution of inflammation [22], and these chemical mediators are nonphlogistic stimulators of monocyte recruitment and macrophage phagocytosis of apoptotic PMN [27, 28].
Further studies on the endogenous mechanisms of anti-inflammation using a murine model of self-limited resolution demonstrated, for the first time, that resolution is an active biochemical process that involves the generation of specific new families of mediators [for recent reviews, see refs. 29, 30]. During self-limited resolution, cell-cell interactions and transcellular biosynthesis lead to the production of these new families of potent bioactive lipid mediators from ω-3 essential fatty acid precursors and were termed resolvins (resolution phase interaction products derived from DHA, EPA and n-3 DPA) and protectins (docosatrienes derived from DHA) [9, 10, 13, 31, 32]. These novel di- and trihydroxy-containing products from n-3 essential fatty acids are biosynthesized by previously unrecognized enzymatic pathways that include resolvins, protectins and maresins. Specific members of each family display potent anti-inflammatory, immunoregulatory and pro-resolving actions in vitro and in vivo in murine models of inflammatory diseases [9, 10, 13] (see Figure 1).
Figure 1. Specialized Pro-Resolving Lipid Mediator Families Biosynthesized From Their Parent Polyunsaturated Fatty Acids.
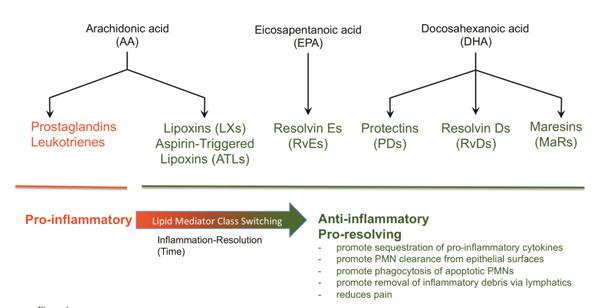
Resolving exudates utilize essential fatty acids such as DHA to form several structurally distinct groups of specialized proresolving mediators that promote clearance and resolution.
The omega-3 polyunsaturated fatty acids were assigned, in 1929, essential roles because their exclusion from the diet gave rise to a new form of deficiency disease [33]. Many more recent reports document the importance of fish oil (omega-3) fatty acids EPA and DHA in human diseases associated with uncontrolled tissue inflammation. In particular, omega-3 DHA and EPA are protective in inflammatory bowel disease and colitis [34], cardiovascular disease [35-38], and Alzheimer's disease [39]. However, the cellular and molecular mechanisms responsible for these now well-documented beneficial actions of omega-3 fatty acids remain an important challenge and public health concern, given the widespread use of n-3 supplements and the many diseases characterized by excessive inflammation. DHA is enriched in neural tissues, where it appears to play functional, not just structural roles [4, 40]. Along these lines, results from earlier studies indicated that DHA was enzymatically converted to products coined docosanoids, whose structures were unknown at the time, that might be linked to retinal protection [41] and potentially neuronal function [42]. The complete structures of those molecules and functions were not established.
Human whole blood, isolated leukocytes, and glial cells each enzymatically convert DHA to 17S-hydroxy-containing docosatrienes (dihydroxy products) and 17Sseries resolvins [9, 13]. The new 10,17S-docosatriene series displayed potent antiinflammatory actions that included reducing or limiting further PMN numbers in exudates in vivo (the cessation process in resolution of inflammation [15]), and down regulating production of proinflammatory lipid mediators and cytokines by glial cells in vitro [13]. During the resolution phase of peritonitis, unesterified DHA levels increase and 10,17S-docosatriene is generated within the resolving exudates, where it appears to promote catabasis (the return from disease, cf. refs. [8, 43]), namely the return to homeostasis, by shortening the resolution interval [9, 43]. This novel DHA-derived 10,17S-docosatriene was next also found to be produced in vivo during strokes in murine tissues, studies in collaboration with Nicolas Bazan and colleagues, and limited the entry of leukocytes into the area of neural damage in the brain, thus reducing the magnitude of tissue injury [44]. Also, in collaboration with Bazan and colleagues, we found that this 10,17S-docosatriene is neuroprotective in retinal pigmented cells and introduced the term neuroprotectin D1 for this potent DHA product [14], a member of the protectin family of mediators [9, 31] that accumulates in the ipsilateral hemisphere of the brain following focal ischemia [45].
NPD1 is formed from DHA in cornea in a lipoxygenase-dependent fashion to protect from thermal injury as well as promote wound healing [46]. Importantly, neuroprotectin D1, resolvin D1, and resolvin D5 are produced by trout brain cells from endogenous DHA, suggesting that the structures of these DHA-derived local mediators are highly conserved from fish to humans [47]. Together, these results underscored the need to establish the complete stereochemistry of endogenous biologically active 10,17S-docosatriene, namely the configuration of the conjugated double-bond system and chirality of the carbon-10 position alcohol in the potent bioactive molecule. In recognition of its wide scope of formation and actions, protectin D1 (PD1) is used to denote the structure of this chemical mediator and the prefix neuro before protectin D1 notes its neural system origins (i.e. retina, brain) and addresses functional role [46-50].
The chemical signals and mediators produced by macrophages are of wide interest, because macrophages play key roles in innate host responses and local inflammation [51, 52], as well as in neovascularization, resolution of inflammation, and wound healing [51, 53, 54]. Along these lines, we also identified a novel family of potent DHA-derived molecules produced by macrophages, denoted the maresins for macrophage mediators in resolving inflammation, that act directly on phagocytes [54, 55]. MaR1, the first mediator identified in this novel family, is defined as possessing potent anti-inflammatory and proresolving actions both in vivo and in vitro [54, 55]. The present review will also discuss the approach employed for establishing the function and complete stereochemistry as well as the biological actions of Protectins, Maresins (Figure 1), some of their natural isomers and biosynthetic intermediates.
Protectin Biosynthesis and Stereochemistry
The DHA-derived 10,17-dihydroxy conjugated triene-containing product, termed PD1, is biosynthesized by several human cell types, murine exudates, skin, and brain tissues [9, 13, 14, 44, 48], as well as isolated fish tissues [47]. PD1 displays potent protective and anti-inflammatory actions [10, 13, 14, 44].
PD1 isolated and identified earlier carries alcohol groups at carbon 10 and 17 positions flanking its conjugated triene portion of this molecule, found to be critical for potent functions of this molecule [9, 13]. The stereochemistry of the carbon 17-position alcohol was retained from the precursor predominantly in the S configuration when derived from the lipoxygenase product 17S-H(p)DHA precursor [9, 13], eliminating isomers from the matching and biosynthetic pathway in Fig. 2 and ref. [50]. The doublebond geometry and stereochemistry of the alcohol group at position 10 were tentatively assigned based on biogenic evidence [9, 48], i.e., the formation of alcohol trapping products in murine brain and human leukocytes as well as identification of two vicinal diols 16,17S-diHDHA. The complete stereochemical assignments and the major biosynthesis route found with isolated human leukocytes (PMN and lymphocytes; refs. [9, 48, 50]) are illustrated in Figure 2.
Figure 2. Protectin Biosynthetic Pathway.
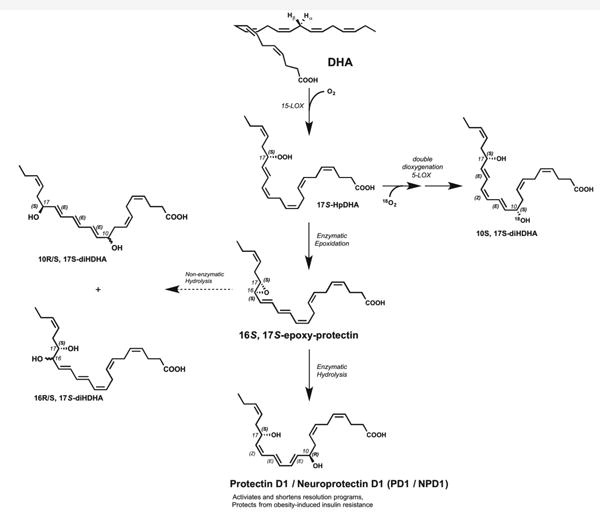
PD1 produced enzymatically from the 16S, 17S epoxy protectin (pictured in a tentative double bond geometry) was confirmed by epoxide trapping experiments. Non-enzymatic hydrolysis of this epoxide intermediate formed two minor products, the all-trans-triene isomer and vicinal 16, 17S diol.
The 10S, 17S double dioxygenation pathway and product occur by sequential actions of two lipoxygenation enzymes as demonstrated in cell incubation and isolated enzymes carried out under an enriched atmosphere of 18O2. See text for further details.
Each of the double bond isomers likely to be biosynthesized were prepared in view of potential biosynthetic routes involved in PD1 formation, namely the involvement of epoxide-containing intermediates and/or double dioxygenation (Fig. 2) intermediates [9, 13, 14, 48]. The R and S configuration of the alcohol group at the carbon 10-position were each prepared by stereocontrolled total organic synthesis. Each of the stereocontrolled steps from defined precursors enabled preparation of geometric isomers of the conjugated triene region that were confirmed by NMR [see ref. 50]. Also, for these experiments we prepared dihydroxydocosanoids using isolated plant lipoxygenase(s) to obtain, as in earlier experiments [56], both positional isomers 7,17S-diHDHA (termed resolvin D5) [57] and 10,17S-diHDHA [9, 13]. The preparation of these using micellar substrate presentations was given in further detail in [56]. These reference compounds prepared by biogenic synthesis with DHA were useful in analyses of biosynthetic routes.
Serhan et al. [50] reported the prominent ions and chromatographic behaviors for each of the double bond and positional isomers prepared by total organic synthesis. Each of the eight isomers gave characteristic UV λmaxMeOH for a conjugated triene chromophore with a λmaxMeOH at ∼270 nm with shoulders at 260 nm and 282 nm (note that these values reflect the ± 1 nm cutoff of the scanning UV spectrophotometer used in refs. [9, 50]. Each of these isomers gave a specific λmaxMeOH, which appeared to reflect the geometry of the double bond system. For example, the Δ15-trans isomer in the conjugated triene portion of 10,17-diHDHA gave a UV λmaxMeOH of 269 nm [50]. Only one of these products matched the chromatographic behavior using both LC-MS and GC-MS including C values (the relative retention time in GC compared to saturated fatty acid standards) and retention times as well as bioactivities. As expected, each of the major prominent ions for these isomers in both LC-MS-MS and GC-MS-MS were identical (i.e., daughter and parent ions were the same for each, with different retention times).
To determine the complete stereochemical assignment of PD1, we directly compared the physical and biologic properties of DHA-derived PD1 and related 10,17 dihydroxy-docosatriene stereoisomers obtained from human and mouse cells to those prepared by total organic and biogenic synthesis [50]. These included the following: 10S17S-dihydroxy-docosa-4Z,7Z,11E,13Z,15E,19Z-hexaenoic acid, also known as PDX; 10R,17S-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic-acid, NPD1/PD1; 10S,17R,-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic-acid; 10R,17Sdihydroxy-docosa-4Z,7Z,11E,13E,15E,19Z-hexaenoic-acid; 10R,17S-dihydroxy-docosa-4Z,7Z,11E,13Z,15E,19Z-hexaenoic-acid; and 10S,17S-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic-acid. The total syntheses of these are reported in refs. [58, 59]. Of interest, 10S,17S-dihydroxy-docosa-4Z,7Z,11E,13Z,15E,19Z-hexaenoic acid and 10S,17S-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic-acid coeluted in this system, as did both compounds 10R,17S-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic-acid and 10S,17R,-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic-acid [see ref. 50]. It is of interest to note that the mass spectral identification of acid alcohol trapping products in human leukocytes suggested that an epoxide-containing intermediate was involved in NPD1/PD1 biosynthesis in human cells [48]. The isolation and identification of alcohol trapping products indicated the involvement of an epoxide intermediate in the conversion of DHA to 10,17S-diHDHA, a docosatriene containing a characteristic conjugated triene structure involving three of the six double bonds present in this compound. The role of a 16(17)epoxide intermediate generated from the 17Shydroperoxy-DHA precursor was further supported by the identification of two vicinal diols, i.e., 16,17S-dihydroxydocosatrienes present in these LC-MS-MS profiles also generated from DHA. The 16(17)epoxy-DHA could open via non-enzymatic hydrolysis to a racemic mixture, i.e., 16R/S,17S-diHDHA, or to a single 16,17S-vicinol alcohol by the actions of an appropriate epoxide hydrolase in a reaction similar to that demonstrated earlier in the biosynthesis of LXA4 [60-62]. Hence, the biosynthesis of PD1 from a 16(17)epoxide intermediate would require an enzymatic reaction to move the double bond configuration to set the triene geometry to 11E,13E,15Z and direct the attack of H2O and insertion of its oxygen into the carbon 10 position of PD1 determined to be in the 10R stereochemical configuration, which also proved critical for potent bioactions.
The chirality of the alcohols and double bond geometry of the triene were systematically addressed in these experiments [see ref. 50]. The MS-MS spectrum of PD1 obtained from murine peritonitis (4 h) biosynthesized in vivo upon challenge with zymosan gave the mass spectrum that was recorded using the same instrument settings and conditions that matched synthetic 10R,17S-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic acid. To obtain additional evidence for matching, GC-MS analyses were also performed. The chromatographic behavior and prominent ions in two separate mass spectrometry systems (LC-MS-MS and GC-MS), together with biological activity [50], permitted criteria for assignment of the physical properties of PD1 and related isomers. Because the parent and daughter ions were the same for each related natural isomer, retention time in two chromatographic systems and bioactivity were key requirements for assigning the stereochemistry of the endogenous NPD1/PD1.
10S,17S-dihydroxy-docosa-4Z,7Z,11E,13Z,15E,19Z-hexaenoic acid, also coined PDX, is consistently identified in profiles obtained from murine peritonitis [50]. It is, however, not the major product of isolated human cells nor does it carry potent actions of NPD1/PD1, also reported earlier [9, 13, 63]. Consistent with its biosynthesis (Fig. 2), the appearance of this double dioxygenation product (namely formed by consecutive sequential actions of two lipoxygenase reactions on the 1,4-cis-penta-dienes) was timedependent both in vivo and in vitro [50]. Stereoselective insertion of oxygen from H2O was expected to give rise to a 10R configuration when attacking the carbonium cation intermediate to form PD1; proposed in refs. [13, 48]. Double bond geometry in the triene portion of the double dioxygenation product, i.e. 10S,17S-diHDHA or PDX [64], was not consistent with the biosynthesis of the triene of PD1 in that the trans, cis, trans configuration is present [48, 50]. Since these and other lipid mediators are highly conserved structures found in many species from fish to human [47], a species difference between mouse and human in PD1 structure is not evident, although the role of these products in lower organisms remains of interest.
The biosynthesis of Resolvin D5 (7,17-diHDHA) in the resolving inflammatory exudates and infectious exudates [9, 10, 57] and its formation from DHA or 17-hydroxy-DHA with isolated human neutrophils suggested that the biosynthesis of this mediator involved sequential lipoxygenation, also known as double dioxygenation [10]. That is, in addition to using molecular oxygen for insertion at the 17-position, lipoxygenation (5-LOX and/or 15-LOX; vide infra) could also insert molecular oxygen at the 7-position in sequential fashion. The identification of this novel from DHA and the sequential lipoxygenation events in its formation [9, 13] appeared to be similar to that of 5S,15SdiHETE generated from arachidonic acid [65, 66]. Hence, it was unexpected in earlier studies [56] when sequential actions of potato 5-lipoxygenase and/or 15-lipoxygenase with the substrates in micellar configuration were discovered to produce both 7,17-diHDHA and 10,17-diHDHA positional isomers as major products as well as multiple geometric isomers as minor products following hydrolysis of enzymatically generated epoxides in vitro [cf. 9, 13]. The formation of these isomers is apparently dependent on substrate, pH, and enzyme concentrations [56].
