Abstract
Sexual abstinence is often deemed the “safest behavior” in HIV prevention, but is sometimes associated with psychological symptoms (e.g., depression) just as sexually risky behavior is. This study explored whether sexual abstinence and risky sexual behavior among men with HIV are associated with similar constellations of psychological symptoms. Prior research has not addressed this issue because abstinent people often are not included in the sample, or when data are analyzed, researchers combine abstinent people with sexually active people who practice safer sex. Past research also neglects the co-morbidity of psychological symptoms. A latent class analysis of the psychological symptoms (assessed with the Symptom Check List 90-R; Derogatis, 1994) of 140 men with HIV, mostly from rural New England, revealed three latent classes; men who were asymptomatic on all symptom domains (28.8%), men who were symptomatic on all domains (34.1%), and men who were symptomatic on internalizing domains (37.1%), but were asymptomatic on the externalizing symptoms of hostility and paranoid ideation. Logistic regression showed that sexual behavior during the past 90 days of men in the all symptom class and the internalizing symptoms class was similar, with abstinence and risky sex predominating, and safer sex being relatively uncommon for both classes. The sexual behavior of men in the asymptomatic class differed, with safer sex being relatively more likely to occur compared to the symptomatic classes. These findings suggest that the psychological symptom profile of sexually abstinent people places them at risk for inconsistent condom use should they engage in sexual behavior.
Keywords: Abstinence (Sexual), HIV, Sexual Risk Taking, Symptoms
Sexual abstainers are commonly perceived to be at low risk in the HIV transmission equation, but abstinence can be difficult to maintain over time (Celentano, Muñoz, Cohn, & Vlahov, 2001) and may result from lack of opportunity, rather than a motivation to prevent transmission (Bogart et al., 2006). Moreover, there is some evidence indicating that abstinent individuals are psychologically distressed in much the same way as are individuals who engage in risky sex (Varni, Miller, & Solomon, 2012). Abstinence, especially abstinence arising from lack of opportunity, is associated with psychological symptoms such as depressed mood (Donnelly, Burgess, Anderson, Davis, & Dillard, 2001; Wagner, Rabkin, & Rabkin, 1993), anger, and frustration (Donnelly, et al., 2001).
Researchers have long suspected that psychological distress can instigate risky sexual behavior, but this relationship is not well understood (Crepaz & Marks, 2001). We hypothesize that this may be because psychological symptoms also play an important role in abstinence. There are several reasons why it is important to understand whether and how psychological distress is implicated in both risky sexual behavior and abstinence. HIV prevention efforts frequently target at-risk populations, and thus do not focus much on abstinent people. Abstinent people might well become sexually active as their life circumstances change, and psychological distress may put them at risk of engaging in unsafe sex should they become sexually active. In addition, providing appropriate services and encouraging sexually risky individuals to become safer may be hampered by lack of knowledge about how psychological distress may be implicated in risky behavior.
The possibility that abstinent people and those who engage in risky sex may both experience similar types of psychological distress has not been investigated much because researchers often screen out abstinent people during study recruitment (Ethier et al., 2006; Golub et al., 2013; Hart & Heimberg, 2005; Mayer et al., 2010; Schroder, Johnson, & Wiebe, 2009; Seth et al., 2011; Williams & Latkin, 2005) or combine them with people practicing safe sex during data analysis (O’Cleirigh et al., 2013; Pines et al., 2014; Shiu, Chen, Tseng, Chung, Wu, Hsu, & Ko, in press). This might obscure the link between psychological distress and sexual risk, especially if abstinent and risky people possess similar levels of psychological distress. This study investigated the hypothesis that psychological distress in men with HIV is linked with both abstinence and risky sex.
In a meta-analysis of the relationship of the first generation of studies on negative affect and sexually risky behavior, Crepaz and Marks (2001) found that the effect size for the relationship between psychological distress and sexually risky behavior was small (average effect size = .05) and did not differ significantly from zero (representing no effect). Effect sizes also were significantly variable, ranging from +0.55 (indicating that risky sex increased as psychological symptoms increased) to −0.41 (indicating that risky sex decreased as symptoms increased). The variability in effect sizes was not moderated by any of the potential moderators Crepaz & Marks (2001) examined, including study quality, study population (HIV positive or negative), which type of distress was examined (depression, anxiety, or anger), or how closely the measures of affect and sexual behavior corresponded with respect to the time period about which participants reported. It also is important to recognize that the studies examined in Crepaz & Marks’ (2001) review were almost as likely to show a negative relationship between psychological symptoms and risky sexual behavior as they were to show a positive relationship.
Research published since this influential review appeared continues to produce inconsistent findings. Some researchers have indeed found that psychological symptoms such as depression and anxiety are associated with increased sexual risk (Brown et al., 2006; Ethier, et al., 2006; Mustanski, Garofalo, Herrick, & Donenberg, 2007; Reisner et al., 2009). The most compelling of these are longitudinal studies, which indicate that depression prospectively predicts sexually risky behavior (Brown, et al., 2006; Seth, et al., 2011; Williams & Latkin, 2005).
However, other recent research has found no relationship between psychological distress and risky sexual behavior. Mayer et al. (2010) examined risky sexual behavior and diagnosis with a sexually transmitted disease among men with HIV. They found several variables related to these indices of risk, including time since diagnosis with HIV and use of illegal drugs. However, none of the several types of psychological distress they assessed, including depression, anxiety, panic disorder, and post-traumatic stress were related to risky sexual behavior or to being diagnosed with a sexually transmitted disease. Other researchers who examined multiple behavioral and health problems have found that depression is unrelated to high risk sexual behavior (Senn, Carey, & Vanable, 2010) or that the relationship between depression and high risk sexual behavior is eliminated when other behavioral and health problems are included in a multivariate model (Parsons, Grov, & Golub, 2012). One recent longitudinal study (Comulada et al., 2010) found a negative relationship between psychological symptoms and risky sexual behavior at baseline, and increases in symptoms over time were associated with decreases in sexually risky behavior. Tsai et al. (2013) reported that in a randomized clinical trial of the effects of treatment for depression on men with HIV, those who received an intervention that was efficacious in alleviating their depression showed no subsequent reduction in risky sexual behavior over a 36-week period.
The rationale for hypothesizing that psychological symptoms should be related to risky sexual behavior is that symptoms instigate cognitive and motivational processes, for example, the perception of risk, that promote risky behavior (Seth, et al., 2011). Symptoms such as depression can lead to cognitive distortions, which can deter rational decision-making and allow emotions to influence behavior (A. T. Beck, 1979; J. S. Beck, 2011). People also may engage in self-gratifying behaviors to distract themselves from negative feelings associated with psychological symptoms, and motivation to care for the well-being of oneself and other people also can be affected (Crepaz & Marks, 2001; Seth, et al., 2011). A number of researchers have pointed out that at very high levels of psychological distress, some of these processes could lead people to avoid sexual activity completely (Crepaz & Marks, 2001; O’Cleirigh, et al., 2013; Seth, et al., 2011). Consequently, increasing distress may increase high-risk sexual behavior only to a point, and then distress becomes so severe that the person’s willingness or ability to engage in sexual relationships is compromised. According to this reasoning, the most risky behavior would occur at moderate levels of distress.
There has been some research that has examined non-linear relationships between psychological symptoms and high-risk sexual behavior. For example, Koblin, Husnik, Colfax, Huang et al. (2006) studied a large (over 4,000 participants) high risk sample of HIV-negative men who have sex with men (MSM) over a 48-month period. When they examined the bivariate relationship between depression and changes in serostatus during the follow-up period, they found a linear relationship with increasing depression related to increased likelihood of the men becoming HIV positive. However, in a multivariate analysis in which other risk factors were included, only mild depression (defined as depression scores in the second lowest quartile for the sample) continued to be a significant predictor of seroconversion. O’Cleirigh et al. (2013) found that among MSM with HIV who were participating in a multi-site study of HIV prevention, those who had baseline moderate levels of depression (defined as a depression score falling in second or third quartiles for the total sample) showed smaller reductions in risky sexual behavior over time compared to those who scored in the lowest or the highest quartiles. In addition, a study of 620 MSM who were recruited at a community health center in metropolitan Taiwan found an inverted U-shaped relationship between depression and unprotected anal and oral sex (Shiu, Chen, Tseng, Chung, Wu, Hsu, & Ko, 2014).
