Abstract
Objective
The “critical comments” dimension of the expressed emotion (EE) construct has been found to predict the illness course of patients with bipolar disorder, but less is known about the “emotional overinvolvement” (EOI) component. The goal of this study was to evaluate whether relatives’ observed appropriate and inappropriate emotional involvement (intrusiveness, self-sacrifice, and distress about patients’ well-being) moderated the effectiveness of a family-based intervention for bipolar disorder.
Method
108 patients with bipolar disorder (mean age = 35.61 years [SD = 10.07]), 57% female) and their relatives (62% spouses) from two clinical trials completed 10-minute problem-solving interactions prior to being treated with pharmacotherapy plus family-based therapy (FBT) or brief psychoeducation (crisis management, CM). Patients were interviewed every 3–6 months over 2 years to assess mood symptoms.
Results
When relatives showed low levels of inappropriate self-sacrifice, CM and FBT were both associated with improvements in patients’ manic symptoms over 2 years. When relatives showed high levels, patients in CM became more manic over time, whereas patients in FBT became less manic. Group differences in mania trajectories were also observed at high levels of inappropriate emotional response but not at low. When relatives showed high levels of appropriate self-sacrifice, patients in both groups became less depressed. At low levels of appropriate self-sacrifice, patients in CM did not improve, whereas patients in FBT became less depressed.
Conclusions
Future studies of bipolar disorder should consider the prognostic value of the amount and appropriateness of relatives’ emotional involvement with patients in addition to their critical behaviors.
Keywords: expressed emotion, emotional overinvolvement, EOI, bipolar disorder, family therapy, behavioral observations
The construct of expressed emotion (EE) is an important predictor of relapse across psychiatric disorders (Butzlaff & Hooley, 1998) and in bipolar disorder has been shown to moderate the response of patients to psychosocial treatments (Miklowitz et al., 2009). Operationally, EE refers to the number of critical comments, presence/absence of hostility, and/or the degree of emotional overinvolvement (EOI) exhibited by a relative. Whereas criticism and hostility refer to emotionally negative statements of the relative about the patient, EOI refers to the relative’s intrusiveness or overprotective behavior, excessively self-sacrificing or overly devoted behavior, or exaggerated emotional responses to the patient’s well-being (Leff & Vaughn, 1985).
The criticism component of EE has received extensive study as a predictor, with the general finding that patients from families in which relatives express a high number of critical comments are at an increased risk of relapse or experience less improvement in symptoms compared with patients whose family members are low in criticism (e.g., Hooley, Orley, & Teasdale; Kim & Miklowitz, 2004; also see Wearden, Tarrier, Barrowclough, Zastony, & Rahill, 2000 for a review). Several studies have demonstrated an association between EOI among relatives and treatment outcome among patients, although findings have been inconsistent. For example, EOI predicted premature treatment dropout for individuals with anxiety disorders (Chambless & Steketee, 1999) and eating disorders (Szmukler, Eisler, Russell, & Dare, 1985) as well as higher levels of residual symptoms following hospitalization among patients with schizophrenia (Miklowitz, Goldstein, & Falloon, 1983). In contrast, among patients hospitalized with borderline personality disorder (Hooley & Hoffman, 1999), EOI in relatives was associated with a lower likelihood of rehospitalization and higher global functioning a year after discharge. Positive associations between relatives’ EOI and patients’ outcomes were also observed by O’Brien et al. (2006), who found that, among adolescents at risk for psychosis, relatives’ EOI predicted improvements in negative symptoms and social functioning three months after initial assessment.
The traditional method for assessing EOI is to assign a single, global score based on the relative’s behavior exhibited during the Camberwell Family Interview (CFI; Vaughn & Leff, 1976), a semi-structured interview conducted with the relative in the patient’s absence. This method of assessment makes it difficult to determine which aspect(s) of EOI are associated with better or worse outcomes for patients suffering from a given psychiatric disorder (King, 2000; Wearden et al., 2000; Wiedemann, Rayki, Feinstein, Hahlweg, 2002). Hooley and Hoffman (1999) have suggested that the excessive self-sacrifice and exaggerated emotional response components of EOI may be emotionally validating to individuals with borderline personality disorder and decrease their desire to self-injure. In contrast, these same behaviors by relatives may be experienced as stressful by someone undergoing exposure therapy for treatment of an anxiety disorder (Chambless & Steketee, 1999).
A number of studies have demonstrated that relatives’ criticism about patients expressed during the CFI corresponds with how critical they are during face-to-face interactions with patients (e.g., Chambless, Bryan, Aiken, Steketee, & Hooley, 1999; Hahlweg et al., 1989; Hooley, 1986). Two studies have demonstrated that relatives’ EOI exhibited during the CFI corresponds with how relatives interact with patients. Using a sample of adult outpatients with agoraphobia and obsessive-compulsive disorder, Fredman, Chambless, and Steketee (2004) demonstrated evidence for the reliability and construct validity of an observational coding system for EOI that permits individual ratings of relatives’ intrusiveness, excessive self-sacrifice, and exaggerated emotional response while they are interacting with patients. Findings were subsequently replicated by Fredman, Baucom, Miklowitz, and Stanton (2008) in a sample of adults with bipolar disorder but also extended by demonstrating the utility of differentiating between family members’ appropriate emotional involvement (i.e., appropriate intrusiveness, self-sacrifice, and emotional response) and inappropriate involvement.
High levels of emotional engagement with patients in the form of unsolicited advice-giving, promoting the patient’s well-being ahead of one’s own, and/or distress about the patient’s well-being might be reasonable in the context of a severe and recurrent mental illness such as bipolar disorder (Miklowitz & Johnson, 2009). For example, it might be appropriate for the relative to remind the patient repeatedly to take mood stabilizing medication if the patient is showing signs of mood deterioration, but unreasonable or inappropriate for the relative to make constant reminders about medications if the patient is euthymic. Similarly, it might be appropriate for the relative of an individual with bipolar disorder to forgo a vacation to assist the patient in paying for medication or therapy sessions, but inappropriate for a family member to forgo saving for retirement in order to provide ongoing financial assistance to a patient who is unable to hold a job due to medication noncompliance or refusal to maintain a regular sleep/wake cycle.
Previous work has demonstrated that patients with bipolar disorder who receive medication plus family-focused therapy (FFT; Miklowitz & Goldstein, 1997), consisting of psychoeducation about coping with bipolar disorder and instruction in communication and problem-solving skills, showed more rapid recovery from illness episodes and longer periods prior to recurrence over 1–2 years compared with patients who received medication plus brief psychoeducation (Miklowitz, George, Richards, Simoneau, & Suddath, 2003; Miklowitz, Richards, et al., 2003; Miklowitz et al., 2007; Miklowitz et al., 2008). In a study of adolescents with bipolar disorder, the effects of FFT were most pronounced among patients from high EE (primarily highly critical) families compared with low EE families (Miklowitz et al., 2009). However, data are lacking about the role of relatives’ emotional involvement in predicting who best responds to family-based interventions. Possibly, patients with bipolar disorder whose caregivers show low levels of appropriate involvement and/or high levels of inappropriate involvement are more likely to benefit from the psychoeducational and skill-based strategies central to FFT or similar treatments.
