Abstract
Background
Depending on interest, knowledge, and skills, oncologists are adapting clinical behaviour to include integrative approaches, supporting patients to make informed complementary care decisions. The present study sought to improve the knowledge base in three ways:
Test the acceptability of a self-reported online survey for oncologists.
Provide preliminary data collection concerning knowledge, attitudes, beliefs, and current referral practices among oncologists with respect to yoga in adult cancer.
List the perceived benefits of and barriers to yoga intervention from a clinical perspective.
Methods
A 38-item self-report questionnaire was administered online to medical, radiation, and surgical oncologists in British Columbia.
Results
Some of the 29 oncologists who completed the survey (n = 10) reported having recommended yoga to patients to improve physical activity, fatigue, stress, insomnia, and muscle or joint stiffness. Other responding oncologists were hesitant or unlikely to suggest yoga for their patients because they had no knowledge of yoga as a therapy (n = 15) or believed that scientific evidence to support its use is lacking (n = 11). All 29 respondents would recommend that their patients participate in a clinical trial to test the efficacy of yoga. In qualitative findings, oncologists compared yoga with exercise and suggested that it might have similar psychological and physical health benefits that would improve patient capacity to endure treatment. Barriers to and limitations of yoga in adult cancer are also discussed.
Conclusions
An online self-report survey is feasible, but has response rate limitations. A small number of oncologists are currently recommending yoga to improve health-related outcomes in adult cancer. Respondents would support clinical yoga interventions to improve the evidence base in cancer patients, including men and women in all tumour groups.
Keywords: Yoga, oncologists, surveys, cam
1. BACKGROUND
In 2012, 14.1 million new cases of cancer were diagnosed, and 32.6 million people were living with cancer worldwide1. Conventional treatment options for cancer include radiotherapy, hormonal therapy, chemotherapy, and surgery2. In parallel with conventional care, cancer patients seek out complementary and alternative medicine (cam) such as herbal remedies, vitamins and minerals, medicinal teas, spiritual therapies, and relaxation techniques3. Patients perceive cam as an additive therapy for increasing the body’s ability to fight cancer or for improving physical and emotional wellbeing4. In Canada, 48% of patients use a cam therapy during cancer treatment—a rate that exceeds the worldwide average by 8 percentage points5. In response to the surge in patients seeking complementary care, oncologists are, depending on their interest, knowledge, and skills, seeking to integrate conventional treatment by supporting patients with their cam decisions6.
The mind–body technique of yoga is frequently recommended as a cam by researchers and health care professionals7; however, a literature review shows a gap in the availability of documentation to understand the current view of oncologists about yoga in adult cancer. Our study is the first that we are aware of that has been designed to understand the clinical relevance, patterns of use, and attitudes among oncologists toward yoga as a therapeutic intervention in conventional adult cancer care. The Knowledge, Attitudes, and Patterns of Yoga (kap-y) survey was developed to test the feasibility of self-reported online surveys of oncologists in Canada. The results of the survey were used to outline potential themes concerning the knowledge, attitudes, beliefs, and current referral practices among oncologists with respect to yoga in adult cancer. The perceptions of oncologists about the benefits of and barriers to yoga interventions for cancer patients were investigated for the first time.
2. METHODS
2.1. Developing the Survey
The 38-item self-report online kap-y survey was designed and piloted with surgical, medical, and radiation oncologists in British Columbia. The format of the questionnaire was based on concepts validated in a cam knowledge, attitudes, and practice survey [Balneaves LG, Truant TLO, Verhoef MJ, Ross B, Porcino A. Assessing the complementary and alternative medicine (cam) information and decision support needs of patients and health professionals at a Canadian cancer agency. Presented at the International Psychological Oncology Society 12th World Congress/Canadian Association of Psychosocial Oncology 2010 Conference; Quebec City, QC; May 25–29, 2010]. The content validity of the survey instrument was assessed using a 5-step process8; face validation included sampling the survey with pediatric oncologists (n = 3) and research experts (n = 5).
