Abstract
Background/Objectives
Higher volumes of ectopic cardiovascular fat (ECF) are associated with greater risk of coronary heart disease (CHD). Identifying factors that are associated with ECF volumes may lead to new preventive efforts to reduce risk of CHD. Significant racial/ethnic differences exist for overall and central adiposity measures which are known to be associated with ECF volumes. Whether racial/ethnic differences also exist for ECF volumes and their associations with these adiposity measures remain unclear.
Subjects/Methods
Body-mass index (BMI), CT-measured ECF volumes (epicardial, pericardial and their summation), and visceral adipose tissue (VAT) were examined in a community-based sample of 1,199 middle-aged men (24.2% Caucasians, 7.0% African-Americans, 23.6% Japanese-Americans, 22.0% Japanese, 23.2% Koreans).
Results
Significant racial/ethnic differences existed in ECF volumes and their relationships with BMI and VAT. ECF volumes were highest among Japanese-Americans and lowest among African-Americans. The associations of BMI and VAT with ECF differed by racial/ethnic groups. Compared to Caucasians, for each 1-unit increase in BMI, African-Americans had lower whereas Koreans had higher increases in ECF volumes (P-values<0.05 for both). Meanwhile, compared to Caucasians, for each 1-unit increase in log-transformed-VAT, African-Americans, Japanese-Americans and Japanese had similar increases, whereas Koreans had a lower increase in ECF volumes (P-value<0.05).
Conclusions
Racial/ethnic groups differed in their propensity to accumulate ECF at increasing level of overall and central adiposity. Future studies should evaluate whether reducing central adiposity or overall-weight will decrease ECF volumes more in certain racial/ethnic groups. Evaluating these questions might help in designing race-specific prevention strategy of CHD risk associated with higher ECF.
Keywords: epidemiology, obesity, pericardium, adipose tissue, epicardial fat
Introduction
Ectopic cardiovascular fat (ECF), fat surrounding the myocardium and the coronary arteries, is a metabolically active organ that releases substances with vascular actions (1) in addition to proinflammatory factors and free fatty acid (FFA). (2,3) Mounting evidence demonstrates a role of ECF in the pathogenesis of coronary heart disease. (4-7)
It has been suggested that ectopic fat accumulation around organs such as the heart could be a consequence of impairment in subcutaneous adipose tissue (SAT) ability to buffer energy excess. (8,9) Because ECF has been found to be positively correlated with adiposity measures including body-mass index (BMI), waist circumference and visceral adipose tissue (VAT) (4-6) it is expected that an increase in any of these adiposity measures will result in an increase in ECF.
Significant racial/ethnic differences have been reported for both SAT and VAT. (10-13) Compared with Caucasian men, African-American men have less VAT and more SAT. (10-12) Further, despite a much lower BMI, Japanese men in Japan have a higher VAT as compared with Caucasian men in the US at each quartile of waist circumference. (13) Japanese men tend to have less SAT than Caucasian men when waist circumference >97.0 cm. (13) Whether racial/ethnic differences also exist for ECF remain unclear. Moreover, very few studies assessed the impact of race/ethnicity on ECF volumes. (14,15) These studies are limited by small sample sizes and evaluating the differences between only two racial groups. In these studies, greater epicardial fat, fat within the pericardial sac, was found in Caucasian as compared with African-American participants. (14,15) Because ECF correlates with adiposity measures which vary by racial/ethnic groups, (10-13) it is plausible to hypothesize that the association of these adiposity measures with ECF volumes may also vary by racial/ethnic groups.
To the best of our knowledge, this is the first large community-based study to evaluate whether ECF depots: 1) Epicardial adipose tissue (fat within the pericardial sac: EAT); 2) pericardial adipose tissue (fat outside the pericardial sac: PAT); 3) Total heart adipose tissue (TAT=EAT+PAT) vary among 5 different racial/ethnic groups (Caucasian, African-American, Japanese-American, Japanese (in Japan) and Korean (in Korea)). Additionally, the current study evaluated the associations of each ECF depot with each of the following adiposity measures: BMI, VAT and SAT and tested if these associations vary by racial/ethnic groups.
Materials and Methods
Subjects
The ERA JUMP study is a population-based study of men (40-49 years) who were free of cardiovascular disease (CVD), type-1-diabetes, or other severe diseases. The research design has been described previously. (16-18) Briefly, between 2002 and 2006, 1,335 men were randomly selected at each of 4 sites: 417 (107 African-American and 310 Caucasian) men from Allegheny County, Pennsylvania, US; 313 Japanese men from Kusatsu, Shiga, Japan; 303 Japanese-American men from a representative sample of offspring of fathers who participated in the Honolulu Heart Program, (19) Honolulu, Hawaii, US. These offspring were the third or fourth generation of Japanese-Americans without ethnic admixture; (20) 302 Korean men from Ansan, South Korea.
For the current study, data on ECF depots were available for 1,199 (89.2%) participants. Participants who were excluded from the current study due to poor image acquisition (n=136) were slightly older and more likely to be Japanese-American. There were no significant differences in any of the adiposity measures between the two groups. Informed consent was obtained from all participants. The study was approved by the Institutional Review Board at each site.