Prior work by Kim and Miklowitz (2004), who used a sample of patients who had participated in one of two family-based treatment outcome studies for bipolar disorder (Miklowitz, George, et al., 2003; Miklowitz, Richards, et al., 2003), revealed that patients from highly critical families experienced less improvement in manic and depressive symptoms over a two-year period than patients from families low in criticism. Further, family-based treatment, consisting of either FFT or a protocol that combined FFT with individual therapy, attenuated the association between criticism and manic symptoms over time but not between criticism and depression. In this same investigation, CFI-assessed EOI did not predict treatment outcome for manic or depressive symptoms, nor did it interact with treatment condition to predict mood symptoms over the two-year period. However, the methodological limitations associated with the Camberwell Family Interview may have obscured the relevance of the emotional involvement/overinvolvement construct to the course of bipolar disorder. Thus, we felt that it was important to disaggregate the EOI construct into separate ratings for appropriate and inappropriate involvement and in different behavioral domains (i.e., intrusiveness, self-sacrifice, and distress related to the patient’s well-being) to better determine the clinical relevance of this construct in the context of bipolar disorder.
The primary objective of the present study was to examine family members’ appropriate and inappropriate emotional involvement1 during face-to-face interactions with patients with bipolar disorder as a moderator of clinical response to family therapy for bipolar disorder. Patients received standard pharmacotherapy for bipolar disorder plus (1) “family-based therapy” (FBT), which refers to FFT alone or an integrated family and individual therapy, or (2) a 2-session standard community care treatment (crisis management, or CM). We hypothesized that when family members demonstrated high levels of inappropriate emotional involvement or low levels of appropriate emotional involvement prior to treatment, medication plus FBT would be associated with greater reductions in mood symptoms over a two-year period than medication plus brief psychoeducation. In contrast, when family members demonstrated low levels of inappropriate emotional involvement behaviors or high levels of appropriate involvement, it was expected that the course of patients’ mood symptoms would not differ significantly between the two treatment groups.
Method
Participants
Patients
Patients (N = 108) were a subsample of adults who participated in one of two family-based treatment trials for bipolar disorder conducted by Miklowitz and colleagues. The first study (Miklowitz, George, et al., 2003; N = 101) was a randomized controlled trial (RCT) comparing medication management plus adjunctive family-focused therapy (FFT) and medication management plus crisis management (CM), a 2-session psychoeducational control designed to emulate standard community care. The second study (Miklowitz, Richards, et al., 2003; N = 30) was an open trial of integrated family and individual therapy (IFIT) for bipolar disorder as an adjunct to medication management that consisted of FFT and alternating weekly individual-interpersonal therapy. The 108 participants selected for the current study represent all patients who received medication plus adjunctive FFT (n = 65: 28 from the RCT, 30 from the open IFIT trial, and 7 who received open FFT in the context of a treatment development study (Miklowitz, Frank, & George, 1996) and met identical inclusion criteria to those patients in the other two studies) or medication plus crisis management, CM (n = 43).2 All patients participated in a videotaped family interactional task with one of their relatives (e.g., spouse or parent) prior to receiving study-based psychosocial treatments.
FFT (Mikowitz & Goldstein, 1997) is a 21-session, 9-month family therapy that consists of psychoeducation about the illness (i.e., a review of symptoms, including early warning signs of relapse, education about risk and protective factors, rehearsal of strategies for relapse prevention), communication enhancement training, and problem-solving skills training. The integrated family and individual treatment consisted of up to 50 sessions of alternating, weekly FFT and interpersonal and social rhythm therapy (Frank, Swartz, & Kupfer, 2000), the latter of which is designed to increase mood stability through regulating daily and nightly routines and management of interpersonal problems. Crisis management (CM), the control condition, consisted of 2 sessions of family-based psychoeducation. Patients in both treatments received emergency sessions when experiencing an exacerbation of mood symptoms or severe family conflict and assistance with hospitalization in the event of a relapse. All patients received standard medications for bipolar disorder as administered by a study-affiliated psychiatrist or community physician. Details regarding pharmacotherapy regimens are fully described in Miklowitz, George, et al. (2003).
Inclusion criteria for the treatment studies were that patients met DSM-IV (American Psychiatric Association, 1994) criteria for a manic, depressed, hypomanic or mixed episode within the three months prior to the family interactional assessment and for lifetime bipolar I or II disorder; were willing to take mood stabilizing medications or antipsychotic agents; and had regular contact with a family member (≥4 hours per week). Exclusion criteria were any signs of a developmental disability or neurological disorder, or any evidence of alcohol or substance use disorder within the previous six months. Patients were recruited while in the hospital for a mood episode or as outpatients during a mood exacerbation. All participants provided written informed consent. The study was approved by the University of Colorado at Boulder Human Research Committee and later by the Institutional Review Board at the University of North Carolina at Chapel Hill.
The Structured Clinical Interview for DSM-IV-Patient Version (SCID-P; First, Spitzer, Gibbon, & Williams, 1995) was used to confirm that patients met DSM-IV (American Psychiatric Association, 1994) criteria for bipolar I (88%) or II (12%) disorder. Interrater reliabilities for SCID-P items ranged from 0.71 to 0.87 (Cohen’s κ, p <.001).
Relatives
Interactional data were collected from adult relatives who lived with the patient or were in regular contact with the patient as defined above. Half of the relatives were female (53%), and approximately two-thirds of the relatives (62%) were spouses or romantic partners. The remainder consisted of parents (28%) or another adult relative, such as a sibling or adult child (10%).
Measures
Mood ratings
The Schedule for Affective Disorders and Schizophrenia, Change Version (SADS-C; Spitzer & Endicott, 1978) is a 36-item interview-based instrument designed to assess the worst period of mood symptoms, psychosis, and anxiety symptoms during a given study interval. It has demonstrated convergent validity with other measures of psychopathology (Endicott & Spitzer, 1978). The SADS-C was administered to patients upon study entry (covering the three months prior to study entry), one month after study entry and prior to the initiation of any psychosocial treatments, three, six, and nine months after study entry, and at 12, 18, and 24 months after study entry. Items were rated from 1 (absent) to 7 (very extreme). Interrater reliability, assessed using intraclass correlations for SADS-C composite total affective symptoms, mania scores, and depression scores, ranged from 0.81 to 0.92 (p < .001 for all).
Family interaction task
Family interactions were completed in a laboratory setting an average of 5.23 weeks (SD = 4.07) after patients were enrolled in the study and occurred prior to patients’ receiving study-based treatment. Each patient-relative dyad engaged in two consecutively completed 10-minute problem-solving interactions in which they were asked to discuss and resolve an issue of concern in their relationship (e.g., communication difficulties, patient self-management) while the investigator was out of the room. One interaction was based on a topic generated by the patient, and the other was based on a topic generated by the relative. Patient-selected topics and relative-selected topics were counterbalanced across interactions. Procedures for conducting the interactions are more fully described in Simoneau, Saleem, and Miklowitz (1998).