The kap-y has 5 sections: professional and personal background (24 items); knowledge, attitudes, and beliefs about yoga (5 items in 55 parts); interest, willingness, and yoga in clinical practice (3 items in 6 parts); concerns and barriers with respect to yoga for cancer patients (3 items in 13 parts); and open remarks about yoga and the survey (3 items, open-ended). The questionnaire collected nominal, ordinal, and Likert-scale quantitative data and free text (qualitative data).
2.2. Administering the Survey
An e-mail invitation to participate in the online survey (with a link to the survey provided) was sent to a purposive sample (n = 260) of oncologists registered with the BC Cancer Agency. Participants were asked to complete an eligibility survey and to provide an e-signature of consent before participating in the study. A $10 donation to the BC Cancer Agency Foundation for research was made on behalf of each participant.
2.3. Analysis
The survey response rates and completion rates are presented in absolute and percentage values. Time to complete survey is presented as an average across all participants. Ordinal, nominal, and ratio scale data are presented in frequency and absolute values. In some cases, nominal data were condensed from 5 to 3 categories to clarify results for the reader. Free text submitted in response to open-ended questions was first analyzed for themes and patterns (MM) and then analyzed using Wordle (http://www.wordle.net/), an information visualization technique.
3. RESULTS
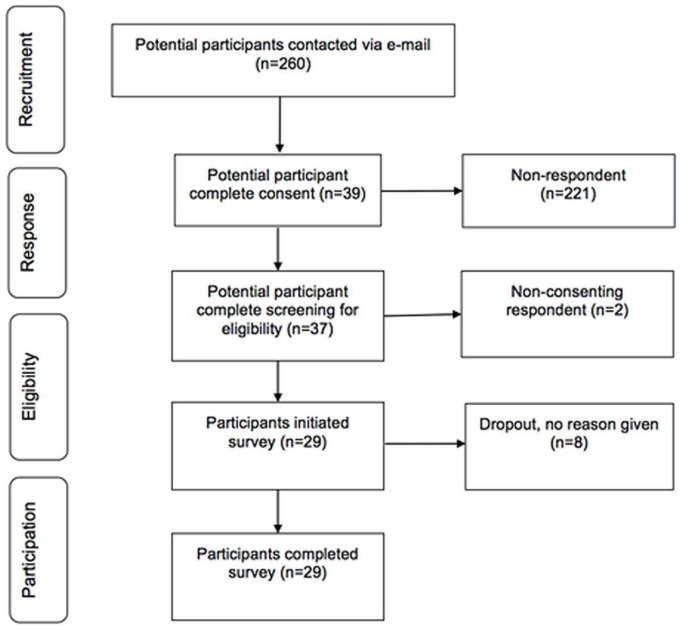
The invitation attracted 39 respondents, 2 of whom did not provide consent, and 8 of whom did not complete the eligibility survey (Figure 1). The response rate was therefore 15% (39 of 260 invitees), and the initiation–completion rate was 100% (29 of 29). Statistical analysis with a 95% confidence interval indicated that the quantitative results are unreliable (confidence interval: ±17.2; p = 0.05). The average time to complete the survey was 16.4 minutes.
FIGURE 1.
Participant flow diagram.
3.1. Characteristics of the Respondents
Of the 29 qualified respondents, 17 (59%) were medical oncologists, and 12 (41%) were radiation oncologists. No surgical oncologists participated in the survey. The sample included men (n = 15) and women (n = 14) 28–56 years of age (mean: 41.9 years) with a wide range of professional experience: less than 5 years (n = 12), 5–25 years (n = 13), and more than 25 years (n = 4). The ethnic backgrounds of the respondents included white (n = 18), Chinese (n = 5), Indian (n = 5), and Hispanic (n = 1). Religious affiliations included Christian (n = 9), Hindu (n = 3), Jewish (n = 3), Sikh (n = 1), and unspecified or not religious (n = 13).