Ectopic Cardiovascular Fat Depots
Existing CT scans for measuring coronary calcification (3-mm-thick transverse images obtained with a GE-Imatron C150 Electron Beam Tomography scanner (GE Medical Systems, South San Francisco, U.S.) were used to quantify ECF depots at the Los Angeles Biomedical Research Institute, Harbor-UCLA Medical Center, CA. Using the same methods that were used in a previously published study, (21) epicardial adipose tissue (EAT) was defined as the adipose tissue within the pericardial sac, pericardial adipose tissue (PAT) was defined as the adipose tissue outside the pericardial sac (Supplemental Figure 1), and total heart adipose tissue (TAT) was the sum of EAT and PAT. ECF depot volumes were determined from 15 mm above to 30 mm below the superior extent of the left main coronary artery. This region of the heart was selected because it includes the epicardial fat located around the proximal coronary arteries (left main coronary, left anterior descending, right coronary, and circumflex arteries). The anterior border of the total heart adipose tissue volume was defined by the chest wall and the posterior border by the aorta and the bronchus. Using volume analysis software (GE Healthcare, Waukesha, WI), fat was distinguished from the remainder of the heart tissue by a threshold of -190 to -30 Hounsfield units. EAT was measured by manually tracing out the pericardium every 2-3 slices below the start point, and then using the software to automatically trace out the segments in between these selected slices. PAT was measured by subtracting EAT from TAT volume. EAT and PAT measures have been demonstrated to have excellent reproducibility. Spearman correlation coefficients between-reader and within-reader were ≥ 0.97.
Visceral and Subcutaneous Abdominal Fat
Areas of the total abdominal adipose tissue and visceral adipose tissue (VAT) were determined using a 6-mm transverse image, at the level between the fourth and fifth lumbar vertebrae using a GE-Imatron C150 scanner (GE Medical Systems, South San Francisco, U.S.) at all study sites. Adipose tissue was determined using image analysis (AccuImage; AccuImage Diagnostics, San Francisco, CA) in a CT range from -130 to 0 Hounsfield Unit. (22) A separation line was drawn manually using a cursor along abdominal wall musculature in continuity with fascia of the para-spinal muscles. (23, 24) Area of subcutaneous adipose tissue (SAT) was calculated as total abdominal adipose tissue minus VAT. All CT images were analyzed at the Cardiovascular Institute, University of Pittsburgh by one trained reader who was blinded to participant’s characteristics. The intra-class correlation coefficients were 0.99 for SAT and 0.99 for VAT. (13)
Other Study Variables
All participants underwent physical examination and lifestyle questionnaire. Body weight and height were measured while the participant was wearing light clothing without shoes. BMI was calculated as weight in kg/(height in meter)2. Blood pressure was measured in the right arm of the seated participant after he emptied his bladder and sat quietly for 5 minutes, using an automated sphygmomanometer and an appropriate-sized cuff. The average of two measurements was used.
Smoking was assessed as current, former or never. Alcohol consumption was assessed as whether the participant drank beer, wine, liquor, sake (Japanese rice wine), or other alcoholic beverages, with quantity and frequency. Alcohol drinkers were defined as those who drank alcohol ≥2 times per week. Uses of medications (anti-hypertensive, anti-diabetic, and lipid-lowering) were reported as yes/no.
Statistical analyses
The distribution for VAT, SAT and ECF depots were highly skewed, and therefore, log-transformation was applied. One-way ANOVA with Bonferroni adjustment was used to determine differences among racial/ethnic groups for continuous measures and Chi-square test was used for categorical measures. Linear regression was used to test whether ECF depots vary by race/ethnicity independent of adiposity measures (separate models), age, smoking status and alcohol consumption. (5) Analysis of covariance was used to determine whether associations between each adiposity measure and each ECF depot were modified by racial/ethnic groups. Stratified analysis by race/ethnicity was performed to estimate the effect size of adiposity measures (separate models) on each ECF depot in each racial/ethnic group. Race/ethnic-specific standardized beta coefficients (slopes) were calculated to facilitate comparisons for effects of changes in BMI and VAT as related to changes in ECF depots. To evaluate if differences between racial/ethnic groups in relation to ECF depots vary at each level of adiposity measures, quartiles were created for adiposity measures with significant interactions with race/ethnicity (BMI and VAT), and geometric means of ECF depot volumes were estimated (supplemental Table 1). Analyses were performed with SAS v9.2 (SAS Institute, Cary, NC). P values less than 0.05 (two-tailed) were considered statistically significant after adjusting for multiple comparisons when appropriate.
Results
Table 1 shows characteristics of the study population for the full cohort as well as by racial/ethnic groups. All characteristics significantly varied by racial/ethnic groups (P<0.001). Japanese-Americans had greater EAT, while African-Americans had less EAT compared with Caucasians. Irrespective of the lower BMI, VAT and SAT levels among Japanese and Koreans, their levels of EAT were similar to that of Caucasians. For PAT, African-Americans, Japanese and Koreans had significantly less PAT while Japanese-Americans had similar levels of PAT as compared with Caucasians. For TAT, African-Americans had significantly less TAT compared with Caucasians. Japanese-Americans, Japanese and Koreans had similar levels of TAT of Caucasians.