Observation coding system for emotional involvement/overinvolvement
An observational coding system for appropriate emotional involvement and inappropriate emotional involvement within the context of bipolar disorder (Fredman et al., 2008) was applied to the 10-minute pretreatment problem-solving interactions between patients and their relatives. The coding system yielded ratings for appropriate and inappropriate emotional involvement by relatives in the following domains: (a) unsolicited advice giving or checking on the patient (intrusiveness); (b) the relative’s willingness to endure negative consequences as a result of the patient’s illness or to sacrifice his or her own well-being to promote the patient’s well-being (self-sacrifice); and (c) concern for the patient’s well-being or identification with the patient (emotional response). Relatives were assigned ratings for appropriate intrusiveness, self-sacrifice, and emotional response to the patient’s well-being and inappropriate intrusiveness, self-sacrifice, and emotional response for the patient-generated topic. They were also assigned six ratings for the relative-generated topic. Each of the six ratings was made on a 1–5 scale in which 1 indicated the absence of the behavior and 5 reflected an extremely high amount of the behavior.
In order to capture relatives’ behavior in its most pronounced form during direct contact with patients, the highest level of a relative’s behavior (e.g., inappropriate self-sacrifice) during either of the two patient-relative interactions was used instead of averaging the two ratings. This strategy was also used when validating the coding system with this sample at baseline. This method reflects our position that individuals with psychological disorders are most likely to be affected by familial behaviors in their most pronounced form, even if these extreme behaviors occur infrequently.
Paired t-tests revealed that ratings across the six scales did not differ significantly depending on whether the patient or the relative had selected the topic (ps > .05). Thus, the relative’s highest rating for each of the six scales across the two interactions was selected for data analysis. Observed ranges for each of the six scales was 1–5. All interactions were rated by Steffany J. Fredman. An undergraduate research assistant who received 10 hours of training prior to coding as well as ongoing training throughout the study to protect against coder drift rated one-third of the interactions for reliability purposes. Both Steffany J. Fredman and the research assistant were uninformed as to patients’ treatment condition and outcome scores for mania and depression. Interrater reliabilities (Shrout & Fleiss, 1979) for the 6 scales ranged from .70 to .86. Prior work conducted with this sample at baseline (Fredman et al., 2008) supported the measure’s convergent validity with respect to CFI-assessed EOI and the measure’s discriminant validity with respect to CFI-assessed criticism and warmth.
Statistical Analyses
A multilevel modeling approach (Raudenbush & Bryk, 2002) using PROC MIXED in SAS 9.3 with restricted maximum likelihood (REML) was used to estimate trajectories of change in manic and depressive symptoms over time (as measured by the SADS-C), using time, treatment group (CM vs. FBT), and relatives’ baseline emotional involvement as independent variables. Time was coded in weeks since study entry, treatment group was dummy coded “0” for CM and “1” for FBT, and emotional involvement variables were grand mean centered. Random effects were estimated for both the intercept and the slope for time to account for individual variability around the intercept and slope for time, respectively. Models were built sequentially for manic and depressive symptoms, starting with an intercept only model (model 1 in Tables 2–4), progressing to an unconditional model in which time was the only predictor (model 2 in Tables 2–4), proceeding to a conditional model that included treatment and relevant covariates (model 3 in Tables 2–4), and culminating with fully conditional models that included time, treatment, an emotional involvement variable, and relevant covariates (model 4 in Tables 2–4). For all growth models, robust standard errors were used to calculate p-values.
Table 2.
Fixed Effects Estimates (Top) and Variance-Covariance Estimates (Bottoms) for Prediction of Mania Growth Trajectory Conditioned on Treatment and Inappropriate Self-Sacrifice
| Parameter | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| Fixed effects | ||||
|
| ||||
| Intercept | 2.14** (.06) | 2.35** (.07) | 2.30** (.10) | 2.31** (.10) |
| Time | −.0059** (.001) | −.0029 (.002) | −.00091 (.002) | |
| Treatment | .083 (.14) | .072 (.14) | ||
| Inappropriate self-sacrifice | - | .52 (.11) | ||
| Time × treatment | −.0055 (.003) | −.0074** (.003) | ||
| Time × inappropriate self-sacrifice | .0077** (.002) | |||
| Treatment × inappropriate self-sacrifice | −.035 (.14) | |||
| Time × treatment × inappropriate self-sacrifice | −.0067** (.002) | |||
|
| ||||
| Random Effects | ||||
|
| ||||
| Intercept | .19** (.05) | .20** (.07) | .20** (.07) | .21** (.08) |
| Covariance of intercept and time | −.0016 (.001) | −.0016 (.001) | −.0017 (.001) | |
| Time | .000074** (.00003) | .000072** (.00003) | .000054* (.00003) | |
| Residual | .98** (.06) | .88** (.05) | .87** (.05) | .87** (.05) |
Note. Standard errors are in parentheses. Asterisks (*) denote significance, where * is p < .05 and ** is p < .01.
Table 4.
Fixed Effects Estimates (Top) and Variance-Covariance Estimates (Bottoms) for Prediction of Depression Growth Trajectory Conditioned on Treatment and Appropriate Self-Sacrifice Controlling for Sex and Index Episode Polarity
| Parameter | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| Fixed effects | ||||
|
| ||||
| Intercept | 2.45** (.07) | 2.64** (.08) | 2.64** (.16) | 2.67** (.16) |
| Time | −.0056** (.001) | −.0014 (.002) | −.0018 (.002) | |
| Sex | .28* (.11) | .27* (.12) | ||
| Index episode | −.59** (.12) | −.60** (.12) | ||
| Treatment | .21 (.15) | .20 (.15) | ||
| Appropriate self-sacrifice | - | .23* (.10) | ||
| Time × treatment | −.0073** (.002) | −.0070** (.002) | ||
| Time × appropriate self-sacrifice | −.0042* (.002) | |||
| Treatment × appropriate self-sacrifice | −.33* (.14) | |||
| Time × treatment × appropriate self-sacrifice | .0060** (.002) | |||
|
| ||||
| Random Effects | ||||
|
| ||||
| Intercept | .39** (.07) | .58** (.11) | .40** (.08) | .39** (.08) |
| Covariance of intercept and time | −.0042** (.001) | −.0030** (.001) | −.0026* (.001) | |
| Time | .000086** (.00002) | .000079** (.00002) | .000074** (.00002) | |
| Residual | .63** (.04) | .51** (.03) | .51** (.03) | .51 (.03)** |
Note. Standard errors are in parentheses. Asterisks (*) denote significance, where * is p < .05 and ** is p < .01.
We examined baseline patient demographic and illness history characteristics to determine which, if any, should be included as covariates in the longitudinal analyses. Patients in the CM, FFT, and integrated individual and family therapy did not differ significantly from one another with respect to age, socio-economic status (SES), sex, race/ethnicity, number of prior episodes, age at onset, or number of prior hospitalizations (ps > .29), but they did differ with respect to years of education (p < .001) and index episode polarity (p = .04). Both variables, along with patient sex, were included as predictors of mood trajectories in unconditional models of mood symptoms over time. Variables that were not related to manic or depressive symptoms over time were not retained in the conditional models for these outcomes.3
Prior to fitting the conditional models, we confirmed the appropriateness of combining the two family-based treatment groups by comparing the trajectories for manic and depressive symptoms for the FFT (n = 35) and combined family and individual therapy (n = 30) groups using contrast coding and the inclusion of a main effect for the treatment variable and a two-way interaction between time and the treatment variable. As expected, the two-way interaction between time and the treatment group was not significant for mania (p = .78) or depression (p = .60), indicating that the slopes for the two family-based treatment groups did not differ from each other and that it was appropriate to combine them into one treatment group, labeled “family-based treatment” (FBT; total n = 65). Consistent with the assumption that data were missing at random, patients who were missing more data were not more manic or depressed at baseline, nor did they have relatives who displayed higher levels of emotional involvement at study entry.
