Abstract
Objective
Despite treatment availability, many cancer patients experience severe pain. Although patient assessments of care are increasingly employed to evaluate quality of care, little is known about its association with cancer symptom burden. The objective of our study was to examine the association between patient-reported quality of care and pain severity in a nationally representative cohort of cancer patients.
Method
Quality of care was measured in three domains: physician communication, care coordination/responsiveness, and nursing care. Quality scores were dichotomized as optimal versus nonoptimal. Pain was measured on a scale of 0 (least) to 100 (worst). We utilized multivariable linear regression to examine the association between patient-reported quality of care and pain severity.
Results
The analytic sample included 2,746 individuals. Fifty and 54% of patients, respectively, rated physician communication and care coordination/responsiveness as nonoptimal; 28% rated nursing care as nonoptimal. In adjusted models, rating physician communication as nonoptimal (versus optimal) was associated with a 1.8-point higher pain severity (p = 0.018), and rating care coordination/responsiveness as nonoptimal was associated with a 2.2-point higher pain severity (p = 0.006).
Significance of results
Patient-reported quality of care was significantly associated with pain severity, although the differences were small. Interventions targeting physician communication and care coordination/responsiveness may result in improved pain control for some patients.
Keywords: Cancer pain, Quality of care, Patient satisfaction, Pain management, Patient-reported outcomes
INTRODUCTION
More than 1.5 million Americans are projected to be diagnosed with cancer in 2014 (Siegel et al., 2014). For many, pain will pose a significant challenge to daily life. Pain is one of the most common and feared consequences of a cancer diagnosis, and, despite the availability of effective therapies, undertreatment of cancer pain is common (van den Beuken-van Ever-dingen et al., 2007). In fact, up to half of cancer patients do not receive appropriate pain management (Deandrea et al., 2008; Fairchild, 2010). Severe cancer pain is associated with diminished quality of life (Tavoli et al., 2008) and with avoidable utilization of ambulatory care and emergency department services (Wagner-Johnston et al., 2010), as well as delay or discontinuation of cancer therapy (McNeill et al., 2004).
Provision of cancer care is complex, frequently involving the participation of multiple specialists, the application of invasive treatments, and management of dynamic and disparate symptoms and side effects. Prior research has found provider communication and coordination of care to be associated with better pain management (Anderson et al., 2002; Antón et al., 2012; Yates et al., 2002), and a recent systematic review highlighted the need for enhanced patient-centered care to improve pain control in cancer (Luckett et al., 2013). While the concept of patient-centered care is not new, progress in integrating the patient into emergent models of cancer care has been inconsistent at best. A recent report by the Institute of Medicine underscored the continuing need to improve communication, coordination, and patient-centeredness in cancer care (National Research Council, 2013).
Patient-reported measures of quality are increasingly being employed to evaluate medical care, including the quality of oncology practice (Ayanian et al., 2005; 2010; Dennison, 2002). Because of the individualized nature of cancer pain and pain management, patient-reported measures of the quality of interpersonal aspects of care, such as physician communication, may be uniquely associated with patient pain in cancer. The majority of prior research on patient-reported quality of care in pain has focused on the specific association among patient satisfaction, pain management, and pain severity (McCracken et al., 1997; Miaskowski et al., 1994; Panteli & Patistea, 2007; Ward&Gordon, 1994). Moreover, the small body of literature linking patient-reported quality of cancer care to symptom burden has looked at satisfaction as a global metric rather than patients’ assessments of specific aspects of care (Avery et al., 2006; von Gruenigen et al., 2006).
To date, patient-reported quality of interpersonal care has not been studied in relation to the cancer pain experience. Consequently, we have a limited understanding of the aspects of interpersonal care that may be appropriate targets for quality improvement efforts aimed at reducing the burden of cancer pain. The purpose of our study was to examine the association between patient assessment of three aspects of interpersonal care—physician communication, coordination/responsiveness of care, and nursing care—and pain severity in a large, nationally representative cohort of colorectal and lung cancer patients (Catalano et al., 2013).
METHODS
Study Population and Survey Methods
Participants in the study came from the Cancer Care Outcomes Research and Surveillance Consortium (CanCORS) prospective cohort study of newly diagnosed colorectal and lung cancer patients, which included nearly 10,000 participants at seven geographically diverse data collection sites throughout the United States.
Participants were recruited between three and five months following diagnosis. Following consent, patients were administered a survey via computer-assisted telephone interview in English, Chinese (Mandarin), or Spanish. Data were collected between 2003 and 2005. Additional details about the CanCORS cohort and study design were reported by Malin and colleagues (2006).
Our analytic cohort included all individuals who completed the survey and reported any pain. Presence of pain was established through responses to two questions: “Have you experienced pain in the past four weeks?” and “Have you been taking medication for pain in the past four weeks?” Individuals responding “yes” to either or both questions were considered to have pain.