3.2. Attitudes of Oncologists Toward Yoga
Responding oncologists believed that yoga is of interest for improving clinical care in adult cancer (69.0%, n = 20). No respondents disapproved of yoga practice during treatment for cancer, and 21 oncologists (72%) did not agree that yoga would be a waste of time for patients. In comparison with cam, yoga attracted a slightly higher level of interest among oncologists. In investigating the perceived definition of yoga among oncologists, 14 (48%) did not agree yoga is a complementary therapy, and 26 (90%) did not agree that yoga is a religious practice or lacks therapeutic value.
Analysis of the qualitative data (free text responses) identified three themes:
Yoga is perceived by oncologists as a gentle, adaptive form of exercise.
Yoga has perceived benefits for relaxation and stress management in patients.
Oncologists are prevented from recommending yoga to patients because of a lack of scientific evidence and absence of knowledge about how and where to access classes.
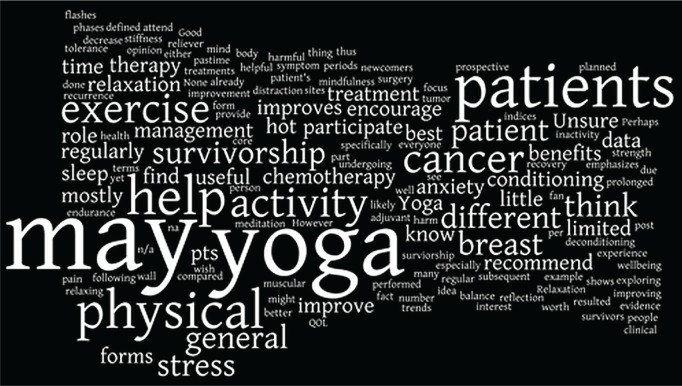
A Wordle pictogram (Figure 2) summarizes the kap-y qualitative data concerning yoga for symptom management in adult cancer (responses from question item 35). Oncologists remarked that yoga’s use in oncology, especially in breast cancer, is “worth exploring” because it might improve relaxation and mindfulness, and reduce pain and fatigue in patients.
FIGURE 2.
Wordle diagram of the views of oncologists about yoga.
Some oncologists (17%, n = 5) suggested that the effect of yoga on physical health might be similar to that of exercise: “In my opinion, all forms of exercise help with stress. Yoga is one of the best forms of exercise [because] each person participates to their level—thus everyone can participate—and little harm is done to the body” (male radiation oncologist, age 36). Another respondent suggested that “if [yoga] improved endurance and physical conditioning, patients may be able to tolerate more treatments” (female medical oncologist, age 31). Participants in the study perceived yoga to be separate from cam, but similar to physical activity. Two respondents disliked the association of yoga and exercise with cam.
3.3. Perceptions of Oncologists About Yoga Evidence
Some oncologists were hesitant or unlikely to suggest yoga for their patients because they reported not having knowledge of yoga as a therapy (52%, n = 15) or because they believed that scientific evidence to support the use of yoga was lacking (38%, n = 11). All 29 respondents said that they would recommend that patients participate in a clinical trial of yoga intervention. A few oncologists (17%, n = 5) made specific requests concerning the design of a clinical trial to test the efficacy of yoga for improving stress and fatigue during radiotherapy and chemotherapy. Three respondents requested implementation of studies to compare yoga with exercise for efficacy in improving physical and psychological health and for determining the effect of yoga on patient tolerance to treatment and on biomarkers for immune response.