For the conditional growth models assessing whether relatives’ emotional involvement moderated the interaction between time and treatment in predicting mood symptoms over time, significant three-way interactions between time, treatment, and the emotional involvement variables were probed post hoc. To facilitate interpretation of effects, the six interactional emotional involvement variables were examined in separate growth models for each outcome (i.e., mania and depression). Consistent with procedures described by Peugh (2010), effect sizes for significant three-way interactions were calculated by estimating the percent decrease in slope variability that resulted when the emotional involvement variable (and associated interactions) was included in the model compared with the model that contained only time, treatment, their interaction, and relevant covariates. Treating this percent reduction in variance as f2, we transformed f2 into R2 (R2 = f2/(1 + f2) and subsequently calculated the square root of this value to produce a correlation coefficient, r, that could be interpreted consistent with Cohen’s (1988) recommendations for small (r = .10), medium (r = .30), and large (r = .50) effect sizes.
Results
Effects of Emotional Involvement as a Moderator of Treatment Effects: Manic symptoms
As hypothesized, the three-way interaction between time, treatment, and inappropriate self-sacrifice was significant, as was the three-way interaction between time, treatment, and inappropriate emotional response. Full results for these models are displayed in Tables 2 and 3, respectively. The inclusion of inappropriate self-sacrifice in the model predicting mania was associated with a 25% reduction in slope variability (r = .45, medium-to-large effect), and the inclusion of inappropriate emotional response in the model predicting mania was associated with an 7% reduction in slope variability (r = .25, small-to-medium effect). None of the other interactions (i.e., appropriate and inappropriate intrusiveness, appropriate self-sacrifice, appropriate emotional response) were significant (all ps > .17)4,5
Table 3.
Fixed Effects Estimates (Top) and Variance-Covariance Estimates (Bottoms) for Prediction of Mania Growth Trajectory Conditioned on Treatment and Inappropriate Emotional Response
| Parameter | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| Fixed effects | ||||
|
| ||||
| Intercept | 2.14** (.06) | 2.35** (.07) | 2.30** (.10) | 2.30** (.10) |
| Time | −.0059** (.001) | −.0029 (.002) | −.0034 (.002) | |
| Treatment | .083 (.14) | .095 (.13) | ||
| Inappropriate emotional response | - | −.014 (.16) | ||
| Time × treatment | −.0055 (.003) | −.0051 (.003) | ||
| Time × inappropriate emotional response | .0064 (.004) | |||
| Treatment × inappropriate emotional response | .19 (.19) | |||
| Time × treatment × inappropriate emotional response | −.0089* (.004) | |||
|
| ||||
| Random Effects | ||||
|
| ||||
| Intercept | .19** (.05) | .20** (.07) | .20** (.07) | .21** (.08) |
| Covariance of intercept and time | −.0016 (.001) | −.0016 (.001) | −.0018 (.001) | |
| Time | .000074** (.00003) | .000072** (.00003) | .000067* (.00003) | |
| Residual | .98** (.06) | .88** (.05) | .87** (.05) | .87** (.05) |
Note. Standard errors are in parentheses. Asterisks (*) denote significance, where * is p < .05 and ** is p < .01.
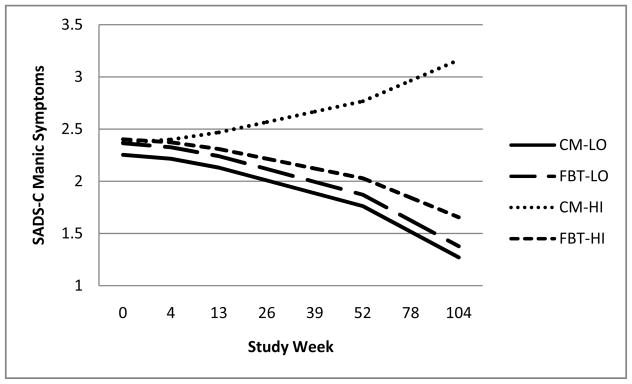
The three-way interaction between time, treatment, and inappropriate self-sacrifice was probed post hoc at low, medium, and high levels of inappropriate self-sacrifice (one standard deviation below the mean, at the mean, and one standard deviation above the mean of inappropriate self-sacrifice, respectively). Examination of the simple slopes revealed that at low levels of inappropriate self-sacrifice, the slope was negative and significant for both groups of patients (γcm = −.0094, p = .0008; γtx = −.0095, p < .0001), indicating that patients became less manic over time regardless of treatment condition. At the mean of inappropriate self-sacrifice, there were differences between the CM and FBT groups: the slope for patients in CM was negative but non-significant (γ = −.0009, p = .68), indicating that patients did not improve; in contrast, the slope for patients in family-based treatment was negative and significant (γ =−.0083, p < .0001), suggesting a significant decrease in manic symptoms. At high levels of inappropriate self-sacrifice, the differences in slopes were even more pronounced: for patients in CM, the slope was positive and significant (γ = .0076, p = .02), indicating that these patients became more manic over time, whereas the slope was negative and significant for patients in FBT (γ = −.0072, p = .002), indicating that these patients became less manic over time (Figure 1).
Figure 1.
Trajectories of manic symptoms as a function of treatment group and relatives’ level of inappropriate self-sacrifice. Note. CM = Crisis Management; FBT = Family-Based Therapy.
The three-way interaction between time, treatment, and inappropriate emotional response was also probed post hoc and revealed the following. At low levels of inappropriate emotional response, the slopes were negative in both groups (γcm = −.0096, p = .005; γtx = −.0062, p = .05). At the mean of inappropriate emotional response, the slope for patients in CM was negative but non-significant (γ = −.0034, p = .13), whereas the slope for patients in FBT was negative and significant (γ = −.0085, p < .0001). At high levels of inappropriate emotional response, the slope for patients in CM was positive and non-significant (γcm = .0028, p = .55), indicating no change in manic symptoms, whereas the slope for patients in FBT was negative and significant (γtx = −.0109, p = .001), indicating improvement.