Independent Measures
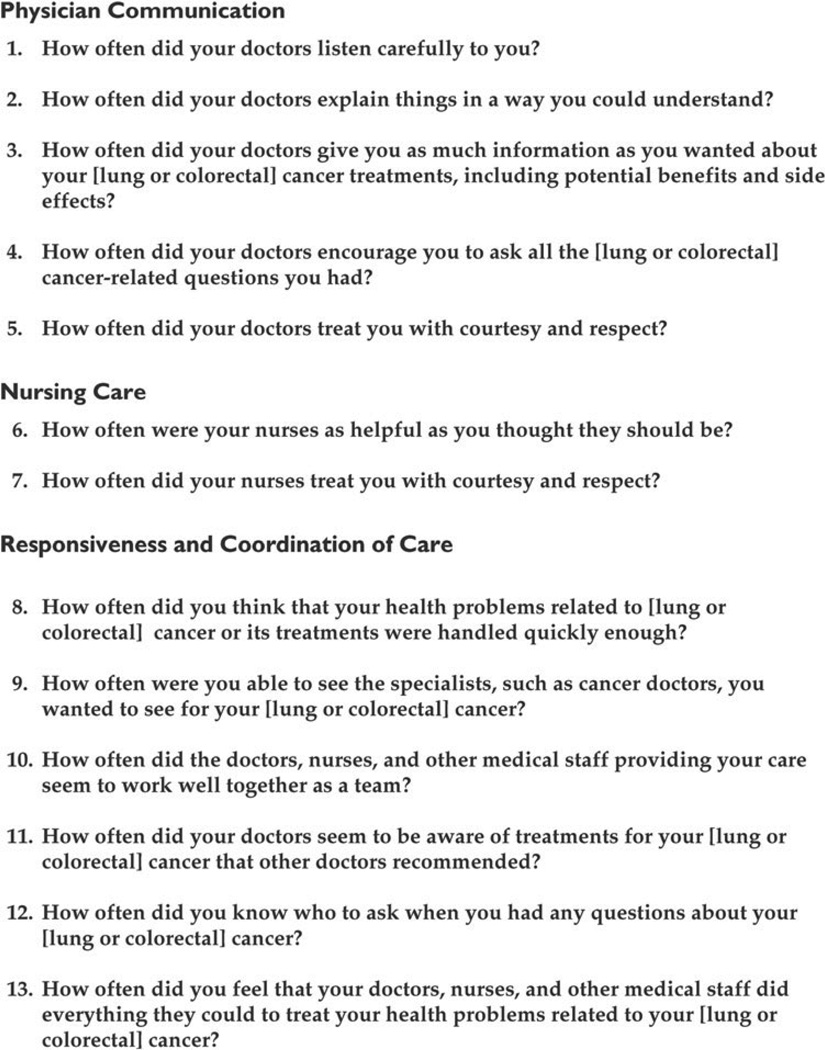
A 13-item instrument developed by the CanCORS study team assessed participants’ assessment of specific aspects of cancer care(Malin et al.,2006).Prior psychometric testing on this instrument established the presence of three distinct factors: coordination/responsiveness of care (six items), nursing care (two items), and physician communication (five items) (Ayanian et al., 2010). Consistent with prior use of the instrument, we transformed scores for each of the factors into 100-point scales, with 100 being the best possible rating of care and 0 the worst. Items and their corresponding factors are presented in Figure 1.
Fig. 1.
Assessment-of-care items and interpersonal care domains.
Scores for the three interpersonal care domains were previously treated as continuous measures (Ayanian et al., 2010). However, because we were specifically interested in the difference between patients reporting no problems with care and those reporting any problems with care, we dichotomized patient ratings into each domain as optimal (100) versus nonoptimal (≤99).
Dependent Measure
The dependent measure in this study was self-reported pain severity, assessed through survey-based administration of the Brief Pain Inventory (BPI) (Cleeland & Ryan, 1994). The BPI asks respondents to rate their pain during the past 4 weeks (worst, least, and average) on a scale of 0 to 10, with 0 being the least imaginable pain and 10 the most. We created an aggregate pain severity score for each patient based on the mean of their worst, least, and average pain scores. We then transformed these scores into 100-point scales, with 0 being the least pain and 100 the most. We defined a minimal clinically important difference for pain severity in our analysis as a difference of ≥10 on the 100-point scale (Norman et al., 2003; Salaffi et al., 2004).We analyzed pain severity as a continuous measure.
Covariates
Based on an extensive review of the literature, we included a number of control measures. Sociodemographic covariates included race/ethnicity, age, sex, marital status, educational level, and wealth. We categorized race/ethnicity as white, black, Hispanic/Latino, Asian/Pacific Islander (API), multiple races, and other (including Native American) according to participant self-report.
We categorized age as 18–54, 55–64, 65–74, and 75 years or older. We subdivided participant sex as male or female, and marital status as “married/living with a partner,” “widowed/divorced/separated,” or “never married.” We categorized education as “less than a high school diploma,” “high school diploma but less than four-year college graduate,” or “four-year college graduate or higher.”
Participant wealth was measured through responses to the question “If you lost all of your current sources of income (for example, your paycheck, Social Security or pension, public assistance) and had to live off your savings, how long could you continue to live at your current address and standard of living?” We categorized this length of time as “less than one month,” “one month to a year,” and “more than one year.”
Survey language (English, Spanish, or Mandarin) was coded by the survey administrator, and we utilized this variable as a covariate to account for acculturation.
Health status variables in our analysis included cancer stage and presence of depressed affect. Stage was determined through evaluation of the medical record and other staging information by the CanCORS Statistical Coordinating Center. We dichotomized this as stage 4 versus stages 1–3.
Depressed affect has been shown to be associated with worse pain experience in cancer (Kroenke et al., 2011). This was measured through an eight-item adaptation of the Center for Epidemiologic Studies Depression Scale Short Form (CESD–SF), which we dichotomized as “yes” or “no” based on a cutpoint of ≥6 to indicate presence of depressed affect (Turvey et al., 1999).