Oxygen Incorporation in Biosynthesis of Protectins
To study the role of sequential lipoxygenase actions in the proposed mechanism of PD1 formation [9, 50] (Figure 2) and its related positional isomer 10S,17S-diHDHA (also known as 10S,17S-DiHDoHE, PDX; https://www.caymanchem.com), we carried out incubations in an atmosphere enriched in isotope 18O2 with 17-hydroperoxy-DHA as substrate and isolated potato 5-lipoxygenase [50]. Note that PD1 and PDX differ in both chirality at carbon 10 and geometry of their respective triene double-bond configuration (Fig. 2) [64]. Following extraction and isolation, the product profiles, GC-MS and LCMS-MS results indicated that 18O was incorporated [50] in the carbon 10-position in 10S,17S-diHDHA (Fig. 2). Chromatographic separation of 10S,17S-diHDHA gave prominent ions with MS-MS, indicating on average >75% incorporation of 18O originating from molecular oxygen in the carbon 10-position with a range of 51.4 to 91.8% increase in diagnostic ions. Since these enzymes use molecular oxygen as a substrate, it is not possible, under these conditions, to completely replace enzymeassociated 16O for the 18O isotope as calculated earlier for lipoxin A4 in refs. [60, 61]. The extent of 18O present in diagnostic ions was determined for m/z 181/183, 261/263, 289/291, 297/299, 315/317, 323/325, 341/343, and 359/361, and the ratio of 16O to 18O calculated from ion intensities and averaged. These results indicate that 10S,17SdiHDHA can be produced via double lipoxygenation in biological systems and in vitro with isolated enzymes.
Results from matching studies indicated that the double bond geometry for the conjugated triene portion of this molecule was in the trans,cis,trans configuration [50]. Double dioxygenation to form 10S,17S-diHDHA was also a mechanism to generate this compound in vivo, since it is a prominent product in murine exudates from peritonitis, suspensions of human leukocytes incubated with DHA [13] and murine brain [9, 10], as well as trout leukocytes and brain [47]. Figure 2 outlines the proposed scheme and proposed role for double dioxygenation and its product 10S,17S-diHDHA, a member of the protectins that may be an independent pathway marker of cell-cell interactions and DHA consumption in vivo. The double bond geometry in the conjugated triene portion of the molecule (trans,cis,trans) is consistent with oxygenation using molecular oxygen with two sequential lipoxygenation steps [13, 50]. This product is also known as PDX [67]. Given the biological actions, chromatographic and physical properties of PD1 as well as the results from epoxide trapping experiments with human PMN and the isolation of two vicinal diol 16,17S-docosatrienes as minor products [13], it is likely that, once the 16,17-epoxide [48, 50] is generated in situ (as illustrated in Figure 2), an enzymatic reaction is needed to produce PD1 carrying the 10R,17S-dihydroxy-trans,trans,cis configuration arising from an epoxide intermediate as depicted in Figure 2 that is produced [48].
Actions of Protectin D1 in vivo
Keep in mind that resolution mechanisms need to proceed in all organs from head to toe, where some organ-dependent differences, i.e. kinetics, may occur [8, 68]. As indicated above, the complete stereochemical assignment for synthetic PD1 also relied on determining biological action of the related isomers. Earlier results indicated that PD1's anti-inflammatory properties were comprised of limiting leukocyte infiltration in murine systems [9, 13, 44, 56]. Synthetic PD1 reduced human PMN transmigration in response to leukotriene B4 and T cells [12, 48, 69]. Amounts as small as 1.0 nM gave 30% inhibition in leukocyte infiltration. The Δ15-trans isomer of PD1, where the conjugated triene portion of the molecule is in the trans configuration, did not block PMN transmigration in vitro [50].
These PMN transmigration experiments were carried out in parallel with murine acute inflammation. In these, acute peritonitis was initiated by challenge with the microbial isolate zymosan A and the actions of five isomers were assessed in vivo. Two compounds (10S,17R,-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic-acid and 10S,17S-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic-acid; see ref. [50]) were excluded from matching with PD1 because the physical retention times on LC and GCMS [50] and biosynthetic considerations indicated that they were not likely candidates for endogenous human PD1 or isomers produced. It is noteworthy that PD1 at doses as low as 1 ng per mouse gave striking inhibition of PMN infiltration within the exudates. In these studies, the double dioxygenation product 10S,17S-docosatriene (PDX) was substantially less potent. In this context, the double dioxygenation product PDX was not active at 0.1 ng compared directly to synthetic PD1. At higher doses, 10S,17S-HDHA blocked PMN infiltration, but it was less potent than PD1. The 10R version of the double dioxygenation products, was essentially equipotent at a 1 ng dose but did not increase potency in a dose-dependent fashion at 10 ng and 100 ng doses [50]. The Δ15-trans isomer of PD1 was, at equal doses of 1 ng/mouse, substantially less potent. Of interest, 10S,17S-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic-acid was the most potent of this series of isomers in vivo. However, only trace amounts were obtained in isolated human PMN extracts. Hence, a rank order of potency at the 0.1 ng dose of these 10,17-diHDHA isomers was 10S,17S-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic- acid ≫ PD1 > 10S,17S-DiHDHA (also known as PDX, the double dioxygenation product [67]) > the Δ15-trans-PD1 ≫ 10S,17R,-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic-acid. In these, we also assessed the carboxy methyl ester of PD1 versus the native synthetic PD1. The carbon 1-position carboxy-methyl ester was similar in its ability to block in vivo the hallmark of acute inflammation, namely PMN infiltration. The methyl ester of 10S,17S-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic-acid also proved to be a potent regulator of PMN infiltration and diminished pain in vivo [70]. One of the protectins, 10,17-docosatriene, is also produced in murine ischemic stroke and is a potent regulator of PMN infiltration, reducing stroke-mediated tissue damage [44], and in ocular systems [71]. Given its potent protective actions in the retina and brain, we initially termed this bioactive mediator neuroprotectin D1 (NPD1) [12, 14, 72]. Since this potent chemical mediator has a broader range of activities in the immune, cardiovascular and renal systems, for nonneuronal local biosynthesis and actions we used the name protectin D1 (PD1) for the first in this family of mediators. The complete stereochemistry and anti-inflammatory actions of PD1 (10R,17S-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic acid) were established [50] and its biosynthesis in lymphocytes and immunoregulatory roles also demonstrated [8, 48, 69]. PD1 is also renoprotective [73], induces corneal nerve regeneration [74] and stimulates cardiac and neural stem cell differentiation at nanomolar potencies [75]; see Table 1.
Table 1. Production and actions of Protectins and Maresins.
| (A) Protectins | |||||
|---|---|---|---|---|---|
|
| |||||
| Mediator | Species /SystemInvestigated | Concentration / Amount | Action(s) | Function | In vivo Production |
| NPD1 / PD1 | Mouse/ Peritonitis | 300 ng / mouse | Inhibits neutrophil recruitment; regulates chemokine/ cytokine production [43, 50] | ||
| 300 ng / mouse | Promotes lymphatic removal of phagocytes [76] | ||||
| 100 ng / mouse | Regulates T-cell migration [48] | ||||
| Mouse/Asthma | 2-200 ng / mouse / 4 days | Protects from lung damage, airway inflammation and hyperresponsiveness [137] | |||
| 100 ng / mouse | Accelerates catabasis of Th2-mediated inflammation [138] | ||||
| 11 pg / mouse | Toll-like receptor triggers production of PD1 [138] | ||||
| Human/Asthma | ∼2 ng | PD1 is generated in human asthma [137] | |||
| Human Eosinophils / Asthma | 10 ng / 106 cells in healthy subjects | Dysregulation of PD1 in eosinophils from asthma patients [139] | |||
| Mouse / Eosinophils | 5 μg / mouse | Rescues delayed resolution in eosinophil depleted mice [140] | |||
| Mouse/Kidney ischemia -reperfusion | 3.5 - 35μg / mouse | Protects from ischemia-reperfusion-induced kidney damage and loss of function; regulates macrophages [73, 141] | |||
| 160 pg / kidney | Endogenous formation in kidney increased for ω-3 PUFA [73] | ||||
| Mouse/ Retinopathy | 10 ng / mouse | Protects against neovascularization[71] | |||
| Ischemic stroke | 100 ng / mouse | Inhibits leukocyte infiltration, NF and cyclooxygenase-2 induction [14, 44] | |||
| Human/Alzheimer's disease | 5 pmol/mg protein | Diminished PD1production in human Alzheimer's disease [142] | |||
| Mouse/Liver Injury | 100 nM | Protects from necro-inflammatory liver injury [143] | |||
| Rabbit/Corneal Injury | 100 ng / rabbit | Promotes regeneration of corneal nerves following surgery [144] | |||
| Mouse / Stem Cells | 50 nM | Protects stem cells from oxidative stress [75] | |||
| Mouse / Lyme Disease | 0.1 pg / mg of tissue | PD1 produced during the resolution of Lyme disease [145] | |||
| Rat / Optic Nerve Injury | 5 μg / rat | Inhibits cell ganglion death [146] | |||
| Mouse / obesity | 100 nM | Regulates adiponectin in adipose tissue of obese (ob/ob) mice [147] | |||
| ∼150 pg / mouse | Generated in adipose tissue [147] | ||||
| Mouse /neuronal plasticity | 1 ng/mL | Reduces TRPV1-mediated inflammatory pain [70] | |||
| Mouse /neuronal plasticity | 300 ng / mouse | Antinociceptive without associated tolerance [148] | |||
| Mouse / Herpes simplex virus 1 | 300 ng / mouse | Reduction of stromal keratitis and neovascularization [149] | |||
| Rats & Mouse / Epilepsy | 50 nM | Attenuates evoked hippocampal seizures [150] | |||
| Fat-1 Mouse / colitis | 0.2 ng / mg colon tissue | Physiologically active levels produced in colon of transgenic mice [151] | |||
| Human / ARPE-19 cells | 50 nM | Anti-apoptotic for ARPE-19 cell survival [152] | |||
| Human Mφ PMN / Phagocytosis | 0.1-10 nM | Promotes bacterial clearance [57] | |||
| Mouse / E. coli peritonitis | 50 ng/mouse | Protects from hypothermia [57] and reduces bacterial titers | |||
| 1 ng / mouse | Lower levels in higher bacterial challenge [57] | ||||
| 10S, 17S diHDHA (PDX) | Mouse/ Peritonitis | 300 ng / mouse | Inhibits neutrophil recruitment; regulates chemokine/ cytokine production [50] | ||
| Mouse/H1N1 | 100 ng/ mouse | Antiviral; attenuates translocation [153] | |||
| Human/ Platelets | 1 μM | Inhibits platelet aggregation [64, 136] | |||
| Mouse / Acute Lung Injury | 200 μg / mouse | Enhances neutrophil apoptosis [154] | |||
| AT-PD1 | Mouse/Diabetes | 1 μg/mouse | Stimulates skeletal muscle IL-6 release; improves insulin sensitivity [67] | ||
| Mouse / Peritonitis | Regulates PMN infiltration and promote efferocytosis [49] | ||||
| Rat / Stroke | 333 μg / kg | Reduces brain infarction and edema in stroke [155] | |||
| (B) Maresins | |||||
|---|---|---|---|---|---|
|
| |||||
| Mediator | Species / System Investigated | Concentration / Amount | Action(s) | Function | In vivo Production |
| Maresins | Mouse / Peritonitis | 0.1 ng / mouse | Inhibits neutrophil recruitment; enhances phagocyte clearance [55] | ||
| Planaria / regeneration | 100 nM | Stimulates tissue regeneration in planaria [54] | |||
| Mouse / pain Human/Rheuma-toid Arthritis | 10ng /mouse7 pg / 50 μL SF | Antinociceptive [54] | Identified in synovial fluid extracts [113] | ||
| Mouse/ Peritonitis | 26 pg / mouse | Elevated levels with CO inhalation [134] | |||
| Human MΦand neutrophils / phagocytosis and efferocytosis | 0.1-10 nM | Inhibits proinflammatory mediator production by LTA4H and AA conversion [55, 115] | |||
| 24 pg / 2×105MΦ43 pg / 3×105PMN | Macrophage and macrophage of apoptotic PMN [112] | ||||
| Mouse/Colitis | 300 ng / mouse | Reduced PMN infiltration and cytokine expression as well as NF-κB activation [156] | |||
| Mouse/Sepsis | 10 nM | Promotes efferocytosis [157] | |||
| Mouse/Acute Lung Injury | 100 nM | Inhibits neutrophil recruitment and promotes clearance [158] | |||
In earlier experiments with mice, when administered i.v., 10,17S-docosatriene (Tables 1 and 2) was found to be more potent than indomethacin in reducing PMN infiltration in peritonitis, i.e., ∼40% inhibition at 100 ng/mouse [13]. Synthetic PD1 in as small a dose as 1 ng/mouse gave ∼40% inhibition of PMN infiltration that was maintained at the 10 ng and 100 ng doses. Thus, PD1 is a potent regulator of human and mouse PMN infiltration but does not completely block PMN recruitment, which is consistent with its autacoid actions and apparently does not compromise host defense via immune suppression of effector cell function [76]. This was also the case with human PMN transmigration, which required 10-100 nM PD1 to reduce PMN transmigration by 35-45% in vitro. Thus, although PD1 stereoselectively reduces PMN transmigration in vitro, given its potent actions in vivo, PD1 likely targets additional cell types in vivo to evoke its potent anti-inflammatory actions in vivo (Table 1). Alternatively, these potencies in vivo vs. isolated human cells might also reflect species differences. As an inducer of peritonitis, zymosan stimulates the initial formation of many endogenous chemoattractants for PMN, i.e., LTB4, the complement component C5a, chemokines and cytokines [56]. Since PD1 stops PMN recruitment in vivo. it counteracts these several different sets of PMN chemoattractants that regulate trafficking of these cells in vivo [56]. Given the inherent chemical labilities of PD1, we also prepared and tested a more chemically stable form denoted 15,16-dehydro-PD1. In general, acetylenic triple bonds are more stable than conjugated double bond systems, which are prone to isomerization. Although less potent, chemical stabilization of the conjugated double bonds with an acetylenic form proved useful as the molecule retained activity in vivo (Tables 1 and 2). These results are consistent with the ∼40% inhibition obtained with a 4,5-acetylenic analog of PD1 [56].
