Abstract
We describe a case of Candida esophagitis in a human immunodeficiency virus elite controller with a preserved CD4 count, a population in which opportunistic infections are almost never seen. The patient has hepatitis C virus coinfection and compensated cirrhosis, suggesting a possible multifactorial etiology of immune dysregulation.
Keywords: Candida esophagitis, cirrhosis, elite controller, hepatitis C, HIV
Elite controllers are patients who control human immunodeficiency virus-1 replication to levels below the limit of detection without antiretroviral therapy. They normally maintain stable CD4 counts and do not develop signs of immunosuppression. We report here a case of an elite controller with cirrhosis who developed asymptomatic Candida esophagitis.
CASE REPORT
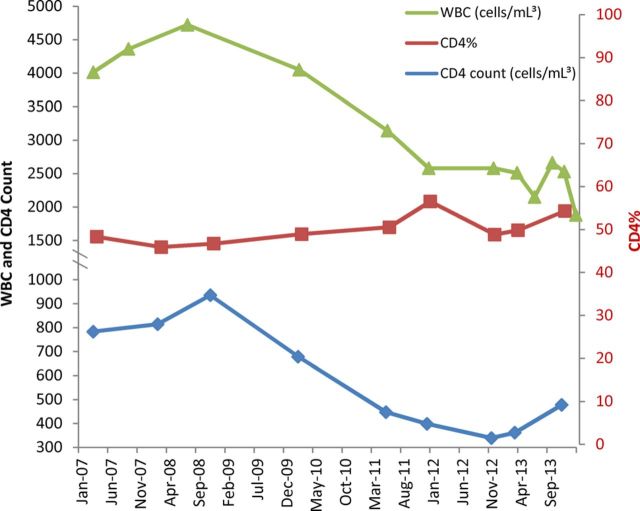
Less than 1% of patients infected with human immunodeficiency virus (HIV)-1 will maintain undetectable viral loads without antiretroviral therapy. These patients are referred to as elite suppressors or elite controllers (ECs) [1]. Although some ECs have declining CD4+ T cell counts [2–4], opportunistic infections are almost never seen in these patients. Patient ES4 is a previously described EC [5] who is coinfected with hepatitis C virus and has developed cirrhosis [6]. His CD4 count remained stable over the first 12 years of infection from 1996 to 2008, with an absolute count between 700–1000 cells/mL3. Since 2008, his absolute CD4 count has declined, with a nadir of 339. However, this has been coincident with a drop in his absolute white blood cell count, likely attributable to his progressive liver disease. During this time, his CD4 percentage has remained unchanged, between 46% and 54%, and his viral load has remained below the limit of detection of clinical assays, with the exception of a one-time blip to a level of 89 copies/mL3 in November 2012. Figure 1 shows his CD4 count, CD4 percentage, and white blood cell count since 2008. As part of the evaluation of his cirrhosis, an esophagogastroduodenoscopy was obtained in 2014 to screen for varices, and the patient was found to have white plaques throughout his esophagus. Biopsies were obtained, and the diagnosis of candida esophagitis was confirmed by cytopathology. It is interesting to note that the patient denied having symptoms of dysphagia or odynophagia.
Figure 1.
The patient's absolute CD4 count, CD4 percentage (CD4%), and white blood cell (WBC) count since 2008. Absolute CD4 count and WBC count are plotted on the primary vertical axis (left) in cells/mL3, and the CD4% is plotted on the secondary vertical axis (right). The viral load is not plotted, but it was undetectable except for a one-time blip of 89 copies/mL3 in November 2012.
DISCUSSION
Human immunodeficiency virus-1 eradication is a major focus of current research [7]. Elite controllers represent a model of a functional cure of this infection; although these patients have not eradicated the virus [5], they are able to control viral replication. However, it seems that elite control is not a perfect model for a functional cure, and this particular case is interesting for several reasons. First, although several studies have documented declining CD4+ T cell counts [2–4], only 2 cases of opportunistic infections (both Kaposi sarcoma) have been described in ECs [2, 8]. Second, even in cases of progressive HIV-1 disease, Candida esophagitis is usually not seen in patients with CD4+ T cell counts over 200 cells/mL3, and this patient had a CD4 count of 477 cells/mL3 (54%) at the time of the Candida diagnosis. Third, we have isolated fully replication competent virus from this patient in a prior study [5]; it is remarkable that his immune system is capable of controlling a pathogenic HIV-1 isolate, yet remains susceptible to an opportunistic infection.
The contribution of his liver disease is unclear. The literature is conflicting regarding whether cirrhosis is an independent risk factor for developing Candida esophagitis [9, 10]. His cirrhosis remains compensated, without clinically evident ascites or hepatic encephalopathy and an overall Model for End-Stage Liver Disease score of 8. There were no other known predisposing risk factors for the development of Candida esophagitis, such as corticosteroids, proton-pump inhibitors, recent antibiotics, cancer, or diabetes.