Table 1. Baseline Characteristics for the Total Study Population (2000-2006) and by Racial/Ethnic Groups.
| Variables | Total N=1199 |
Caucasians N=290 (24.2%) |
African- Americans N=84 (7.0%) |
Japanese- Americans N=283 (23.6%) |
Japanese N=264 (22.0%) |
Koreans N=278 (23.2%) |
|---|---|---|---|---|---|---|
| Age, mean(SD), years | 45.3(2.8) | 45.0(2.8) § | 45.2(2.7) | 46.1(2.8) †, ∥, ¶ | 45.2(2.8) § | 44.8(2.8) § |
| BMI, mean(SD), Kg/m2 | 26.3(4.3) | 27.8(4.2) ∥, ¶ | 29.1(5.7) §, ∥, ¶ | 27.9(4.3) ‡, ∥, ¶ | 23.8(3.1) †, ‡, § | 24.7(2.6) †, ‡, § |
| VAT *, cm2 | 144.3(105.6,186.0) | 162.2(116.4,211.0) ‡, ∥, ¶ | 129.3(81.2,170.3) †, § | 158.4(124.0,213.6) ‡, ∥, ¶ | 134.8(96.7,171.6) †, § | 126.6(99.7,163.2) †, § |
| SAT *, cm2 | 168.5(126.5,244.2) | 226.5(173.4,317.4) ∥, ¶ | 242.3(161.3,335.8) ∥, ¶ | 207.3(160.7,278.3) ∥, ¶ | 130.4(100.9,162.7) †, ‡, § | 134.3(101.9,164.8) †, ‡, § |
| EAT *, cm3 | 44.5(33.1,58.2) | 41.7(32.4,57.4) ‡, § | 34.6(23.1,47.3) †, §, ∥, ¶ | 51.9(37.1,70.2) †, ‡, ∥, ¶ | 44.9(33.2,56.7) ‡, § | 43.5(34.1,54.7) ‡, § |
| PAT *, cm3 | 12.4(6.9,22.4) | 14.9(8.6,30.5) ‡, ∥, ¶ | 11.0(5.4,20.9) †, § | 16.2(8.7,27.4) ‡, ∥, ¶ | 10.8(5.9,16.7) †, § | 10.0(6.0,16.4) †, § |
| TAT *, cm3 | 57.9(42.0,80.5) | 58.5(41.7,86.4) † | 47.3(30.1,67.8) †, §, ∥, ¶ | 67.2(47.7,98.2) ‡, ∥, ¶ | 56.1(41.5,72.8) ‡, § | 55.5(41.0,69.5) ‡, § |
| Hypertension, n(%) | 281(23.4%) | 45(15.5%) | 24(28.6%) | 90(31.8%) | 78(29.6%) | 44(15.8%) |
| Use of antihypertensive, n(%) | 126(10.5%) | 26(9.0%) | 14(16.7%) | 57(20.1%) | 16(6.1%) | 13(4.7%) |
| History of high cholesterol, n(%) | 295(24.6%) | 70(24.1%) | 11(13.1%) | 116(41.0%) | 59(22.35%) | 39(14.0%) |
| Use of lipid lowering medications, n(%) | 123(10.3%) | 38(13.1%) | 5(6.0%) | 66(23.3%) | 10(3.8%) | 4(1.4%) |
| Diabetes, n(%) | 96( 8.1%) | 10(3.5%) | 6(7.2%) | 36(12.7%) | 17(6.4%) | 27(9.7%) |
| Use of anti-diabetic medications, n(%) | 25( 2.1%) | 3(1.0%) | 0(0.0%) | 16(5.6%) | 5(1.9%) | 1(0.4%) |
| Current smoker, n(%) | 314(26.2%) | 20(6.9%) | 26(31.0%) | 35(12.4%) | 127(48.11%) | 106(38.1%) |
| Alcohol consumption >=2 times/week, n(%) | 576(48.0%) | 128(44.1%) | 33(39.3%) | 109(38.5%) | 181(68.6%) | 125(45.0%) |
VAT: visceral adipose tissue; SAT: subcutaneous adipose tissue; EAT: epicardial adipose tissue; PAT: pericardial adipose tissue; TAT: total heart adipose tissue. All variables significantly varied by racial/ethnic groups. P>0.001
Median (Q1, Q3) was presented
Significantly differed from Caucasians, adjusted for multiple comparisons
Significantly differed from African-Americans, adjusted for multiple comparisons
Significantly differed from Japanese-Americans, adjusted for multiple comparisons
Significantly differed from Japanese, adjusted for multiple comparisons
Significantly differed from Koreans, adjusted for multiple comparisons
Race was significantly associated with each ECF depots in both unadjusted and adjusted analyses (Table 2). In minimally adjusted models (Model 1), African-Americans had significantly lower volumes of ECF depots as compared with Caucasians. These differences remained significant after adjusting for BMI or SAT but not for VAT. Additionally, adjusting for age, current smoking, alcohol drinking and BMI or SAT, Japanese-Americans, Japanese and Koreans had significantly higher EAT and TAT as compared with Caucasians. Results for PAT varied based on the adiposity measure that was adjusted for.
Table 2. Associations between Race and ECF Depots Adjusted for Adiposity Measures.