Effects of Emotional Involvement as a Moderator of Treatment Effects: Depressive Symptoms
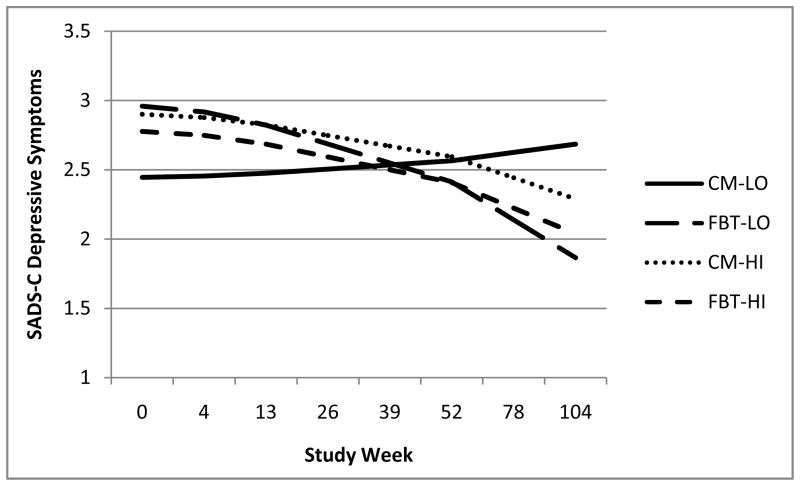
As displayed in Table 4, the three-way interaction between time, treatment, and appropriate self-sacrifice was significant. The interaction between time, treatment, and appropriate intrusiveness was also significant (B = .0038, p = .04). The inclusion of appropriate self-sacrifice in the model predicting depression was associated with a 6% reduction in slope variability (r = .24, small-to-medium effect), and the inclusion of appropriate intrusiveness in the models predicting depression was associated with a 4% reduction in slope variability (r = .19, small effect). None of the three-way interactions with the other emotional involvement variables (inappropriate intrusiveness, inappropriate self-sacrifice, appropriate and inappropriate emotional response) were significant (all ps > .09)6,7.
The three-way interaction between time, treatment, and appropriate self-sacrifice predicting depression was probed post hoc and revealed the following: At low levels of appropriate self-sacrifice, the slope for patients in CM was flat (γ = .0023, p = .40), indicating that these patients did not experience a reduction in depressive symptoms; in contrast, the slope for patients in FBT was negative and significant (γ = −.0105, p < .0001). At the mean of appropriate self-sacrifice, the slope for patients in CM was negative but non-significant (γ = −.0018, p = .30), whereas the slope for patients in FBT was negative and significant (γ = −.0088, p < .0001). At high levels of appropriate self-sacrifice, the slopes for the two groups were both negative and significant (γcm = −.0059, p = .003; γtx = −.0071, p = .0007), suggesting that when relatives made appropriate gestures to indicate their support at baseline, patients became significantly less depressed over time, regardless of whether or not they received family-based treatment.
The three-way interaction between time, treatment, and appropriate intrusiveness was also probed post hoc: At low levels of appropriate intrusiveness, the slope for patients in CM was flat (γ = −.0014, p = .57), whereas the slope for patients in FBT was negative and significant (γ = −.0125, p < .0001). At the mean of appropriate intrusiveness, the slope for patients in CM was flat (γ = −.0014, p = .46), whereas the slope for patients in FBT was negative (γ = −.0084, p < .0001). At high levels of appropriate intrusiveness, the slope for CM was flat (γcm = −.0014, p = .48), and the slope for FBT was negative (γtx = −.0044, p = .02), indicating improvement.
Discussion
In a sample of adults with bipolar disorder undergoing adjunctive FBT or a brief psychoeducational intervention with case management (CM), we sought to determine whether level of relatives’ appropriate and inappropriate emotional involvement moderated the effects of psychosocial intervention on mood symptoms over a two-year period. We observed that, at low levels of family members’ inappropriate self-sacrifice, patients in both treatment groups experienced improvements in manic symptoms, but at medium levels, patients in FBT improved but those in CM did not. At high levels of inappropriate self-sacrifice, patients in CM became more manic over time, whereas patients in FBT experienced significant declines in manic symptoms. At medium and high levels of inappropriate emotional response, patients in FBT improved, whereas those in CM did not. Finally, when relatives showed low and moderate levels of appropriate self-sacrifice, patients in CM did not improve in depression scores, whereas patients in FBT did experience a significant decrease in depressive symptoms over time.
The cause/effect relationship between patients’ symptoms and emotional involvement behaviors in relatives cannot be resolved by this study. Nonetheless, the findings suggest that family intervention may alter an adverse trajectory of symptoms among patients whose family members show an excess of these behaviors in laboratory-based family interactions.
It is noteworthy that the behaviors we have labeled as inappropriate in relatives - namely, self-sacrifice and emotional response – moderated the effects of FBT on manic but not depressive symptoms. In contrast, appropriate self-sacrifice moderated the effects of FBT on depressive but not manic symptoms. The finding that, in the absence of FBT, low and moderate levels of appropriate self-sacrifice were associated with lack of improvement in depressive (but not manic) symptoms parallels findings from naturalistic studies that low levels of social support were associated with a longer time to recovery, greater relapse likelihood, and less improvement of bipolar depressive symptoms (Johnson et al., 1999; Cohen et al., 2004). Thus, appropriate self-sacrifice in relatives may be a proxy for social support and an important protective factor in the course of depressive symptoms in bipolar disorder.
There are several clinical implications from this investigation. First, in addition to attending to negative affective tones (e.g., as in the case of criticism), it is important for clinicians to be sensitized to family members’ self-sacrificing behaviors and distress related to the disorder as a way of identifying high-risk families who may benefit from family-based treatment. Providing family therapy for bipolar disorder on a large-scale basis is economically unviable in most community health systems; furthermore, patients in low stress households may experience improvement in mood symptoms in the absence of family interventions (e.g., Miklowitz et al., 2009; Miller, Keitner, Ryan, Uebelacker, Johnson, & Solomon, 2008). Thus, the use of intensive family-based interventions for patients in high risk environments might be an efficient use of limited clinical resources.
Previous work has demonstrated that a single item measure of perceived criticism predicts outcome in bipolar disorder (Miklowitz, Wisniewski, Miyahara, Otto, & Sachs, 2005; Scott, Colom, Pope, Reinares, & Vieta, 2012). Prior efforts to develop self-report measures of emotional involvement have been conducted with samples of family members of individuals with schizophrenia, and these measures have demonstrated modest concordance with CFI EOI (e.g., Docherty & Serper, 1990; Wiedemann et al., 2002). One study has also demonstrated concordance between perceived expressed emotion, including emotional involvement, by patients with eating disorders and their relatives’ CFI EOI scores (Medina-Pradas, Navarro, López, Grau, & Obiols, 2011). However, data are lacking regarding the predictive validity of these instruments. The development of valid and reliable patient and relative self-report measures of emotional involvement – perhaps using separate scales for the various dimensions of involvement and their perceived appropriateness - could be useful in treatment planning for bipolar disorder provided that they predict outcomes in the context of this condition.
Results from the present investigation also raise questions about mechanisms through which family-based treatment for bipolar disorder might mitigate the association between relatives’ emotional involvement behavior and patients’ improvement during and following treatment. For example, it is possible that through psychoeducation, relatives become better equipped to recognize early signs of manic recurrence. As a result, they may be less willing to accommodate maladaptive patient behaviors (e.g., medication noncompliance or unwillingness to maintain a consistent sleep/wake cycle) and correspondingly less likely to be rated with inappropriately self-sacrificing behaviors. As relatives allow patients to assume more responsibility for their own well-being, they may experience lower levels of caregiver burden and other forms of psychological distress. Consequently, they may be less likely to exhibit inappropriate displays of emotional distress regarding patients’ well-being that might otherwise impede patients’ recovery with respect to manic symptoms.
