Abstract
Background:
The classic technique of hepatectomy with venovenous bypass may cause a longer anhepatic phase and increase the rate of some complications, such as post-operative renal failure and thromboembolic events. But, in some cases, such as tumors and anatomic difficulties, the surgeon is obligated to use the classic technique even though there is some controversy about the safety of this technique without venovenous bypass in liver transplantation. The aim of this study was to compare the results of using the classic technique without venovenous bypass and the piggyback technique for liver transplantation.
Methods:
A retrospective case-series study was conducted on 227 consecutive successful liver transplants, including 55 cases in which the classic technique was used and 172 cases in which the piggyback technique was used. The transplants were performed from March 2010 through June 2011 in the Visceral Transplantation Ward at Namazi Hospital in Shiraz, Iran. The piggyback method was the preferred approach for hepatectomy, but the classic technique without venovenous bypass was performed in cirrhotic cases with anatomic difficulties, when there was a tumor, or when the surgeon preferred it.
Results:
There were no significant differences in post-operative rise in creatinine, decreases in intraoperative blood pressure, transfused packed red blood cells (RBC), or survival rates between the groups. Warm ischemic time (duration that donor liver is out of ice until it’s blood reperfusion in the recipient) was approximately seven minutes longer in the classic group (P = 0), but it was less than 52 minutes, which is an acceptable time for this phase. Hospital stays were shorter in the classic group than in the piggyback group (P = 0.024).
Conclusion:
Although the piggyback technique is the preferred technique for hepatectomy in liver transplantation, the classic technique without venovenous bypass can be used safely in cirrhotic livers when necessary or if the physician prefers it.
Keywords: classic technique, venovenous bypass, liver transplantation, piggyback technique
1. Introduction
The first orthotopic liver transplants (OLTs) with the classic technique in humans were attempted by Starzl (1, 2). Thereafter, some extensive experimental studies were conducted by other investigators, and alternative techniques for liver transplants were devised. Calne developed the piggyback technique, which is now the most popular technique for orthotopic liver transplantation (3). The classic technique consists of clamping the inferior vena cava above the renal veins and excision of the retrohepatic vena cava. Many patients can tolerate this procedure, but some require a venovenous bypass (VVB) to maintain a blood pressure level that perfuses essential organs, especially the kidneys, during clamping. This classic procedure is associated with unique complications that can be avoided by using the technique of liver resection without caval excision (the piggyback technique) (4). According to some authors, the classic technique may increase the rate of post-operative renal failure, hemodynamic instability, bleeding, and blood product consumption. Also, it can lead to a longer anhepatic phase, more time in the hospital, and, because of VVB, more thromboembolic complications, air emboli, wound seromas, infections, and additional costs (4–9). However, in some cases, the surgeon has an obligation to use the classic technique due to presence of tumors or anatomic difficulties (6, 8), but there is some controversy concerning the safety of this technique without VVB in liver transplantation.
More than 1700 OLTs, including 200 classic hepatectomies without VVB, have been performed at the Shiraz Transplant Center, and no significant changes have been observed in vital perioperative factors, such as renal function. This study was designed to compare the complications and outcomes of liver transplantations using two different techniques of hepatectomy (classic without VVB and the piggyback techniques) to ascertain whether the classic technique without VVB is a safe method to use in certain situations.
2. Materials and Methods
From March 2010 through June 2011, all 283 patients in the Visceral Transplantation Ward at Namazi Hospital in Shiraz, Iran, for orthotopic liver transplantation entered this retrospective case series study. However, 56 patients were excluded because they had partial liver transplants, i.e., from a living donor or a split liver from a deceased donor, which required the use of the piggyback technique. Eventually thus, 227 patients were included, of which 172 had the piggyback technique (group 1) and 55 had the classic technique (group 2).
The main method of hepatectomy was piggyback without VVB (no need to use it), but the classic technique without VVB (no need to use it) was used in cirrhotic cases with anatomic difficulties, including circulated liver parenchyma around the retrohepatic inferior vena cava (IVC) and the presence of tumors close to the retrohepatic IVC. The surgeon’s preference was also a reason for using the classic technique, with one of five of the main surgeons exhibiting this preference, especially in cases of Budd-chiari Syndrome. The patients’ demographics and other factors were compared between the two groups, including model of end stage liver disease (MELD) score, donor’s age, cold ischemic time (CIT: duration between the aort clamp in the donor and the liver exit from ice for implantation in the recipient), warm ischemic time (WIT), operative time, transfusions, pre-operative creatinine, early post-operative one-week renal function, pre-operative bilirubin, the lowest mean blood pressure in the pre-anhepatic, anhepatic, and post-anhepatic phases, bleeding (before and after hepatectomy), urine output, continuous renal replacement therapy (CRRT) usage, in-hospital mortality, mean Alanine aminotransferase (ALT) in the first post-transplant week, and survival.