In all of these studies sexually abstinent men either were not included (Koblin, et al., 2006) or were not examined separately from sexually active men who had safer sex (Myers et al., 2010; O’Cleirigh, et al., 2013; Shiu et al., in press). Thus, these studies may have left out an important “tail” of the distribution of distress – those whose high level of depression may have led them to avoid sex. In addition, in these studies “moderate” depression was defined relative to the specific samples under investigation. Samples with greater or lesser levels of depression might produce different findings with respect to whether moderately depressed people are the most risky.
Other investigators have proposed that understanding the role of psychological symptoms in risky sexual behavior requires taking into account the co-morbidity of psychological symptoms (Krueger & Markon, 2006) and other risk factors (Klein, 2011; Stall et al., 2003). Much of the research on psychological symptoms and risky sexual behavior has focused on bivariate relationships between one symptom or type of distress and engaging in behaviors that risk the transmission of HIV. This approach ignores the synergies that may occur with different symptom combinations (Safren, Reisner, Herrick, Mimiaga, & Stall, 2010). Researchers taking a syndemic approach suggest that multiple social and psychological forces converge to affect behavioral risk factors in complex ways in which the effects of one variable can amplify or modulate the effects of another. For example, in a study of MSM in New York City, Parsons et al. (2012) found that polydrug use, partner violence, childhood sexual abuse, risky sexual behavior, and depression are correlated with one another. They also found that as the number of psychosocial vulnerabilities increases, the incidence of high risk sexual behavior increases in an additive fashion, a finding consistent with other studies using a syndemic approach (Mustanski, et al., 2007; Senn, et al., 2010).
Although the syndemic approach casts a much broader net than the present study does in terms of the types of variables it examines, its emphasis on the way that one condition can affect another suggests that a fruitful approach to understanding the effects of psychological symptoms on risky sexual behavior is to examine groups of co-occurring symptoms. The approach used in the present study to achieve this objective was Latent Class Analysis (LCA; Collins & Lanza, 2010).
LCA is a person-centered approach that describes constellations or groupings of attributes that characterize individuals. Variable-centered approaches, such as factor analysis, identify relationships between variables, and assume that these relationships apply across all people, whereas person-centered approaches describe individuals on the basis of their patterns of individual characteristics (Bergman, Magnusson, & El-Khouri, 2003). LCA groups individuals into distinct classes, based on their responses to categorical variables (Althoff, Rettew, Boomsma, & Hudziak, 2009; Rutledge, Siebert, Siebert, & Chonody, 2012). This allows a shift in focus from single psychological symptoms to one in which multiple symptoms are considered. As the name implies, the classes that emerge from this analysis are latent variables that are measured indirectly based on the individual’s standing on two or more observed categorical variables.
LCA organizes the categorical variables such that the pattern of categorical responses is equivalent within a particular latent class, and different from the pattern of responses observed in the other resulting latent classes. For example, a latent class analysis of the co-occurrence of being symptomatic on anxiety, depression, and hostility can be understood in simplified terms by imagining the person is assigned a “1” if he or she crosses a threshold indicative of clinically significant levels of distress, and a “0” if the person is below that threshold. The number of possible combinations of three symptoms would be eight, but only some of those combinations may actually be present in individuals. Hypothetical results could include the pattern “1 1 0” (symptomatic for anxiety and depression, but not hostility)"1 1 1” (symptomatic on all three symptoms)"1 0 1” (symptomatic on anxiety and hostility, but not depression) and so on. Note that in all of these patterns individuals are symptomatic on anxiety. What differentiates the patterns (latent classes) is whether people in that class also are symptomatic on depression and/or hostility.
Previous research (Mustanski, et al., 2007; Stall, et al., 2003) has found that that the odds of risky sexual behaviors increase as the number of psychosocial health problems increase. However, by taking a LCA approach we are able to focus on specific patterns in which the symptoms aggregate and not simply the number of symptoms present. The current study employed LCA to identify latent class profiles of psychological symptom clusters of men living with HIV to better understand how symptoms are related to sexual abstinence, inconsistent condom use and consistent condom use. We hypothesized that sexual abstinence and risky sexual behavior among men living with HIV would be associated with similar psychological symptom profiles, and that these profiles would differ from those associated with engaging in safer sex.
Method
Participants
Participants in the current study were 148 men with HIV. They were recruited as part of a larger project (Miller, Bunn, Grover, & Solomon, 2014: Miller, Grover, Bunn, & Solomon, 2011; Varni, Miller, McCuin, & Solomon, 2012; Varni, Miller, & Solomon, 2012).) that involved extensive assessment of HIV stigma as it is experienced by men and women with HIV in rural New England, and as it is expressed by the communities in which they live (Miller, Bunn, Grover, & Solomon, 2014: Miller, Grover, Bunn, & Solomon, 2011; Varni, Miller, McCuin, & Solomon, 2012; Varni, Miller, & Solomon, 2012). Data from three male participants were not recorded due to computer errors, and five men did not answer questions about their sexual behavior. This resulted in a final sample size of 140 men. The 55 women who had participated in the parent project were not included in the current analysis because the outcome of interest was condom use among men living with HIV and the issues involved in condom use are different for men and women.
Recruitment of participants was conducted through medical centers, regional infectious disease clinics, and clinics providing comprehensive care to individuals with HIV in Vermont, New Hampshire and neighboring states. We also recruited participants through local newspaper advertisements, word-of-mouth and through AIDS Services Organizations (ASOs) or community based organizations providing advocacy services to individuals with HIV. Eligibility requirements were that the participants were 18 years of age or older, had been diagnosed with HIV or AIDS, and could speak, read and write the English language without assistance. All study recruitment and procedures were approved by the university Institutional Review Board.
Procedure
Participants completed the study protocol at project research space located on campus or at an off-site facility (e.g., ASO or hospital-based infectious disease clinic). Data were collected in sessions lasting approximately two hours using computer-assisted survey software (MediaLab; Jarvis, 2004). At the conclusion of the session, participants were reimbursed for their time and travel expenses.
Demographic and Other Descriptive Measures
Participants indicated their age (in years). Sexual orientation was assessed on a seven-point rating scale with anchors labeled “exclusively heterosexual” (1) “bisexual” (4), and “exclusively heterosexual” (7). Participants were classified as exclusively heterosexual if they responded by selecting “1,” and otherwise were categorized as bisexual/homosexual.
Participants identified their race/ethnicity by choosing as many categories as they wanted from a list that included African American, Asian American/Pacific Islander, Latina/Latino/Hispanic, Native American/American Indian, White/Caucasian/European, biracial, or other. Those who selected anything other than “White/Caucasian/European” were classified as men of color. Participants indicated their annual income by choosing from among ranges that included “under $11,000” and ranged in $10,000 increments up to “over $75,000” with an additional option to report no independent income. Nearly three quarters of the sample reported annual incomes in the lowest three brackets, and consequently the highest three brackets were collapsed into a single category of “$31,000 or higher.” Participants reported the highest level of education they had completed by selecting from the following options: no formal education, primary elementary school, middle school, high school, college/technical school, or graduate/professional school. Participants answered a single item (yes/no) to report whether or not they were in a current relationship with a spouse or partner.
Measures of Sexual Behavior and Psychological Symptoms
NIMH Multisite HIV Prevention Trial Survey (Fishbein & Coutinho, 1997)
The participants’ sexual behavior was assessed with the NIMH Multisite Prevention Survey. This measure asks participants to answer detailed questions about their sexual behavior. Self-report offers a relatively unobtrusive way to measure a very private behavior (Fenton, Johnson, McManus, & Erens, 2001). Participants were asked about a specific time frame of the previous 90 days to reduce recall bias. The questions also explicitly defined the sexual behaviors in lay-terms to help avoid misinterpretation.