| EAT* | PAT* | TAT* | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| β(SE) | P | β(SE) | P | β(SE) | P | |
|
Model 1: Adjusted for age + current
smoking+ drinking alcohol | ||||||
| Race | <0.001 | <0.001 | <0.001 | |||
| African-Americans | −0.27(0.05) | <0.001 | −0.41(0.11) | 0.001 | −0.31(0.06) | <0.001 |
| Japanese-Americans | 0.15(0.04) | 0.001 | −0.10(0.07) | 0.18 | 0.09(0.04) | 0.03 |
| Japanese | 0.01(0.04) | 0.84 | −0.46(0.08) | <0.001 | −0.10(0.04) | 0.02 |
| Koreans | 0.00(0.04) | 0.98 | −0.53(0.07) | <0.001 | −0.12(0.04) | 0.004 |
| Caucasians | --- | --- | --- | |||
|
| ||||||
| Model1 + BMI | ||||||
|
| ||||||
| Race | <0.001 | <0.001 | <0.001 | |||
| African-Americans | −0.37(0.04) | <0.001 | −0.59(0.09) | <0.001 | −0.42(0.05) | <0.001 |
| Japanese-Americans | 0.15(0.03) | <0.001 | −0.08(0.06) | 0.14 | 0.10(0.03) | 0.002 |
| Japanese | 0.27(0.03) | <0.001 | 0.04(0.06) | 0.49 | 0.22(0.03) | <0.001 |
| Koreans | 0.22(0.03) | <0.001 | −0.12(0.06) | 0.05 | 0.14(0.03) | <0.001 |
| Caucasians | --- | --- | --- | |||
|
| ||||||
| Modell + VAT | ||||||
|
| ||||||
| Race | <0.001 | 0.001 | <0.001 | |||
|
| ||||||
| African-Americans | −0.07(0.04) | 0.10 | −0.04(0.09) | 0.64 | −0.06(0.04) | 0.15 |
| Japanese-Americans | 0.15(0.03) | <0.001 | −0.09(0.06) | 0.13 | 0.09(0.03) | 0.002 |
| Japanese | 0.14(0.03) | <0.001 | −0.21(0.06) | <0.001 | 0.06(0.03) | 0.06 |
| Koreans | 0.17(0.03) | <0.001 | −0.22(0.06) | <0.001 | 0.08(0.03) | 0.01 |
| Caucasians | --- | --- | --- | |||
|
| ||||||
| Model1 + SAT | ||||||
|
| ||||||
| Race | <0.001 | <0.001 | <0.001 | |||
| African-Americans | −0.25(0.04) | <0.001 | −0.38(0.09) | <0.001 | −0.28(0.05) | <0.001 |
| Japanese-Americans | 0.20(0.03) | <0.001 | 0.01(0.06) | 0.86 | 0.16(0.03) | <0.001 |
| Japanese | 0.35(0.03) | <0.001 | 0.17(0.07) | 0.01 | 0.30(0.04) | <0.001 |
| Koreans | 0.33(0.03) | <0.001 | 0.09(0.06) | 0.18 | 0.27(0.03) | <0.001 |
| Caucasians | --- | --- | --- | |||
ECF: ectopic cardiovascular fat; EAT: epicardial adipose tissue; PAT: pericardial adipose tissue; TAT: total heart adipose tissue; BMI: body mass index; VAT: visceral adipose tissue; SAT: subcutaneous adipose tissue. Reference group: Caucasian
Log transformed
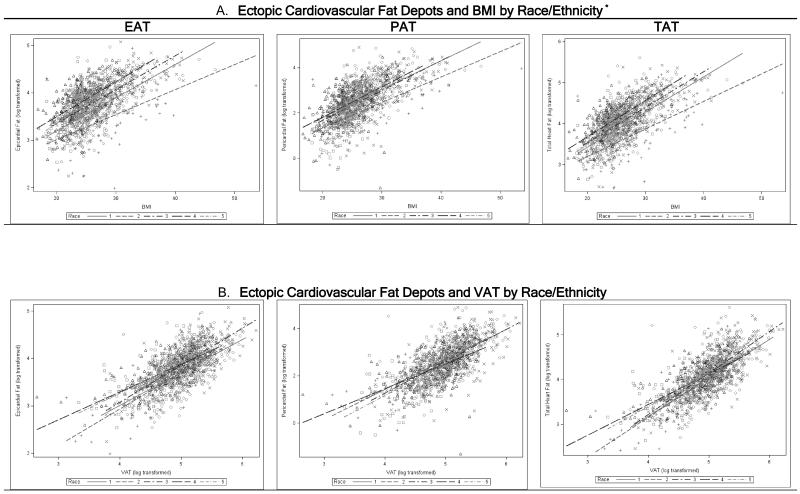
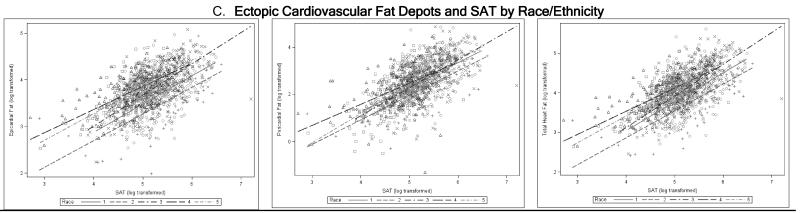
Higher levels of adiposity measures were significantly associated with higher volumes of ECF depots (Figure 1). These positive associations were modified by racial/ethnic groups for BMI (Figure 1. A) and VAT (Figure 1. B) as related to ECF depots. Regression coefficients for interactions between adiposity measures and race/ethnicity as related to ECF depots were presented in Table 3. Compared with Caucasians, African-Americans showed a lower increase in EAT and TAT as related to increases in BMI (Figure 1. A). This was also consistent with the race-specific slopes for EAT and TAT as related to BMI (Table 4). The increments in PAT as related to increases in BMI among African-Americans were similar to that among Caucasians (Figure 1. A and Table 4). Although Japanese-Americans had higher EAT compared with Caucasians, the increments of ECF volumes per 1 unit increase in BMI were similar to that in Caucasians (Figure 1. A and Table 4). Koreans who had the lowest BMI and similar volumes of EAT, PAT and TAT to those in Japanese showed the steepest slopes for BMI as related to ECF depots (Figure 1. A and Table 4).
Figure 1. Scatterplots and Regression Lines of Associations between Ectopic Cardiovascular Fat Depots and Adiposity Measures by Race/Ethnicity.