Statistical Analysis
We employed descriptive statistics to compare the characteristics of patients reporting nonoptimal care (≤99) versus optimal care (100) in the three interpersonal care domains. To explore the unadjusted associations between patient-reported quality of care and pain severity, we examined mean BPI scores associated with patient report of either optimal (100) or nonoptimal (≤99) care in each of the three interpersonal domains.
Using analysis of variance (ANOVA), we found no evidence of clustering by data collection site. Moreover, bivariate analyses examining key variables by data collection site and health system type (Veterans Administration versus non-VA) showed no significant associations. Consequently, we did not include data collection site or health system variables in our final models.
Finally, we employed multivariable linear regression to examine the adjusted associations among patient assessment of physician communication, nursing care, and coordination/responsiveness of care and pain severity in three separate models.
Our study was approved by the CanCORS Steering Committee and the Johns Hopkins Bloomberg School of Public Health Institutional Review Board. All analyses were conducted with Stata software (v. 13.0; StataCorp, 2013).
RESULTS
The analytic sample included 2,746 individuals, 51% of whom were male. The majority of participants were white (69%), followed by black (14%), and Hispanic/Latino (7%). Nearly a quarter of the sample (24%) had stage 4 disease at the time of survey administration. Further sample characteristics are presented in Table 1.
Table 1.
Sample characteristics
| Characteristic | N (%) |
|---|---|
| Total | 2,746 (100.0) |
| Sex | |
| Male | 1,339 (50.9) |
| Female | 1,347 (49.1) |
| Age (years) | |
| 18–54 | 675 (24.6) |
| 55–64 | 828 (30.1) |
| 65–74 | 739 (26.9) |
| 75 and above | 504 (18.4) |
| Race/ethnicity | |
| White | 1,878 (68.5) |
| Black | 385 (14.1) |
| Hispanic/Latino | 194 (7.1) |
| Asian/Pacific Islander | 115 (4.2) |
| Multiple races | 98 (3.6) |
| Other | 70 (2.6) |
| Marital status | |
| Married/living with partner | 1,655 (60.4) |
| Widowed/divorced/separated | 933 (34.1) |
| Never married | 151 (5.5) |
| Education | |
| Less than a high school diploma | 494 (18.1) |
| High school diploma or more | 1,660 (60.7) |
| College graduate | 583 (21.3) |
| Survey language | |
| English | 2,640 (96.4) |
| Spanish | 72 (2.6) |
| Mandarin | 27 (1.0) |
| Wealth | |
| Less than 1 month | 687 (27.3) |
| 1 month to a year | 861 (34.2) |
| More than a year | 972 (38.6) |
| Stage | |
| Stages 1–3 | 1,971 (75.9) |
| Stage 4 | 626 (24.1) |
| Depressed affect | |
| No | 1,966 (75.9) |
| Yes | 623 (24.1) |
| Cancer type | |
| Lung | 1,460 (53.2) |
| Colorectal | 1,286 (46.8) |
Analysis of patient responses to the three interpersonal domains of care has been reported previously (Ayanian et al., 2010). Briefly, we found that 50% of patients rated their physician communication as nonoptimal, 54% rated their coordination/responsiveness of care as nonoptimal, and 28% rated their nursing care as nonoptimal. Further details on differences in ratings of interpersonal care by patient and health status characteristics are presented in Table 2.
Table 2.
Proportion of patients reporting less than optimal care, by sample characteristics (N = 2,746)
| Physician Communication | Coordination/ Responsiveness of Care |
Nursing Care | ||||
|---|---|---|---|---|---|---|
| Characteristic | n (%) | p Value | n (%) | p Value | n (%) | p Value |
| Total | 1,376 (50.2) | – | 1,473 (53.7) | – | 778 (28.4) | – |
| Sex | ||||||
| Male | 711 (50.9) | 0.458 | 752 (53.8) | 0.923 | 363 (26.0) | |
| Female | 665 (49.4) | 721 (53.7) | 415 (31.0) | 0.004 | ||
| Age (years) | ||||||
| 18–54 | 353 (52.3) | 0.641 | 384 (56.9) | 0.052 | 225 (33.3) | 0.011 |
| 55–64 | 407 (49.2) | 457 (55.3) | 229 (27.8) | |||
| 65–74 | 368 (49.8) | 370 (50.1) | 192 (26.1) | |||
| 75 and above | 248 (49.4) | 0.641 | 262 (52.3) | 132 (26.5) | ||
| Race/Ethnicity | ||||||
| White | 960 (51.2) | <0.001 | 1,019 (54.4) | <0.001 | 532 (28.5) | <0.001 |
| Black | 155 (40.3) | 171 (44.4) | 86 (22.5) | |||
| Hispanic/Latino | 102 (52.6) | 114 (58.8) | 73 (37.6) | |||
| Asian/Pacific Islander | 68 (59.1) | 77 (67.0) | 40 (34.8) | |||
| Multiple races | 46 (46.9) | 54 (55.1) | 27 (27.6) | |||
| Other | 39 (55.7) | 32 (46.4) | 14 (20.0) | |||
| Marital status | ||||||
| Married/living w/partner | 810 (48.9) | 0.176 | 870 (52.6) | 0.310 | 455 (27.5) | 0.249 |
| Widowed/Div./Sep. | 474 (51.0) | 508 (54.6) | 266 (28.7) | |||
| Never married | 85 (56.3) | 88 (58.3) | 51 (33.8) | |||
| Education | ||||||
| <High school diploma | 229 (46.4) | 0.0005 | 223 (45.2) | <0.001 | 120 (24.3) | <0.001 |