The immunosuppressive therapy was the same in groups (triple therapy with corticosteroid, tacrolimus or cyclosporine, and mycophenolate mofetil). We used three factors to compare the post-operative renal function of the two groups, i.e., serum creatinine > 1.5 mg/dl, pre-operative creatinine vs. post-operative mean creatinine of days 1–7, and oliguria requiring CRRT during the first post-operative week. Data were analyzed using chi-squared, the Fisher exact test, the t-test, repeated measurements, and Kaplan-Meier (log rank for survival), where appropriate. Statistical significance was defined as a P value of < 0.05. All statistical analyses were performed using SPSS version 15 (SSPS Inc., Chicago, IL, U.S.).
3. Results
There were no significant differences in the ages and genders between the two groups. The causes of liver transplantations and their frequencies in both groups are presented in Table 1. Also, there were no significant differences between the two groups with respect to MELD scores, donor’s age, CIT, operation time, transfused packed RBC volume, intra-operative urine output, pre-operative creatinine, pre-operative bilirubin, CRRT usage, in-hospital mortality, or the mean ALT in the first post-operative week (Table 2). Serial creatinine measurements in the first post-operative week indicated that there was at least one episode of a level greater than 1.5 mg/dl in 49 of the 172 patients in group 1 and in 18 of the 55 patients in group 2; however, this difference was not statistically significant (P = 0.611).
Table 1.
Causes of liver transplantation and their frequencies in the two groups
| Cause | Group 1 (n = 172) n (%) | Group 2 (n = 55) n (%) |
|---|---|---|
| HBV cirrhosis | 38 (22.1) | 6 (10.9) |
| Cryptogenic cirrhosis | 32 (18.6) | 12 (21.8) |
| Autoimmune hepatitis | 32 (18.6) | 9 (16.4) |
| Wilson’s disease | 10 (5.8) | 1 (1.8) |
| HCV cirrhosis | 9 (5.2) | 2 (3.6) |
| PSC | 9 (5.2) | 8 (14.6) |
| HCC | 8 (4.7) | 5 (9.1) |
| Budd-chiari syndrome | 2 (1.2) | 6 (10.9) |
| Other | 32 (18.6) | 6 (10.9) |
Table 2.
Characteristics of the subjects in the study and findings
| Parameters | Group 1 (n = 172) | Group 2 (n = 55) | P-value |
|---|---|---|---|
| Age (yr) | 36.95 ± 15.29 | 40.17 ± 15.7 | NS |
| Gender (M/F) | 108/64 | 40/15 | NS |
| MELD score | 21.34 ± 5.22 | 20.62 ± 7.03 | NS |
| Donor’s age (yr) | 32.58 ± 14.8 | 31.33 ± 12.4 | NS |
| Cold ischemic time (hr) | 8.03 ± 2.82 | 7.89± 2.7 | NS |
| Warm Ischemic Time (min) | 45.07 ± 9.54 | 51.76±8.28 | 0.0* |
| Duration of Operation (min) | 349.51 ± 67.57 | 370.58±79.98 | NS |
| Crystalloid infused Volume (lit) | 3.62 ± 1.7 | 4.4±1.7 | 0.003* |
| Albumin infused Volume (cm3) | 58.17 ± 20.93 | 65.82± 19.4 | 0.017* |