Family-based therapy may also increase relatives’ provision of appropriate social support that may, in turn, lead to improvements in patients’ depressive symptoms. Appropriate self-sacrifice, as coded in the current observational coding system, may be a proxy for esteem support or instrumental support, such as the willingness to assist the patient in implementing behavioral activation plans (e.g., “I don’t really like to exercise but am willing to keep you company and do it if exercising will help your mood”). Exploring the mediating role of social support in the associations between family-based treatment and patients’ depressive symptoms could elucidate these putative mechanisms.
This study had several limitations. First, problem topics for the family interactions were self-generated and not standardized. In some of the family interactions, patients and their family members discussed the illness, whereas other families discussed areas of family functioning that appeared to be unrelated to the illness (e.g., whether to spend leisure time together versus apart). As a result, relatives might not have been afforded the opportunity to display the full extent of their thoughts, feelings, and behaviors in reaction to their roles as family member. Other limitations were that the sample included patients from two studies with different designs. Notably, the first trial compared FFT with CM based on random assignment; in the second, the individual and family therapy was offered openly within the context of a treatment development study. In addition, the treatment and control conditions were not balanced on the number of sessions, raising the possibility that differences in the trajectory of symptoms in FBT versus CM were a function of the amount of therapy contact rather than the content of sessions.
Most importantly, the current investigation focuses upon one multidimensional construct, family involvement/overinvolvement, which appears to be an important factor in patients’ response to treatment. Yet, family interaction patterns are not restricted to this single phenomenon. As demonstrated in other investigations, additional important aspects of family interaction such as level of criticism and hostility toward the patient also influence the course of the disorder (Kim & Miklowitz, 2004; Miklowitz, Goldstein, Nuechterlein, Snyder, & Mintz, 1988; Yan, Hammen, Cohen, Daley, & Henry, 2004). Various combinations of these variables may represent quite different family environments that call for different treatment emphases. For example, a family in which relatives demonstrate inappropriate self-sacrifice and intrusiveness along with low levels of criticism and hostility might make the patient feel infantilized. On the other hand, a family with high levels of inappropriate self-sacrifice and intrusion along with high levels of criticism and hostility might make the patient feel guilty about the burden of the illness on family members. In the former case, treatment might emphasize the teaching of problem-solving skills designed to help families negotiate roles in such a way that promotes the patient’s autonomy and sense of responsibility for maintaining health. In the latter, family treatment might first aim to reduce negative affective expression between family members through the use of communication skills training and then shift to a focus on role negotiation. In future research, it will be important to consider how various family attributes interact in influencing a patient’s response to psychosocial interventions.
Finally, this study was conducted with patients who had already developed bipolar disorder. Thus, we cannot determine whether high levels of self-sacrifice or emotional response among parents or spouses develop in reaction to the patient’s recurrences or are features of the relationship even when patients are well. Examining family interactions in which a child is genetically vulnerable to mood or psychotic disorders may help to disentangle the cause/effect relationship between family reactivity and patients’ prodromal symptoms, at least in families in which the relative is a parent. The few studies that have examined high-risk samples suggest that parental EE may escalate in reaction to the functional deterioration of an offspring with prodromal signs of psychiatric disorder but may also be a stressor in the subsequent course of the illness (McFarlane & Cook, 2007; Miklowitz, 2004).
In summary, the current investigation builds on the efforts of others who have identified criticism and other negative behaviors by family members as an impediment to recovery by considering the construct of emotional involvement as well. As such, it adds to the list of family variables that should be targeted in the context of family-based interventions for bipolar disorder and other conditions involving affective dysregulation.
Supplementary Material
Figure 2.
Trajectories of depressive symptoms as a function of treatment group and relatives’ level of appropriate self-sacrifice. Note. CM = Crisis Management; FBT = Family-Based Therapy.
Table 1.
Patient Demographics, Illness, and Emotional Involvement Variables
| Variable | All groups (n = 108) | CM (n = 43) | FFT (n = 35) | IFIT (n = 30) | p-value comparing CM, FFT, and IFIT groups |
|---|---|---|---|---|---|
| Age | 35.61 (10.07) | 34.65 (10.42) | 35.49 (8.56) | 37.13 (11.27) | .59 |
| SES (Hollingshead-Redlich, 1985) | 2.24 (.96) | 2.15 (.94) | 2.39 (.99) | 2.20 (1.03) | .58 |
| Number of females (%) | 62 (57%) | 28 (65%) | 20 (57%) | 14 (47%) | .29 |
| Number Caucasian (%) | 101 (93%) | 40 (93%) | 32 (91%) | 29 (97%) | .68 |
| Years of education (SD) | 14.45 (2.39) | 13.79 (2.03) | 14.00 (2.54) | 15.90 (2.14) | <.001 |
| Prior episodes | 4.43 (3.76) | 4.16 (3.94) | 4.57 (3.79) | 4.92 (3.43) | .81 |
| Age at onset (SD) | 23.20 (9.97) | 24.56 (10.32) | 22.97 (8.94) | 21.44 (10.73) | .45 |
| Number of prior hospitalizations (SD) | 2.14 (3.28) | 2.21 (2.36) | 2.26 (3.22) | 1.85 (4.52) | .87 |
| Index episode polarity (%) | |||||
| Depressed | 25 (23%) | 5 (20%) | 9 (36%) | 11 (44%) | .04 |
| Manic | 53 (49%) | 25 (47%) | 13 (25%) | 15 (28%) | |
| Mixed | 30 (28%) | 13 (43%) | 13 (43%) | 4 (14%) | |
| Symptom severity (SD) | |||||
| SADS-C Mania | 3.18 (1.26) | 3.21 (1.14) | 3.24 (1.41) | 3.05 (1.27) | .81 |
| SADS-C Depression | 2.90 (1.09) | 2.66 (1.08) | 3.13 (1.09) | 2.98 (1.09) | .16 |
| Emotional involvement (SD) | |||||
| Appropriate intrusiveness | 1.91 (1.06) | 1.93 (1.16) | 1.89 (1.07) | 1.90 (.93) | .98 |
| Appropriate self-sacrifice | 1.99 (.97) | 1.88 (.91) | 1.83 (.95) | 2.33 (1.03) | .07 |
| Appropriate emotional response | 1.90 (1.17) | 1.77 (1.11) | 2.14 (1.29) | 1.80 (1.10) | .32 |
| Inappropriate intrusiveness | 2.05 (1.12) | 2.14 (1.01) | 2.26 (1.31) | 1.67 (.96) | .08 |
| Inappropriate self-sacrifice | 1.60 (1.11) | 1.40 (.82) | 1.91 (1.38) | 1.53 (1.07) | .11 |
| Inappropriate emotional response | 1.54 (.96) | 1.58 (.88) | 1.63 (1.11) | 1.37 (.89) | .51 |
Note. CM = Crisis Management; FFT = Family Focused Therapy; IFIT = Integrated Family and Individual Therapy; SES = socio-economic status; SADS-C = Schedule for Affective Disorders and Schizophrenia-Change Version.