| High school diploma+ | 815 (49.2) | 876 (52.9) | 430 (26.0) | |||
| College graduate | 325 (55.7) | 367 (62.9) | 222 (38.2) | |||
| Survey language | ||||||
| English | 1,307 (49.6) | <0.001 | 1,404 (53.3) | <0.001 | 731 (27.8) | 0.003 |
| Spanish | 39 (54.2) | 37 (51.4) | 25 (34.7) | |||
| Mandarin | 23 (85.2) | 25 (92.6) | 15 (55.6) | |||
| Wealth | ||||||
| Less than 1 month | 340 (49.6) | 0.536 | 360 (52.5) | 0.643 | 185 (26.9) | 0.458 |
| 1 month to a year | 416 (48.4) | 457 (53.1) | 255 (29.7) | |||
| More than a year | 495 (50.9) | 531 (54.7) | 269 (27.8) | |||
| Stage | ||||||
| Stages 1–3 | 977 (49.6) | 0.300 | 1,057 (53.7) | 0.962 | 611 (31.1) | <0.001 |
| Stage 4 | 325 (50.0) | 336 (53.8) | 123 (19.7) | |||
| Depressed affect | ||||||
| No | 906 (46.1) | <0.001 | 975 (49.6) | <0.001 | 502 (25.6) | <0.001 |
| Yes | 371 (59.7) | 397 (63.8) | 214 (34.5) | |||
| Cancer type | ||||||
| Lung | 737 (50.5) | 0.696 | 757 (51.9) | 0.046 | 348 (23.9) | <0.001 |
| Colorectal | 639 (49.8) | 716 (55.8) | 430 (33.5) | |||
Table 3 presents unadjusted differences in mean pain severity scores by ratings of care and sample characteristics. Mean pain severity scores were significantly different between those individuals reporting nonoptimal care versus those reporting optimal care in the domains of physician communication (40.1 vs. 38.4, p = 0.020) and coordination/responsiveness of care (40.1 vs. 38.2, p = 0.009) but not nursing care. Mean pain severity differed by respondent race/ethnicity: scores ranged from 34.2 for API respondents to 45.0 for black respondents (p < 0.001). Scores also varied significantly by survey language: Mandarin survey respondents reported a mean pain severity score of 23.9 versus 39.1 for English respondents (p < 0.001). Individuals with depressed affect reported a mean pain severity score of 47.2 versus 36.5 among those without depressed affect (p < 0.001). We also observed significant differences in mean pain severity score by sex (p = 0.008), age (p < 0.001), marital status (p = 0.006), education (p < 0.001), wealth (p < 0.001), and cancer stage (p = 0.031). There was no difference in mean pain severity by cancer type in the unadjusted analysis.
Table 3.
Mean BPI scores by sample characteristics and patient assessments of care
| Mean (SD) | p Value | |
|---|---|---|
| Physician communication | ||
| Optimal | 38.4 (19.2) | 0.020 |
| Nonoptimal | 40.1 (19.1) | |
| Coordination/responsiveness of care | ||
| Optimal | 38.2 (19.0) | 0.009 |
| Nonoptimal | 40.1 (12.2) | |
| Nursing care | ||
| Optimal | 39.2 (18.2) | 0.949 |
| Nonoptimal | 39.2 (18.9) | |
| Sex | ||
| Male | 38.3 (18.8) | 0.008 |
| Female | 40.2 (19.4) | |
| Age (years) | ||
| 18–54 | 41.9 (19.8) | |
| 55–64 | 39.8 (18.9) | <0.001 |
| 65–74 | 37.3 (19.1) | |
| 75 and above | 37.4 (18.1) | |
| Race/ethnicity | ||
| White | 37.6 (18.0) | |
| Black | 45.0 (21.1) | |
| Hispanic/Latino | 43.5 (19.6) | <0.001 |
| Asian/Pacific Islander | 34.2 (20.6) | |
| Multiple races | 43.2 (23.1) | |
| Other | 41.1 (19.7) | |
| Marital Status | ||
| Married/living w/partner | 38.3 (18.7) | 0.006 |
| Widowed/divorced/separated | 40.5 (19.9) | |
| Never married | 41.4 (18.8) | |
| Education | ||
| <High school diploma | 44.6 (20.6) | <0.001 |
| High school diploma or more | 39.4 (18.8) | |
| College graduate | 34.1 (17.4) | |
| Survey language | ||
| English | 39.1 (19.0) | <0.001 |
| Spanish | 48.7 (18.9) | |
| Mandarin | 23.9 (18.9) | |
| Wealth | ||
| Less than 1 month | 43.8 (20.3) | <0.001 |
| 1 month to a year | 39.8 (18.7) | |
| More than a year | 35.4 (17.8) | |
| Stage | ||
| Stages 1–3 | 38.6 (19.0) | 0.031 |
| Stage 4 | 40.5 (19.4) | |
| Depressed affect | ||
| No | 36.5 (18.2) | <0.001 |
| Yes | 47.2 (19.9) | |
| Cancer type | ||
| Lung | 39.7 (18.9) | <0.129 |
| Colorectal | 38.6 (19.5) |
The three adjusted linear models examining the association between each patient-reported domain of interpersonal care and pain severity are presented in Table 4. In the model examining the adjusted association between physician communication and pain severity (model 1), rating physician communication as nonoptimal was associated with a 1.8-point higher average pain severity (on a 100-point scale) compared to those reporting optimal communication (p = 0.018). In the adjusted model examining the association between coordination/responsiveness of care and pain severity (model 2), rating care as nonoptimal was associated with a 2.2-point higher average pain severity compared to those reporting optimal coordination/responsiveness of care (p = 0.006). We found no significant association between ratings of nursing care and pain severity in the adjusted analysis (model 3).