ECF: ectopic cardiovascular fat; EAT: epicardial adipose tissue; PAT: pericardial adipose tissue; TAT: total heart adipose tissue; VAT: visceral adipose tissue; SAT: subcutaneous adipose tissue. Results adjusted for age, smoking and drinking alcohol. Race/ethnic groups: 1=Caucasians, 2=African-Americans, 3=Japanese-Americans, 4=Japanese, 5=Koreans
* Interactions with race were significant for associations with BMI and VAT but not SAT. All P values <0.05
Table 3. Regression Coefficients for Interactions between Adiposity Measures and Race as related to ECF depots.
| EAT* | PAT* | TAT* | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| β(SE) | P | β(SE) | P | β(SE) | P | |
| Model1 ‡ + BMI + Interaction term | ||||||
|
| ||||||
| Race interaction with BMI | 0.01 | 0.008 | 0.02 | |||
| African-Americans | −0.02(0.01) | 0.04 | −0.01(0.02) | 0.44 | −0.02(0.01) | 0.04 |
| Japanese-Americans | 0.002(0.01) | 0.79 | 0.01(0.01) | 0.58 | 0.001(0.01) | 0.84 |
| Japanese | 0.01(0.01) | 0.47 | 0.01(0.02) | 0.52 | 0.01(0.01) | 0.57 |
| Koreans | 0.02(0.01) | 0.03 | 0.06(0.02) | 0.001 | 0.02(0.01) | 0.05 |
| Caucasians | --- | --- | --- | |||
|
| ||||||
| Model1 † + VAT+ Interaction term | ||||||
|
| ||||||
| Race interaction with VAT | <0.001 | <0.001 | <0.001 | |||
| African-Americans | 0.09(0.08) | 0.23 | 0.04(0.20) | 0.82 | 0.05(0.08) | 0.53 |
| Japanese-Americans | 0.09(0.06) | 0.15 | 0.08(0.13) | 0.52 | 0.07(0.07) | 0.30 |
| Japanese | −0.08(0.06) | 0.21 | −0.19(0.13) | 0.15 | −0.14(0.07) | 0.04 |
| Koreans | −0.26(0.06) | <0.001 | −0.38(0.12) | 0.002 | −0.34(0.06) | <0.001 |
| Caucasians | --- | --- | --- | |||
|
| ||||||
| Model1 † + SAT + Interaction term | ||||||
|
| ||||||
| Race interaction with SAT | 0.23 | 0.14 | 0.10 | |||
| African-Americans | −0.01(0.07) | 0.93 | 0.02(0.15) | 0.90 | −0.02(0.08) | 0.78 |
| Japanese-Americans | 0.06(0.06) | 0.32 | 0.14(0.13) | 0.26 | 0.07(0.07) | 0.30 |
| Japanese | −0.08(0.06) | 0.20 | −0.12(0.13) | 0.34 | −0.11(0.07) | 0.10 |
| Koreans | −0.03(0.07) | 0.61 | 0.19(0.14) | 0.16 | −0.05(0.07) | 0.49 |
| Caucasians | --- | --- | --- | |||
ECF: ectopic cardiovascular fat; EAT: epicardial adipose tissue; PAT: pericardial adipose tissue; TAT: total heart adipose tissue; BMI: body mass index; VAT: visceral adipose tissue; SAT: subcutaneous adipose tissue. Reference group: Caucasian
Log transformed
Model 1: Adjusted for age + current smoking+ drinking alcohol
Table 4. Coefficients and Standardized coefficients for Relationships between Ectopic Cardiovascular Fat Depots and other Adiposity Measures by Race.
| Epicardial Fat (cm3)* |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Caucasians N=290 |
African- Americans N=84 |
Japanese- Americans N=283 |
Japanese N=264 |
Koreans N=278 |
||||||
|
|
||||||||||
| β(SE) | S-β † | β(SE) | S-β † | β(SE) | S-β † | β(SE) | S-β † | β(SE) | S-β † | |
| BMI (Kg/m2) | 0.07(0.01) | 0.64 | 0.05(0.01) | 0.54 | 0.07(0.004) | 0.66 | 0.07(0.01) | 0.61 | 0.09(0.01) | 0.62 |
| VAT (cm2) * | 0.69(0.05) | 0.65 | 0.79(0.08) | 0.76 | 0.77(0.04) | 0.75 | 0.60(0.04) | 0.70 | 0.43(0.04) | 0.58 |
|
| ||||||||||
| Pericardial Fat (cm3)* | ||||||||||
|
| ||||||||||
| Caucasians |
African-
Americans |
Japanese-
Americans |
Japanese | Koreans | ||||||
|
| ||||||||||
| BMI (Kg/m2) | 0.12(0.01) | 0.61 | 0.11(0.01) | 0.65 | 0.13(0.01) | 0.62 | 0.13(0.01) | 0.52 | 0.18(0.01) | 0.61 |
| VAT (cm2) * | 1.25(0.09) | 0.63 | 1.27(0.14) | 0.72 | 1.33(0.09) | 0.65 | 1.07(0.09) | 0.58 | 0.87(0.08) | 0.55 |
|
| ||||||||||
| Total Heart Fat (cm3)* | ||||||||||
| Caucasians |
African-
Americans |
Japanese-
Americans |
Japanese | Koreans | ||||||
|
| ||||||||||
| BMI (Kg/m2) | 0.08(0.01) | 0.66 | 0.07(0.01) | 0.61 | 0.09(0.01) | 0.70 | 0.09(0.01) | 0.65 | 0.10(0.01) | 0.67 |
| VAT (cm2) * | 0.84(0.05) | 0.68 | 0.90(0.08) | 0.78 | 0.91(0.05) | 0.76 | 0.70(0.04) | 0.73 | 0.50(0.04) | 0.61 |
BMI: body mass index; VAT: visceral adipose tissue. Results adjusted for age, smoking and drinking alcohol. All P values <0.001
Log transformed
S-β=Standardized estimates: show the estimated change in Y (in standard deviation units) when X is increased by one standard deviation
Different patterns were observed for the associations between VAT and ECF depots. Increments in ECF depots (mainly EAT) for each unit increase in log VAT were the highest among African-Americans and Japanese-Americans (Figure 1. B and Table 4), however the differences were not statistically significant compared with Caucasians (Table 3). Additionally, Japanese and Koreans who had lower levels of VAT as compared with Caucasians, showed also lower inclines in ECF depots per 1 unit increase in log VAT. Compared with Caucasians, increases in ECF depots were lower among Koreans. Associations between SAT and ECF depots did not vary by race (Figure 1. C, Table 3).