3.4. Knowledge and Beliefs Among Oncologists About Yoga
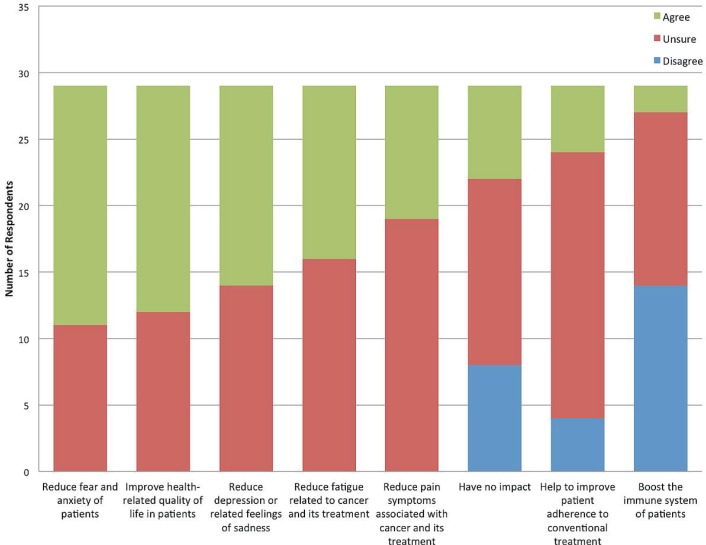
Respondents believed that practising yoga during conventional treatment reduces fear and anxiety among patients (62%, n = 18) and would improve health-related quality of life (59%, n = 17). Most of the respondents strongly disagreed that practising yoga decreases tumour size (52%, n = 15) and were unsure (or did not believe) that yoga would boost the immune system in patients (93%, n = 27). Respondents disagreed that yoga would cause a patient to make dangerous decisions or would interfere with patient treatment in some negative way (66%, n = 19). Respondents were uncertain about whether yoga might improve patient adherence to conventional treatment (69%, n = 20). See Figure 3 for a summary of beliefs among the responding oncologists about specific psychological and physical benefits of yoga in adult cancer.
FIGURE 3.
Beliefs reported by responding oncologists about the effects of yoga in adult cancer patients.
3.5. Patterns of Yoga Use in Conventional Treatment
Responding oncologists suggested that yoga would be suitable for male and female patients with early-or late-stage cancer of all tumour types. Of our B.C. respondents, 34% (n = 10) have recommended yoga to patients to improve physical activity, fatigue, stress, insomnia, and muscle or joint stiffness. Some respondents felt happy to refer patients to a yoga intervention (55%, n = 16), but fewer than half felt willing to recommend it to patients at this time (38%, n = 11). Oncologists have suggested yoga to patients for stress relief in adjuvant breast cancer (female medical oncologist, age 55) and for assisting with hot flashes and sleep quality (female radiation oncologist, age 40). When asked about the frequency with which they recommended other complementary or adjunct therapies to improve health outcomes in patients, all 29 responding oncologists reported that they currently recommend physical exercise. Oncologists also reported recommending massage (79%, n = 23), acupuncture (48%, n = 14), and meditation (41%, n = 12) to their cancer patients.
3.6. Perceived Barriers to Yoga Adherence
Oncologists identified several potential limitations and barriers to practising yoga during cancer treatment (Table i). Respondents believed that attendance at yoga classes would be most difficult for patients experiencing serious side effects of treatment, including pain and fatigue. Fear of infection was also identified as a potential deterrent to attending group yoga classes.
TABLE I.
Potential barriers perceived by oncologists to patient adherence to a yoga class
| Barrier type | Barrier |
|---|---|
| Physical | Fatigue |
| Pain | |
| Nausea | |
| Logistic | Finances |
| Transportation | |
| Scheduling | |
| Psychological | Stress |
| Anxiety | |
| Depression | |
| Yoga-related | Lack of patient-perceived benefit |
| Lack of patient interest |
4. DISCUSSION
A bibliometric analysis cited a surge in yoga research in health care publications since 2007, with a significant rise in cancer studies in the preceding 5 years9. The present pilot survey is an important first step in tracking the acceptance and use of yoga in conventional cancer care. Its quantitative and qualitative results suggest that interest and clinical equipoise10 are sufficient to warrant research into the field of yoga intervention and potential health-related outcomes in adult cancer. Responding medical and radiation oncologists demonstrated a positive, curious attitude toward yoga and recommended that yoga be tested for efficacy in adult cancer. Some oncologists are recommending yoga to improve anxiety levels, pain management, and sleep quality.