Table 4.
Multivariable linear regressions, patient assessments of interpersonal care and pain severity
| Model 1 Physician Communication N = 2,242 |
Model 2 Coordination/ Responsiveness of Care N = 2,241 |
Model 3 Nursing Care N = 2,238 |
||||
|---|---|---|---|---|---|---|
| Est. | p Value | Est. | p Value | Est. | p Value | |
| Physician communication | ||||||
| Optimal | – | – | – | – | ||
| Nonoptimal | +1.8 | 0.018 | ||||
| Coordination/responsiveness of care | ||||||
| Optimal | – | – | – | – | ||
| Nonoptimal | +2.2 | 0.006 | ||||
| Nursing care | ||||||
| Optimal | – | – | – | – | ||
| Nonoptimal | +0.4 | 0.651 | ||||
| Sex | ||||||
| Male | ||||||
| Female | +1.6 | 0.050 | +1.5 | 0.050 | +1.5 | 0.058 |
| Age (years) | ||||||
| 18–54 | ||||||
| 55–64 | −2.3 | 0.028 | +2.3 | 0.025 | −2.3 | 0.030 |
| 65–74 | −3.3 | 0.004 | −3.2 | 0.004 | −3.4 | 0.003 |
| 75 and above | −2.0 | 0.110 | −2.1 | 0.104 | −2.1 | 0.104 |
| Race/Ethnicity | ||||||
| White | ||||||
| Black | +5.6 | <0.001 | +5.6 | <0.001 | +5.2 | <0.001 |
| Hispanic/Latino | +0.6 | 0.733 | +0.6 | 0.764 | +0.6 | 0.758 |
| Asian/Pacific Islander | +0.2 | 0.947 | +0.1 | 0.966 | +0.2 | 0.921 |
| Multiple races | +5.6 | 0.006 | +5.4 | 0.008 | +5.5 | 0.008 |
| Other | +2.6 | 0.296 | +2.9 | 0.241 | +2.6 | 0.289 |
| Marital Status | ||||||
| Married/living w/ partner | ||||||
| Widowed/divorced/separated | +0.3 | 0.774 | +0.2 | 0.798 | +0.2 | 0.834 |
| Never married | +1.2 | 0.487 | +1.2 | 0.483 | +1.3 | 0.454 |
| Education | ||||||
| <High school diploma | ||||||
| High school diploma+ | −3.7 | <0.001 | −3.8 | <0.001 | −3.7 | <0.001 |
| College graduate | −7.2 | <0.001 | −7.4 | <0.001 | −7.1 | <0.001 |
| Survey language | ||||||
| English | ||||||
| Spanish | +4.6 | 0.138 | +4.7 | 0.125 | +4.6 | 0.137 |
| Mandarin | −15.9 | <0.001 | −16.2 | <0.001 | −15.6 | <0.002 |
| Wealth | ||||||
| Less than 1 month | ||||||
| 1 month to a year | −2.7 | 0.007 | −2.7 | 0.007 | −2.7 | 0.006 |
| More than a year | −4.8 | <0.001 | −4.8 | <0.001 | −4.8 | <0.001 |
| Stage | ||||||
| Stages 1–3 | ||||||
| Stage 4 | +1.5 | 0.109 | +1.5 | 0.099 | +1.4 | 0.117 |
| Depressed affect | ||||||
| No | ||||||
| Yes | +8.2 | <0.001 | +8.1 | <0.001 | +8.4 | <0.001 |
| Cancer type | ||||||
| Lung | ||||||
| Colorectal | −0.7 | 0.352 | −0.8 | 0.299 | −0.7 | 0.357 |
Across the adjusted three models, lower pain scores were associated with younger age, more education, greater wealth, and Mandarin survey language. Higher pain scores were reported by black and multiracial participants and those with depressed affect.
The associations between black participant race/ethnicity and pain severity in the three adjusted models were particularly strong. Black participants rated their pain severity between 5.2 and 5.6 points higher on average than whites (p < 0.001 for all three models), as did multiracial participants (range: 5.4 to 5.6 points higher compared to whites; p < 0.010 for all three models). Presence of depressed affect was also strongly associated with pain severity. Scores ranged from 8.1 to 8.4 points higher for those with depressed affect compared to those without (p < 0.001 for all models).
The only adjusted difference in pain severity that met our criteria for minimally clinically important difference was for Mandarin survey respondents who reported average pain severity at 15.6–16.2 points lower compared to English survey respondents (p < 0.001 for all models).
As a sensitivity analysis, we ran all final models using a cutpoint of ≤90 instead of ≤99 in order to define nonoptimal care in each domain. This did not significantly alter the results.