The race-specific standardized slopes for ECF depots as related to VAT and BMI were presented in Table 4. Only in Caucasians, increases in ECF depot volumes in SD units were almost the same for each 1 SD increase in BMI or in log VAT. The increments (in SD units) in ECF volumes per 1 SD increase in log VAT were higher than the increments (in SD units) per 1 SD increase in BMI among African-Americans, Japanese-Americans and Japanese. For Koreans, increases in ECF depots (in SD units) per 1 SD increase in BMI were larger than increases per 1 SD unit in log VAT.
Discussion
Using a large multi-racial/ethnic community-based sample of middle-aged men we demonstrated significant racial/ethnic differences in ECF depots that were independent of overall or central adiposity measures. Median volumes of ECF depots were highest among Japanese-Americans and lowest among African-Americans irrespective of their high BMI. Both Koreans and Japanese, who had lower BMI levels, had higher levels of EAT and TAT compared with Caucasians when accounting for adiposity measures. Moreover, the current study showed that the slopes of the associations between BMI, VAT and each ECF depots differed by racial/ethnic groups with African-Americans having lower increase while Koreans having higher increase compared with Caucasians for each 1 unit increase in BMI. On the other hand, for each 1 unit increase in log VAT, African-Americans, Japanese-Americans and Japanese (except for TAT) showed similar increases, while Koreans showed less increase in ECF volumes compared with Caucasians. These findings suggest that higher levels of ECF volumes were more likely to be driven by changes in VAT than changes in BMI among African-Americans, Japanese-Americans and Japanese, whereas among Koreans higher levels of ECF seemed to be more driven by changes in BMI. The study also suggests that changes in BMI as well as in VAT seemed to have similar influence on ECF volumes among Caucasians. These suggestions need to be confirmed in future longitudinal studies.
Our finding that African-Americans had significantly lower volumes of ECF compared with Caucasians is in agreement with the result from previous studies which evaluated racial/ethnic differences in ECF. (14,15) We reported similar racial/ethnic differences between African-American and Caucasian middle-aged men in volumes of all ECF depots that were independent of BMI and SAT but more interestingly not of VAT. In fact, African-Americans were found to have similar or even slightly higher volumes of ECF to that in Caucasians at higher VAT quartiles (supplemental Table 1). These findings suggest that changes in VAT may have greater influence on ECF volumes in African-American than in Caucasian men. Consistent with this suggestion, the magnitude of the positive change in ECF volumes per 1 unit change in log VAT were found to be greater in African-American than Caucasian men.
These results provide new insights into the paradoxical body of literature which states that despite of a lower level of VAT, African-American men have higher risk of obesity-related CVD than Caucasian men. (10-13) When VAT is ≥ 105.6 cm2, African-American men tended to have similar or even slightly higher volumes of ECF than Caucasian men in the current study. Therefore, the higher CV risk among African-Americans could possibly be due to the greater influence of VAT on ECF volumes than in Caucasians. In support to the-above suggestion, the relationship between ECF (EAT +PAT) and CVD risk factors diminished after further adjustment for VAT among African-Americans. (25)
The mechanism by which VAT may impact ECF deposition is not known. However, VAT is a depot with high lipolytic activity that produces FFA directly into the portal vein. (26) The notable hyperlipolytic activity of VAT induces a lipotoxic state that increases the exposure of the liver, skeletal muscle and cardiovascular system to excess FFA. When levels of circulating FFA increase, both circulating levels of adiponectin and leptin resistance decrease, which in turns reduce lipid oxidation in non-adipose tissues and therefore contribute to the accumulation of ectopic fat, lipotoxicity and insulin resistance. (27) Therefore, it may be possible that the lipolytic activity of VAT is much higher in African-Americans compared with Caucasians irrespective of its size.
Despite similar levels of BMI, VAT and SAT, Japanese-Americans had significantly higher volumes of EAT but not of PAT as compared to Caucasians. This suggests that ECF accumulation indeed varies by location for certain racial/ethnic groups. Given the proximity of EAT to the myocardium and coronary arteries as compared to PAT, these differences may subject Japanese-Americans to a greater risk of CVD as compared to Caucasians. EAT has distinct endocrine properties such as greater fatty acid synthesis and breakdown, and greater insulin-induced lipogenesis compared with PAT. (28) The higher volume of EAT in Japanese-Americans may contribute to their higher coronary atherosclerosis as compared with Caucasians which we previously reported.(16) More research is needed to test this hypothesis.