As was found in earlier work11, accessibility, unclear cost–benefit, and lack of evidence-based guidance are significant barriers to recommendations by oncologists of yoga in adult cancer. The present study adds to that list concerns by oncologists that patient fatigue, anxiety, pain, nausea, scheduling issues, and lack of interest could also decrease participation in yoga.
4.1. Implications for Study Design
Our online survey was initiated and completed by 29 of 260 contacted oncologists in Vancouver, British Columbia. The low response rate restricted use of the data to a preliminary descriptive analysis only. Most respondents (n = 25) identified no issues of formatting, content, or threatening bias in the questionnaire. Two respondents registered complaints that “Other” or “Not applicable” choices forced them to select responses that were not entirely indicative of their position, and that some (unspecified) questions appeared vague.
4.1.1. Survey Method
The online survey was a cost-efficient method for gathering data from oncologists and was easily administered by a small research team. The survey also offered anonymity for respondents and a rapid completion time (about 16 minutes). An electronic survey format lowered the risk of human error and researcher bias, but added complications in terms of piloting12. The survey identified serious risks of reporting bias and a low response rate (<15%). In future applications, a larger randomized sample would be needed to improve the generalizability of results.
To improve the response rate, future studies will consider extending the recruitment period (perhaps to 6–12 months) or conducting the survey with a “captive” audience—during a conference, for instance. Financial or other incentives might increase participation13. An indirect incentive of $10 was allocated to the BC Cancer Agency Foundation for kap-y participation, which in retrospect might have been inadequate; a sample of oncologists reported solicitations from private companies to complete online surveys with offers up to CA$100 in personal compensation to participate. According to a recent randomized controlled trial of response rates for general practitioners (n = 125), even a small nonfinancial incentive in the form of a pen increased the rate to 61.9% from 47% (in a control group), and when given a choice between paper and online survey methods, health care professionals completed only the paper version14. Those results indicate that future surveys might consider including a paper option and a small gift for participants.
Additional research methods including focus groups or semistructured interviews might improve the contextual understanding of how yoga is perceived by oncologists and might provide more in-depth qualitative findings15. The qualitative components of our survey were limited to 3 open-ended questions and one-way communication.
4.2. Implications for Yoga in Oncology
4.2.1. Yoga Intervention in Adult Cancer
A literature review shows that clinical trials in adult cancer are usually conducted in female breast cancer survivors. Few clinical studies have been performed in male cancer patients or in other cancer types during treatment. It is unclear whether those tendencies are a result of patient interest, adherence rates associated with patient demographic factors16, or other research bias. Based on findings about the perspectives of the oncologists surveyed, yoga intervention would be appropriate for male and female patients with all tumour types and should be explored further.
4.2.2. Is Yoga CAM?
Existing research tends to characterize yoga as cam. The open-ended responses of several oncologists (n = 3) indicated that they distinguished both yoga and exercise from cam. Although a definition of yoga was outside the scope of the present study, it is evident that future research will want to consider such a definition, especially in terms of the clinical perception of yoga. According to the U.S. National Center for Complementary and Alternative Medicine18, “complementary” generally refers to the use of a non-mainstream approach together with conventional medicine—usually natural or mind–body practices. Results of the present study indicate that oncologists believe yoga to be analogous to exercise and not necessarily cam. The World Health Organization defines exercise as “any bodily movement produced by skeletal muscles that requires energy expenditure”19. Although both definitions appear to capture the essence of yoga, the acceptability of yoga as exercise might be more established in oncology.