DISCUSSION
In our study of colorectal and lung cancer patients reporting the presence of pain, we found small yet statistically significant associations between patient ratings of both physician communication/coordination and responsiveness of care and pain severity; however, patient race/ethnicity and depressed affect were more important factors in self-reported pain severity. We did not, find any association between patient assessment of nursing care and pain severity. While our outcomes suggest that interventions aimed at improving physician communication and coordination and responsiveness of care may result in improved cancer pain experience for some patients, differences in pain severity by ratings of interpersonal care in our study were extremely small and were not clinically meaningful.
We found significant differences in patient-reported pain severity by sociodemographic characteristics. Of note in our results were the large differences in pain severity between black and white participants in each of the assessment-of-care models, despite adjustment for patient ratings of care. Black/white disparities in cancer pain have been widely reported in the literature (Anderson et al., 2002; Fisch et al., 2012). Quality of care deficits, particularly around interpersonal communication, have been hypothesized to contribute to disparities in pain (Cintron & Morrison, 2006). In our study, black participants rated care in each of the three interpersonal domains, including physician communication, better than whites, while rating pain severity significantly more severe. Yet, given the small size of the association we found between patient ratings of care and pain severity, our findings support the notion that patient variability in ratings of interpersonal care is only one of many factors affecting the cancer pain experience.
Patient-reported quality of care is increasingly being used to evaluate medical care, as well as to inform strategies and priorities for quality improvement (Dennison, 2002; Groene, 2011). One hypothesis underlying the increasing use of these measures is that patient appraisals of care may relate to health outcomes through improved patient adherence to treatment (Dang et al., 2013; Isaac et al., 2010). Some prior literature supports this association (Alazri & Neal, 2003; Fremont et al., 2001; Safran et al., 1998). Yet, other recent work has questioned the relationship between patient satisfaction and health outcomes (Fenton et al., 2012) and suggested that the observed associations in this domain may largely be explained by patient factors, rather than as a direct result of satisfaction (Jerant et al., 2014).
Prior studies of the association between patient pain and satisfaction with care have also yielded mixed results. In fact, some studies have documented the phenomenon of a “pain paradox” wherein patients report very high satisfaction with care despite reporting a concurrently high pain burden (Beck et al., 2010; Dawson et al., 2002; McCracken et al., 1997; Miaskowski et al., 1994; Panteli & Patistea, 2007). These studies have demonstrated that patient satisfaction among individuals experiencing pain is largely associated with interpersonal aspects of care, such as patient–provider communication (Dawson et al., 2002), or generally feeling “cared for” (Beck et al., 2010), rather than a reflection of their symptom experience. Moreover, satisfaction with pain management may be modulated by patient expectations about pain control (Dawson et al., 2002), suggesting that individuals with lower expectations for pain relief may report high satisfaction with care, despite experiencing high levels of pain. This may be particularly true for nonwhite patients or those of low socioeconomic status, who have been shown to have lower expectations for pain control in cancer (Anderson et al., 2002).
Despite the challenges of using patient-reported measures of quality of care in this domain, cancer pain remains a common and problematic symptom experience, disproportionately experienced by certain patient groups. The findings from our study and others suggest that quality enhancement efforts to improve pain outcomes should consider including interventions to improve interpersonal cancer care, but also require other types of interventions.
Our study had several limitations. Patient-reported pain is the gold standard in pain assessment; however, prior research has demonstrated patient and group differences in underlying pain thresholds (Rahim-Williams et al., 2012) and expectations about pain management (Naveh et al., 2011). Moreover, patient preferences for pain management vary, and some patients have been shown to be willing to tolerate higher levels of pain in order to avoid the side effects associated with pain medication (Gan et al., 2004). We were unable to measure patient pain thresholds, expectations about pain management, or patient satisfaction with pain control. Our findings were also limited by the fact that the survey instrument utilized to measure patient assessment of care was not specific to a particular provider. The patients in our study likely interacted with a number of providers, not all of whom were involved in pain management.
CONCLUSIONS
We found modest evidence that interventions targeting physician communication and coordination/responsiveness of care may improve pain burden in some groups of patients. However, differences in pain severity by ratings of care in these domains were not clinically significant. Further, we found large and significant differences in pain severity by survey language, race/ethnicity, and presence of depressed affect, despite controlling for a number of patient-reported sociodemographic and health status factors. Given the observed variability in both patient ratings of interpersonal care as well as patient pain severity, continued refinement of patient-reported measures of interpersonal care, with a particular focus on use of these measures among nonwhite patients and those with depressed affect, may be useful in improving the quality of life for cancer patients experiencing pain.