The case is different among Asian men from Japan and Korea. Irrespective of higher volumes of EAT and TAT in Japanese and Koreans as compared with Caucasians when adjusting for adiposity measures, the magnitude of change in each ECF depot (mainly TAT) per 1 unit increase in log VAT was significantly less in Japanese and Korean men. These results may partly help explain the findings that Asians have lower risk of coronary artery disease compared with Caucasians. (16,29) Asians may be at lower risk than Caucasians via the smaller influence of VAT on levels of TAT volume. Interestingly, in the current study, Japanese and Korean men had significantly lower levels of VAT compared with Caucasian men.
According to the ectopic fat theory, ectopic fat accumulation around organs such as the heart could be a consequence of impairment in SAT ability to buffer energy excess. (8,9) In compliance with this, the current study showed that EAT volumes tend to be higher in racial/ethnic groups with lower SAT (Japanese-Americans, Japanese and Koreans as compared with Caucasians) and lower in racial/ethnic groups with higher SAT (African-Americans as compared with Caucasians).
There are several limitations to the current findings. The cross-sectional design did not permit assessing temporality. The unavailability of total body fat prevented us from evaluating the association between total fat and ECF volumes; however we used BMI as a surrogate marker. The limited sample size of African-Americans may result in less power to detect significant differences with other racial/ethnic groups. Non-significant results mean that the data provide little or no evidence that the null hypothesis is false, yet with our sample size per each group we have 80% power to detect a minimum difference of 5.1 cm3 in EAT between each group and Caucasian group (except for comparison with African Americans) at an alpha level of 0.05. Finally, the current findings may not be generalized to women or unevaluated racial/ethnic groups.
Our findings provide new insights that may help in explaining paradoxical risk in certain racial/ethnic groups. The current findings call for a longitudinal assessment of the impact of changes in adiposity measures on ECF accumulation overtime. It is crucial to evaluate whether VAT reduction will decrease ECF volumes in certain racial/ethnic groups while overall weight loss will reduce ECF in other racial/ethnic groups. Evaluating these questions will help in designing the right prevention strategy to reduce risk of CVD associated with higher ECF volumes. (4-7)
In conclusion, significant racial/ethnic differences existed in ECF volumes and their relationships with adiposity measures. The results suggested that racial/ethnic groups differed in their propensity to accumulate ECF at increasing level of overall and central adiposity.
Supplementary Material
Acknowledgments
Funding Source:
The work was supported by grants HL068200, HL071561, from the National Institutes of Health, USA (Bethesda, MD, USA), Korea Center for Disease Control and Prevention (Government budget code: 2004-E71001-00, 205-E71001-00), and grants B 16790335, A 13307016, 17209023, 21249043, A 25253046, and B 23390174 from the Japanese Ministry of Education, Culture, Sports, Science and Technology (Tokyo, Japan).
Footnotes
Conflict of interest: none.
Supplementary information is available at International Journal of Obesity website.
References
- 1.Gao YJ, Takemori K, Su LY, An WS, Lu C, Sharma AM, et al. Perivascular adipose tissue promotes vasoconstriction: the role of superoxide anion. Cardiovasc Res. 2006;71:363–373. doi: 10.1016/j.cardiores.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 2.Iacobellis G, Pistilli D, Gucciardo M, Leonetti F, Miraldi F, Brancaccio G, et al. Adiponectin expression in human epicardial adipose tissue in vivo is lower in patients with coronary artery disease. Cytokine. 2005;29:251–255. doi: 10.1016/j.cyto.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H, et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003;108:2460–2466. doi: 10.1161/01.CIR.0000099542.57313.C5. [DOI] [PubMed] [Google Scholar]
- 4.Iacobellis G, Ribaudo MC, Assael F, Vecci E, Tiberti C, Zappaterreno A, et al. Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: a new indicator of cardiovascular risk. J Clin Endocrinol Metab. 2003;88:5163–5168. doi: 10.1210/jc.2003-030698. [DOI] [PubMed] [Google Scholar]
- 5.Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA, Vasan RS, et al. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation. 2008;117:605–613. doi: 10.1161/CIRCULATIONAHA.107.743062. [DOI] [PubMed] [Google Scholar]
- 6.Lehman SJ, Massaro JM, Schlett CL, O’Donnell CJ, Hoffmann U, Fox CS. Peri-aortic fat, cardiovascular disease risk factors, and aortic calcification: the Framingham Heart Study. Atherosclerosis. 2010;210:656–661. doi: 10.1016/j.atherosclerosis.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mahabadi AA, Massaro JM, Rosito GA, Levy D, Murabito JM, Wolf PA, et al. Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: the Framingham Heart Study. Eur Heart J. 2009;30:850–856. doi: 10.1093/eurheartj/ehn573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ravussin E, Smith SR. Increased fat intake, impaired fat oxidation, and failure of fat cell proliferation result in ectopic fat storage, insulin resistance, and type 2 diabetes mellitus. Ann N Y Acad Sci. 2002;967:363–378. doi: 10.1111/j.1749-6632.2002.tb04292.x. [DOI] [PubMed] [Google Scholar]