| Packed RBC transfused Volume (unit) | 2.78 ±9.45 | 3.35±3.18 | NS |
| Pre-operation Creatinine (mg/dl) | 1.031 ±1.22 | 0.97± 0.6 | NS |
| Preoperation Bilirubin (mg/dl) | 7.27 ±9.5 | 8.75± 11.25 | NS |
| Creatinine (days 1–7) (patients < 1.5/patients > 1.5) | 123/49 | 37/18 | NS |
| BP Drop (during operation) | NS | ||
| BP (mmHg) (in anhepatic phase) | 61.98 ± 9.6 | 64.24±9.38 | NS |
| ALT (U/L) (1–8 days) | NS | ||
| Creatinine (all patients) (1–7 days vs. pre-operation) | NS | ||
| CRRT use | NS | ||
| In-hospital mortality (%) | 1.75 | 1.81 | NS |
| Hospital stay (day) | 14.6 ± 9.76 | 12.42 ± 4.5 | 0.024** |
| Mortality rate (%) | 8.14 | 5.45 | NS |
| One-year survival rate, % | 92 | 94.4 | NS |
| Bleeding volume before hepatectomy (cm3) | 613.31 ± 628.1 | 1167.27 ± 1098.9 | 0.001* |
| Bleeding volume after hepatectomy (cm3) | 916.53 ± 1138.73 | 1161.82 ± 1103.9 | NS |
| Total bleeding (cm3) | 1529.22 | 2319.45 | 0.010* |
| Urine output (intraoperative) (cm3) | 827.85 | 1001.57 | 0.035** |
NS = Not Significant;
= better in group 1;
= better in group 2
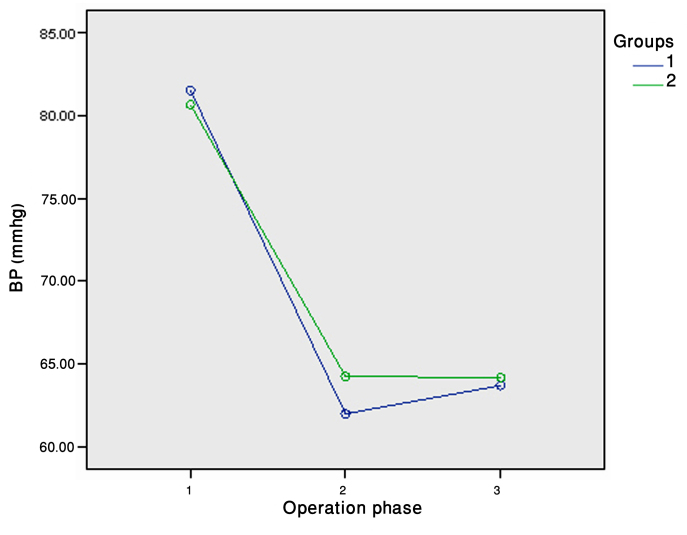
Furthermore, no remarkable increase was observed when the mean measured creatinine level in the first post-operative week was compared to the mean level in the pre-operative week (P = 0.391). There was no significant difference between the lowest mean arterial blood pressure of group 1 (62 mmHg) and group 2 (64.5 mmHg) in the anhepatic phase (P = 0.13) . Although there was a significant decrease in blood pressure from before clamping (pre-anhepatic phase) to the unclamping phase in all patients, there was no significant difference between the two groups (P = 0.1) (Table 2 and Figure 1).
Figure 1.
Blood pressure (BP) changes during the phases of the operation
(1: pre-anhepatic, 2: anhepatic, 3: post-anhepatic)
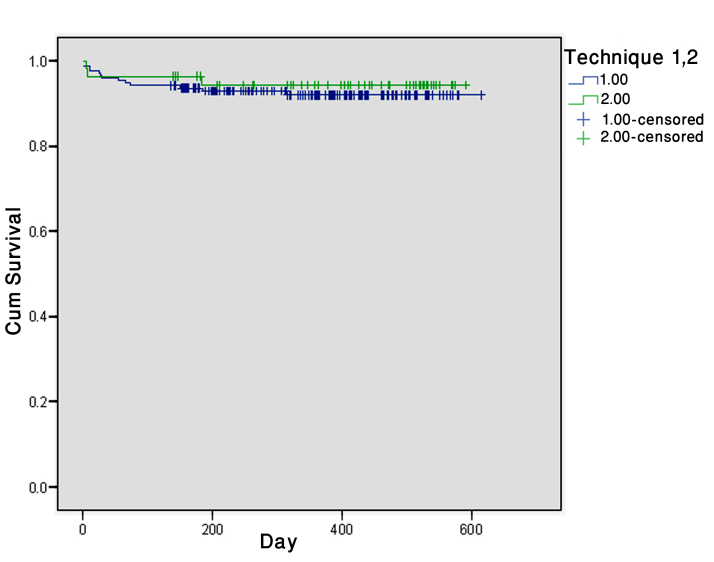
The mortality rates were 7.6% (13 cases) in group 1 and 5.5% (3 cases) in group 2 (P = 0.766). The one-year survival when the classic technique was used (94.4%) was insignificantly better than that when the piggyback technique was used (92%) (P = 0.580) (Figure 2). Comparing WIT (45.07 ± 9.54 min vs. 51.76 ± 8.28 min), infused crystalloid and albumin volumes were significantly different between the two groups. Total bleeding and the bleeding volume of group 1 before hepatectomy were significantly lower than those of group 2 (P = 0.01 and 0.001, respectively), but comparing bleeding volume after hepatectomy showed no considerable difference between the two groups (P = 0.164). Interestingly, time spent in the hospital was shorter in group 2 than in group 1 (12.42 ± 4.5 days vs. 14.6 ± 9.76 days, P = 0.024,) and urine output was significantly greater in group 2 (P = 0.035).