Table 2. Anti-inflammatory and tissue-protective roles: 12/15-lipoxygenase, 15-lipoxygenase type I and their products.
| (A) In vivo modification | ||||
|---|---|---|---|---|
|
| ||||
| Animal models | Alox15 gene modification | Actions/Phenotypes | References | |
| Periodontitis in rabbit | Alox15 transgenic | ↓PMN-mediated tissue degradation and bone loss | [132] | |
| Cornea injury | Alox12/15 deficient mice | ↑Inflammation ↓ Wound healing ↓ Corneal re-epithelialization ↓ Endogenous LXA4 production ↓ Heme-oxygenase 1 LXA4 rescues exacerbated inflammation and impaired wound healing in Alox15 deficient mice |
[46][159] | |
| Atherosclerosis | Alox12/15 transgenic mice | Delayed atherosclerosis ↓ IL-17, CCL5, PGE2 ↑ PD1 |
[133] | |
| Alox12/15 deficient mice | Accelerated atherosclerosis ↑ IL-12p40, CCL5 ↑ LXA4 production in macrophages |
|||
| Peritonitis | Alox12/15 deficient mice | ↓14-HDHA | [55] | |
| Arthritis | Alox12/15 deficient mice | ↑ Inflammatory gene expression ↓ LXA4 in inflamed synovia and macrophages |
[160] | |
| Collagen-induced arthritis | COX-2 product PGE2 induces Alox12/15. PGE2 stimulates resolution via LXA4 |
[161] | ||
| Suture-induced chronic cornea Injury | Alox12/15 deficient mice | ↑ Inflammatory neovascularization | [162] | |
| Peritonitis | Alox12/15 deficient mice | Resolution deficit caused by eosinophil depletion was rescued by eosinophil restoration or the administration of PD1. Eosinophils from Alox12/15 deficient mice could not rescue the resolution | [140] | |
| phenotype | ||||
| Dermal fibrosis | Alox12/15 deficient mice | ↑ TGF-b stimulated MAPK pathway LXA4 counters TGF-b stimulated fibroblast activation |
[163] | |
| Endometriosis | Alox12/15 deficient mice | EPA administration decreased the number of lesions in controls but not in Alox12/15 deficient mice. Reduced levels of RvE3 after EPA administration in Alox12/15 deficient mice compared to control |
[164] | |
| Airway inflammation | Alox12/15 deficient mice | ↓ TLR7-mediated resolution of airway inflammation | [138] | |
| Peritonitis | Alox12/15 deficient mice | Low dose inhaled CO treatment reduces PMN infiltration in WT control, but failed to regulate PMN in Alox12/15 deficient mice | [134] | |
| (B) In vitro modification | |||
|---|---|---|---|
|
| |||
| Cellular systems | Alox15 gene modification | Actions/Phenotypes | References |
| Isolated Th2 cells | Alox15 type 1 siRNA knockdown | ↓ PD1 production | [69] |
| Retinal pigment epithelial cells | Alox15 type 1 siRNA knockdown | ↑ Sensitivity to oxidative stress-induced apoptosis NPD1 rescues Alox15-silenced cells from oxidative stress-induced apoptosis |
[135] |
| Human macrophages | Alox15 type 1 siRNA knockdown | ↓ CO-induced HO-1 expression ↓RvD1 and RvD5 |
[134] |
On identification and structural elucidation of 10,17-diHDHA in resolving inflammatory exudates [9, 48, 56] and its potent anti-inflammatory actions, it was critical to establish its biosynthesis from DHA. To address this, we also studied isolated human PMN, whole blood, microglial cells, and murine exudates and tissues for the purpose of direct comparison [9, 13].
In addition to PD1, which carried potent bioactions, an isomer of PD1, 10S,17SdiHDHA (PDX), was also identified for the first time (Fig. 2). This compound proved to be a double dioxygenation product and was also formed from DHA but in a reaction that required two sequential lipoxygenation steps and oxygen incorporation that was directed at the 10S position from molecular oxygen (i.e., 18O2 in an enriched atmosphere in vitro). This reaction to products of 10S,17S-diHDHA is markedly different from the proposed enzymatic hydrolysis of the epoxide intermediate. The double dioxygenation product formed in vivo is different from PD1 in at least three key ways: a) PD1 carbon 10 position alcohol is in the 10R configuration while the dioxygenation product is in the 10S configuration; b) the double bond structure of PD1 conjugated triene is in the 11E,13E,15Z configuration; the 10S,17S-dioxygenation product is in the 11E,13Z,15E configuration; c) most importantly, PD1 is more potent: PD1 ≫ 10S,17S-diHDHA; and d) PD1 is generated by isolated human leukocytes and tissues.
Also in support of the stereospecific basis of these DHA-derived products in human and murine systems is the bioaction of the Δ15-trans-PD1 isomer, which can arise via workup-induced isomerization of PD1 and possesses little bioactivity in vitro or in vivo within the dose or concentration range (Fig. 2) observed with biogenic or synthetic PD1. Also, 10R,17S-dihydroxy-docosa-4Z,7Z,11E,13Z,15E,19Z-hexaenoic-acid, identified in human leukocytes (Fig. 2) and which differed from 10S,17S-dihydroxy-docosa-4Z,7Z,11E,13Z,15E,19Z-hexaenoic acid at the 10R position and carried the same double bond geometry, was essentially equipotent at a 1 ng dose (Fig. 2). Hence, the biosynthesis of PD1 from DHA appears to require stereoselective enzymatic steps to evoke bioactions. This requirement for stereoselective enzymatic reactions is widely appreciated in the biosynthesis of eicosanoids (9, 44). Of interest, human leukocytes specifically bind 3H-labeled NPD1/PD1 [77]. Thus the fidelity of the enzyme that produces PD1 from the proposed carbonium cation intermediate [13] in its ability to direct insertion of H2O-derived alcohol at carbon 10 exclusively in the 10R with apparently trace amounts of 10S as in 10S,17S-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic-acid is an intriguing point for further studies. The GPCR for NPD1/PD1 is currently not known, whereas the GPCRs for RvE1, RvD1 and LXA4 are known and were recently reviewed in Serhan and Chiang [78].
Earlier results indicated that DHA, which does not appear to be a natural substrate for potato 5-lipoxygenase, is converted to 10-HDHA by this enzyme and the double dioxygenation product 10,20-diHDHA [79]. Of interest, Whelan et al. [80] demonstrated that this plant lipoxygenase is highly versatile with DHA as a substrate and identified several monohydroxy-DHA products at carbon positions 4, 7, 8, 11, 13, 14, 16, 17 to give positional isomers of HDHA. Each of these was an enzymatic product of this flexible enzyme. As with other lipoxygenases, we found that potato 5-LOX as well as the soybean 15-lipoxygenase gave specific diHDHA profiles of products that were dependent on pH, enzyme, and substrate concentrations used in the incubations [9]. When the substrates were presented in micellar configuration with the enzymes, hydroperoxy intermediates were converted to epoxides that, on hydrolysis, gave many of the isomers as relatively minor products but were nonetheless in quantities useful for in vitro and in vivo studies [56]. These results were advantageous in the preparation of key pathway intermediates (i.e., 7,17-diHDHA, Resolvin D5, 17S-HDHA, and 17 S-H(p)DHA) to mammalian systems used in biosynthesis studies and determining the identity and actions of enzymatic products generated in vivo as well as by isolated human cells from DHA [9, 13, 48].
Both DHA potato 5-LOX products 10,20-diDHA and 10-HDHA were originally reported [Ref 79; doctoral thesis]. The classic steric analysis of 10S-HDHA and the formation of 10,20-diHDHA and 17-H(p)DHA were reportedly optimized for the plant LOs [81]. In our experiments, the double dioxygenation product prepared, matched, and identified in both human PMN and in vivo during peritonitis carries its alcohols as expected in the 10S,17S configuration in this diHDHA (10S,17S-dihydroxy-docosa-4Z,7Z,11E,13Z,15E,19Z-hexaenoic acid). Hence, this natural isomer of PD1 formed in vivo from DHA has its Δ13 position double bond in the cis configuration (i.e., 13Z) and its Δ11 in the trans configuration within the conjugated triene portion of the molecule (11E,13Z,15E) and possesses some anti-inflammatory activity in vivo. albeit proved to be much less potent than natural or synthetic PD1. In humans in vivo, PD1 level may not be apparent on chromatographic analysis with LC-MS-MS, but the endogenous biosynthetic isomers Δ15-trans-PD1, 10-epi-15-trans-PD1, etc. can be identified in substantial amounts that signify the activation of the pathways in situ [82].
In addition to this lipoxygenase-initiated route of biosynthesis for PD1, an aspirintriggered route with a 17R epimer of PD1 (17R series) is apparent with human cells via acetylated COX-2 and subsequent reactions [9, 44]; the complete stereochemistry of this bioactive epimer is now determined; see below. It is of interest to note that 10S,17R-dihydroxy-docosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic acid [50] was essentially inactive in vivo.
Aspirin-Triggered Mediators
Aspirin-triggered resolvins and related ω-3 -derived mediators were first identified in self-limited resolving murine exudates as well as brain, and their production documented with isolated human cells (i.e., leukocytes, microglia and vascular cells) [9] and in stroke [44]. The complete stereochemistry and bioactions of this aspirin-triggered 10,17-docosatriene was recently established [49]. The complete stereochemistry of the aspirin-triggered protectin pathway from murine exudates and human PMN is shown in Figure 3. AT-(NPD1/PD1) displays potent protective bioactions comparable to NPD1/PD1 both in vitro and in vivo. reducing both PMN infiltration and enhancing the removal of apoptotic PMN by macrophages, and hence signals the cardinal signs of resolution.
Figure 3. Aspirin-Triggered (AT) Protectin Biosynthetic Pathway.
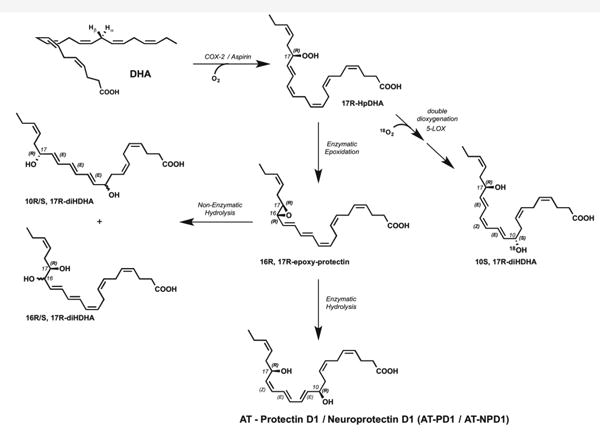
An additional pathway via aspirin-acetylated COX-2 enzyme gives rise to inversion of stereochemistry at the 17 position to afford the 17R hydroxyl-containing products. The 17R hydroperoxide precursor can undergo enzymatic epoxidation to the 16R, 17R epoxy protectin. This epoxide is then enzymatically hydrolyzed to the 10R, 17R AT-(NPD1/PD1).
Aspirin is unique in its mode of action. Unlike many of the current antiinflammatories that delay complete resolution and are considered toxic to this vital process (i.e., resolution toxic) [76, 83], aspirin jump-starts resolution by novel previously unrecognized mechanisms that involve the biosynthesis of aspirin-triggered (AT) lipid mediators [84, 85]. Along these lines, aspirin-triggered lipoxins were the first aspirintriggered lipid mediators uncovered [86]. Aspirin is well appreciated for its ability to inhibit COX-1 and inactivate this enzyme, blocking both prostaglandin and thromboxane production in cells that possess these biosynthetic pathways [87, 88]. The mechanism of aspirin's action involves acetylation of COX within the enzyme's catalytic region. This prevents alignment of the substrate arachidonic acid for oxygenation within the catalytic center that produces the prostaglandin endoperoxide intermediate (PGG2) required for the biosynthesis of both thromboxanes and prostaglandins via COX-1.
Aspirin's action within cells that possess COX-2 appears different. The catalytic region of COX-2 is larger than that of COX-1 and when acetylated by aspirin the biosynthesis of endoperoxide is blocked. Yet, unlike COX-1, acetylated COX-2 remains active producing lipoxygenase-like products such as 15-HETE from arachidonic acid [10] but with the oxygen insertion in the R configuration rather than S as is the case with lipoxygenases [86, 89]. The COX-2-produced 15R-HETE is converted to the potent bioactive aspirin-triggered lipoxins that retain the carbon 15 position alcohol in the R configuration as in AT-15R-(epi)-lipoxin A4, which is produced in vivo in humans [90]. AT-LXA4 is longer acting in vivo than LXA4 because the 15R alcohol is less efficiently enzymatically converted to the inactive 15-oxo-LXA4 metabolite [91]. This aspirintriggered pathway was recently demonstrated in humans, where low-dose aspirin is antiinflammatory and triggers the endogenous biosynthesis of AT-LXA4, which in turn stops PMN infiltration in skin blisters [Ref. 92 and references within].
AT-(NPD1/PD1) was identified in resolving murine exudates treated with aspirin [9]. Thus, biologic AT-(NPD1/PD1) was obtained from resolving murine exudates in vivo. To this end, peritonitis was initiated via intra-peritoneal (i.p.) administration of zymosan A (1 mg/mouse), and exudates were harvested 24 hours post injection (i.e. within the resolution phase [43]). Exudates were taken for LC-UV-MS-MS-based mediator lipidomics [49]. Among the candidates, synthetic AT-(NPD1/PD1) matched peak I, by co-injection. Synthetic AT-(NPD1/PD1) gave a UV spectrum and tandem mass spectrum that was essentially identical to the material beneath, which further confirmed the matching. AT-(NPD1/PD1) was also isolated and identified from activated human leukocytes, namely, aspirin treated human PMN. By matching biologic materials from both human and murine exudates AT-(NPD1/PD1) with synthetic candidates, the results established the complete stereochemistry of endogenous AT-(NPD1/PD1) as 10R,17Rdihydroxydocosa-4Z,7Z,10E,12E,14Z,19Z-hexaenoic acid [Ref 49 and see Figure 3].
AT-NPD1/PD1 Stops Neutrophil Infiltration: PMN Cessation in vivo
The complete stereochemical assignment for AT-(NPD1/PD1) also relied on determining in parallel its biological actions [49]. Earlier results indicated that NPD1/PD1 exerted potent anti-inflammatory actions regulating leukocyte trafficking in murine systems [9, 13, 50]. In these studies, we compared directly the bioactions of NPD1/PD1 to that of AT-(NPD1/PD1) carried out in parallel with the physical matching experiments. Synthetic AT-(NPD1/PD1) limited PMN infiltration into the peritoneum in TNFα-stimulated peritonitis. Both NPD1/PD1 (0.1 ng-10 ng) and AT-(NPD1/PD1) (0.01ng-10.0 ng) proved to be significant regulators of TNFα-stimulated leukocyte infiltration into the peritoneum (Tables 1 and 2). AT-(NPD1/PD1) reduced total leukocyte population of the exudate including PMN, monocyte and lymphocyte infiltrates, reaching a maximal reduction at 1 ng/mouse by as much as 50.4%. Also, both PD1 and AT-NPD1/PD1 reduced PMN infiltration in response to zymosan [49].
We studied whether PD1 or AT-NPD1 impacts PMN transendothelial migration using isolated human cells because this is the first committed step of leukocytes in acute inflammation. AT-(NPD1/PD1) and NPD1/PD1 (0.1-10.0 nM) each reduced (∼30% and ∼50%, respectively) PMN transendothelial migration induced by LTB4 [49]. In comparison, equal concentrations of the Δ15-trans isomer of AT-(NPD1/PD1) where the conjugated triene portion of the molecule was in the trans rather than cis configuration did not significantly reduce PMN transendothelial migration. Again in this system, the precursor DHA did not reduce LTB4-stimulated PMN-transendothelial migration at these concentrations. To corroborate these findings, we next used an electric cell-substrate impedance sensing system (ECIS) that sensitively quantitates cellular responses in two cell systems by real-time monitoring of barrier impedance [93]. Both AT-(NPD1/PD1) and NPD1/PD1 (1nM) decreased LTB4-stimulated PMN-transendothelial migration by ∼40 and 30%. AT-(NPD1/PD1) also enhanced the uptake of apoptotic human PMN by human macrophages at concentrations as low as 0.1 nM, as did NPD1/PD1 when compared directly [49].
This novel aspirin-triggered DHA metabolome impacts inflammation and resolution of cellular processes. On the basis of physical and biological properties in matching results with material from human cells, murine exudates and total organic syntheses, the complete stereochemistry of AT-(NPD1/PD1) proved to be 10R,17Rdihydroxydocosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic acid. The new aspirin-triggered product demonstrated potent regulatory actions with leukocytes in vivo and reduced human PMN transendothelial migration and enhances efferocytosis [49]. This matching approach was deemed necessary because typically less than nanogram amounts of a given lipid mediator are produced in vivo and >100 μg of isolated product is required for direct NMR determinations of conjugated double bonds that might give assignments for stereochemistry [50, 94-96] (see Figure 3).