Participants reported whether or not they had vaginal, anal and/or oral sex over the previous 90 days. If they answered affirmatively, they were asked to estimate their condom use separately for oral sex and for vaginal or anal sex, with responses ranging from “all of the time” to “never.” Participants who answered that they used condoms all of the time for both vaginal/anal and oral sex were classified as consistent condom users. Participants who reported that they used condoms inconsistently for vaginal/anal and/or oral sex were classified as inconsistent condom users. Participants who reported that they had not had vaginal, anal, or oral sex in the past 90 days were classified as abstinent. This label is intended only as a descriptive label without any connotation about whether they chose to be abstinent or refrained from sex to prevent HIV infection risk. The questionnaire also included detailed questions about up to three specific sexual partners. However, participants were not reminded of how many times they said they engaged in a particular sexual behavior with each partner when they reported the number of times they used condoms with that partner. This resulted in inconsistencies in the ratio of frequency of condom use to frequency of sexual behavior. Consequently, the present study focused on the questions about use of condoms in general for particular types of sexual behavior.
Symptom Check List 90-Revised. (SCL-90-R; Derogatis, 1994 )
The SCL-90-R is a 90-item self-report measure assessing psychological symptoms across nine domains. The domains were developed to assess symptoms that have been documented in the scientific literature and which are targeted for clinical intervention. Several domains parallel the major diagnostic categories that are standard in clinical practice, as described by the DSM-IV-TR (American Psychiatric Association, 2000). These domains include depression (e.g., feeling blue; 13 items), anxiety (e.g., feeling fearful; 10 items), phobic anxiety (e.g., feeling afraid to go out of your house alone; 7 items), obsessive-compulsive (e.g., having to check and double-check what you do; 10 items), somatization (e.g., nausea or upset stomach; 12 items), paranoid ideation (e.g., feeling that you are watched or talked about by others; 6 items), and psychoticism (e.g., hearing voices that other people do not hear; 10 items) dimensions. Domains that included symptoms that are more diffuse across different DSM-IV-TR diagnostic categories are hostility (e.g., feeling easily annoyed or irritated; 6 items) and interpersonal sensitivity (e.g., feeling very self-conscious with others; 9 items). Participants read short descriptions of each of the symptoms associated with all nine of the domains and reported how much they were distressed by each symptom over the past week on a scale ranging from 0 (not at all) to 4 (extremely). Domain scores were obtained in accord with standard scoring procedures by calculating the mean of items in each domain. Alpha coefficients ranged from 0.84 to 0.93. Standard scoring of the SCL-90-R also produces a global severity index (GSI), which is calculated across all items in the above domains, plus responses to seven items that are clinically significant for treatment but are not part of a domain (e.g., poor appetite; feelings of guilt).
The SCL-90-R includes validated cut-offs for clinically significant levels of symptoms based on population norms. For each domain and the GSI, raw scores were converted to standardized T-scores based on general population norms provided in the scoring manual. A T-score of 60 indicates that a person is in the 84th percentile of a normal population, and thus has a clinically significant elevation in symptoms in that domain (Derogatis, 1994). Using standardized scores allows for comparison of symptoms across domains. Thus, the SCL-90-R produces a dichotomous score that indicates whether individuals are symptomatic or asymptomatic in a particular domain.
Statistical Analysis
A series of LCAs (Collins & Lanza, 2010) were conducted to identify latent classes based on whether participants were symptomatic or asymptomatic on each domain of the SCL-90-R. Solutions with from one to five classes were examined, with the selection of the best-fitting solution based on the Bayesian Information Criteria (BIC), the Akaike Information Criteria (AIC) and the G-squared statistic. Once the best fitting solution was identified, the posterior probability of belonging to a specific latent class was calculated for each participant. Participants were then categorized as being in the latent class for which they had the highest probability. Multinomial logistic regression was used to examine the relationship between psychological latent class and sexual behavior/condom use. This was performed in two steps. Step 1 included demographic characteristics, and Step 2 included these variables as well as participants’ latent symptom class. The latent class analysis was performed using the proc lca procedure developed for SAS (Lanza, Dziak, Huang, Xu, & Collins, 2011; SAS Institute Inc., 2011). The multinomial logistic regression was performed using the proc logistic procedure of SAS.
Results
Descriptive Statistics for Participant Characteristics
Participants were predominantly White (n = 114; 81.4%), homosexual or bisexual (n = 105; 75.0%), and currently married or in a relationship (n = 81, 57.9%). Their average age was 43.69 years (SD = 8.24), and they had been diagnosed with HIV for an average of 11.36 years (SD = 6.30). The highest level of education completed by 42.9% (n = 60) of participants was high school or GED, another 45.0% (n = 63) had completed college or technical school; and 12.1% (n = 17) had completed graduate or professional school. The modal income was under $11,000 annually (n = 65, 46.4%), with 22.1% (n = 31) reporting an income between $11,000 and $20,000, 12.9% (n = 18) reporting an income between $21,000 and $30,000, and 18.6% (n = 26) reporting an income of $31,000 or more.
Overall, men in this study reported high levels of psychological distress on the SCL-90-R. The vast majority (82.1%, n = 115) scored above the cutoff for significant distress on at least one of the nine domains, and 66.4% (n = 93) had a GSI T-score greater than 60. As can be seen in Table 1, the majority of the men had T-scores greater than 60 for every domain except for hostility and paranoid ideation. What may distinguish these domains from the other domains of the SCL-90-R is that they capture thoughts and feelings directed toward other people rather than toward the self. Finally, 45.0% of participants (n = 63) were abstinent during the previous 90 days, 37.9% (n = 53) were inconsistent condom users, and 17.1% (n = 24) were consistent condom users.
Table 1.
Percentage of Participants With T-scores In the Clinical and Nonclinical Range on SCL-90-R Domains
| Psychological Symptom | % T-score < 60 | % T-score ≥ 60 |
|---|---|---|
| Global Severity Index | 33.6 | 66.4 |
| (47) | (93) | |
| Somatization | 45.7 | 54.3 |
| (64) | (76) | |
| Obsessive Compulsive Disorder | 39.3 | 60.7 |
| (55) | (85) | |
| Interpersonal Sensitivity | 44.3 | 55.7 |
| (62) | (78) | |
| Depression | 35.0 | 65.0 |
| (49) | (91) | |
| Anxiety | 47.9 | 52.1 |
| (67) | (73) | |
| Hostility | 62.9 | 37.1 |
| (88) | (52) | |
| Phobic Anxiety | 43.6 | 56.4 |
| (61) | (79) | |
| Paranoid Ideation | 65.0 | 35.0 |
| (91) | (49) | |
| Psychoticism | 34.3 | 65.7 |
| (48) | (92) |
Note: Numbers in parentheses are ns.
Latent Class Analysis
Identification of classes
Table 2 shows the AIC, BIC, and G2 statistics for models that have from one to five latent classes. The AIC and BIC are information criteria which provide a way to compare the relative balance between model fit and parsimony. These information criteria impose a penalty on G2, the index of absolute model fit, such that G2 is directly related to the number of classes in the model. G2 decreases as the number of parameters increases. Choosing the best fitting model requires a judgment about which solution optimizes BIC and AIC, with lower values indicative of better fit. When models with differing numbers of classes have essentially equivalent AIC or BIC, the model with fewer classes is preferred because it is more parsimonious. The fit statistics in Table 2 show that the 3-class solution had the lowest BIC of all the models. In addition, AIC became successively smaller as the number of classes increased from one to three classes, and then leveled off after three classes. The AIC and BIC thus suggested that the 3-class solution is the preferred solution. LCA assumes conditional independence of items (symptoms) within classes. We used the methods recommended by Collins and Lanza (http://methodology.psu.edu/ra/lca/faq#t21n124) to examine the assumption of local independence among the symptom domains. The results indicated that the assumption of local independence holds for these data.
Table 2.