4.2.3. Impact of Oncologist Characteristics
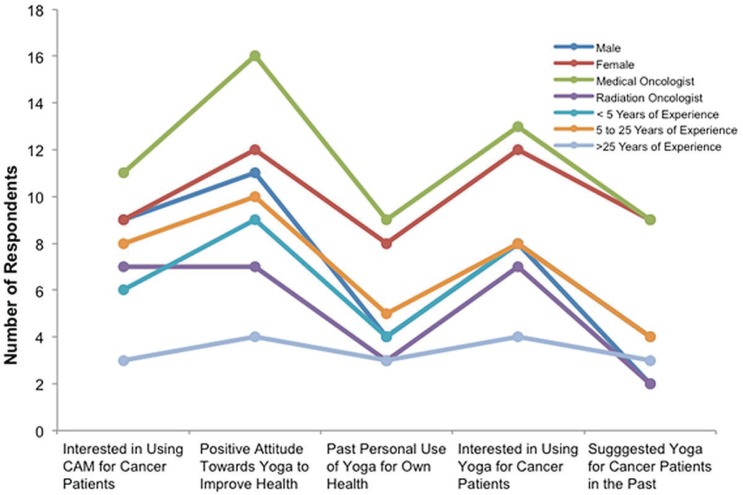
A yoga market study reported that 82.2% of people who practise yoga are female17. Sex, age, years of professional experience, and religious affiliation were requested from our surveyed oncologists, and a preliminary subgroup analysis indicates that female and medical oncologists were more likely than male and radiation oncologists to report a positive attitude toward yoga. The female and medical oncologist respondents also reported higher rates of personal yoga practise and historical recommendation of yoga in patient care. Years of professional experience did not appear to influence attitudes toward yoga among oncologists (Figure 4). Other demographic or professional characteristics might affect the attitudes, beliefs, and willingness of oncologists to prescribe yoga as a therapeutic option; however, additional research with a larger randomized sample is needed to understand potential associations.
FIGURE 4.
Characteristics and attitudes toward yoga of the responding oncologists.
5. CONCLUSIONS
Most respondents believed that scientific evidence to support the use of yoga in adult cancer is lacking. A few oncologists are currently recommending yoga to improve health-related outcomes in adult cancer. All responding oncologists would support the development of randomized controlled trials of a yoga intervention across all tumour groups, including male cancer patients.
The results of our survey suggest that future developments of yoga intervention should address potential barriers of patient adherence, including excessive fatigue, pain, and fear of infection in a group class. Our findings also confirm that some oncologists have a favourable attitude toward yoga, and those oncologists suggest that, like exercise, yoga has the potential to improve psychological and physical health in cancer patients.
6. ACKNOWLEDGMENTS
The authors thank the reporting oncologists and colleagues from the University of British Columbia, the University of Oxford, and the BC Cancer Agency for their assistance with the administration and completion of the oncologist survey. Permission to use or amend the kap-y instrument can be obtained by contacting the corresponding author. The survey is available for free download at https://www.research.net/s/ONC_KAPY.
7. ACKNOWLEDGMENT OF SUPPORT
The present study was self-funded and completed as partial fulfilment of a research doctorate in Evidence-based Health Care, University of Oxford. Supervision of the study and contributions to the manuscript were provided by Drs. Carl Heneghan and Alison Ward, Department of Primary Health Care Sciences, University of Oxford. The ethical application to perform the research in Vancouver, British Columbia, was sponsored by Drs. Sally Thorne and Lynda Balneaves, University of British Columbia. Data collection was facilitated by Fiona Walks, BC Cancer Agency. A special thank-you goes to Drs. Caron Strahlendorf and Sian Harrison for assistance in validating the questionnaire.
8. CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
9. REFERENCES
- 1.Ferlay J, Soerjomataram I, Ervik M, et al. globocan 2012: Estimated Cancer Incidence and Mortality Worldwide in 2012 [Web resource] Lyon, France: International Agency for Research on Cancer; 2012. Ver 1.0. [Google Scholar]
- 2.World Health Organization (who) Fact sheet 297. Geneva, Switzerland: WHO; 2014. Cancer [Web page] [Available at: http://www.who.int/mediacentre/factsheets/fs297; cited February 25, 2014] [Google Scholar]
- 3.Deng GE, Frenkel M, Cohen L, et al. on behalf of the Society for Integrative Oncology Evidence-based clinical practice guidelines for integrative oncology: complementary therapies and botanicals. J Soc Integr Oncol. 2009;7:85–120. [PubMed] [Google Scholar]
- 4.Molassiotis A, Fernadez–Ortega P, Pud D, et al. Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol. 2005;16:655–63. doi: 10.1093/annonc/mdi110. [DOI] [PubMed] [Google Scholar]
- 5.Horneber M, Bueschel G, Dennert G, Less D, Ritter E, Zwahlen M. How many cancer patients use complementary and alternative medicine: a systematic review and meta- analysis. Integr Cancer Ther. 2012;11:187–203. doi: 10.1177/1534735411423920. [DOI] [PubMed] [Google Scholar]
- 6.Brazier AS, Balneaves LG, Seely D, Stephen JE, Suryaprakash N, Taylor–Brown JW. Integrative practices of Canadian oncology health professionals. Curr Oncol. 2008;15(suppl 2):S110.es87–91. doi: 10.3747/co.v15i0.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sewitch MJ, Cepoiu M, Rigillo N, Sproule D. A literature review of health care professional attitudes toward complementary and alternative medicine. Complement Health Pract Rev. 2008;13:139–54. [Google Scholar]
- 8.Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;35:382–5. doi: 10.1097/00006199-198611000-00017. [DOI] [PubMed] [Google Scholar]
- 9.McCall MC. In search of yoga: research trends in a Western medical database. Int J Yoga. 2013;7:4–8. doi: 10.4103/0973-6131.123470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freedman B. Equipoise and the ethics of clinical research. N Engl J Med. 1987;317:141–5. doi: 10.1056/NEJM198707163170304. [DOI] [PubMed] [Google Scholar]
- 11.Slocum–Gori S, Howard AF, Balneaves LG, Kazanjian A. Investigating the perceived feasibility of integrative medicine in a conventional oncology setting: yoga therapy as a treatment for breast cancer survivors. Integr Cancer Ther. 2013;12:103–12. doi: 10.1177/1534735412443851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andrews D, Nonnecke B, Preece J. Electronic survey methodology: a case study in reaching hard-to-involve internet users. Int J Hum Comput Interact. 2003;16:185–210. doi: 10.1207/S15327590IJHC1602_04. [DOI] [Google Scholar]
- 13.Groves RM, Fowler FJ Jr, Couper MP, Lepkowski JM, Singer E, Tourangeau R, editors. Survey Methodology. 2nd ed. Hoboken, NJ: John Wiley and Sons; 2009. [Google Scholar]
- 14.Pit SW, Hansen V, Ewald D. A small unconditional non- financial incentive suggests an increase in survey response rates amongst older general practitioners (gps): a randomised controlled trial study. BMC Fam Pract. 2013;14:108. doi: 10.1186/1471-2296-14-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bourgeault I, Dingwall R, de Vries R. The Sage Handbook of Qualitative Methods in Health Research. London, UK: Sage; 2013. [Google Scholar]
- 16.Cramer H, Lauche R, Langhorst J, Paul A, Michalsen A, Dobos G. Predictors of yoga use among internal medicine patients. BMC Complement Altern Med. 2013;13:172. doi: 10.1186/1472-6882-13-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoga Journal Yoga JournalReleases 2012 Yoga in America Market Study [press release]. Daytona Beach, FL: Yoga Journal; 2012[Available online at: http://www.yogajournal.com/article/press-releases/yoga-journal-releases-2012-yoga-in-america-market-study/; cited December 21, 2013] [Google Scholar]
- 18.United States Department of Health and Human Services, National Institutes of Health, National Center for Complementary and Alternative Medicine (nccam) Complementary, Alternative, or Integrative Health: What’s In a Name? [Web page] Bethesda, MD: NCCAM; 2013. [Available at: http://nccam.nih.gov/health/whatiscam; cited January 28, 2014] [Google Scholar]
- 19.World Health Organization (who) Health topics: Physical activity [Web page] Geneva, Switzerland: WHO; 2014. [Available at: http://www.who.int/topics/physical_activity; cited January 18, 2014] [Google Scholar]