Similar to the inversion of stereochemistry observed in the aspirin-triggered lipoxin and resolvin pathways, we anticipated that AT-(NPD1/PD1) was likely to possess the carbon 17R stereochemistry [9], rather than the 17S chirality present in NPD1/PD1 produced via a lipoxygenase reaction [12]. Aspirin acetylation of COX-2 gives rise to a catalytic activity that converts DHA to 17R-hydroxy-containing products [9]. It is noteworthy to point out that the chirality at the C-10 position and the double bond geometry of the triene system could not be reliably predicted based on LC-MS-MS lipidomics alone. As proposed for other potent polyunsaturated fatty acid-derived local mediators, it is likely that the aspirin-triggered protectin pathway involves the conversion of the hydroperoxide 17R-HpDHA to an epoxide intermediate (Figure 3). Given the significant conformational differences anticipated for these DHA-derived products, the stereochemical mode of the enzymatic epoxide opening and the resulting triene geometry needed to be verified by matching with isomers of known stereochemistry. In order to achieve the complete stereochemical assignments for the bioactive product(s), therefore, we prepared several geometric isomers of the 10,17R-dihydroxydocosa-4Z,7Z,11,13,15,19Z-hexaenoic acid with specific changes in R/S and Z/E configurations, and confirmed their stereochemistry using NMR spectroscopy. These synthetic materials were also used for the direct matching and comparison with biologically produced AT-(NPD1/PD1) [96].
Matching results indicate that in this aspirin-triggered DHA metabolome, the stereochemical configuration of AT-(NPD1/PD1) differs from NPD1/PD1 only at carbon C-17, so the two are diastereomers. Results from earlier investigations have shown that the differences in the MS and UV spectra between lipid mediator diastereomers are minimum if any [86, 94, 95]. The tandem mass spectra of the AT-17R-containing product and NPD1/PD1 were essentially identical, and both compounds displayed essentially the same triplet-band of absorbance-shaped UV spectra with λmaxMeOH at 271 nm (Figure 3), characteristic of “ol-triene-ol” structures [50, 97]. Some diastereomers can possess different physical properties [98] by which they can be physically differentiated. Indeed, NPD1/PD1 and its aspirin-triggered isoform were well separated using reverse phase lipid chromatography conditions. Diastereomers can give different biological properties, such as LTB4 and its natural isomer 12-epi-6-trans-LTB4, which is log orders of magnitude less active [97, 99].
TNFα is a well-known cytokine for its role in host defense, however aberrant or uncontrolled TNFα responses are associated with several inflammatory disorders [7]. Although anti-TNF therapies are widely available and in clinical use, it is becoming increasingly clear that a complete blockade of TNFα may promote adverse side effects [100], thus indicating limitations in this approach [101]. Importantly, AT-(NPD1/PD1) is a potent regulator of PMN infiltration in vivo yet did not completely block PMN recruitment, and hence is not immunosuppressive. This is consistent with the unique counterregulatory actions of resolvins and specialized proresolving mediators that do not compromise host defense via immune suppression of effector cell function [95]. In human PMN transmigration, 1-10 nM amounts of AT-(NPD1/PD1) reduced LTB4-stimulated PMN transmigration, and the Δ15-trans isomer of AT-(NPD1/PD1) was less potent, underscoring the stereoselectivity of AT-(NPD1/PD1) and the counterregulatory yet not immunosuppressive actions of pro-resolving mediators.
This assignment implies that the postulated enzyme-catalyzed opening of the 16R,17R epoxide precursor of AT-(NPD1/PD1) would proceed, in theory, via the introduction of the C-10 hydroxyl from the same side as the epoxide oxygen atom to give the 10R,17R configuration, likely from water (Fig. 3). This addition would be opposite of the observed opening of the 16S,17S epoxide-containing intermediate precursor of NPD1/PD1 that leads to the 10R,17S configuration. This difference suggests that the C-10 hydroxyl group is introduced via an enzyme-catalyzed process, and that the enzyme involved has a strong preference for the formation of the 10R isomer, rather than the stereochemical inversion of the epoxide precursor. These observations are consistent with the formation of a rigid cationic-type intermediate at the enzyme active site, which undergoes stereospecific attack by a water molecule from the same direction to afford the 10R product. Also, the well known antarafacial hydrogen abstraction in LTA4 biosynthesis in this case to produce the 16,17-epoxide-containing intermediate from DHA might be similar to the biosynthetic mechanism of LTA4 from 5-HpETE as carried out by the 5-LOX [102, 103]. It is possible in this scheme (Figure 3) that the 17-hydroperoxide intermediate is converted to an epoxide at C16-C17 position that could give to cis or trans epoxides that require enzymatic processing in situ to give the potent active stereochemical structure of AT-(NPD1/PD1).
In humans, low-dose aspirin triggers 15-epi-lipoxin production that appears in plasma of healthy subjects [90]. At low dose, aspirin increases 15-epi-LXA4 in skin blisters, which reduces PMN infiltration to the skin blister, demonstrating the antiinflammatory actions of low-dose aspirin in humans [92]. Aspirin treatment reduces mortality from colorectal cancer in long-term studies with daily use [104]. Omega-3 EFA (EPA and DHA) at ∼1g/day reduce cardiovascular mortality [105]. Thus, the combination of aspirin with omega-3 EFA and the aspirin-triggered lipid mediators (i.e., AT-LX, ATRv) may have a beneficial impact in many diseases associated with ongoing inflammation and host-mediated local tissue injury. Indeed, in a recent clinical study, the combination of both aspirin (81 mg/day) and omega-3 EPA and DHA significantly reduced periodontal disease in patients with chronic periodontitis [106], presumably by jump-starting resolution of periodontal inflammation via production of aspirin-triggered mediators and inhibition of prostanoids [107]. Hence, it is likely that the aspirin inhibition of prostanoids and concomitant biosynthesis of aspirin-triggered lipid mediators such as AT-lipoxins, AT-resolvins and AT-protectins, including the AT-(NPD1/PD1) pathway (Figs. 1 and 3), may each contribute to some of these beneficial outcomes, which remains to be established in humans taking aspirin long term.
Maresins
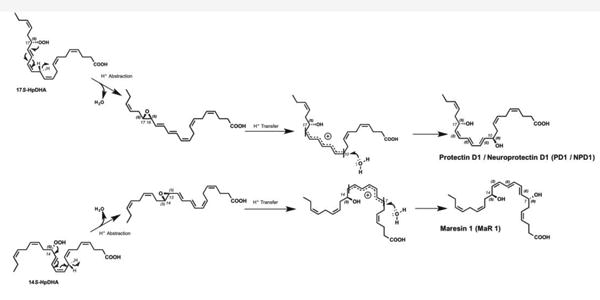
Macrophages play key roles in regulating the innate host response to local inflammation and tissue regeneration. These cells are also central in orchestrating other processes including neovascularization and wound healing [108-110]. A new family of DHA-derived pro-resolving mediators from macrophages was recently described and coined maresins (macrophage mediators in resolving inflammation). The first members of this family exert potent phagocyte-directed actions that include inhibition of neutrophil recruitment and stimulation of macrophage efferocytosis by the dihydroxy-containing products in this pathway [111]. The biosynthesis of maresins is initiated in macrophages by the 14-lipoxygenation of DHA producing the 14S-hydro(peroxy)-docosa- 4Z,7Z,10Z,12E,16Z,19Z-hexaenoic acid (14S-HpDHA; Figure 4). Profiling of LM using LC-MS-MS of murine self-resolving exudates demonstrates that 14S-HDHA levels, the maresin pathway marker, peak late into the resolution phase, suggesting a role for these mediators in re-establishing tissue homeostasis [111]. The maresin pathway is also present in human macrophages [111, 112] and was identified in human synovial fluids from patients with arthritis [113].
Figure 4. Maresin Biosynthetic Pathway.
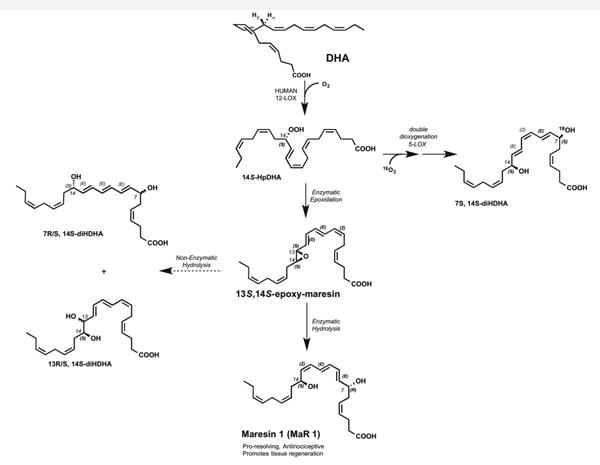
The biosynthesis of MaR1 is formed through 13, 14 epoxide intermediate confirmed by alcohol trapping products. In addition, several isomers formed through alternative pathways were confirmed by matching studies of synthetic compounds made in a stereo-controlled manner. See text for further details.
Maresin 1 (MaR1) is the first member identified from this family of macrophagederived pro-resolving mediators. As demonstrated by the identification of alcohol trapping products, the biosynthesis of MaR1 is proposed to involve a 13,14-epoxide intermediate as the MaR1 precursor. This epoxide intermediate is then proposed to be enzymatically hydrolyzed (see Figure 5) via an acid-catalyzed nucleophilic attack by water at carbon 7, resulting in the introduction of a hydroxyl group at that position and double-bond rearrangement to form the stereochemistry of bioactive MaR1 [111]. The complete stereochemistry of MaR1 proved to be 7R,14S-dihydroxy-docosa-4Z,8E,10E,12Z,16Z,19Z-hexaenoic acid, that was shown to possess potent bioactions [114]. MaR1 exerts stereospecific leukocyte-directed actions, characteristic of the maresin family. This pro-resolving mediator also exerts potent cancer-induced antinociceptive and tissue regenerative actions in wound healing in planaria (8).
Figure 5. Comparison of Mechanisms in Protectin and Maresin Biosynthesis.
Proton abstraction of the 17S hydroperoxide pictured above or the 14S hydroperoxide pictured below forms the 16S, 17S epoxide and 13S, 14S epoxide respectively. Enzymecatalyzed formation of a rigid carbonium cation intermediate from the respective epoxides undergoes a stereospecific attack by oxygen from a water molecule. This enzyme-catalyzed hydrolysis affords predominantly the R insertion of oxygen from water at the 10 position in the upper protectin pathway and at the 7 position in the lower maresin pathway.
These findings and the biosynthesis of MaR1 in flatworms suggested that maresin structure and function are conserved in evolution [114]. Given the potent actions of MaR1 it was deemed critical to establish the complete stereochemistry and stereospecific conversion of the proposed epoxide intermediate to MaR1. Also, using stereochemically pure material obtained by total organic synthesis we uncovered novel bioactions of this key epoxy-containing intermediate that regulates leukotriene B4 production via directly inhibiting LTA4 hydrolase and provides novel mechanisms for phagocytes to stimulate the tissues' return to homeostasis [115]. Recently, MaR2 was elucidated and named because it also possesses potent bioactions in vivo [116].
Maresin Biosynthesis and Structural Elucidation
Using material obtained by stereo-controlled organic synthesis in combination with NMR spectroscopy and LM metabololipidomics, we establish the complete stereochemistry of this 13S,14S–epoxy-docosahexaenoic acid as 13S,14S-epoxy-docosa-4Z,7Z,9E,11E,16Z,19Z-hexaenoic acid (Fig. 4) and demonstrate its precursor role in conversion to MaR1 by human macrophages. Also, incubation of this epoxide intermediate with isolated human recombinant LTA4 hydrolase (LTA4H) inhibited LTB4 production from LTA4. Moreover, incubation of human macrophage LOX with 13S,14Sepoxy-DHA selectively inhibited AA conversion to 12-HpETE. Together, these findings demonstrate novel bioactions within the maresin pathway in controlling proinflammatory LM (i.e. LTB4) as well as establish the stereochemistry of the epoxide intermediate in MaR1 biosynthesis.
Macrophages are key regulators of the inflammatory response with distinct macrophage subtypes linked with the propagation versus resolution of inflammation [112, 117]. In this context there are two broad categories of macrophages: M1 macrophages or classical macrophages are considered as pro-inflammatory, while M2 macrophages are linked with the re-establishment of homeostasis, wound healing and tissue regeneration [108, 110, 117]. A third macrophage subtype referred to as resolution phase macrophages was identified in resolving exudates, with these macrophages possessing characteristics of both M1 and M2 cells [108, 109], and each human subpopulation expresses 12-LOX [112, 116]. Recent results indicate that DHA and DHAderived pro-resolving mediators, including RvD1, can stimulate a switch in macrophage phenotype from pro-inflammatory to a pro-resolving M2-like phenotype [118, 119]. We recently found that human M2 macrophages are associated with higher MaR1 levels [112], a finding that is in line with the homeostatic and tissue regenerative actions of this pro-resolving mediator [111, 114]. Recently, we demonstrated that this is, at least in part, a result of enhanced ability of this macrophage subtype to convert the 13S,14S epoxide intermediate to MaR1 [115].
To establish the biosynthetic pathways for LM biosynthesis, it was deemed essential to determine the presence and stereochemistry of their intermediates [111, 115]. In the biosynthesis of MaR1 (Figure 4), DHA undergoes 14S-lipoxygenation to give 14-HpDHA, following H abstraction, that is converted to 13S,14S-epoxy-DHA, a proposed intermediate that is then further transformed to 7R,14S-dihydroxydocosa-4Z,8E,10E,12Z,16Z,19Z-hexaenoic acid, MaR1 [111]. Recently, we found that this 13,14-epoxide is produced by isolated human macrophage lipoxygenase, as demonstrated by the identification of the aqueous hydrolysis products of 13S,14S-epoxy-DHA along with the corresponding acid methanol trapping products from DHA [115] (Figure 1). Of note in these incubations we also identified the double dioxygenation isomer of MaR1, 7S,14S-dihydroxydocosa-4Z,8E,10Z,12E,16Z,19Z-hexaenoic acid [cf. 111, 114], suggesting that this macrophage 12-LOX also oxygenates DHA at C7. Although this double dioxygenation product (7S,14S-diHDHA) possesses some bioactivity [111, 114], within the context of inflammation it displays lower anti-inflammatory and pro-resolving actions than MaR1. Along these lines, the 14-HpDHA intermediate can also undergo another double dioxygenation at the penultimate carbon (omega-1) to give the 14S,21Rdihydroxydocosa-4Z,7Z,10Z,12E,16Z,19Z-hexaenoic acid [120]. This maresin-related pathway product displays tissue protective actions promoting wound healing in diabetic models and following renal ischemia reperfusion injury by restoring mesenchymal stem cell function [121, 122].
Biosynthesis of lipid mediators occurs at sites of inflammation and tissue injury whereby the intermediates are either rapidly transformed to bioactive mediators via stereospecific enzyme-mediated conversion or non-enzymatically hydrolyzed to virtually inactive products [96, 123, 124]. Therefore, tissue levels of these intermediates are transient and hence do not reach quantities that can be isolated for direct stereochemical determination by NMR spectroscopy [96]. To this end, we used direct matching of material obtained by total organic synthesis (which allows for the generation of compounds with known absolute stereochemistry) with biological materials [115]. This approach again permitted both the scale-up and confirmation of the potent antiinflammatory and pro-resolving actions of resolvins, protectins and MaR1 [reviewed in refs. 96, 114] as well as their unambiguous identification in biological tissues via targeted lipidomics (LC-MS-MS-based). The ability to identify resolvins revealed their remarkable protective actions including their ability to enhance immune vigilance [125] and to stimulate host immune responses, lowering antibiotic requirements during infection [126].