Fit Statistics for Five Psychological Symptom Latent Classes That Were Considered
| Number of latent classes |
G2 | AIC | BIC |
|---|---|---|---|
| 1 | 725.19 | 743.19 | 769.66 |
| 2 | 279.87 | 317.87 | 373.76 |
| 3 | 198.39 | 256.39 | 341.70 |
| 4 | 180.52 | 258.52 | 373.25 |
| 5 | 155.32 | 253.32 | 397.46 |
Table 3 shows the probabilities of each of the three latent classes for participants being symptomatic on each domain of the SCL-90-R. In the first latent class, which described 34.1% of the sample, participants were likely (probability > .500) to score in the symptomatic range on all nine domains of the SCL-90-R. Participants in this class had probabilities ranging from .728 for paranoid ideation to .995 for depression. The second latent class, which described 37.1% of the participants, had probabilities greater than .500 of scoring in the symptomatic range for all symptoms except hostility (probability = .286) and paranoid ideation (probability = .273). The probability that people in this class were symptomatic on anxiety was 0.499, which means they had almost even odds of being symptomatic or asymptomatic on anxiety. The third latent class, which described 28.8% of participants, had a low probability (less than .500) of scoring as symptomatic on any domain.
Table 3.
Probability for Each Psychological Symptom Latent Class of Scoring In the Symptomatic Range on Domains of the SC-90-R
| SCL-90-R domain |
All symptoms class 34.1% of sample |
Internalizing symptoms class 37.1% of sample |
Asymptomatic class 28.8% of sample |
|---|---|---|---|
| Somatization | .947 | .530 | .082 |
| Obsessive Compulsive Disorder | .992 | .668 | .074 |
| Interpersonal Sensitivity | .993 | .532 | .075 |
| Depression | .995 | .829 | .013 |
| Anxiety | .970 | .499 | .021 |
| Hostility | .775 | .286 | .004 |
| Phobic Anxiety | .896 | .625 | .095 |
| Paranoid Ideation | .728 | .273 | .003 |
| Psychoticism | .985 | .759 | .140 |
We will refer to the three classes as the all symptoms class, the internalizing symptoms class, and the asymptomatic class, respectively. The labels all symptoms and asymptomatic labels are self-explanatory. We refer to the group that is symptomatic on all domains except hostility and paranoid ideation (and had nearly even odds of being anxious), as the internalizing class because what distinguishes members of this class from the all symptoms class is that they were not symptomatic on other-directed symptoms (hostility and paranoid ideation). This term is consistent with research on the underlying structure of adult and child psychopathology which suggests that disorders cluster into those that involve internalizing psychological distress and those that involve externalizing distress (for a review, see Achenbach & Edelbrock, 1978; Krueger & Markon, 2006).
Relationships of demographic variables and latent classes with sexual behavior
Demographic characteristics were included as independent variables in the first step of the multinomial logistic regression analyses. Results showed that with other demographic variables controlled, age (Wald χ2(2) =7.24, p = 0.027), sexual orientation (Wald χ2(2) =11.47, p = 0.003), and having a current spouse/partner (Wald χ2(2) = 20.09, p < 0.001) were all significantly related to sexual risk category. Although race/ethnicity was not significantly related to sexual behavior (χ2 (2) = 2.59, p = 0.274), it was retained in the model to control for small differences between men of color and white men in the final model.
In the second step of the analyses, psychological symptom latent class was added to the model that included the demographic variables from the first step. Results showed that after controlling for the effects of demographic variables, psychological symptom latent class was related to sexual behavior (Wald χ2 (4) = 11.50, p = 0.022).
Table 4 presents the odds ratios, confidence intervals for the odds ratios, and p values for all variables in the final model for three comparisons: (1) inconsistent condom use versus abstinence, (2) consistent condom use versus abstinence, and (3) consistent versus inconsistent condom use. We refer to these comparisons as Comparisons 1, 2, and 3.
Table 4.
Associations of Demographic Variables and Psychological Latent Class with Sexual Risk Group
| Comparison 1 Inconsistent Condom Use versus Abstinent |
Comparison 2 Consistent Condom Use versus Abstinent |
Comparison 3 Consistent Condom Use versus Inconsistent Condom Use |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beta (SE) |
OR | 95% CI |
p | Beta (SE) |
OR | 95% CI |
p | Beta (SE) |
OR | 95% CI |
p | |
| Age | −0.522 (0.289) |
0.594 | 0.34, 1.05 |
0.07 | −0.934 (0.356) |
0.393 | 0.196, 0.789 |
0.01 | −0.413 (0.365) |
0.662 | 0.32, 1.36 |
0.26 |
| Men of Color vs. White Men |
0.000 (0.647) |
1.000 | 0.28, 3.55 |
1.00 | 1.32 (0.649) |
3.776 | 1.057, 13.484 |
0.04 | 1.329 (0.699) |
3.776 | 0.96, 14.87 |
0.06 |
| Heterosexuals vs. Homosexual/Bisexual |
−1.648 (0.317) |
0.192 | 0.06, 0.67 |
0.01 | 0.532 (0.594) |
1.702 | 0.531, 5.451 |
0.37 | 1.090 (0.351) |
8.846 | 2.23, 35.06 |
<0.01 |
| No current partner vs. Having a current pouse/partner |
1.918 (0.451) |
6.809 | 2.82, 16.47 |
<0.01 | 1.435 (0.586) |
4.201 | 1.333, 13.242 |
0.01 | −0.483 (0.636) |
.617 | 0.18, 2.15 |
0.45 |
|
Internalizing vs. All Symptoms |
−0.301 (0.526) |
0.740 | 0.27, 2.06 |
0.57 | 0.903 (0.782) |
2.466 | 0.533, 11.413 |
0.25 | 1.204 (0.794) |
3.332 | 0.70, 15.80 |
0.13 |
|
Asymptomatic vs. All Symptoms |
−0.560 (0.589) |
0.571 | 0.18, 1.81 |
0.34 | 2.001 (0.753) |
7.393 | 1.692, 32.311 |
<0.01 | 2.560 (0.788) |
12.941 | 2.76, 60.73 |
<0.01 |
|
Asymptomatic vs. Internalizing |
−0.259 (0.558) |
0.772 | 0.26, 2.31 |
0.64 | 1.098 (0.654) |
2.998 | 0.833, 10.796 |
0.09 | 1.357 (0.696) |
3.884 | 0.99, 15.19 |
0.05 |
Results for demographic variables showed that for age, Comparison 2 produced a significant odds ratio, indicating that with every 10-year increase in age, the odds of being a consistent condom user decrease relative to the odds of being abstinent. Age did not affect the odds of being an inconsistent condom user versus being abstinent (Comparison 1), or the odds of being a consistent versus inconsistent condom user (Comparison 3). Heterosexuals (vs. homosexuals/bisexuals) had significantly lower odds of being inconsistent condom users relative to the odds of being abstinent (Comparison 1), and had greater odds of being consistent condom users relative to the odds of being inconsistent condom users (Comparison 3). Men who had a spouse or partner were more likely to use condoms inconsistently or to use condoms consistently relative to being abstinent (Comparisons 1 and 2), but partnership status did not differentiate between the inconsistent and the consistent condom users (Comparison 3).
The fifth and sixth rows of Table 4 summarize results for the relationship of latent symptom class to sexual risk behavior. In these comparisons, the all symptoms latent class is the referent group for comparison with other classes. Thus, the row labeled “internalizing vs. all symptoms” shows results for predicting each of the three sexual behavior/condom use comparisons for the internalizing class versus the all symptoms class. Similarly, the row labeled “asymptomatic vs. all symptoms” summarizes results for predicting each of the three comparisons for sexual behavior/condom use for the asymptomatic class versus the all symptoms class.