Acknowledgments
This study was conducted in partial fulfillment of the requirements for the doctoral degree in the Department of Psychology at the University of North Carolina at Chapel Hill for Steffany J. Fredman and was supported by National Institute of Mental Health grants MH72124 (to Steffany J. Fredman), MH43931, MH55101, MH62555, and MH93676, Grant 9009473A from the John D. and Catherine T. MacArthur Foundation Network on the Psychobiology of Depression, and a Distinguished Investigator Award from the National Alliance for Research on Schizophrenia and Depression (to David J. Miklowitz). Dr. Miklowitz receives book royalties from Guilford Press and John Wiley and Sons. We gratefully acknowledge Elizabeth Dulin, Jillian Horne, Randi Lane, and Jonathan Schulz for their assistance coding the videotaped interactions. We also thank Jeffrey Richards for his assistance with database management and Ruth Baldasaro, Brian Baucom, Ph.D., Galena Rhoades, Ph.D., Michael Rovine, Ph.D., Michael Suvak, Ph.D., and Chris Wiesen, Ph.D., for their assistance with data analysis.
Footnotes
We use the term “emotional involvement” rather than “emotional overinvolvement” because the CFI emotional overinvolvement (EOI) scale appears to be misnamed. The CFI EOI scale captures relatives’ emotional involvement, not just overinvolvement, which represents the upper end of the scale.
Thirty patients from the Miklowitz, George, et al. (2003) randomized controlled trial were not included in the present study because the baseline family interactional assessment was not completed (n = 28) or was inaudible (n = 2). The patients who were not included were compared with those who were included on a number of demographic and illness variables, including age, sex, race, SES, years of education, age at onset, number of prior episodes, index episode polarity, number of prior hospitalizations, baseline mania, and baseline depression. The two groups of patients did not differ significantly with respect to age, sex, age at onset, number of prior episodes, index episode polarity, number of prior hospitalizations, or baseline mania severity (all ps > .10). Compared with patients who participated in the videotaped interactions, those who did not or whose interactions were inaudible were less depressed (p = .04), had fewer years of education (p = .047), had lower SES (p = .01), and were more likely to be non-Caucasian (p = .002).
Patients who entered the study in a manic or hypomanic state demonstrated lower levels of depression throughout the follow-up period. Furthermore, female patients had higher levels of depression than males throughout the study period.
The pattern of results was virtually identical when conducted on just the subsample of 71 patients who participated in the randomized controlled trial of FFT versus CM. The three-way interaction between time, treatment, and inappropriate self-sacrifice in predicting mania was in the same direction, but the p-value increased from .005 to .046. The p-value also increased for the three-way interaction between time, treatment, and inappropriate emotional response in predicting mania from p = .03 to p = .08. The results are presented on the fully available sample (n = 108) to maximize statistical power.
In light of the non-normal distribution of the emotional involvement variables, the variables were transformed by centering at the median rather than the mean and standardizing by the interquartile range. Re-running the multilevel models with these transformed variables produced an identical pattern of results.
An identical pattern of findings was obtained when conducted on just the subsample of 71 patients who participated in the randomized controlled trial of FFT versus CM. The p-value associated with the three-way interaction between time, treatment, and appropriate self-sacrifice in predicting depression increased from p = .006 to .03, and the p-value associated with the three-way interaction between time, treatment, and appropriate intrusiveness decreased from p = .04 to p = .007. Results are presented on the fully available sample (n = 108).
Re-running the multilevel models with emotional involvement variables centered at the median and standardized by the interquartile range produced an identical pattern of results.
Contributor Information
Steffany J. Fredman, The Pennsylvania State University
Donald H. Baucom, University of North Carolina at Chapel Hill
Sara Boeding, University of North Carolina at Chapel Hill.
David J. Miklowitz, University of California at Los Angeles
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse: A meta-analysis. Archives of General Psychiatry. 1998;55:547–552. doi: 10.1001/archpsyc.55.6.547. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Bryan AD, Aiken LS, Steketee G, Hooley JM. The structure of expressed emotion: A three-construct representation. Psychological Assessment. 1999;11:67–76. doi: 10.1037/1040-3590.11.1.67. [DOI] [Google Scholar]
- Chambless DL, Steketee G. Expressed emotion and behavior therapy outcome: A prospective study with obsessive-compulsive and agoraphobic outpatients. Journal of Consulting and Clinical Psychology. 1999;67:658–665. doi: 10.1037//0022-006X.67.5.658. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- Cohen AN, Hammen C, Henry RM, Daley SE. Effects of stress and social support on recurrence in bipolar disorder. Journal of Affective Disorders. 2004;82:143–147. doi: 10.1016/j.jad.2003.10.008. [DOI] [PubMed] [Google Scholar]
- Docherty NM, Serper MR. Development and preliminary validation of a questionnaire assessment of expressed emotion. Psychological Reports. 1990;67:279–287. doi: 10.2466/pr0.1990.67.1.279. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: The Schedule for Affective Disorders and Schizophrenia. Archives of General Psychiatry. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID-I/P) New York, NY: Biometric Institute, New York State Psychiatric Institute; 1995. [Google Scholar]
- Frank E, Swartz HA, Kupfer DJ. Interpersonal and social rhythm therapy: Managing the chaos of bipolar disorder. Biological Psychiatry. 2000;48:593–604. doi: 10.1016/S0006-3223(00)00969-0. [DOI] [PubMed] [Google Scholar]
- Fredman SJ, Chambless DL, Steketee G. Development and validation of an observational coding system for emotional overinvolvement. Journal of Family Psychology. 2004;18:339–347. doi: 10.1037/0893-3200.18.2.339. [DOI] [PubMed] [Google Scholar]
- Fredman SJ, Baucom DH, Miklowitz DJ, Stanton SE. Observed emotional involvement and overinvolvement in families of patients with bipolar disorder. Journal of Family Psychology. 2008;22:71–79. doi: 10.1037/0893-3200.22.1.71. [DOI] [PubMed] [Google Scholar]
- Hahlweg K, Goldstein MJ, Nuechterlein KH, Magaña AB, Mintz J, Doane JA, Snyder KS. Expressed emotion and patient-relative interaction in families of recent onset schizophrenics. Journal of Consulting and Clinical Psychology. 1989;57:11–18. doi: 10.1037//0022-006X.57.1.11. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB, Redlich FC. Social class and mental illness: A community study. New York: Wiley; 1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooley JM. Expressed emotion and depression: Interactions between patients and high-versus low-expressed-emotion spouses. Journal of Abnormal Psychology. 1986;95:633–642. doi: 10.1037//0021-843X.95.3.237. [DOI] [PubMed] [Google Scholar]