- 9.Després JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444:881–887. doi: 10.1038/nature05488. [DOI] [PubMed] [Google Scholar]
- 10.Stanforth PR, Jackson AS, Green JS, Gagnon J, Rankinen T, Desprès JP, et al. Generalized abdominal visceral fat prediction models for Black and White adults aged 17-65 y: the Heritage Family Study. Int J Obes. 2004;28:925–932. doi: 10.1038/sj.ijo.0802563. [DOI] [PubMed] [Google Scholar]
- 11.Hoffman DJ, Wang ZM, Gallagher D, Heymsfield SB. Comparison of visceral adipose tissue mass in adult African Americans and Whites. Obes Res. 2005;13:66–74. doi: 10.1038/oby.2005.9. [DOI] [PubMed] [Google Scholar]
- 12.Hill JO, Sidney S, Lewis CE, Tolan K, Scherzinger AL, Stamm ER. Racial differences in amounts of visceral adipose tissue in young adults: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Am J Clin Nutr. 1999;69:381–387. doi: 10.1093/ajcn/69.3.381. [DOI] [PubMed] [Google Scholar]
- 13.Kadowaki T, Sekikawa A, Murata K, et al. Japanese men have larger areas of visceral adipose tissue than Caucasian men in the same levels of waist circumference in a population-based study. Int J Obes (Lond) 2006;30:1163–1165. doi: 10.1038/sj.ijo.0803248. [DOI] [PubMed] [Google Scholar]
- 14.Salami SS, Tucciarone M, Bess R, Kolluru A, Szpunar S, Rosman H, et al. Race and epicardial fat: the impact of anthropometric measurements, percent body fat and sex. Ethn Dis. 2013;23:281–285. [PubMed] [Google Scholar]
- 15.Willens HJ, Gómez-Marín O, Chirinos JA, Goldberg R, Lowery MH, Iacobellis G. Comparison of epicardial and pericardial fat thickness assessed by echocardiography in African American and non-Hispanic White men: a pilot study. Ethn Dis. 2008;18:311–316. [PubMed] [Google Scholar]
- 16.Sekikawa A, Curb JD, Ueshima H, El-Saed A, Kadowaki T, Abbott RD, et al. Marine-derived n-3 fatty acids and atherosclerosis in Japanese, Japanese-American, and white men: a cross-sectional study. J Am Coll Cardiol. 2008;52:417–424. doi: 10.1016/j.jacc.2008.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Saed A, Sekikawa A, Edmundowicz D, Evans RW, Sutton-Tyrrell K, Kadowaki T, et al. Coronary calcification is more predictive of carotid intimal medial thickness in black compared to white middle aged men. Atherosclerosis. 2008;196:913–918. doi: 10.1016/j.atherosclerosis.2007.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sekikawa A, Shin C, Curb JD, Barinas-Mitchell E, Masaki K, El-Saed A, et al. Aortic stiffness and calcification in men in a population-based international study. Atherosclerosis. 2012;222:473–477. doi: 10.1016/j.atherosclerosis.2012.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kagan A, Harris BR, Winkelstein W, Jr, Johnson KG, Kato H, Syme SL, et al. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California: demographic, physical, dietary and biochemical characteristics. J Chronic Dis. 1974;27:345–364. doi: 10.1016/0021-9681(74)90014-9. [DOI] [PubMed] [Google Scholar]
- 20.Abbott RD, Ueshima H, Rodriguez BL, Kadowaki T, Masaki KH, Willcox BJ, et al. Coronary artery calcification in Japanese men in Japan and Hawaii. Am J Epidemiol. 2007;166:1280–1287. doi: 10.1093/aje/kwm201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ding J, Kritchevsky SB, Harris TB, Burke GL, Detrano RC, Szklo M, et al. The association of pericardial fat with calcified coronary plaque. Obesity (Silver Spring) 2008;16:1914–1919. doi: 10.1038/oby.2008.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Azuma K, Kadowaki T, Cetinel C, Kadota A, El-Saed A, Kadowaki S, et al. Higher liver fat content among Japanese in Japan compared with non-Hispanic whites in the United States. Metabolism. 2009;58:1200–1207. doi: 10.1016/j.metabol.2009.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee S, Janssen I, Ross R. Interindividual variation in abdominal subcutaneous and visceral adipose tissue: influence of measurement site. J Appl Physiol (1985) 2004;97:948–954. doi: 10.1152/japplphysiol.01200.2003. [DOI] [PubMed] [Google Scholar]
- 24.Shen W, Punyanitya M, Wang Z, Gallagher D, St-Onge MP, Albu J, et al. Visceral adipose tissue: relations between single-slice areas and total volume. Am J Clin Nutr. 2004;80:271–272. doi: 10.1093/ajcn/80.2.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu J, Fox CS, Hickson D, Sarpong D, Ekunwe L, May WD, et al. Pericardial adipose tissue, atherosclerosis, and cardiovascular disease risk factors: the Jackson heart study. Diabetes Care. 2010;33:1635–1639. doi: 10.2337/dc10-0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ferrannini E, Sironi AM, Iozzo P, Gastaldelli A. Intra-abdominal adiposity, abdominal obesity, and cardiometabolic risk. European Heart Journal Supplements. 2008;10(Supplement B):B4–B10. [Google Scholar]
- 27.Lionetti L, Mollica MP, Lombardi A, Cavaliere G, Gifuni G, Barletta A. From chronic overnutrition to insulin resistance: the role of fat-storing capacity and inflammation. Nutr Metab Cardiovasc Dis. 2009;19:146–152. doi: 10.1016/j.numecd.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 28.Rabkin SW. Epicardial fat: properties, function and relationship to obesity. Obes Rev. 2007;8:253–2561. doi: 10.1111/j.1467-789X.2006.00293.x. [DOI] [PubMed] [Google Scholar]
- 29.Fujiyoshi A, Sekikawa A, Shin C, Masaki K, David Curb J, Ohkubo T, et al. A cross-sectional association of obesity with coronary calcium among Japanese, Koreans, Japanese Americans, and U.S. whites. Eur Heart J Cardiovasc Imaging. 2013;14:921–927. doi: 10.1093/ehjci/jet080. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.