As Table 4 shows, the internalizing symptom latent class and the all symptom classes did not differ significantly for any of the sexual behavior comparisons. Members of these two groups did not differ in whether they were consistent condom users versus abstinent (Comparison 1), inconsistent condom users versus abstinent (Comparison 2), or inconsistent versus consistent condom users (Comparison 3). In contrast, the asymptomatic latent class was significantly more likely than the all symptoms latent class to be consistent rather than inconsistent condom users (Comparison 3), and to be consistent condom users rather than abstinent (Comparison 2). Members of these two latent classes did not differ in whether they were inconsistent condom users versus abstinent (Comparison 1).
One comparison not addressed by the above analysis was between the internalizing symptoms class and the asymptomatic class. In order to make this comparison, we conducted an additional analysis using the asymptomatic class as the referent group. The last row of Table 4 shows that men in the asymptomatic class were more likely than those in the internalizing class to be consistent condom users than to be inconsistent condom users, and were marginally more likely to be consistent condom users than to be abstinent.
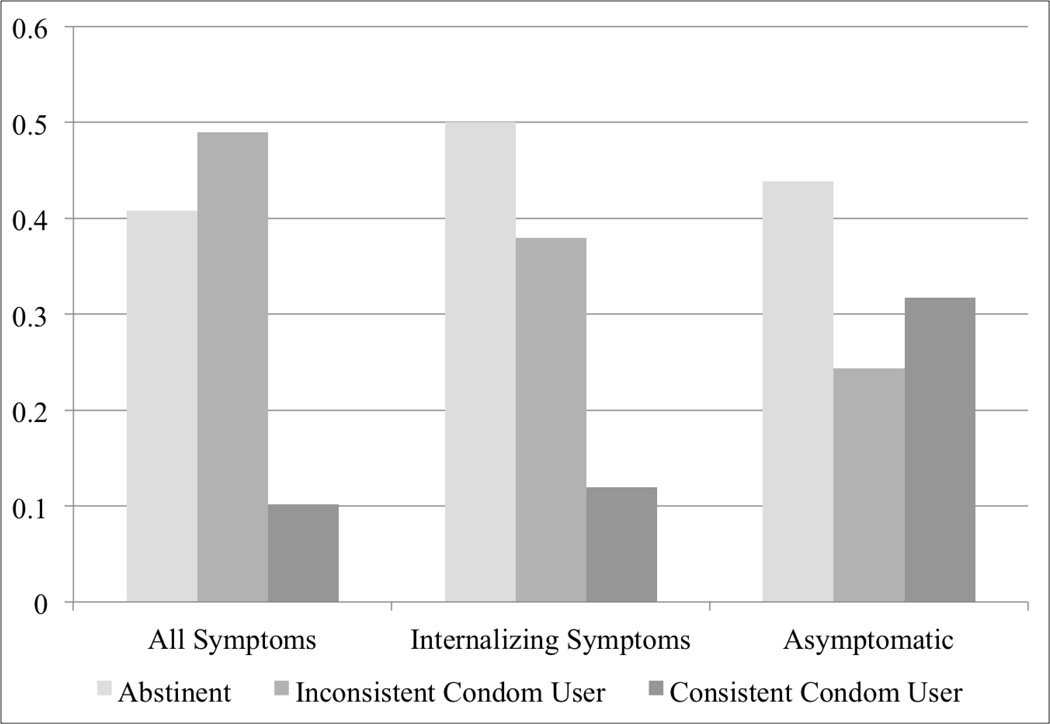
Because it is difficult to visualize the pattern of differences between the symptom latent classes from the odds ratios alone, Figure 1 shows the percentages of men in each symptom latent class who were abstinent, consistent condom users, or inconsistent condom users. Although the Wald χ2 described above and the odds ratios and significance tests shown in Table 4 provide the formal test of whether the symptom latent classes differ in sexual behavior, a chi square test of the percentages shown in Figure 1 confirms that there is an association between symptom latent class and sexual behavior (χ2(4) = 11.266, p = .024). Figure 1 graphically illustrates the findings summarized in Table 4, which indicated that the pattern of sexual behavior in the all symptoms latent class does not differ from the pattern displayed by the internalizing symptom class. Figure 1 also shows that abstinence and inconsistent condom use predominated in the all symptoms and the internalizing symptoms groups, with consistent condom use being relatively uncommon. Figure 1 also illustrates the differences between men in the asymptomatic class relative to the other men. Asymptomatic men were more likely to be consistent than to be inconsistent condom users than men in the internalizing symptoms or all symptoms classes. They also were relatively more likely than men in the all symptoms class to be consistent condom users than to be abstinent, and marginally more likely than men in the internalizing symptoms class to be consistent condom users than to be abstinent. Note that this does not mean that most men in the asymptomatic class were sexually active, but it does mean that safer sex was more likely among these men compared to other men.
Figure 1.
Proportions of participants in each symptom class who were abstinent, inconsistent condom users, and consistent condom users.
Discussion
This study adds to nascent work suggesting that psychological symptoms play a role in risky sexual behavior, but that they do not increase risk in a simple fashion. For the first time of which we are aware, this study examined the possibility that constellations of psychological symptoms may push people to either abstinence or to risky sex, but people who share these constellations are relatively unlikely to engage in safer sex.
An advantage of the LCA approach used in this study is that it allowed us to simultaneously examine a constellation of symptoms as they relate to sexual risk behavior. Examining single symptoms in isolation without considering other symptoms that the individual is likely to have risks missing the overall symptom context in which the effects of a particular symptom play out. Thus, LCA can help clarify the symptom-sexual behavior link.
There are other approaches that can be used to examine the complexity of how symptoms might operate together to affect sexual behavior. For example, Senn, Carey, & Vanable (2010), pointed out that a strict interpretation of syndemic theory requires examining the interactions between variables, not just counting up their additive effects. These researchers examined the interactive effects of five psychosocial health conditions, including depression. A disadvantage of their approach is that five independent variables could potentially produce ten 2-way interactions, as well as several 3-way and 4-way interactions, and one 5-way interaction. The authors examined only the 2-way interactions, of which only two were significant, neither of which involved depression. An advantage of LCA is that it can capture some of the complexity of how different conditions or symptoms work together to shape sexual behavior without plunging the hapless researcher into the morass of deciphering numerous higher order statistical interactions (Halford, Baker, McCredden, & Bain, 2005).
LCA is useful when symptoms or other predictors are categorized according to some meaningful threshold. Clinical practitioners often use diagnostic criteria in which it is important to ascertain whether an individual is above a threshold for symptom severity. Several measures commonly used to examine the relationship of psychological symptoms to sexual behavior are normed or have standard cut-offs that indicate clinically relevant elevations in symptoms. For example, the Center for Epidemiologic Studies Depression Scale (Radloff, 1977) and the Beck Depression Inventory (A. Beck, Steer, & Brown, 1996) have cutoffs that indicate clinically significant levels of distress.
A limitation of LCA is that it sacrifices the ability to capture fine-grained gradations of individual symptoms conceptualized as continuous variables. It also leaves open the possibility that one particular symptom may be driving an effect – which of course would be obscured when participants in the same latent class are symptomatic on other symptoms as well. However, in a review of the correlates of risky sexual behavior, Crepaz & Marks (2002) called for research that takes a multivariate approach to understanding risk. LCA is not the only approach that can do this, but it does allow researchers to consider how clusters of naturally co-occurring symptoms are related to sexual risk. Developing ways to conceptualize and capture the multiplicity of symptoms people experience is essential to understanding how psychological symptoms are related to sexual risk behavior.
This is especially important in risk behavior of people with HIV because poor mental health is implicated in the acquisition of HIV (Prince et al., 2007), and once acquired, HIV exerts its own toll on mental health. Thus, it is not surprising that our participants generally showed high levels of distress. Most participants (82.1%) scored above the clinically significant cutoffs in at least one domain. Poor mental health not only can cause a great deal of distress, but it also can affect the trajectory of the physical disease (Schuster, Bornovalova, & Hunt, 2012).