Using total organic synthesis, we established the absolute stereochemistry of the novel 13S,14S-epoxy-containing intermediate, which proved to be 13S,14S-epoxy-4Z,7Z,9E,11E,16Z,19Z-hexaenoic acid (Figure 4). When incubated with activated human macrophages this synthetic compound was readily converted to MaR1 (Figure 4). In contrast, incubation of this synthetic epoxide with heat-inactivated cells gave no conversion to MaR1, since the epoxide was instead converted to its corresponding nonenzymatic hydrolysis products (Figure 4). Hence, in the proposed biosynthesis of MaR1, the LOX first abstracts a hydrogen from the methylene group at C12 and inserts molecular oxygen at C14 to yield 14S-HpDHA.
In macrophages lacking the murine homologue of this enzyme (12/15-LOX), the conversion of DHA to 14-HpDHA was greatly reduced (>95%), indicating the role of the murine orthologue of 12-LOX in initiating MaR1 biosynthesis in macrophages [111] (Table 2). This HpDHA is then converted to the 13S,14S-epoxide by the same enzyme following a second hydrogen abstraction from the methylene group at C9. These results together indicate that in addition to catalyzing the 14-lipoxygenation of DHA this same enzyme is also an epoxidase producing the novel maresin epoxide intermediate (see scheme in Figure 4). This type of reaction has been demonstrated for 5-LOX, which converts arachidonic acid to 5-HpETE and then to LTA4 [102]. The conversion of the 13S,14S-epoxide to MaR1 then proceeds via an enzyme-mediated hydrolysis that converts the double bond geometry at the carbon 8 position from Z to E and at the carbon 12 position from Z to E, giving a final geometry around the triene region of MaR1 corresponding to 8E,10E,12Z (see Figure 4), as well as directs the insertion of a hydroxyl group (from H2O) at C7 [111]. Thus, the epoxide intermediate to MaR1 requires an enzyme-mediated hydrolysis and Z/E reconfiguration in order to give the conversion of the double bond geometry at Δ12 from trans to cis orientation, giving a final geometry of MaR1 (i.e. 7R,14S-dihydroxy-docosa-4Z,8E,10E,12Z,16Z,19Z-hexaenoic acid). In the absence of this enzyme, the 13S,14S-epoxide intermediate decays to aqueous hydrolysis products 7R/S,14S-dihydroxy-docosa-4Z,8E,10E,12E,16Z,19Z-hexaenoic acid and 13R/S,14S-dihydroxy-docosa-4Z,7Z,9E,11E,16Z,19Z-hexaenoic acid [115].
Because human LTA4H catalyzes LTA4 conversion to LTB4 [127] and is involved in the conversion of EPA to RvE1 in the E-series resolvins [128], we next assessed conversion of 13S,14S-epoxy-DHA with LTA4H, which did not result in MaR1 production [115]. These results rule out a role for LTA4H in converting the 13S,14Sepoxide intermediate to MaR1 (Figure 4). Leukocytes and in particular phagocytes are key cellular players regulating the onset and resolution of inflammation [129]. MaR1 is produced by macrophages during inflammation-resolution and exerts phagocyte-directed actions [111, 114].
Action of Maresins
When administered in vivo. MaR1 at concentrations as low as 0.1ng per mouse significantly reduced PMN accumulation in response to sterile injury [111, 114]. MaR1 is also a potent pro-phagocytic stimulus enhancing human macrophage phagocytosis as well as efferocytosis of apoptotic cells [111, 114]. Apart from leukocyte-directed actions, this pro-resolving mediator also exerts tissue-directed actions, whereby administration of MaR1 to surgically injured planaria accelerates tissue regeneration at the site of injury [114]. These results emphasize the role of MaR1 in regulating both local inflammatory responses and potentially stem cell function(s). One mechanism by which MaR1 might regulate stem cell responses is by promoting stem cell differentiation as recently described for another pro-resolving mediator, protectin D1 [130]. MaR1 also displays potent analgesic actions controlling local inflammation resolution and associated inflammatory pain, as well as neuropathic pain, via blocking TRPV1-mediated responses [114].
Activation of the maresin pathway can also impact inflammation-resolution by selectively reducing LTB4 production via direct inhibition of LTA4H (Figure 5). This is a regulatory mechanism that the 13S,14S-epoxide intermediate shares with LTA4 [131] and that would be operative in the conversion of DHA to MaR1. The ability of the 13S,14Sepoxy-DHA to directly inactivate LTA4H is not shared with MaR1; therefore conversion of the epoxide to MaR1 could result in a reduction of its LTA4H inhibition. We also found a novel regulatory mechanism in eicosanoid biosynthesis, whereby this 13S,14Sepoxy-maresin selectively inhibited AA conversion by 12-LOX [115]. Of interest, both MaR1 and 13S-14S-epoxy-DHA regulate macrophage phenotype skewing the macrophage profile towards a homeostatic and tissue protective phenotype. These findings point to novel anti-inflammatory mechanisms by the MaR1 biosynthetic pathway, and utilization of DHA can regulate pro-inflammatory eicosanoids via direct enzyme interactions with the potent autacoid actions of MaR1 and related products themselves as well as changing the macrophage phenotype.
Anti-Inflammatory and Tissue-Protective Roles of Mouse 12/15-Lipoxygenase, Human 15-Lipoxygenase Type 1 and Their Respective Products
Human 15-LOX type I (15-LOX-1) is essential for biosynthesis of lipoxins, protectins and D-series resolvins (Figure 1). In acute periodontitis, transgenic (TG) rabbits overexpressing human 15-LOX-1 markedly reduced bone loss and local inflammation compared to WT animals [132]. Enhanced LX production was associated with an increased anti-inflammatory status of 15-LO TG rabbits. These results indicate that overexpression of 15-LO type 1 and LXA4 is associated with reduced PMN-mediated tissue degradation and bone loss. On the other hand, ALOX12/15- (mouse orthologue of human 15-LOX-1) deficient mice exhibited exacerbated inflammation in numerous disease models as well as in cornea wound healing, associated with reduced endogenous levels of LXA4 (see Table 2 and references within). In addition, in cornea thermal injury, LXA4 rescues excessive inflammation and impaired wound healing in Alox15-deficient mice. Moreover, in ALOX12/15 deficient mice, 14-HDHA levels were greatly reduced, indicating the key role of ALOX12/15 in MaR1 biosynthesis pathway [55]. Thus, 12/15-lipoxygenase in mice shows both pro-inflammatory phenotype and anti-inflammatory phenotype [133] that appear to depend on cell type specificity and diet. For human cells, in vitro shRNA knockdown of human 15-LOX-1, PD1 and resolvin levels were also significantly reduced in isolated Th2 lymphocytes, macrophages [48, 134] and epithelial cells [135] (Table 2).
Concluding Remarks
Identification of novel lipid mediators involved in the active resolution of inflammation will lead to future innovative therapeutic strategies toward many inflammatory diseases. Therefore, each SPM has to be fully documented in terms of structure, which is intrinsically related to its functions. Our group first reported PD1 in murine exudates and human cells [9] as well as murine brains [13], and we established stereochemistry of the bioactive molecule and related products [50]. Using total organic synthesis, PD1 stereochemistry was unambiguously assigned and separated from its double oxygenation isomer 10S,17S-diHDHA [48, 50], which was also confirmed and named PDX by Chen et al. [64]. PDX belongs to the Poxytrins family (for PUFA oxygenated trienes), which regroup lipid mediators produced by a double lipoxygenation process leading to a specific E,Z,E motif [136] without the requirement for an epoxide formation (such as PD1). These two bioactive lipid mediators from DHA, even though belonging to the protectin family [50], have very distinct structures and biosynthesis, and therefore very distinct potency, bioactivity and target cell types of action. While investigating the potential biological actions of the protectins (i.e. PD1 and PDX), it is important to remember that, despite their common name, their presence reflects different biosynthetic pathways; therefore, their production is likely to be differentially regulated depending on the cell trafficking.
Figure 5 illustrates a comparison in the mechanism of protectin and maresin biosynthesis; each is initiated via H abstraction from the precursor DHA that is catalyzed by distinct lipoxygenase enzymes in a stereospecific manner. Maresin biosynthesis is initiated by human macrophage 12-lipoxygenase and converts DHA to an epoxide intermediate 13S,14S-eMAR, which itself displays anti-inflammatory actions and promotes macrophage phenotype switching. 13S,14S-eMaR in turn is enzymatically converted to MaR1, which displays potent pro-resolving, anti-nociceptive and tissue regenerative actions. The complete stereochemistry of this mediator, several of its biosynthetic isomers as well as that of 13S,14S-eMaR have now been elucidated, thus providing novel tools for investigating the biological roles of maresins in host responses and re-establishment of homeostasis.
In conclusion, the acute inflammatory response is the first line of protection in response to both sterile and infectious insults. Within this, mediators produced by cellular traffic at the site of inflammation are critical in determining the amplitude and duration of this response. Classic arachidonic acid-derived pro-inflammatory eicosanoids promote vascular leakage, pain, thrombosis and the amplification of leukocyte recruitment. The specialized pro-resolving mediators, including protectins and maresins, actively counterregulate the actions of these pro-inflammatory mediators. Resolution mediators evoke the cardinal signs of resolution, namely, they: a) limit further neutrophil recruitment, b) promote macrophage clearance of debris and bacteria, c) stimulate tissue regeneration and d) reduce pain. The complete stereochemistry and biosynthetic pathways have now been established for each of the main pro-resolving mediators, in addition to their total confirmation by organic synthesis. These open new directions in understanding their roles in pathobiology and provide novel avenues for treatment of conditions where resolution pathways may be defective.
Highlights.
Proresolving mediators are biosynthesized during resolution phase of acute inflammation
Resolution is a biosynthetically active process
Protectins and maresins are two structurally distinct families of potent local mediators
NPD1/PD1 reduces neural inflammation, stimulates resolution and reduces pain
MaR1 stimulates tissue regeneration and resolution mechanisms, is antiinflammatory and reduces pain.
Acknowledgments
We thank Mary H. Small for expert assistance in manuscript preparation. This work was supported in part by a research grant from the Mérieux Foundation and NIH grant nos. R01GM038765 and P01GM095467.
Abbreviations used in this paper
- 5S-HETE
5S-hydroxy-6E,8Z,11Z,14Z-eicosatetraenoic acid
- 7S
14S-diHDHA, 7S,14S-dihydroxydocosa-4Z,8E,10Z,12E,16Z,19Z-hexaenoic acid
- 10S
17S-diHDHA, 10S,17S-dihydroxy-docosa-4Z,7Z,11E,13Z,15E,19Z-hexaenoic acid (the dioxygenation product)
- 12-HETE
12-hydroxy-5Z,8Z,10E,14Z-eicosatetraenoic acid
- 14S-HDHA
14S-hydroxy-4Z,7Z,10Z,12E,16Z,19Z-docosahexaenoic acid
- 14SHDHA
14S-hydroxy-4Z,7Z,10Z,12E,16Z,19Z-docosahexaenoic acid
- 14S-HpDHA
14S-hydro(peroxy)-4Z,7Z,10Z,12E,16Z,19Z-docosahexaenoic acid
- 17S-H(p)DHA
17Shydro(peroxy)-DHA
- DHA, C22
6, docosahexaenoic acid
- EPA, C20
5, eicosapentaenoic acid
- GC
gas chromatography
- NMR
nuclear magnetic resonance
- hm12-LOX
human macrophage 12-lipoxygenase
- LC
liquid chromatography
- LOX
lipoxygenase
- LM
lipid mediator
- LT
leukotriene
- LTB4
5S,12R-dihydroxy-6Z,8E,10E,14Z-eicosatetraenoic acid
- LX
lipoxin
- Maresin
macrophage mediator in resolving inflammation
- MaR1
maresin 1 (7R, 14S-dihydroxy-docosa-4Z, 8E,10E, 12Z,16Z, 19Z-hexaenoic acid)
- MSMS
tandem mass spectrometry
- NPD1
neuroprotectin D1
- PMN
polymorphonuclear leukocyte
- PD1
protectin D1/neuroprotectin D1,10R,17S-dihydroxydocosa-4Z,7Z,11E,13E,15Z,19Z-hexaenoic acid (neuro prefix is added to denote the tissue and functional role of protectin D1)
- pt5LOX
5-LOX from potato
- RvD1
Resolvin D1 (7S, 8R, 17S-trihydroxy-docosa-4Z, 9E, 11E, 13Z, 15E, 19Z-hexaenoic acid)
- RvD2
Resolvin D2 (7S, 16R, 17S-trihydroxy-docosa-4Z, 8E, 10Z, 12E, 14E, 19Z-hexaenoic acid)
- RvD3
Resolvin D3 (4S, 11R, 17S- trihydroxy-docosa-5Z, 7E, 9E, 13Z, 15E, 19Z-hexaenoic acid)
- RvE1
Resolvin E1, 5S,12R,18R-trihydroxy-6Z,8E,10E,14Z,16E-eicosapentaenoic acid
- STZ
serum-treated zymosan
Footnotes
Disclosure: CNS is an inventor on patents [resolvins] assigned to BWH and licensed to Resolvyx Pharmaceuticals. CNS is a scientific founder of Resolvyx Pharmaceuticals and owns equity in the company. CNS' interests were reviewed and are managed by the Brigham and Women's Hospital and Partners HealthCare in accordance with their conflict of interest policies.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bazan NG. Cell survival matters: docosahexaenoic acid signaling, neuroprotection and photoreceptors. Trends Neurosci. 2006;29:263–271. doi: 10.1016/j.tins.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Crawford MA, Broadhurst CL, Guest M, Nagar A, Wang Y, Ghebremeskel K, Schmidt WF. A quantum theory for the irreplaceable role of docosahexaenoic acid in neural cell signalling throughout evolution. Prostaglandins Leukot Essent Fatty Acids. 2013;88:5–13. doi: 10.1016/j.plefa.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 3.Lands WEM. Fish,Omega-3 and Human Health. 2nd. AOCS Press; Champaign, IL: 2005. [Google Scholar]
- 4.Salem N, Jr, Litman B, Kim HY, Gawrisch K. Mechanisms of action of docosahexaenoic acid in the nervous system. Lipids. 2001;36:945–959. doi: 10.1007/s11745-001-0805-6. [DOI] [PubMed] [Google Scholar]
- 5.Serhan CN. Novel resolution mechanisms in acute inflammation: to resolve or not? Am J Pathol. 2010;177:1576–1591. doi: 10.2353/ajpath.2010.100322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Majno G, Cotran RS. Current Topics in Inflammation and Infection. In: Kaufman N, editor. International Academy of Pathology Monograph. Vol. 23. Williams & Wilkins; Baltimore: 1982. p. 242. [Google Scholar]