REFERENCES
- Alazri MH, Neal RD. The association between satisfaction with services provided in primary care and outcomes in type 2 diabetes mellitus. Diabetic Medicine. 2003;20(6):486–490. doi: 10.1046/j.1464-5491.2003.00957.x. [DOI] [PubMed] [Google Scholar]
- Anderson KO, Richman SP, Hurley J, et al. Cancer pain management among underserved minority outpatients: Perceived needs and barriers to optimal control. Cancer. 2002;94(8):2295–2304. doi: 10.1002/cncr.10414. [DOI] [PubMed] [Google Scholar]
- Antón A, Montalar J, Carulla J, et al. Pain in clinical oncology: Patient satisfaction with management of cancer pain. European Journal of Pain (London, England) 2012;16(3):381–389. doi: 10.1002/j.1532-2149.2011.00036.x. [DOI] [PubMed] [Google Scholar]
- Avery KNL, Metcalfe C, Nicklin J, et al. Satisfaction with care: An independent outcome measure in surgical oncology. Annals of Surgical Oncology. 2006;13(6):817–822. doi: 10.1245/ASO.2006.08.019. [DOI] [PubMed] [Google Scholar]
- Ayanian JZ, Zaslavsky AM, Guadagnoli E, et al. Patients’ perceptions of quality of care for colorectal cancer by race, ethnicity, and language. Journal of Clinical Oncology. 2005;23(27):6576–6586. doi: 10.1200/JCO.2005.06.102. [DOI] [PubMed] [Google Scholar]
- Ayanian JZ, Zaslavsky AM, Arora NK, et al. Patients’ experiences with care for lung cancer and colorectal cancer: Findings from the Cancer Care Outcomes Research and Surveillance Consortium. Journal of Clinical Oncology. 2010;28(27):4154–4161. doi: 10.1200/JCO.2009.27.3268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck SL, Towsley GL, Berry PH, et al. Core aspects of satisfaction with pain management: Cancer patients’ perspectives. Journal of Pain and Symptom Management. 2010;39(1):100–115. doi: 10.1016/j.jpainsymman.2009.06.009. [DOI] [PubMed] [Google Scholar]
- Catalano PJ, Ayanian JZ, Weeks JC, et al. Representativeness of participants in the cancer care outcomes research and surveillance consortium relative to the surveillance, epidemiology, and end results program. Medical Care. 2013;51(2):e9–e15. doi: 10.1097/MLR.0b013e318222a711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cintron A, Morrison RS. Pain and ethnicity in the United States: A systematic review. Journal of Palliative Medicine. 2006;9(6):1454–1473. doi: 10.1089/jpm.2006.9.1454. [DOI] [PubMed] [Google Scholar]
- Cleeland CS, Ryan KM. Pain assessment: Global use of the Brief Pain Inventory. Annals of the Academy of Medicine, Singapore. 1994;23(2):129–138. [PubMed] [Google Scholar]
- Dang BN, Westbrook RA, Black WC, et al. Examining the link between patient satisfaction and adherence to HIV care: A structural equation model. PloS One. 2013;8(1):e54729. doi: 10.1371/journal.pone.0054729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson R, Spross JA, Jablonski ES, et al. Probing the paradox of patients’ satisfaction with inadequate pain management. Journal of Pain and Symptom Management. 2002;23(3):211–220. doi: 10.1016/s0885-3924(01)00399-2. [DOI] [PubMed] [Google Scholar]
- Deandrea S, Montanari M, Moja L, et al. Prevalence of undertreatment in cancer pain: A review of published literature. Annals of Oncology. 2008;19(12):1985–1991. doi: 10.1093/annonc/mdn419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennison CR. The role of patient-reported outcomes in evaluating the quality of oncology care. The American Journal of Managed Care. 2002;8(18 Suppl):S580–S586. [PubMed] [Google Scholar]
- Fairchild A. Under-treatment of cancer pain. Current Opinion in Supportive and Palliative Care. 2010;4(1):11–15. doi: 10.1097/SPC.0b013e328336289c. [DOI] [PubMed] [Google Scholar]
- Fenton JJ, Jerant AF, Bertakis KD, et al. The cost of satisfaction: A national study of patient satisfaction, health care utilization, expenditures, and mortality. Archives of Internal Medicine. 2012;172(5):405–411. doi: 10.1001/archinternmed.2011.1662. [DOI] [PubMed] [Google Scholar]
- Fisch MJ, Lee J-W, Weiss M, et al. Prospective, observational study of pain and analgesic prescribing in medical oncology outpatients with breast, colorectal, lung, or prostate cancer. Journal of Clinical Oncology. 2012;30(16):1980–1988. doi: 10.1200/JCO.2011.39.2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fremont AM, Cleary PD, Hargraves JL, et al. Patient-centered processes of care and long-term outcomes of myocardial infarction. Journal of General Internal Medicine. 2001;16(12):800–808. doi: 10.1111/j.1525-1497.2001.10102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan TJ, Lubarsky DA, Flood EM, et al. Patient preferences for acute pain treatment. British Journal of Anaesthesia. 2004;92(5):681–688. doi: 10.1093/bja/aeh123. [DOI] [PubMed] [Google Scholar]
- Groene O. Patient centredness and quality improvement efforts in hospitals: Rationale, measurement, implementation. International Journal for Quality in Health Care. 2011;23(5):531–537. doi: 10.1093/intqhc/mzr058. [DOI] [PubMed] [Google Scholar]