- Hooley JM, Hoffman PD. Expressed emotion and clinical outcome in borderline personality disorder. American Journal of Psychiatry. 1999;156:1557–1562. doi: 10.1176/ajp.156.10.1557. [DOI] [PubMed] [Google Scholar]
- Hooley JM, Orley J, Teasdale JD. Levels of expressed emotion and relapse in depressed patients. British Journal of Psychiatry. 1986;148:642–647. doi: 10.1192/bjp.148.6.642. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Winett CA, Meyer B, Greenhouse WJ, Miller I. Social support and course of bipolar disorder. Journal of Abnormal Psychology. 1999;108:558–566. doi: 10.1037//0021-843X.108.4.558. [DOI] [PubMed] [Google Scholar]
- Kim EY, Miklowitz DJ. Expressed emotion as a predictor of outcome among bipolar patients undergoing family therapy. Journal of Affective Disorders. 2004;82:343–352. doi: 10.1016/j.jad.2004.02.004. [DOI] [PubMed] [Google Scholar]
- King S. Is expressed emotion cause or effect in the mothers of schizophrenic young adults? Schizophrenia Research. 2000;45:65–78. doi: 10.1016/S0920-9964(99)00174-7. [DOI] [PubMed] [Google Scholar]
- Leff J, Vaughn C. Expressed emotion in families: Its significance for mental illness. New York: Guilford; 1985. [Google Scholar]
- McFarlane WR, Cook WL. Family expressed emotion prior to onset of psychosis. Family Process. 2007;46:185–197. doi: 10.1111/j.1545-5300.2007.00203.x. [DOI] [PubMed] [Google Scholar]
- Medina-Pradas C, Navarro JB, López SR, Grau A, Obiols JE. Further development of a scale of perceived expressed emotion and its evaluation in a sample of patients with eating disorders. Psychiatry Research. 2011;190:291–296. doi: 10.1016/j.psychres.2011.06.011. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ. The role of family systems in severe and recurrent psychiatric disorders: A developmental psychopathology view. Development and Psychopathology. 2004;16:667–688. doi: 10.1017/S0954579404004729. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Axelson DA, Birmaher B, George EL, Taylor DO, Schneck CD, Brent DA. Family-focused treatment for adolescents with bipolar disorder: Results of a 2-year randomized trial. Archives of General Psychiatry. 2008;65:1053–61. doi: 10.1001/archpsyc.65.9.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Axelson DA, George EL, Taylor DO, Schneck CD, Sullivan AE, Birmaher B. Expressed emotion moderates the effects of family-focused treatment for bipolar adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:643–51. doi: 10.1097/CHI.0b013e3181a0ab9d. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Frank E, George EL. New psychosocial treatments for the outpatient management of bipolar disorder. Psychopharmacology Bulletin. 1996;32:613–621. [PubMed] [Google Scholar]
- Miklowitz DJ, George EL, Richards JA, Simoneau TL, Suddath RL. A randomized study of family-focused psychoeducation and pharmacotherapy in the outpatient management of bipolar disorder. Archives of General Psychiatry. 2003;60:904–12. doi: 10.1001/archpsyc.60.9.904. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Goldstein MJ. Bipolar disorder: A family-focused treatment approach. New York: Guilford; 1997. [Google Scholar]
- Miklowitz DJ, Goldstein MJ, Falloon IR. Premorbid and symptomatic characteristics of schizophrenics from families with high and low levels of expressed emotion. Journal of Abnormal Psychology. 1983;92:359–67. doi: 10.1037//0021-843X.92.3.359. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Goldstein MJ, Nuechterlein KH, Snyder KS, Mintz J. Family factors and the course of bipolar affective disorder. Archives of General Psychiatry. 1988;45:225–31. doi: 10.1001/archpsyc.1988.01800270033004. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Johnson SL. Social and familial risk factors in the course of bipolar disorder: Basic processes and relevant interventions. Clinical Psychology: Science and Practice. 2009;16:281–296. doi: 10.1111/j.1468-2850.2009.01166.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Wisniewski SR, Kogan JN, Sachs GS. Psychosocial treatments for bipolar depression: A 1-year randomized trial from the Systematic Treatment Enhancement Program. Archives of General Psychiatry. 2007;64:419–26. doi: 10.1001/archpsyc.64.4.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Richards JA, George EL, Frank E, Suddath RL, Powell KB, Sacher JA. Integrated family and individual therapy for bipolar disorder: Results of a treatment development study. Journal of Clinical Psychiatry. 2003;64:182–191. doi: 10.4088/JCP.v64n0211. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Wisniewski SR, Miyahara S, Otto MW, Sachs GS. Perceived criticism from family members as a predictor of the 1-year course of bipolar disorder. Psychiatry Research. 2005;136:101–11. doi: 10.1016/j.psychres.2005.04.005. [DOI] [PubMed] [Google Scholar]
- Miller IW, Keitner GI, Ryan CE, Uebelacker LA, Johnson SL, Solomon DA. Family treatment for bipolar disorder: Family impairment by treatment interactions. Journal of Clinical Psychiatry. 2008;69:732–40. doi: 10.4088/JCP.v69n0506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien MP, Gordon JL, Bearden CE, Lopez SR, Kopelowicz A, Cannon TD. Positive family environment predicts improvement in symptoms and social functioning among adolescents at imminent risk for onset of psychosis. Schizophrenia Research. 2006;81:269–75. doi: 10.1016/j.schres.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Peugh JL. A practical guide to multilevel modeling. Journal of School Psychology. 2010;48:85–112. doi: 10.1016/j.jsp.2009.09.002. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Scott J, Colom F, Pope M, Reinares M, Vieta E. The prognostic role of perceived criticism, medication adherence and family knowledge in bipolar disorders. Journal of Affective Disorders. 2012;142:72–76. doi: 10.1016/j.jad.2012.04.005. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Simoneau TL, Miklowitz DJ, Saleem R. Expressed emotion and interactional patterns in the families of bipolar patients. Journal of Abnormal Psychology. 1998;107:497–507. doi: 10.1037//0021-843X.107.3.497. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J. Schedule for Affective Disorders and Schizophrenia, Change Version. New York: New York State Psychiatric Institute; 1978. [Google Scholar]
- Szmukler GI, Eisler I, Russell GF, Dare C. Anorexia nervosa, parental “expressed emotion” and dropping out of treatment. British Journal of Psychiatry. 1985;147:265–271. doi: 10.1192/bjp.147.3.265. [DOI] [PubMed] [Google Scholar]
- Vaughn CE, Leff JP. The measurement of expressed emotion in the families of psychiatric patients. British Journal of Social and Clinical Psychology. 1976;15:157–165. doi: 10.1111/j.2044-8260.1976.tb00021.x. [DOI] [PubMed] [Google Scholar]
- Wearden AJ, Tarrier N, Barrowclough C, Zastony TR, Rahill AA. A review of expressed emotion research in health care. Clinical Psychology Review. 2000;20:633–666. doi: 10.1016/S0272-7358(99)00008-2. [DOI] [PubMed] [Google Scholar]
- Wiedemann G, Rayki O, Feinstein E, Hahlweg K. The Family Questionnaire: Development and validation of a new self-report scale for assessing expressed emotion. Psychiatry Research. 2002;109:265–279. doi: 10.1016/S0165-1781(02)00023-9. [DOI] [PubMed] [Google Scholar]
- Yan LJ, Hammen C, Cohen AN, Daley SE, Henry RM. Expressed emotion versus relationship quality variables in the prediction of recurrence in bipolar patients. Journal of Affective Disorders. 2004;83:199–206. doi: 10.1016/j.jad.2004.08.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.