Figure 2.
Survival rates in group 1 and group 2
4. Discussion
According to some authors, one of the major shortcomings of the classic technique is that it has a higher incidence of post-operative Acute Renal Failure (ARF) than the piggyback technique (10). Cabezuelo et al. reported that the classic technique represented an independent risk factor for post-operative ARF (11), while some studies did not report any differences between the two techniques (12–16). The present study showed no significant difference between the techniques with respect to post-operative renal function. The exact reason for the reported difference is not clear, but accurate intra-operative, hemodynamic monitoring and probable interventions to keep appropriate renal perfusion may prevent post-operative ARF in the classic technique. Furthermore, with such a comparable low rate of post-operative ARF in the classic technique without VVB and the high rate of complications associated with VVB, it seems unnecessary to use VVB as an essential part of classic hepatectomy just to decrease the rate of post-transplantation renal failure.
Our study showed that, although the infused solutions and bleeding were more in the classic technique than in the piggyback technique, the intra-operative decrease in BP was not significantly different for the two groups, and the intra-operative urine output was even greater in the classic group. This shows that prompt replacement of blood loss using crystalloid and colloid solutions to avoid decreased BP is critical, especially in the anhepatic phase, for the prevention of intra-operative and post-operative renal damage. In the present study, there was no significant difference between the two groups regarding the duration of the operation or CIT, but, in agreement with some other studies (14, 15, 17, and 18), WIT was longer in the classic group, which was probably the result of one more anastomosis in the infrahepatic vena cava. However, the difference was only about seven minutes, and the mean duration of WIT for patients in the classic group was less than 52 minutes, which is an acceptable duration for this phase. The results of this study showed that, in contrast with some studies (8, 12), the time spent in the hospital was shorter in the classic group than in the piggyback group. This might be due to the surgeon’s extensive experience with the classic technique without VVB, resulting in patients’ experiences being similar to those of the patients who had the piggyback procedure.
The limitation of this study was our center policy (try to do piggyback technique until obligation to use classic technique because of excessive bleeding), which had an insistent preference for the piggyback technique, even with its anatomical difficulties, in the most primary cases of classic technique. Such a preference may cause a methodological bias, imposing on the patients more intra-operative bleeding (before the hepatectomy and in total) and a longer time to complete the hepatectomy.
5. Conclusions
Our findings showed that, although the piggyback technique was probably the technique of choice for hepatectomy in liver transplantation, the classic technique even without VVB can be used safely in necessary situations and in accordance with the surgeon’s preference. We also found that the choice of surgical technique had no significant effect on the primary and final outcome in non-acute (cirrhotic) causes of liver transplantation. Therefore, we recommend the classic technique even without VVB in the above situations because it can be performed without any significant problems or complications.
Acknowledgments
The authors thank Dr. Nasrin Shokrpour for help in editing the manuscript. We also thank Mrs. Sareh Rousta and Mrs. Marjan Gholami at the Center for Development of Clinical Research at Shiraz Namazi Hospital for their assistance with the research.
Footnotes
Conflict of Interest: There is no conflict of interest to be declared.
Authors’ contributions: All of authors contributed to this project and article equally. All authors read and approved the final manuscript.