This study also shines much needed attention on abstinent individuals. HIV prevention efforts encourage people to be abstinent, which is considered to be the safest behavior in terms of avoiding transmission of HIV. Much of the research and discussion of abstinence centers around whether abstinence-only approaches are effective in reducing HIV transmission risk (Barnett & Parkhurst, 2005). The psychological well-being of people who are abstinent receives little attention. As noted above, it is important to consider the psychological health of people with HIV who are abstinent for their own sake, but since psychological symptoms are associated with abstinence in much the same way as they are associated with risky sex, understanding abstinence has implications for understanding risky sex as well. Consequently, abstinent people warrant attention because they may not stay sexually inactive. If psychological symptoms lead people to both unsafe sex and abstinence, abstinent people with clusters of psychological symptoms who become sexually active may be relatively unlikely to engage in protected sex.
A key unanswered question is what determines whether the psychologically distressed person with HIV is sexually active, but risky, or abstains from sex. One variable that determines which outcome occurs is partner availability. Abstinence is not always a choice, and so if the opportunity arises, psychologically troubled individuals may have sex but not take the steps necessary to have safer sex. We assessed whether our participants were currently in a relationship, and those who were in a relationship were more likely to have sex than those who were not in a relationship. However, even after controlling for current relationship status, we still found that participants with symptoms in all domains or in internalizing domains had increased odds of having unprotected sex compared to asymptomatic participants, and they also had significantly increased odds (all symptoms class) or tended to have increased odds (internalizing class) of being abstinent.
Another important trigger for abstinence versus risky sex may be disease stage. In a review of HIV disease stage and HIV risk-related behavior, Eaton and Kalichman (2009) concluded that there is a typical trajectory of risky sexual behavior among people with HIV. Immediately prior to diagnosis, most people have been engaging in high levels of risky behavior. In the months after diagnosis, there is typically a sharp reduction in risky behavior, although some people continue to be risky. As the years go on, many, but not all, people revert to risk, particularly during times when their HIV is asymptomatic. Eaton and Kalichman (2009) noted that more research is needed to understand why some people rebound from less risk to more risk following the initial months after HIV diagnosis and as the physical manifestations of the disease change.
Our findings suggest that mental health may shape whether people rebound back to risky behavior after initially reducing risk following a diagnosis of HIV. In the immediate aftermath of learning that one has HIV, the balance may tip to abstinence. A diagnosis of HIV may strain existing sexual relationships and impede establishing new ones, and individuals may become overwhelmed with dealing with a host of problems with which they have little prior experience. Having lived with the diagnosis for a period of time, individuals might better manage some of these issues, and sexual behavior resumes. However, psychological symptoms that are untreated or do not improve on their own may interfere with the ability to implement safer sex practices, and the individuals subsequently revert to risky sex. One implication of this reasoning is that the mental health needs of people newly diagnosed with HIV require special attention. In the present study, years since diagnosis were not associated with risky sexual behavior or abstinence. However, participants in our study on average had been living with an HIV diagnosis for over a decade, so whatever rebound in risky behavior that might be expected to occur had probably already happened.
Eaton and Kalichman’s (2009) review of research also indicated that high-risk behavior tends to decline as CD4 counts decline and/or viral load increases. They speculated that declines in risky behavior that are associated with increased viral load and decreased CD4 counts may occur because of the psychological impact of a worsening immune system. Our results suggest that examining psychological symptom clusters may be a fruitful way to understand how declines in physical health are related to sexual behavior.
There are other dynamics that may influence whether people are abstinent or engage in risky sex. For example, a study by Varni, Miller, & Solomon (2012) found that the odds of people with HIV being abstinent versus sexually risky were related to the amount of perceived HIV discrimination they experienced. Among those who coped with HIV discrimination using high levels of disengagement (avoidance) coping, increasing levels of HIV discrimination were associated with increased odds of being abstinent versus being sexually risky. In other words, abstinence was less likely (and risky sex more likely) among those who perceived low levels of HIV discrimination. Varni et al. speculated that for people who use avoidance to cope with discrimination, high levels of perceived stigma increases reluctance to begin even the initial steps required to enter into or maintain a sexual relationship. Those with lower levels of perceived stigma may be able to take those steps, but the tendency to avoid thinking about or dealing with HIV discrimination makes it difficult for them to take the steps needed to use condoms consistently (e.g., communication with partners, acquiring condoms).
Researchers who have found non-linear associations between depression and risky sex have proposed similar explanations. For example, in explaining the inverted-U relationship they found between depression and unprotected oral and anal sex, Shiu et al. (2014) noted that people with low levels of depression have the emotional and cognitive resources to seek sexual partners and use condoms effectively. Those with high levels of depression experience symptoms, such as decreased sexual desire, that may discourage them from engaging in sexual behavior at all. Because being “safe” in the Shiu et al. study meant that the individual had not engaged in unprotected oral or anal sex, the notion that high levels of depression reduced risk via abstinence could not be evaluated.
Our conceptual analysis assumes that psychological symptoms put people at risk for having unprotected sex or increase the chances of being abstinent. Results were consistent with this view, but it also is possible that psychological symptoms are outcomes of sexual behavior rather than being behavioral instigators. For example, abstinent people may develop psychological symptoms because they are socially isolated (Frost, Parsons, & Nanín, 2007; Meade & Sikkema, 2007; Overstreet, Earnshaw, Kalichman, & Quinn, 2013). However, it is less clear why using condoms inconsistently would lead to the same set of psychological symptoms that abstinence does. Nonetheless, these data are cross-sectional, and therefore our findings leave open the question of whether psychological symptoms increase the odds of risky sexual behavior and abstinence or whether those who engage in these behaviors are at risk for psychological distress.
In thinking about the implications of these findings, we must also be mindful that although the same symptom clusters were associated with abstinence as those that were associated with risky sex, there were two different symptom clusters that predicted these behaviors. In other words, among both abstinent and sexually risky participants, some participants were generally distressed (i.e., the all symptoms group) and some were distressed in particular ways (i.e., the internalizing symptoms group). Some prior research suggests that outer-directed negative emotions of anger (Crepaz & Marks, 2002) and blaming others for HIV infection (Bingman, Marks, & Crepaz, 2001) are associated with unsafe sex. People who feel hostility towards others may care less about what happens to them, and have reduced motivation to protect them from HIV infection. The chief difference between the all symptoms and internalizing symptoms latent classes was in whether members of those classes were symptomatic on hostility and paranoid ideation. This difference suggests that the all symptoms class should be more closely associated with unprotected sex than with abstinence, and that the internalizing symptoms class should be more closely associated with abstinence than with risky sex. This was not the case in the present study, but the possible role of hostility and blaming others in tipping the balance between abstinence and risky sex warrants additional attention.
One limitation of this study is that the sample was relatively homogeneous with respect to race/ethnicity. Although many assume that disproportionate rates of HIV infection among men of color result from high risk sexual behavior, there is evidence that at least some men of color, specifically African American MSM, are not more risky than other men are (Millett, Flores, Peterson, & Bakeman, 2007; Millett, Peterson, Wolitski, & Stall, 2006). Our participants included too few men of color to make comparisons between different minority groups. It also is worth noting that although the individual comparisons shown in Table 4 suggest that men of color were more likely than White men to be consistent condom users rather than abstinent, the overall Wald χ2 indicated that race/ethnicity was not a signifcant predictor of sexual behavior, and thus this finding should not be overinterpreted.
Study participants also were mainly from rural areas of New England. The latent symptom classes that emerged from this study may differ from the constellations of symptoms that people in urban areas, other regions, or other cultures may experience. Sexual behavior and condom use were assessed by self-report, and although care was taken to ask about a time period that people can reasonably recall, and to use questions that defined the behaviors in lay terms, it is possible that people were unwilling or unable to accurately report their behavior and/or misunderstood what we were asking about.