This case suggests a multifactorial etiology of immune dysregulation. Individually, neither HIV EC status nor cirrhosis has been shown to predispose to opportunistic infections. Perhaps combined, these were adequate risk factors. This may be a reason to treat ECs who have declining CD4+ T-cell counts or other potential risk factors. Furthermore, recent studies have suggested that some EC may have higher levels of inflammation [11, 12] and an increased rate of hospitalization due to cardiovascular disease [8], and treatment may lead to modest CD4+ T-cell gains [3, 13] or a decrease in immune activation [14, 15]. However, more studies are needed to determine whether asymptomatic ECs who maintain high CD4+ T cell counts will derive long-term benefit from antiretroviral therapy.
Acknowledgments
Financial support. This work was supported by the National Institute of Allergy and Infectious Diseases at the National Institutes of Health (grant R56AI080328-05A1).
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1.Blankson JN. Control of HIV-1 replication in elite suppressors. Discov Med. 2010;9:261–6. [PubMed] [Google Scholar]
- 2.Hunt PW, Brenchley J, Sinclair E, et al. Relationship between T cell activation and CD4+ T cell count in HIV-seropositive individuals with undetectable plasma HIV RNA levels in the absence of therapy. J Infect Dis. 2008;197:126–33. doi: 10.1086/524143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sedaghat AR, Rastegar DA, O'Connell KA, et al. T cell dynamics and the response to HAART in a cohort of HIV-1-infected elite suppressors. Clin Infect Dis. 2009;49:1763–6. doi: 10.1086/648081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pereyra F, Palmer S, Miura T, et al. Persistent low-level viremia in HIV-1 elite controllers and relationship to immunologic parameters. J Infect Dis. 2009;200:984–90. doi: 10.1086/605446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blankson JN, Bailey JR, Thayil S, et al. Isolation and characterization of replication-competent human immunodeficiency virus type 1 from a subset of elite suppressors. J Virol. 2007;81:2508–18. doi: 10.1128/JVI.02165-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salgado M, Kirk GD, Cox A, et al. Protective interleukin-28B genotype affects hepatitis C virus clearance, but does not contribute to HIV-1 control in a cohort of African-American elite controllers/suppressors. AIDS. 2011;25:385–7. doi: 10.1097/QAD.0b013e328341b86a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deeks SG, Autran B, Berkhout B, et al. Towards an HIV cure: a global scientific strategy. Nat Rev Immunol. 2012;12:607–14. doi: 10.1038/nri3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crowell TA, Gebo KA, Blankson JN, et al. Elite controllers are hospitalized more often than persons with medically controlled HIV. J Infect Dis. 2014 doi: 10.1093/infdis/jiu809. doi:10.1093/infdis/jiu809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ortuno Cortes JA, Tovar Martinez A, Ruiz Riquelme J, Garcia Garcia A. Esophageal candidiasis in HIV-negative patients. Rev Esp Enferm Dig. 1997;89:503–10. [PubMed] [Google Scholar]
- 10.Mimidis K, Papadopoulos V, Margaritis V, et al. Predisposing factors and clinical symptoms in HIV-negative patients with candida oesophagitis: are they always present? Int J Clin Pract. 2005;59:210–3. doi: 10.1111/j.1742-1241.2004.00249.x. [DOI] [PubMed] [Google Scholar]
- 11.Krishnan S, Wilson EM, Sheikh V, et al. Evidence for innate immune system activation in HIV type 1-infected elite controllers. J Infect Dis. 2014;209:931–9. doi: 10.1093/infdis/jit581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noel N, Boufassa F, Lecuroux C, et al. Elevated IP10 levels are associated with immune activation and low CD4(+) T-cell counts in HIV controller patients. AIDS. 2014;28:467–76. doi: 10.1097/QAD.0000000000000174. [DOI] [PubMed] [Google Scholar]
- 13.Boufassa F, Lechenadec J, Meyer L, et al. Blunted response to combination antiretroviral therapy in HIV elite controllers: an international HIV controller collaboration. PLoS One. 2014;9:e85516. doi: 10.1371/journal.pone.0085516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chun TW, Shawn Justement J, Murray D, et al. Effect of antiretroviral therapy on HIV reservoirs in elite controllers. J Infect Dis. 2013;208:1443–7. doi: 10.1093/infdis/jit306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatano H, Yukl SA, Ferre AL, et al. Prospective antiretroviral treatment of asymptomatic, HIV-1 infected controllers. PLoS Pathog. 2013;9:e1003691. doi: 10.1371/journal.ppat.1003691. [DOI] [PMC free article] [PubMed] [Google Scholar]