References
- 1.Starzl TE, Marchioro TL, Vonkaulla KN, Hermann G, Brittain RS, Waddell WR. HOMOTRANSPLANTATION OF THE LIVER IN HUMANS. Surg Gynecol Obstet. 1963;117:659–76. [PMC free article] [PubMed] [Google Scholar]
- 2.Starzl TE, Groth CG, Brettschneider L, Penn I, Fulginiti VA, Moon JB, et al. Orthotopic homotransplantation of the human liver. Ann Surg. 1968;168:392–415. doi: 10.1097/00000658-196809000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Calne RY, Williams R. Liver transplantation in man. I. Observations on technique and organization in five cases. Br Med J. 1968;4:535–40. doi: 10.1136/bmj.4.5630.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nikeghbalian S, Dehghani M, Salahi H, Bahador A, Kazemi K, Kakaei F, et al. Effects of surgical technique on postoperative renal function after orthotopic liver transplant. Exp Clin Transplant. 2009;7:25–7. [PubMed] [Google Scholar]
- 5.Stieber AC. One surgeon’s experience with the piggyback versus the standard technique in orthotopic liver transplantation: is one better than the other? Hepatogastroenterology. 1995;42:403–5. [PubMed] [Google Scholar]
- 6.Busque S, Esquivel CO, Concepcion W, So SK. Experience with the piggyback technique without caval occlusion in adult orthotopic liver transplantation. Transplantation. 1998;65:77–82. doi: 10.1097/00007890-199801150-00015. [DOI] [PubMed] [Google Scholar]
- 7.Remiszewski P, Zieniewicz K, Krawczyk M. Early results of orthotopic liver transplantations using the technique of inferior vena cava anastomosis. Transplant Proc. 2006;38:237–9. doi: 10.1016/j.transproceed.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 8.Hosein Shokouh-Amiri M, Osama Gaber A, Bagous WA, Grewal HP, Hathaway DK, Vera SR, et al. Choice of surgical technique influences perioperative outcomes in liver transplantation. Ann Surg. 2000;231:814–23. doi: 10.1097/00000658-200006000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoffmann K, Weigand MA, Hillebrand N, Buchler MW, Schmidt J, Schemmer P. Is veno-venous bypass still needed during liver transplantation? A review of the literature. Clin Transplant. 2009;23:1–8. doi: 10.1111/j.1399-0012.2008.00897.x. [DOI] [PubMed] [Google Scholar]
- 10.Jovine E, Mazziotti A, Grazi GL, Ercolani G, Masetti M, Morganti M, et al. Piggy-back versus conventional technique in liver transplantation: report of a randomized trial. Transpl Int. 1997;10:109–12. doi: 10.1007/pl00003824. [DOI] [PubMed] [Google Scholar]
- 11.Cabezuelo JB, Ramirez P, Acosta F, Torres D, Sansano T, Pons JA, et al. Does the standard vs piggyback surgical technique affect the development of early acute renal failure after orthotopic liver transplantation? Transplant Proc. 2003;35:1913–4. doi: 10.1016/s0041-1345(03)00598-0. [DOI] [PubMed] [Google Scholar]
- 12.Khan S, Silva MA, Tan YM, John A, Gunson B, Buckels JA, et al. Conventional versus piggyback technique of caval implantation; without extra-corporeal veno-venous bypass. A comparative study. Transpl Int. 2006;19:795–801. doi: 10.1111/j.1432-2277.2006.00331.x. [DOI] [PubMed] [Google Scholar]
- 13.Salizzoni M, Andorno E, Bossuto E, Cerutti E, Livigni S, Lupo F, et al. Piggyback techniques versus classical technique in orthotopic liver transplantation: a review of 75 cases. Transplant Proc. 1994;26:3552–3. [PubMed] [Google Scholar]
- 14.Miyamoto S, Polak WG, Geuken E, Peeters PM, de Jong KP, Porte RJ, et al. Liver transplantation with preservation of the inferior vena cava. A comparison of conventional and piggyback techniques in adults. Clin Transplant. 2004;18:686–93. doi: 10.1111/j.1399-0012.2004.00278.x. [DOI] [PubMed] [Google Scholar]
- 15.Reddy KS, Johnston TD, Putnam LA, Isley M, Ranjan D. Piggyback technique and selective use of veno-venous bypass in adult orthotopic liver transplantation. Clin Transplant. 2000;14:370–4. doi: 10.1034/j.1399-0012.2000.14040202.x. [DOI] [PubMed] [Google Scholar]
- 16.Vieira de Melo PS, Miranda LE, Batista LL, Neto OC, Amorim AG, Sabat BD, et al. Orthotopic liver transplantation without venovenous bypass using the conventional and piggyback techniques. Transplant Proc. 2011;43:1327–33. doi: 10.1016/j.transproceed.2011.03.061. [DOI] [PubMed] [Google Scholar]
- 17.Isern MR, Massarollo PC, de Carvalho EM, Baia CE, Kavakama J, de Andrade Lima P, et al. Randomized trial comparing pulmonary alterations after conventional with venovenous bypass versus piggyback liver transplantation. Liver Transpl. 2004;10:425–33. doi: 10.1002/lt.20067. [DOI] [PubMed] [Google Scholar]
- 18.Nishida S, Nakamura N, Vaidya A, Levi DM, Kato T, Nery JR, et al. Piggyback technique in adult orthotopic liver transplantation: an analysis of 1067 liver transplants at a single center. HPB (Oxford) 2006;8:182–8. doi: 10.1080/13651820500542135. [DOI] [PMC free article] [PubMed] [Google Scholar]