- 7.Dinarello CA. Anti-inflammatory agents: present and future. Cell. 2010;140:935–950. doi: 10.1016/j.cell.2010.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Serhan CN, Savill J. Resolution of inflammation: the beginning programs the end. Nat Immunol. 2005;6:1191–1197. doi: 10.1038/ni1276. [DOI] [PubMed] [Google Scholar]
- 9.Serhan CN, Hong S, Gronert K, Colgan SP, Devchand PR, Mirick G, Moussignac RL. Resolvins: a family of bioactive products of omega-3 fatty acid transformation circuits initiated by aspirin treatment that counter pro-inflammation signals. J Exp Med. 2002;196:1025–1037. doi: 10.1084/jem.20020760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Serhan CN, Clish CB, Brannon J, Colgan SP, Chiang N, Gronert K. Novel functional sets of lipid-derived mediators with antiinflammatory actions generated from omega-3 fatty acids via cyclooxygenase 2-nonsteroidal antiinflammatory drugs and transcellular processing. J Exp Med. 2000;192:1197–1204. doi: 10.1084/jem.192.8.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Samuelsson B. Leukotrienes: mediators of immediate hypersensitivity reactions and inflammation. Science. 1983;220:568–575. doi: 10.1126/science.6301011. [DOI] [PubMed] [Google Scholar]
- 12.Bazan NG, Calandria JM, Serhan CN. Rescue and repair during photoreceptor cell renewal mediated by docosahexaenoic acid-derived neuroprotectin D1. J Lipid Res. 2010;51:2018–2031. doi: 10.1194/jlr.R001131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hong S, Gronert K, Devchand P, Moussignac RL, Serhan CN. Novel docosatrienes and 17S-resolvins generated from docosahexaenoic acid in murine brain, human blood and glial cells autacoids in anti-inflammation. J Biol Chem. 2003;278:14677–14687. doi: 10.1074/jbc.M300218200. [DOI] [PubMed] [Google Scholar]
- 14.Mukherjee PK, Marcheselli VL, Serhan CN, Bazan NG. Neuroprotectin D1: a docosahexaenoic acid-derived docosatriene protects human retinal pigment epithelial cells from oxidative stress. Proc Natl Acad Sci U S A. 2004;101:8491–8496. doi: 10.1073/pnas.0402531101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Majno G, Joris I. Cells, Tissues, and Disease: Principles of General Pathology. 2nd. Oxford University Press; New York: 2004. [Google Scholar]
- 16.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Libby P. Inflammation in atherosclerosis. Nature. 2002;420:868–878. doi: 10.1038/nature01323. [DOI] [PubMed] [Google Scholar]
- 18.Weiner HL, Selkoe DJ. Inflammation and therapeutic vaccination in CNS diseases. Nature. 2002;420:879–884. doi: 10.1038/nature01325. [DOI] [PubMed] [Google Scholar]
- 19.Samuelsson B. Role of basic science in the development of new medicines: examples from the eicosanoid field. J Biol Chem. 2012;287:10070–10080. doi: 10.1074/jbc.X112.351437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nathan C. Points of control in inflammation. Nature. 2002;420:846–852. doi: 10.1038/nature01320. [DOI] [PubMed] [Google Scholar]
- 21.Serhan CN, Chiang N. Novel endogenous small molecules as the checkpoint controllers in inflammation and resolution entrée for resoleomics. Rheum Dis Clin N Am. 2004;30:69–95. doi: 10.1016/S0889-857X(03)00117-0. [DOI] [PubMed] [Google Scholar]
- 22.Levy BD, Clish CB, Schmidt B, Gronert K, Serhan CN. Lipid mediator class switching during acute inflammation: signals in resolution. Nat Immunol. 2001;2:612–619. doi: 10.1038/89759. [DOI] [PubMed] [Google Scholar]
- 23.Samuelsson B, Dahlén SE, Lindgren JÅ, Rouzer CA, Serhan CN. Leukotrienes and lipoxins: structures, biosynthesis, and biological effects. Science. 1987;237:1171–1176. doi: 10.1126/science.2820055. [DOI] [PubMed] [Google Scholar]
- 24.McMahon B, Godson C. Lipoxins: endogenous regulators of inflammation. Am J Physiol Renal Physiol. 2004;286:F189–F201. doi: 10.1152/ajprenal.00224.2003. [DOI] [PubMed] [Google Scholar]
- 25.Serhan CN. Lipoxin biosynthesis and its impact in inflammatory and vascular events. Biochim Biophys Acta. 1994;1212:1–25. doi: 10.1016/0005-2760(94)90185-6. [DOI] [PubMed] [Google Scholar]
- 26.Wallace JL, Fiorucci S. A magic bullet for mucosal protection…and aspirin is the trigger! Trends Pharmacol Sci. 2003;24:323–326. doi: 10.1016/S0165-6147(03)00166-4. [DOI] [PubMed] [Google Scholar]
- 27.Godson C, Mitchell S, Harvey K, Petasis NA, Hogg N, Brady HR. Cutting edge: Lipoxins rapidly stimulate nonphlogistic phagocytosis of apoptotic neutrophils by monocyte-derived macrophages. J Immunol. 2000;164:1663–1667. doi: 10.4049/jimmunol.164.4.1663. [DOI] [PubMed] [Google Scholar]
- 28.Maddox JF, Serhan CN. Lipoxin A4 and B4 are potent stimuli for human monocyte migration and adhesion: selective inactivation by dehydrogenation and reduction. J Exp Med. 1996;183:137–146. doi: 10.1084/jem.183.1.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gilroy DW, Lawrence T, Perretti M, Rossi AG. Inflammatory resolution: new opportunities for drug discovery. Nat Rev Drug Discov. 2004;3:401–416. doi: 10.1038/nrd1383. [DOI] [PubMed] [Google Scholar]
- 30.Serhan CN. A search for endogenous mechanisms of anti-inflammation uncovers novel chemical mediators: missing links to resolution. Histochem Cell Biol. 2004;122:305–321. doi: 10.1007/s00418-004-0695-8. [DOI] [PubMed] [Google Scholar]
- 31.Serhan CN, Gotlinger K, Hong S, Arita M. Resolvins, docosatrienes, and neuroprotectins, novel omega-3-derived mediators, and their aspirin-triggered endogenous epimers: an overview of their protective roles in catabasis. Prostaglandins Other Lipid Mediat. 2004;73:155–172. doi: 10.1016/j.prostaglandins.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 32.Dalli J, Colas RA, Serhan CN. Novel n-3 immunoresolvents: structures and actions. Sci Rep. 2013;3:1940. doi: 10.1038/srep01940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burr GO, Burr MM. A new deficiency disease produced by the rigid exclusion of fat from the diet. J Biol Chem. 1929;82:345–367. [Google Scholar]
- 34.Camuesco D, Galvez J, Nieto A, Comalada M, Rodriguez-Cabezas ME, Concha A, Xaus J, Zarzuelo A. Dietary olive oil supplemented with fish oil, rich in EPA and DHA (n-3) polyunsaturated fatty acids attenuates colonic inflammation in rats with DSS-induced colitis. J Nutr. 2005;135:687–694. doi: 10.1093/jn/135.4.687. [DOI] [PubMed] [Google Scholar]
- 35.Billman GE, Kang JX, Leaf A. Prevention of sudden cardiac death by dietary pure w-3 polyunsaturated fatty acids in dogs. Circulation. 1999;99:2452–2457. doi: 10.1161/01.cir.99.18.2452. [DOI] [PubMed] [Google Scholar]
- 36.Marchioli R, Barzi F, Bomba E, Chieffo C, Di Gregorio D, Di Mascio R, Franzosi MG, Geraci E, Levantesi G, Maggioni AP, Mantini L, Marfisi RM, Mastrogiuseppe G, Mininni N, Nicolosi GL, Santini M, Schweiger C, Tavazzi L, Tognoni G, Tucci C, Valagussa F. Early protection against sudden death by n-3 polyunsaturated fatty acids after myocardial infarction: time-course analysis of the results of the Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico (GISSI)-Prevenzione. Circulation. 2002;105:1897–1903. doi: 10.1161/01.cir.0000014682.14181.f2. [DOI] [PubMed] [Google Scholar]
- 37.Holub DJ, Holub BJ. Omega-3 fatty acids from fish oils and cardiovascular disease. Mol Cell Biochem. 2004;263:217–225. doi: 10.1023/B:MCBI.0000041863.11248.8d. [DOI] [PubMed] [Google Scholar]
- 38.Engler MM, Engler MB, Malloy M, Chiu E, Besio D, Paul S, Stuehlinger M, Morrow JD, Ridker PM, Rifai N, Mietus-Snyder M. Docosahexaenoic acid restores endothelial function in children with hyperlipidemia: results from the EARLY study. Int J Clin Pharmacol Ther. 2004;42:672–679. doi: 10.5414/cpp42672. [DOI] [PubMed] [Google Scholar]
- 39.Lim GP, Calon F, Morihara T, Yang F, Teter B, Ubeda O, Salem N, Jr, Frautschy SA, Cole GM. A diet enriched with the omega-3 fatty acid docosahexaenoic acid reduces amyloid burden in an aged Alzheimer mouse model. J Neurosci. 2005;25:3032–3040. doi: 10.1523/JNEUROSCI.4225-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bazan NG. Supply of n-3 polyunsaturated fatty acids and their significance in the central nervous system. In: Wurtman RJ, Wurtman JJ, editors. Nutrition and the Brain. Vol. 8. Raven Press; New York: 1990. pp. 1–22. [Google Scholar]
- 41.Bazan NG, Birkle DL, Reddy TS. Docosahexaenoic acid (22:6, n-3) is metabolized to lipoxygenase reaction products in the retina. Biochem Biophys Res Commun. 1984;125:741–747. doi: 10.1016/0006-291x(84)90601-6. [DOI] [PubMed] [Google Scholar]
- 42.Sawazaki S, Salem N, Jr, Kim HY. Lipoxygenation of docosahexaenoic acid by the rat pineal body. J Neurochem. 1994;62:2437–2447. doi: 10.1046/j.1471-4159.1994.62062437.x. [DOI] [PubMed] [Google Scholar]
- 43.Bannenberg GL, Chiang N, Ariel A, Arita M, Tjonahen E, Gotlinger KH, Hong S, Serhan CN. Molecular circuits of resolution: formation and actions of resolvins and protectins. J Immunol. 2005;174:4345–4355. doi: 10.4049/jimmunol.174.7.4345. [DOI] [PubMed] [Google Scholar]
- 44.Marcheselli VL, Hong S, Lukiw WJ, Hua Tian X, Gronert K, Musto A, Hardy M, Gimenez JM, Chiang N, Serhan CN, Bazan NG. Novel docosanoids inhibit brain ischemia-reperfusion-mediated leukocyte infiltration and pro-inflammatory gene expression. J Biol Chem. 2003;278:43807–43817. doi: 10.1074/jbc.M305841200. [DOI] [PubMed] [Google Scholar]
- 45.Belayev L, Marcheselli VL, Khoutorova L, Rodriguez de Turco EB, Busto R, Ginsberg MD, Bazan NG. Docosahexaenoic acid complexed to albumin elicits highgrade ischemic neuroprotection. Stroke. 2005;36:118–123. doi: 10.1161/01.STR.0000149620.74770.2e. [DOI] [PubMed] [Google Scholar]
- 46.Gronert K, Maheshwari N, Khan N, Hassan IR, Dunn M, Schwartzman ML. A role for the mouse 12/15-lipoxygenase pathway in promoting epithelial wound healing and host defense. J Biol Chem. 2005;280:15267–15278. doi: 10.1074/jbc.M410638200. [DOI] [PubMed] [Google Scholar]
- 47.Hong S, Tjonahen E, Morgan EL, Yu L, Serhan CN, Rowley AF. Rainbow trout (Oncorhynchus mykiss) brain cells biosynthesize novel docosahexaenoic acidderived resolvins and protectins -- mediator lipidomic analysis. Prostaglandins Other Lipid Mediat. 2005;78:107–116. doi: 10.1016/j.prostaglandins.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 48.Ariel A, Li PL, Wang W, Tang WX, Fredman G, Hong S, Gotlinger KH, Serhan CN. The docosatriene protectin D1 is produced by TH2 skewing and promotes human T cell apoptosis via lipid raft clustering. J Biol Chem. 2005;280:43079–43086. doi: 10.1074/jbc.M509796200. [DOI] [PubMed] [Google Scholar]
- 49.Serhan CN, Fredman G, Yang R, Karamnov S, Belayev LS, Bazan NG, Zhu M, Winkler JW, Petasis NA. Novel proresolving aspirin-triggered DHA pathway. Chem Biol. 2011;18:976–987. doi: 10.1016/j.chembiol.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Serhan CN, Gotlinger K, Hong S, Lu Y, Siegelman J, Baer T, Yang R, Colgan SP, Petasis NA. Anti-inflammatory actions of neuroprotectin D1/protectin D1 and its natural stereoisomers: assignments of dihydroxy-containing docosatrienes. J Immunol. 2006;176:1848–1859. doi: 10.4049/jimmunol.176.3.1848. [DOI] [PubMed] [Google Scholar]
- 51.Sica A, Mantovani A. Macrophage plasticity and polarization: in vivo veritas. J Clin Invest. 2012;122:787–795. doi: 10.1172/JCI59643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gordon S. Targeting a monocyte subset to reduce inflammation. Circ Res. 2012;110:1546–1548. doi: 10.1161/RES.0b013e31825ec26d. [DOI] [PubMed] [Google Scholar]
- 53.Stables MJ, Shah S, Camon EB, Lovering RC, Newson J, Bystrom J, Farrow S, Gilroy DW. Transcriptomic analyses of murine resolution-phase macrophages. Blood. 2011;118:e192–e208. doi: 10.1182/blood-2011-04-345330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Serhan CN, Dalli J, Karamnov S, Choi A, Park CK, Xu ZZ, Ji RR, Zhu M, Petasis NA. Macrophage pro-resolving mediator maresin 1 stimulates tissue regeneration and controls pain. FASEB J. 2012;26:1755–1765. doi: 10.1096/fj.11-201442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Serhan CN, Yang R, Martinod K, Kasuga K, Pillai PS, Porter TF, Oh SF, Spite M. Maresins: novel macrophage mediators with potent anti-inflammatory and proresolving actions. J Exp Med. 2009;206:15–23. doi: 10.1084/jem.20081880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Serhan CN. U.S. Patent 7,585,856 and Application Publication 2004/0116408 A1. Brigham and Women's Hospital; Resolvins: biotemplates for novel therapeutic interventions. 2004
- 57.Chiang N, Fredman G, Bäckhed F, Oh SF, Vickery TW, Schmidt BA, Serhan CN. Infection regulates pro-resolving mediators that lower antibiotic requirements. Nature. 2012;484:524–528. doi: 10.1038/nature11042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yang R. Doctoral thesis. University of Southern California; Los Angeles: 2005. Synthetic study of lipid mediators. [Google Scholar]
- 59.Petasis NA, Yang R, Winkler JW, Zhu M, Uddin J, Bazan NG, Serhan CN. Stereocontrolled total synthesis of neuroprotectin D1 / protectin D1 and its aspirintriggered stereoisomer. Tetrahedron Lett. 2012;53:1695–1698. doi: 10.1016/j.tetlet.2012.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Serhan CN, Samuelsson B. Lipoxins: a new series of eicosanoids (biosynthesis, stereochemistry, and biological activities) Adv Exp Med Biol. 1988;229:1–14. doi: 10.1007/978-1-4757-0937-7_1. [DOI] [PubMed] [Google Scholar]
- 61.Serhan CN, Nicolaou KC, Webber SE, Veale CA, Dahlen SE, Puustinen TJ, Samuelsson B. Lipoxin A. Stereochemistry and biosynthesis. J Biol Chem. 1986;261:16340–16345. [PubMed] [Google Scholar]
- 62.Kuhn H, Brash AR, Wiesner R, Alder L. Lipoxygenase catalyzed oxygenation of hydroxy fatty acids to lipoxins. Adv Exp Med Biol. 1988;229:39–49. doi: 10.1007/978-1-4757-0937-7_4. [DOI] [PubMed] [Google Scholar]
- 63.Gronert K, Clish CB, Romano M, Serhan CN. Transcellular regulation of eicosanoid biosynthesis. In: Lianos EA, editor. Eicosanoid Protocols. Humana Press; Totowa, NJ: 1999. pp. 119–144. [DOI] [PubMed] [Google Scholar]