Finally, HIV prevention/intervention efforts that focus mainly on reducing HIV risk behaviors have inconsistent effects, and behavior change over the long term is difficult to achieve (Safren, Reisner, Herrick, Mimiaga, & Stall, 2010). Research indicates that men with HIV expressed in an interest in health promotion interventions, but they did not always express enthusiasm for programs that focused exclusively on promoting safer sex (Vanable et al., 2012). Understanding the role that psychological symptoms play with regard to risky sexual behavior and abstinence is important in designing effective interventions (Abdala et al., 2013; Crosby et al., 2013; Lorimer et al., 2013; Vanable et al., 2012). Shiu et al (2014) suggested that identifying depression levels of MSM might be necessary to tailor preventative services to meet their unique needs. Our results suggest that it is important to move beyond a focus on specific symptoms to obtain a more comprehensive assessment of the array of co-morbid symptoms individuals may be experiencing.
There have been several calls for the next generation of prevention/intervention initiatives for men with HIV to include components that are designed not only to reduce risky sex, but also to address psychological symptoms and support behaviors to effectively cope with HIV discrimination (Cook, Purdie-Vaughns, Meyer, & Busch, 2014; Frost, Parsons, & Nanín, 2007; Safren, Blashill, & O'Cleirigh, 2011). Safren et al. noted that most models of HIV risk behavior focus on judgments and appraisals (e.g., perception of norms, evaluation of risk) that can be affected by the individual’s mental health. Thus, lack of attention to mental health issues can hamper prevention and intervention efforts to reduce risky sexual behavior. A novel insight emerging from the results of this study that men with HIV who are abstinent may benefit from these efforts just as much as those who already are engaging in at risk behavior. A pro-active strategy to promote psychological well-being may lay the foundation and build a pathway towards safer sexual behaviors should men who report sexual abstinence engage in sexual activity in the future.
References
- Abdala N, Zhan W, Shaboltas AV, Skochilov RV, Kozlov AP, Krasnoselskikh TV. Efficacy of a brief HIV prevention counseling intervention among STI clinic patients in Russia: A randomized controlled trial. AIDS and Behavior. 2013;17:1016–1024. doi: 10.1007/s10461-012-0311-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achenbach TM, Edelbrock CS. The classification of child psychopathology: A review and analysis of empirical efforts. Psychological Bulletin. 1978;85:1275–1301. [PubMed] [Google Scholar]
- Althoff RR, Rettew DC, Boomsma DI, Hudziak JJ. Latent class analysis of the Child Behavior Checklist Obsessive-Compulsive Scale. Comprehensive Psychiatry. 2009;50:584–592. doi: 10.1016/j.comppsych.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. DSM-IV-TR: Diagnostic and statistical manual of mental disorders, text revision. American Psychiatric Association; 2000. [Google Scholar]
- Barnett T, Parkhurst J. HIV/AIDS: Sex, abstinence, and behaviour change. The Lancet Infectious Diseases. 2005;5:590–593. doi: 10.1016/S1473-3099(05)70219-X. [DOI] [PubMed] [Google Scholar]
- Beck A, Steer R, Brown G. Beck Depression Inventory–Second Edition: Manual. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. Penguin; 1979. [Google Scholar]
- Beck JS. Cognitive behavior therapy: Basics and beyond. Guilford Press; 2011. [Google Scholar]
- Bergman LR, Magnusson D, El-Khouri BM. Studying individual development in an interindividual context: A person-oriented approach. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2003. [Google Scholar]
- Bingman CR, Marks G, Crepaz N. Attributions about one's HIV infection and unsafe sex in seropositive men who have sex with men. AIDS and Behavior. 2001;5:283–289. [Google Scholar]
- Bogart LM, Collins RL, Kanouse DE, Cunningham W, Beckman R, Golinelli D, Bird CE. Patterns and correlates of deliberate abstinence among men and women with HIV/AIDS. American Journal of Public Health. 2006;96:1078–1084. doi: 10.2105/AJPH.2005.070771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LK, Tolou-Shams M, Lescano C, Houck C, Zeidman J, Pugatch D, Lourie KJ. Depressive symptoms as a predictor of sexual risk among African American adolescents and young adults. Journal of Adolescent health. 2006;39:444.e441–444.e448. doi: 10.1016/j.jadohealth.2006.01.015. [DOI] [PubMed] [Google Scholar]
- Celentano DD, Muñoz A, Cohn S, Vlahov D. Dynamics of behavioral risk factors for HIV/AIDS: a 6-year prospective study of injection drug users. Drug and Alcohol Dependence. 2001;61:315–322. doi: 10.1016/s0376-8716(00)00154-x. [DOI] [PubMed] [Google Scholar]
- Collins LM, Lanza ST. Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. Vol. 718. John Wiley & Sons; 2010. [Google Scholar]
- Comulada WS, Rotheram-Borus MJ, Pequegnat W, Weiss RE, Desmond KA, Arnold EM, Chesney MA. Relationships over time between mental health symptoms and transmission risk among persons living with HIV. Psychology of Addictive Behaviors. 2010;24:109–118. doi: 10.1037/a0018190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crepaz N, Marks G. Are negative affective states associated with HIV sexual risk behaviors? A meta-analytic review. Health Psychology. 2001;20:291–299. doi: 10.1037//0278-6133.20.4.291. [DOI] [PubMed] [Google Scholar]
- Crepaz N, Marks G. Towards an understanding of sexual risk behavior in people living with HIV: A review of social, psychological, and medical findings. AIDS. 2002;16:135–149. doi: 10.1097/00002030-200201250-00002. [DOI] [PubMed] [Google Scholar]
- Cook JE, Purdie-Vaughns V, Meyer IH, Busch JTA. Intervening within and across levels: A multilevel approach to stigma and public health. Social Science & Medicine. 2014;103:101–109. doi: 10.1016/j.socscimed.2013.09.023. [DOI] [PubMed] [Google Scholar]
- Crosby RA, DiClemente RJ, Salazar LF, Wingood GM, McDermott-Sales J, Young AM, Rose E. Predictors of consistent condom use among young African American women. AIDS and Behavior. 2013;17:865–871. doi: 10.1007/s10461-011-9998-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR. SCL-90-R Administration, Scoring, and Procedures Manual. Third ed. Minneapolis, MN: NCS Pearson; 1994. [Google Scholar]
- Donnelly D, Burgess E, Anderson S, Davis R, Dillard J. Involuntary Celibacy: A Life Course Analysis. The Journal of Sex Research. 2001;38:159–169. [Google Scholar]
- Eaton LA, Kalichman SC. Changes in transmission risk behaviors across stages of HIV disease among people living with HIV. JANAC: Journal of the Association of Nurses in AIDS Care. 2009;20:39–49. doi: 10.1016/j.jana.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ethier KA, Kershaw TS, Lewis JB, Milan S, Niccolai LM, Ickovics JR. Self-esteem, emotional distress and sexual behavior among adolescent females: Inter-relationships and temporal effects. Journal of Adolescent Health. 2006;38:268–274. doi: 10.1016/j.jadohealth.2004.12.010. [DOI] [PubMed] [Google Scholar]
- Fenton KA, Johnson AM, McManus S, Erens B. Measuring sexual behaviour: Methodological challenges in survey research. Sexually Transmitted Infections. 2001;77:84–92. doi: 10.1136/sti.77.2.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbein M, Coutinho Re. Demographic and behavioral predictors of sexual risk in the NIMH Multisite HIV Prevention Trial. AIDS. 1997;11:S21–S27. [PubMed] [Google Scholar]
- Frost DM, Parsons JT, Nanín JE. Stigma, concealment and symptoms of depression as explanations for sexually transmitted infections among gay men. Journal of Health Psychology. 2007;12:636–640. doi: 10.1177/1359105307078170. [DOI] [PubMed] [Google Scholar]
- Golub S, Botsko M, Gamarel K, Parsons J, Brennan M, Karpiak S. Dimensions of psychological well-being predict consistent condom use among older adults living with HIV. Ageing International. 2013;38:179–194. [Google Scholar]
- Halford GS, Baker R, McCredden JE, Bain JD. How many variables can humans process? Psychological Science. 2005;16:70–76. doi: 10.1111/j.0956-7976.2005.00782.x. [DOI] [PubMed] [Google Scholar]
- Hart TA, Heimberg RG. Social anxiety as a risk factor for unprotected intercourse among gay and bisexual male youth. AIDS and Behavior. 2005;9:505–512. doi: 10.1007/s10461-005-9021-2. [DOI] [PubMed] [Google Scholar]