- Isaac T, Zaslavsky AM, Cleary PD, et al. The relationship between patients’ perception of care and measures of hospital quality and safety. Health Services Research. 2010;45(4):1024–1040. doi: 10.1111/j.1475-6773.2010.01122.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerant A, Fenton JJ, Bertakis KD, et al. Satisfaction with health care providers and preventive care adherence: A national study. Medical Care. 2014;52(1):78–85. doi: 10.1097/MLR.0000000000000021. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Wu J, Bair MJ, et al. Reciprocal relationship between pain and depression: A 12-month longitudinal analysis in primary care. The Journal of Pain. 2011;12(9):964–973. doi: 10.1016/j.jpain.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luckett T, Davidson PM, Green A, et al. Assessment and management of adult cancer pain: A systematic review and synthesis of recent qualitative studies aimed at developing insights for managing barriers and optimizing facilitators within a comprehensive framework of patient care. Journal of Pain and Symptom Management. 2013;46(2):229–253. doi: 10.1016/j.jpainsymman.2012.07.021. [DOI] [PubMed] [Google Scholar]
- Malin JL, Ko C, Ayanian JZ, et al. Understanding cancer patients’ experience and outcomes: Development and pilot study of the Cancer Care Outcomes Research and Surveillance patient survey. Supportive Care in Cancer. 2006;14(8):837–848. doi: 10.1007/s00520-005-0902-8. [DOI] [PubMed] [Google Scholar]
- McCracken LM, Klock PA, Mingay DJ, et al. Assessment of satisfaction with treatment for chronic pain. Journal of Pain and Symptom Management. 1997;14(5):292–299. doi: 10.1016/s0885-3924(97)00225-x. [DOI] [PubMed] [Google Scholar]
- McNeill JA, Sherwood GD, Starck PL. The hidden error of mismanaged pain: A systems approach. Journal of Pain and Symptom Management. 2004;28(1):47–58. doi: 10.1016/j.jpainsymman.2003.11.005. [DOI] [PubMed] [Google Scholar]
- Miaskowski C, Nichols R, Brody R, et al. Assessment of patient satisfaction utilizing the American Pain Society’s Quality Assurance Standards on acute and cancer-related pain. Journal of Pain and Symptom Management. 1994;9(1):5–11. doi: 10.1016/0885-3924(94)90140-6. [DOI] [PubMed] [Google Scholar]
- National Research Council. Delivering high-quality cancer care: Charting a new course for a system in crisis. Washington, DC: The National Academies Press; 2013. [PubMed] [Google Scholar]
- Naveh P, Leshem R, Dror YF, et al. Pain severity, satisfaction with pain management, and patient-related barriers to pain management in patients with cancer in Israel. Oncology Nursing Forum. 2011;38(4):E305–E313. doi: 10.1188/11.ONF.E305-E313. [DOI] [PubMed] [Google Scholar]
- Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Medical Care. 2003;41(5):582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- Panteli V, Patistea E. Assessing patients’ satisfaction and intensity of pain as outcomes in the management of cancer-related pain. European Journal of Oncology Nursing. 2007;11(5):424–533. doi: 10.1016/j.ejon.2007.09.002. [DOI] [PubMed] [Google Scholar]
- Rahim-Williams B, Riley JL, Williams AKK, et al. A quantitative review of ethnic group differences in experimental pain response: Do biology, psychology, and culturematter? Pain Medicine (Malden, Massachusetts) 2012;13(4):522–540. doi: 10.1111/j.1526-4637.2012.01336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safran DG, Taira DA, Rogers WH, et al. Linking primary care performance to outcomes of care. The Journal of Family Practice. 1998;47(3):213–220. [PubMed] [Google Scholar]
- Salaffi F, Stancati A, Silvestri CA, et al. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. European Journal of Pain (London, England) 2004;8(4):283–291. doi: 10.1016/j.ejpain.2003.09.004. [DOI] [PubMed] [Google Scholar]
- Siegel R, Ma J, Zou Z, et al. Cancer statistics 2014. CA: A Cancer Journal for Clinicians. 2014;64(1):9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: Release 13. College Station, TX: StataCorp; 2013. [Google Scholar]
- Tavoli A, Montazeri A, Roshan R, et al. Depression and quality of life in cancer patients with and without pain: The role of pain beliefs. BMC Cancer. 2008;8:177. doi: 10.1186/1471-2407-8-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turvey CL, Wallace RB, Herzog R. A revised CES–D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatrics/IPA. 1999;11(2):139–148. doi: 10.1017/s1041610299005694. [DOI] [PubMed] [Google Scholar]
- van den Beuken-van Everdingen MHJ, de Rijke JM, Kessels AG, et al. Prevalence of pain in patients with cancer: A systematic review of the past 40 years. Annals of Oncology. 2007;18(9):1437–1449. doi: 10.1093/annonc/mdm056. [DOI] [PubMed] [Google Scholar]
- von Gruenigen VE, Hutchins JR, Reidy AM, et al. Gynecologic oncology patients’ satisfaction and symptom severity during palliative chemotherapy. Health and Quality of Life Outcomes. 2006;4:84. doi: 10.1186/1477-7525-4-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner-Johnston ND, Carson KA, Grossman SA. High outpatient pain intensity scores predict impending hospital admissions in patients with cancer. Journal of Pain and Symptom Management. 2010;39(2):180–185. doi: 10.1016/j.jpainsymman.2009.06.012. [DOI] [PubMed] [Google Scholar]
- Ward SE, Gordon D. Application of the American Pain Society quality assurance standards. Pain. 1994;56(3):299–306. doi: 10.1016/0304-3959(94)90168-6. [DOI] [PubMed] [Google Scholar]
- Yates PM, Edwards HE, Nash RE, et al. Barriers to effective cancer pain management: A survey of hospitalized cancer patients in Australia. Journal of Pain and Symptom Management. 2002;23(5):393–405. doi: 10.1016/s0885-3924(02)00387-1. [DOI] [PubMed] [Google Scholar]