- 64.Chen P, Fenet B, Michaud S, Tomczyk N, Véricel E, Lagarde M, Guichardant M. Full characterization of PDX, a neuroprotectin/protectin D1 isomer, which inhibits blood platelet aggregation. FEBS Lett. 2009;583:3478–3484. doi: 10.1016/j.febslet.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 65.Maas RL, Turk J, Oates JA, Brash AR. Formation of a novel dihydroxy acid from arachidonic acid by lipoxygenase-catalyzed double oxygenation in rat mononuclear cells and human leukocytes. J Biol Chem. 1982;257:7056–7067. [PubMed] [Google Scholar]
- 66.Serhan CN. On the relationship between leukotriene and lipoxin production by human neutrophils: evidence for differential metabolism of 15-HETE and 5-HETE. Biochim Biophys Acta. 1989;1004:158–168. doi: 10.1016/0005-2760(89)90264-6. [DOI] [PubMed] [Google Scholar]
- 67.White PJ, St-Pierre P, Charbonneau A, Mitchell PL, St-Amand E, Marcotte B, Marette A. Protectin DX alleviates insulin resistance by activating a myokine-liver glucoregulatory axis. Nat Med. 2014;20:664–669. doi: 10.1038/nm.3549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tabas I, Glass CK. Anti-inflammatory therapy in chronic disease: challenges and opportunities. Science. 2013;339:166–172. doi: 10.1126/science.1230720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ariel A, Fredman G, Sun YP, Kantarci A, Van Dyke TE, Luster AD, Serhan CN. Apoptotic neutrophils and T cells sequester chemokines during immune response resolution via modulation of CCR5 expression. Nat Immunol. 2006;7:1209–1216. doi: 10.1038/ni1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Park CK, Lü N, Xu ZZ, Liu T, Serhan CN, Ji RR. Resolving TRPV1 and TNF-α-mediated spinal cord synaptic plasticity and inflammatory pain with neuroprotectin D1. J Neurosci. 2011;31:15072–15085. doi: 10.1523/JNEUROSCI.2443-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Connor KM, SanGiovanni JP, Lofqvist C, Aderman CM, Chen J, Higuchi A, Hong S, Pravda EA, Majchrzak S, Carper D, Hellstrom A, Kang JX, Chew EY, Salem NN, Jr, Serhan CN, Smith LEH. Increased dietary intake of omega-3-polyunsaturated fatty acids reduces pathological retinal angiogenesis. Nat Med. 2007;13:868–873. doi: 10.1038/nm1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Stark DT, Bazan NG. Neuroprotectin D1 induces neuronal survival and downregulation of amyloidogenic processing in Alzheimer's disease cellular models. Mol Neurobiol. 2011;43:131–138. doi: 10.1007/s12035-011-8174-4. [DOI] [PubMed] [Google Scholar]
- 73.Hassan IR, Gronert K. Acute changes in dietary omega-3 and omega-6 polyunsaturated fatty acids have a pronounced impact on survival following ischemic renal injury and formation of renoprotective docosahexaenoic acid-derived protectin D1. J Immunol. 2009;182:3223–3232. doi: 10.4049/jimmunol.0802064. [DOI] [PubMed] [Google Scholar]
- 74.Cortina MS, He J, Li N, Bazan NG, Bazan HE. Neuroprotectin D1 synthesis and corneal nerve regeneration after experimental surgery and treatment with PEDF plus DHA. Invest Ophthalmol Vis Sci. 2010;51:804–810. doi: 10.1167/iovs.09-3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yanes O, Clark J, Wong DM, Patti GG, Sánchez-Ruiz A, Benton HP, Trauger SA, Desponts C, Ding S, Siuzdak G. Metabolic oxidation regulates embryonic stem cell differentiation. Nat Chem Biol. 2010;6:411–417. doi: 10.1038/nchembio.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Schwab JM, Chiang N, Arita M, Serhan CN. Resolvin E1 and protectin D1 activate inflammation-resolution programmes. Nature. 2007;447:869–874. doi: 10.1038/nature05877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Marcheselli VL, Mukherjee PK, Arita M, Hong S, Antony R, Sheets K, Petasis N, Serhan CN, Bazan NG. Neuroprotectin D1/protectin D1 stereoselective and specific binding with human retinal pigment epithelial cells and neutrophils. Prostaglandins Leukot Essent Fatty Acids. 2010;82:27–34. doi: 10.1016/j.plefa.2009.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Serhan CN, Chiang N. Resolution phase lipid mediators of inflammation: agonists of resolution. Curr Opin Pharmacol. 2013;13:632–640. doi: 10.1016/j.coph.2013.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Whelan J. Arachidonic acid cascade: the 5-lipoxygenase pathway, in: Department of Nutrition. Pennsylvania State University; University Park: 1988. [Google Scholar]
- 80.Whelan J, Reddanna P, Nikolaev V, Hildenbrandt GR, Reddy TS. Biological Oxidation Systems. Vol. 2. Academic Press; San Diego: 1990. The unique characteristics of the purified 5-lipoxygenase from potato tubers and the proposed mechanism of formation of leukotrienes and lipoxins; pp. 765–778. [Google Scholar]
- 81.Butovich IA, Hamberg M, Rådmark O. Novel oxylipins formed from docosahexaenoic acid by potato lipoxygenase--10(S)-hydroxydocosahexaenoic acid and 10,20-dihydroxydocosahexaenoic acid. Lipids. 2005;40:249–257. doi: 10.1007/s11745-005-1379-z. [DOI] [PubMed] [Google Scholar]
- 82.Kalish BT, Le HD, Fitzgerald JM, Wang S, Seamon K, Gura KM, Gronert K, Puder M. Intravenous fish oil lipid emulsion promotes a shift toward anti-inflammatory proresolving lipid mediators. Am J Physiol Gastrointest Liver Physiol. 2013;305:G818–828. doi: 10.1152/ajpgi.00106.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gilroy DW, Colville-Nash PR, Willis D, Chivers J, Paul-Clark MJ, Willoughby DA. Inducible cycloxygenase may have anti-inflammatory properties. Nat Med. 1999;5:698–701. doi: 10.1038/9550. [DOI] [PubMed] [Google Scholar]
- 84.Serhan CN. Resolution phases of inflammation: novel endogenous antiinflammatory and pro-resolving lipid mediators and pathways. Annu Rev Immunol. 2007;25:101–137. doi: 10.1146/annurev.immunol.25.022106.141647. [DOI] [PubMed] [Google Scholar]
- 85.Gilroy DW, Perretti M. Aspirin and steroids: new mechanistic findings and avenues for drug discovery. Curr Op Pharmacol. 2005;5:405–411. doi: 10.1016/j.coph.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 86.Clària J, Serhan CN. Aspirin triggers previously undescribed bioactive eicosanoids by human endothelial cell-leukocyte interactions. Proc Natl Acad Sci U S A. 1995;92:9475–9479. doi: 10.1073/pnas.92.21.9475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Samuelsson B. Les Prix Nobel: Nobel Prizes, Presentations, Biographies and Lectures. Almqvist & Wiksell; Stockholm: 1982. From studies of biochemical mechanisms to novel biological mediators: prostaglandin endoperoxides, thromboxanes and leukotrienes; pp. 153–174. [Google Scholar]
- 88.Vane JR. Les Prix Nobel: Nobel Prizes, Presentations, Biographies and Lectures. Almqvist & Wiksell; Stockholm: 1982. Adventures and excursions in bioassay: the stepping stones to prostacyclin; pp. 181–206. [Google Scholar]
- 89.Rowlinson SW, Crews BC, Goodwin DC, Schneider C, Gierse JK, Marnett LJ. Spatial requirements for 15-(R)-hydroxy-5Z,8Z,11Z,13E-eicosatetraenoic acid synthesis within the cyclooxygenase active site of murine COX-2. J Biol Chem. 2000;275:6586–6591. doi: 10.1074/jbc.275.9.6586. [DOI] [PubMed] [Google Scholar]
- 90.Chiang N, Bermudez EA, Ridker PM, Hurwitz S, Serhan CN. Aspirin triggers anti-inflammatory 15-epi-lipoxin A4 and inhibits thromboxane in a randomized human trial. Proc Natl Acad Sci U S A. 2004;101:15178–15183. doi: 10.1073/pnas.0405445101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Serhan CN, Fiore S, Brezinski DA, Lynch S. Lipoxin A4 metabolism by differentiated HL-60 cells and human monocytes: conversion to novel 15-oxo and dihydro products. Biochemistry (Mosc) 1993;32:6313–6319. doi: 10.1021/bi00076a002. [DOI] [PubMed] [Google Scholar]
- 92.Morris T, Stables M, Hobbs A, de Souza P, Colville-Nash P, Warner T, Newson J, Bellingan G, Gilroy DW. Effects of low-dose aspirin on acute inflammatory responses in humans. J Immunol. 2009;183:2089–2096. doi: 10.4049/jimmunol.0900477. [DOI] [PubMed] [Google Scholar]
- 93.Tsikitis VL, Morin NA, Harrington EO, Albina JE, Reichner JS. The lectinlike domain of complement receptor 3 protects endothelial barrier function from activated neutrophils. J Immunol. 2004;173:1284–1291. doi: 10.4049/jimmunol.173.2.1284. [DOI] [PubMed] [Google Scholar]
- 94.Sun YP, Oh SF, Uddin J, Yang R, Gotlinger K, Campbell E, Colgan SP, Petasis NA, Serhan CN. Resolvin D1 and its aspirin-triggered 17R epimer: stereochemical assignments, anti-inflammatory properties and enzymatic inactivation. J Biol Chem. 2007;282:9323–9334. doi: 10.1074/jbc.M609212200. [DOI] [PubMed] [Google Scholar]
- 95.Spite M, Norling LV, Summers L, Yang R, Cooper D, Petasis NA, Flower RJ, Perretti M, Serhan CN. Resolvin D2 is a potent regulator of leukocytes and controls microbial sepsis. Nature. 2009;461:1287–1291. doi: 10.1038/nature08541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Serhan CN, Petasis NA. Resolvins and protectins in inflammation-resolution. Chem Rev. 2011;111:5922–5943. doi: 10.1021/cr100396c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Borgeat P, Samuelsson B. Arachidonic acid metabolism in polymorphonuclear leukocytes: Effects of ionophore A23187. Proc Natl Acad Sci USA. 1979;76:2148–2152. doi: 10.1073/pnas.76.5.2148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Carey FA, Sundberg RJ. Advanced Organic Chemistry, Part A: Structure and Mechanisms. Springer Science; New York: 2007. [Google Scholar]
- 99.Lewis RA, Goetzl EJ, Drazen JM, Soter NA, Austen KF, Corey EJ. Functional characterization of synthetic leukotriene B and its stereochemical isomers. J Exp Med. 1981;154:1243–1248. doi: 10.1084/jem.154.4.1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Antoni C, Braun J. Side effects of anti-TNF therapy: current knowledge. Clin Exp Rheumatol. 2002;20:S152–157. [PubMed] [Google Scholar]
- 101.Lin J, Ziring D, Desai S, Kim S, Wong M, Korin Y, Braun J, Reed E, Gjertson D, Singh RR. TNFalpha blockade in human diseases: an overview of efficacy and safety. Clin Immunol. 2008;126:13–30. doi: 10.1016/j.clim.2007.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Shimizu T, Rådmark O, Samuelsson B. Enzyme with dual lipoxygenase activities catalyzes leukotriene A4 synthesis from arachidonic acid. Proc Natl Acad Sci USA. 1984;81:689–693. doi: 10.1073/pnas.81.3.689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wetterholm A, Haeggström JZ, Samuelsson B, Yuan W, Munoz B, Wong CH. Potent and selective inhibitors of leukotriene A4 hydrolase: Effects on purified enzyme and human polymorphonuclear leukocytes. J Pharmacol Exp Ther. 1995;275:31–37. [PubMed] [Google Scholar]
- 104.Rothwell PM, Wilson M, Elwin CE, Norrving B, Algra A, Warlow CP, Meade TW. Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet. 2010;376:1713–1714. doi: 10.1016/S0140-6736(10)61543-7. [DOI] [PubMed] [Google Scholar]
- 105.Skulas-Ray AC, Kris-Etherton PM, Harris WS, Vanden Heuvel JP, Wagner PR, West SG. Dose-response effects of omega-3 fatty acids on triglycerides, inflammation, and endothelial function in healthy persons with moderate hypertriglyceridemia. Am J Clin Nutr. 2011;93:243–252. doi: 10.3945/ajcn.110.003871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.El-Sharkawy H, Aboelsaad N, Eliwa M, Darweesh M, Alshahat M, Kantarci A, Hasturk H, Van Dyke TE. Adjunctive treatment of chronic periodontitis with daily dietary supplementation with omega-3 fatty acids and low-dose aspirin. J Periodontol. 2010;81:1635–1643. doi: 10.1902/jop.2010.090628. [DOI] [PubMed] [Google Scholar]
- 107.Van Dyke TE, Serhan CN. A novel approach to resolving inflammation. Sci Am Oral and Whole Body Health. 2006:42–45. [Google Scholar]
- 108.Ariel A, Serhan CN. New Lives Given by Cell Death: Macrophage Differentiation Following Their Encounter with Apoptotic Leukocytes during the Resolution of Inflammation. Front Immunol. 2012;3:4. doi: 10.3389/fimmu.2012.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Stables MJ, Shah S, Camon EB, Lovering RC, Newson J, Bystrom J, Farrow S, Gilroy DW. Transcriptomic analyses of murine resolution-phase macrophages. Blood. 2011;118:e192–208. doi: 10.1182/blood-2011-04-345330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhang MJ, Spite M. Resolvins: anti-inflammatory and proresolving mediators derived from omega-3 polyunsaturated fatty acids. Annu Rev Nutr. 2012;32:203–227. doi: 10.1146/annurev-nutr-071811-150726. [DOI] [PubMed] [Google Scholar]
- 111.Serhan CN, Yang R, Martinod K, Kasuga K, Pillai PS, Porter TF, Oh SF, Spite M. Maresins: novel macrophage mediators with potent antiinflammatory and proresolving actions. J Exp Med. 2009;206:15–23. doi: 10.1084/jem.20081880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Dalli J, Serhan CN. Specific lipid mediator signatures of human phagocytes: microparticles stimulate macrophage efferocytosis and pro-resolving mediators. Blood. 2012;120:e60–72. doi: 10.1182/blood-2012-04-423525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Giera M, Ioan-Facsinay A, Toes R, Gao F, Dalli J, Deelder AM, Serhan CN, Mayboroda OA. Lipid and lipid mediator profiling of human synovial fluid in rheumatoid arthritis patients by means of LC-MS/MS. Biochim Biophys Acta. 2012;1821:1415–1424. doi: 10.1016/j.bbalip.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Serhan CN, Dalli J, Karamnov S, Choi A, Park CK, Xu ZZ, Ji RR, Zhu M, Petasis NA. Macrophage proresolving mediator maresin 1 stimulates tissue regeneration and controls pain. FASEB J. 2012;26:1755–1765. doi: 10.1096/fj.11-201442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Dalli J, Zhu M, Vlasenko NA, Deng B, Haeggstrom JZ, Petasis NA, Serhan CN. The novel 13S,14S-epoxy-maresin is converted by human macrophages to maresin1 (MaR1), inhibits leukotriene A4 hydrolase (LTA4H), and shifts macrophage phenotype. FASEB J. 2013;27:2573–2583. doi: 10.1096/fj.13-227728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Deng B, Wang CW, Arnardottir HH, Li Y, Cheng CY, Dalli J, Serhan CN. Maresin biosynthesis and identification of maresin 2, a new anti-inflammatory and proresolving mediator from human macrophages. PLoS One. 2014;9:e102362. doi: 10.1371/journal.pone.0102362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ingersoll MA, Platt AM, Potteaux S, Randolph GJ. Monocyte trafficking in acute and chronic inflammation. Trends Immunol. 2011;32:470–477. doi: 10.1016/j.it.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hellmann J, Tang Y, Kosuri M, Bhatnagar A, Spite M. Resolvin D1 decreases adipose tissue macrophage accumulation and improves insulin sensitivity in obesediabetic mice. FASEB J. 2011;25:2399–2407. doi: 10.1096/fj.10-178657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Titos E, Rius B, Gonzalez-Periz A, Lopez-Vicario C, Moran-Salvador E, Martinez-Clemente M, Arroyo V, Claria J. Resolvin D1 and its precursor docosahexaenoic acid promote resolution of adipose tissue inflammation by eliciting macrophage polarization toward an M2-like phenotype. J Immunol. 2011;187:5408–5418. doi: 10.4049/jimmunol.1100225. [DOI] [PubMed] [Google Scholar]
- 120.Lu Y, Tian H, Hong S. Novel 14,21-dihydroxy-docosahexaenoic acids: structures, formation pathways, and enhancement of wound healing. J Lipid Res. 2010;51:923–932. doi: 10.1194/jlr.M000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tian H, Lu Y, Shah SP, Wang Q, Hong S. 14S,21R-dihydroxydocosahexaenoic acid treatment enhances mesenchymal stem cell amelioration of renal ischemia/reperfusion injury. Stem Cells Dev. 2012;21:1187–1199. doi: 10.1089/scd.2011.0220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Tian H, Lu Y, Shah SP, Hong S. 14S, 21R-dihydroxydocosahexaenoic acid remedies impaired healing and mesenchymal stem cell functions in diabetic wounds. J Biol Chem. 2011;286:4443–4453. doi: 10.1074/jbc.M110.100388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Samuelsson B. Role of basic science in the development of new medicines: examples from the eicosanoid field. J Biol Chem. 2012;287:10070–10080. doi: 10.1074/jbc.X112.351437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Shimizu T. Lipid mediators in health and disease: enzymes and receptors as therapeutic targets for the regulation of immunity and inflammation. Annu Rev Pharmacol Toxicol. 2009;49:123–150. doi: 10.1146/annurev.pharmtox.011008.145616. [DOI] [PubMed] [Google Scholar]
- 125.Spite M, Norling LV, Summers L, Yang R, Cooper D, Petasis NA, Flower RJ, Perretti M, Serhan CN. Resolvin D2 is a potent regulator of leukocytes and controls microbial sepsis. Nature. 2009;461:1287–1291. doi: 10.1038/nature08541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chiang N, Fredman G, Backhed F, Oh SF, Vickery T, Schmidt BA, Serhan CN. Infection regulates pro-resolving mediators that lower antibiotic requirements. Nature. 2012;484:524–528. doi: 10.1038/nature11042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Rudberg PC, Tholander F, Thunnissen MMGM, Haeggström JZ. Leukotriene A4 hydrolase/aminopeptidase: Glutamate 271 is a catalytic residue with specific roles in two distinct enzyme mechanisms. J Biol Chem. 2002;277:1398–1404. doi: 10.1074/jbc.M106577200. [DOI] [PubMed] [Google Scholar]
- 128.Oh SF, Pillai PS, Recchiuti A, Yang R, Serhan CN. Pro-resolving actions and stereoselective biosynthesis of 18S E-series resolvins in human leukocytes and murine inflammation. J Clin Invest. 2011;121:569–581. doi: 10.1172/JCI42545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Serhan CN, Ward PA, Gilroy DW. Fundamentals of inflammation. Cambridge University Press; Cambridge: 2010. p. 473. [Google Scholar]
- 130.Yanes O, Clark J, Wong DM, Patti GJ, Sanchez-Ruiz A, Benton HP, Trauger SA, Desponts C, Ding S, Siuzdak G. Metabolic oxidation regulates embryonic stem cell differentiation. Nat Chem Biol. 2010;6:411–417. doi: 10.1038/nchembio.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Mueller MJ, Wetterholm A, Blomster M, Jornvall H, Samuelsson B, Haeggstrom JZ. Leukotriene A4 hydrolase: mapping of a henicosapeptide involved in mechanism-based inactivation. Proc Natl Acad Sci U S A. 1995;92:8383–8387. doi: 10.1073/pnas.92.18.8383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Serhan CN, Jain A, Marleau S, Clish C, Kantarci A, Behbehani B, Colgan SP, Stahl GL, Merched A, Petasis NA, Chan L, Van Dyke TE. Reduced inflammation and tissue damage in transgenic rabbits overexpressing 15-lipoxygenase and endogenous anti-inflammatory lipid mediators. J Immunol. 2003;171:6856–6865. doi: 10.4049/jimmunol.171.12.6856. [DOI] [PubMed] [Google Scholar]
- 133.Merched A, Ko K, Gotlinger KH, Serhan CN, Chan L. Atherosclerosis: Evidence for impairment of resolution of vascular inflammation governed by specific lipid mediators. FASEB J. 2008;22:3595–3606. doi: 10.1096/fj.08-112201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Chiang N, Shinohara M, Dalli J, Mirakaj V, Kibi M, Choi AMK, Serhan CN. Inhaled carbon monoxide accelerates resolution of inflammation via unique pro-resolving mediator--heme oxygenase-1 circuits. J Immunol. 2013;190:6378–6388. doi: 10.4049/jimmunol.1202969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Calandria JM, Marcheselli VL, Mukherjee PK, Uddin J, Winkler JW, Petasis NA, Bazan NG. Selective survival rescue in 15-lipoxygenase-1-deficient retinal pigment epithelial cells by the novel docosahexaenoic acid-derived mediator, neuroprotectin D1. J Biol Chem. 2009;284:17877–17882. doi: 10.1074/jbc.M109.003988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Chen P, Vericel E, Lagarde M, Guichardant M. Poxytrins, a class of oxygenated products from polyunsaturated fatty acids, potently inhibit blood platelet aggregation. FASEB J. 2011;25:382–388. doi: 10.1096/fj.10-161836. [DOI] [PubMed] [Google Scholar]
- 137.Levy BD, Kohli P, Gotlinger K, Haworth O, Hong S, Kazani S, Israel E, Haley KJ, Serhan CN. Protectin D1 is generated in asthma and dampens airway inflammation and hyperresponsiveness. J Immunol. 2007;178:496–502. doi: 10.4049/jimmunol.178.1.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Koltsida O, Karamnov S, Pyrillou K, Vickery T, Chairakaki AD, Tamvakopoulos C, Sideras P, Serhan CN, Andreakos E. Toll-like receptor 7 stimulates production of specialized pro-resolving lipid mediators and promotes resolution of airway inflammation. EMBO Mol Med. 2013;5:762–775. doi: 10.1002/emmm.201201891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Miyata J, Fukunaga K, Iwamoto R, Isobe Y, Niimi K, Takamiya R, Takihara T, Tomomatsu K, Suzuki Y, Oguma T, Sayama K, Arai H, Betsuyaku T, Arita M, Asano K. Dysregulated synthesis of protectin D1 in eosinophils from patients with severe asthma. J Allergy Clin Immunol. 2013;131:353–360. doi: 10.1016/j.jaci.2012.07.048. [DOI] [PubMed] [Google Scholar]
- 140.Yamada T, Tani Y, Nakanishi H, Taguchi R, Arita M, Arai H. Eosinophils promote resolution of acute periotonitis by producing proresolving mediators in mice. FASEB J. 2011;25:561–568. doi: 10.1096/fj.10-170027. [DOI] [PubMed] [Google Scholar]
- 141.Duffield JS, Hong S, Vaidya V, Lu Y, Fredman G, Serhan CN, Bonventre JV. Resolvin D series and protectin D1 mitigate acute kidney injury. J Immunol. 2006;177:5902–5911. doi: 10.4049/jimmunol.177.9.5902. [DOI] [PubMed] [Google Scholar]
- 142.Lukiw WJ, Cui JG, Marcheselli VL, Bodker M, Botkjaer A, Gotlinger K, Serhan CN, Bazan NG. A role for docosahexaenoic acid-derived neuroprotectin D1 in neural cell survival and Alzheimer disease. J Clin Invest. 2005;115:2774–2783. doi: 10.1172/JCI25420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.González-Périz A, Planagumà A, Gronert K, Miquel R, López-Parra M, Titos E, Horrillo R, Ferré N, Deulofeu R, Arroyo V, Rodés J, Clària J. Docosahexanenoic acid (DHA) blunts liver injury by conversion to protective lipid mediators: protectin D1 and 17S-hydroxy-DHA. FASEB J. 2006;20:2537–2539. doi: 10.1096/fj.06-6250fje. [DOI] [PubMed] [Google Scholar]
- 144.Cortina MS, He J, Russ T, Bazan NG, Bazan HE. Neuroprotectin D1 restores corneal nerve integrity and function after damage from experimental surgery. Invest Ophthalmol Vis Sci. 2013;54:4109–4116. doi: 10.1167/iovs.13-12075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Blaho VA, Buczynski MW, Brown CR, Dennis EA. Lipidomic analysis of dynamic eicosanoid responses during the induction and resolution of Lyme arthritis. J Biol Chem. 2009;284:21599–21612. doi: 10.1074/jbc.M109.003822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Qin Q, Patil KA, Gronert K, Sharma SC. Neuroprotectin D1 inhibits retinal ganglion cell death following axotomy, Prostaglandins Leukot. Essent Fatty Acids. 2008;79:201–207. doi: 10.1016/j.plefa.2008.09.022. [DOI] [PubMed] [Google Scholar]
- 147.González-Périz A, Horrillo R, Ferré N, Gronert K, Dong B, Morán-Salvador E, Titos E, Martínez-Clemente M, López-Parra M, Arroyo V, Clària J. Obesity-induced insulin resistance and hepatic steatosis are alleviated by omega-3 fatty acids: a role for resolvins and protectins. FASEB J. 2009;23:1946–1957. doi: 10.1096/fj.08-125674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Xu ZZ, Liu XJ, Berta T, Park CK, Lu N, Serhan CN, Ji RR. Neuroprotectin/protectin D1 protects against neuropathic pain in mice after nerve trauma. Ann Neurol. 2013;74:490–495. doi: 10.1002/ana.23928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Rajasagi NK, Reddy PB, Mulik S, Gjorstrup P, Rouse BT. Neuroprotectin D1 reduces the severity of herpes simplex virus-induced corneal immunopathology. Invest Ophthalmol Vis Sci. 2013;54:6269–6279. doi: 10.1167/iovs.13-12152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Musto AE, Gjorstrup P, Bazan NG. The omega-3 fatty acid-derived neuroprotectin D1 limits hippocampal hyperexcitability and seizure susceptibility in kindling epileptogenesis. Epilepsia. 2011;52:1601–1608. doi: 10.1111/j.1528-1167.2011.03081.x. [DOI] [PubMed] [Google Scholar]
- 151.Hudert CA, Weylandt KH, Wang J, Lu Y, Hong S, Dignass A, Serhan CN, Kang JX. Transgenic mice rich in endogenous n-3 fatty acids are protected from colitis. Proc Natl Acad Sci U S A. 2006;103:11276–11281. doi: 10.1073/pnas.0601280103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Antony R, Lukiw WJ, Bazan NG. Neuroprotectin D1 induces dephosphorylation of Bcl-xL in a PP2A-dependent manner during oxidative stress and promotes retinal pigment epithelial cell survival. J Biol Chem. 2010;285:18301–18308. doi: 10.1074/jbc.M109.095232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Morita M, Kuba K, Ichikawa A, Nakayama M, Katahira J, Iwamoto R, Watanebe T, Sakabe S, Daidoji T, Nakamura S, Kadowaki A, Ohto T, Nakanishi H, Taguchi R, Nakaya T, Murakami M, Yoneda Y, Arai H, Kawaoka Y, Penninger JM, Arita M, Imai Y. The lipid mediator protectin D1 inhibits influenza virus replication and improves severe influenza. Cell. 2013;153:112–125. doi: 10.1016/j.cell.2013.02.027. [DOI] [PubMed] [Google Scholar]
- 154.Li X, Li C, Liang W, Bi Y, Chen M, Dong S. Protectin D1 promotes resolution of inflammation in a murine model of lipopolysaccharide-induced acute lung injury via enhancing neutrophil apoptosis. Chin Med J (Engl) 2014;127:810–814. [PubMed] [Google Scholar]
- 155.Bazan NG, Eady TN, Khoutorova L, Atkins KD, Hong S, Lu Y, Zhang C, Jun B, Obenaus A, Fredman G, Zhu M, Winkler JW, Petasis NA, Serhan CN, Belayev L. Novel aspirin-triggered neuroprotectin D1 attenuates cerebral ischemic injury after experimental stroke. Exp Neurol. 2012;236:122–130. doi: 10.1016/j.expneurol.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Marcon R, Bento AF, Dutra RC, Bicca MA, Leite DF, Calixto JB. Maresin 1, a proresolving lipid mediator derived from omega-3 polyunsaturated fatty acids, exerts protective actions in murine models of colitis. J Immunol. 2013;191:4288–4298. doi: 10.4049/jimmunol.1202743. [DOI] [PubMed] [Google Scholar]
- 157.Li Y, Dalli J, Chiang N, Baron RM, Quintana C, Serhan CN. Plasticity of leukocytic exudates in resolving acute inflammation is regulated by microRNA and proresolving mediators. Immunity. 2013;39:885–898. doi: 10.1016/j.immuni.2013.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Nordgren TM, Heires AJ, Wyatt TA, Poole JA, Levan TD, Cerutis DR, Romberger DJ. Maresin-1 reduces the pro-inflammatory response of bronchial epithelial cells to organic dust. Respir Res. 2013;14:51. doi: 10.1186/1465-9921-14-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Biteman B, Hassan IR, Walker E, Leedom AJ, Dunn M, Seta F, Laniado-Schwartzman M, Gronert K. Interdependence of lipoxin A4 and heme-oxygenase in counter-regulating inflammation during corneal wound healing. FASEB J. 2007;21:2257–2266. doi: 10.1096/fj.06-7918com. [DOI] [PubMed] [Google Scholar]
- 160.Kronke G, Katzenbeisser J, Uderhardt S, Zaiss MM, Scholtysek C, Schabbauer G, Zarbock A, Koenders MI, Axmann R, Zwerina J, Baenckler HW, van den Berg W, Voll RE, Kuhn H, Joosten LA, Schett G. 12/15-lipoxygenase counteracts inflammation and tissue damage in arthritis. J Immunol. 2009;183:3383–3389. doi: 10.4049/jimmunol.0900327. [DOI] [PubMed] [Google Scholar]
- 161.Chan MMY, Moore AR. Resolution of inflammation in murine autoimmune arthritis is disrupted by cyclooxygenase-2 inhibition and restored by prostaglandin E2-mediated lipoxin A4 production. J Immunol. 2010;184:6418–6426. doi: 10.4049/jimmunol.0903816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Leedom AJ, Sullivan AB, Dong B, Lau D, Gronert K. Endogenous LXA4 circuits are determinants of pathological angiogenesis in response to chronic injury. Am J Pathol. 2010;176:74–84. doi: 10.2353/ajpath.2010.090678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kronke G, Reich N, Scholtysek C, Akhmetshina A, Uderhardt S, Zerr P, Palumbo K, Lang V, Dees C, Distler O, Schett G, Distler JH. The 12/15-lipoxygenase pathway counteracts fibroblast activation and experimental fibrosis. Ann Rheum Dis. 2012;71:1081–1087. doi: 10.1136/annrheumdis-2011-200745. [DOI] [PubMed] [Google Scholar]
- 164.Tomio K, Kawana K, Taguchi A, Isobe Y, Iwamoto R, Yamashita A, Kojima S, Mori M, Nagamatsu T, Arimoto T, Oda K, Osuga Y, Taketani Y, Kang JX, Arai H, Arita M, Kozuma S, Fujii T. Omega-3 polyunsaturated Fatty acids suppress the cystic lesion formation of peritoneal endometriosis in transgenic mouse models. PLoS One. 2013;8:e73085. doi: 10.1371/journal.pone.0073085. [DOI] [PMC free article] [PubMed] [Google Scholar]