- Jarvis B. MediaLab (Version 2004.3.24) New York, NY: Empirisoft Corporation; 2004. [Google Scholar]
- Klein H. Using a syndemics theory approach to study HIV risk taking in a population of men who use the internet to find partners for unprotected sex. American Journal of Mens Health. 2011;5:466–476. doi: 10.1177/1557988311398472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, Buchbinder S. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20:731–739. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Dziak JJ, Huang L, Xu S, Collins LM. PROC LCA & PROC LTA user’s guide (version 1.2. 7) University Park, PA: Methodology Center, Penn State University; 2011. [Google Scholar]
- Lorimer K, Kidd L, Lawrence M, McPherson K, Cayless S, Cornish F. Systematic review of reviews of behavioural HIV prevention interventions among men who have sex with men. AIDS Care. 2013;25:133–150. doi: 10.1080/09540121.2012.699672. [DOI] [PubMed] [Google Scholar]
- Mayer K, O'Cleirigh C, Skeer M, Covahey C, Leidolf E, Vanderwarker R, Safren SA. Which HIV-infected men who have sex with men in care are engaging in risky sex and acquiring sexually transmitted infections: findings from a Boston community health centre. Sexually Transmitted Infections. 2010;86:66–70. doi: 10.1136/sti.2009.036608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade CS, Sikkema KJ. Psychiatric and Psychosocial Correlates of Sexual Risk Behavior among Adults with Severe Mental Illness. Community Mental Health Journal. 2007;43:153–169. doi: 10.1007/s10597-006-9071-6. [DOI] [PubMed] [Google Scholar]
- Miller CT, Grover KW, Bunn JY, Solomon SE. Community norms about suppression of AIDS-related prejudice and perceptions of stigma by people with HIV or AIDS. Psychological Science. 2011;22(5):579–583. doi: 10.1177/0956797611404898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller CT, Bunn JY, Grover KW, Solomon SE. Perceptions of behavioral norms related to HIV transmission by people with HIV and by residents of their communities. Social Influence. 2014;9:1–19. doi: 10.1080/15534510.2012.712548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: A meta-analysis of HIV risk behaviors. AIDS. 2007;21:2083–2091. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: A critical literature review. Journal Information. 2006;96 doi: 10.2105/AJPH.2005.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: Preliminary evidence of a syndemic in need of attention. Annals of Behavioral Medicine. 2007;34:37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers J, Shade S, Rose C, Koester K, Maiorana A, Malitz F, Morin S. Interventions delivered in clinical settings are effective in reducing risk of HIV transmission among people living with HIV: Results from the Health Resources and Services Administration (HRSA)’s Special Projects of National Significance Initiative. AIDS and Behavior. 2010;14:483–492. doi: 10.1007/s10461-010-9679-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Cleirigh C, Newcomb ME, Mayer KH, Skeer M, Traeger L, Safren SA. Moderate levels of depression predict sexual transmission risk in HIV-infected MSM: A longitudinal analysis of data from six sites involved in a “prevention for positives” study. AIDS and Behavior. 2013;17:1764–1769. doi: 10.1007/s10461-013-0462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overstreet NM, Earnshaw VA, Kalichman SC, Quinn DM. Internalized stigma and HIV status disclosure among HIV-positive Black men who have sex with men. AIDS Care. 2013;25:466–471. doi: 10.1080/09540121.2012.720362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: further evidence of a syndemic. American Journal of Public Health. 2012;102:156–162. doi: 10.2105/AJPH.2011.300284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pines HA, Gorbach PM, Weiss RE, Shoptaw S, Landovitz RJ, Javanbakht M, Plankey M. Sexual risk trajectories among MSM in the United States: Implications for pre-exposure prophylaxis delivery. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2014;65:579–586. doi: 10.1097/QAI.0000000000000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, Rahman A. No health without mental health. The Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reisner SL, Mimiaga MJ, Skeer M, Bright D, Cranston K, Isenberg D, Mayer KH. Clinically significant depressive symptoms as a risk factor for HIV infection among black MSM in Massachusetts. AIDS and Behavior. 2009;13:798–810. doi: 10.1007/s10461-009-9571-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutledge SE, Siebert DC, Siebert C, Chonody J. Attitudes Toward Gays and Lesbians: A Latent Class Analysis of University Students. [Article] Journal of Social Service Research. 2012;38:18–28. [Google Scholar]
- Safren SA, Blashill AJ, O'Cleirigh CM. Promoting the Sexual Health of MSM in the Context of Comorbid Mental Health Problems. Aids and Behavior. 2011;15:S30–S34. doi: 10.1007/s10461-011-9898-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, Reisner SL, Herrick A, Mimiaga MJ, Stall R. Mental health and HIV risk in men who have sex with men. Journal of Acquired Immune Deficiency Syndromes. 2010;55:S74. doi: 10.1097/QAI.0b013e3181fbc939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS (Version 9.2) 2011. [Google Scholar]
- Schroder KE, Johnson CJ, Wiebe JS. An event-level analysis of condom use as a function of mood, alcohol use, and safer sex negotiations. Archives of Sexual Behavior. 2009;38:283–289. doi: 10.1007/s10508-007-9278-9. [DOI] [PubMed] [Google Scholar]
- Schuster R, Bornovalova M, Hunt E. The influence of depression on the progression of HIV: Direct and indirect effects. Behavior Modification. 2012;36:123–145. doi: 10.1177/0145445511425231. [DOI] [PubMed] [Google Scholar]
- Senn TE, Carey MP, Vanable PA. The intersection of violence, substance use, depression, and STDs: Testing of a syndemic pattern among patients attending an urban STD clinic. Journal of the National Medical Association. 2010;102:614. doi: 10.1016/s0027-9684(15)30639-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seth P, Patel SN, Sales JM, DiClemente RJ, Wingood GM, Rose ES. The impact of depressive symptomatology on risky sexual behavior and sexual communication among African American female adolescents. Psychology Health & Medicine. 2011;16:346–356. doi: 10.1080/13548506.2011.554562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiu C-S, Chen Y-C, Tseng P-C, Chung A-C, Wu M-T, Hsu S-T, Ko N-Y. Curvilinear relationship between depression and unprotected sexual behaviors among men who have sex with men: Depression and unprotected sexual behaviors. The Journal of Sexual Medicine. 2014 doi: 10.1111/jsm.12638. n/a–n/a. [DOI] [PubMed] [Google Scholar]
- Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, Catania JA. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health. 2003;93:939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Mimiaga MJ, Dilley JW, Hammer GP, Karasic DH, Charlebois ED, Bangsberg DR. Does effective depression treatment alone reduce secondary HIV transmission risk? Equivocal findings from a randomized controlled trial. AIDS and Behavior. 2013;17:2765–2772. doi: 10.1007/s10461-013-0600-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanable PA, Carey MP, Brown JL, Littlewood RA, Bostwick R, Blair D. What HIV-positive MSM want from sexual risk reduction interventions: Findings from a qualitative study. AIDS and Behavior. 2012;16:554–563. doi: 10.1007/s10461-011-0047-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni SE, Miller CT, McCuin T, Solomon SE. Disengagement and engagement coping with HIV/AIDS stigma and psychological well-being of people with HIV/AIDS. Journal of Social and Clinical Psychology. 2012;31:123–150. doi: 10.1521/jscp.2012.31.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni SE, Miller CT, Solomon SE. Sexual behavior as a function of stigma and coping with stigma among people with HIV/AIDS in rural New England. AIDS and Behavior. 2012;16:2330–2339. doi: 10.1007/s10461-012-0239-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner GJ, Rabkin JG, Rabkin R. Sexual activity among HIV-seropositive gay men seeking treatment for depression. Journal of Clinical Psychiatry. 1993;54:470–475. [PubMed] [Google Scholar]
- Williams CT, Latkin CA. The role of depressive symptoms in predicting sex with multiple and high-risk partners. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2005;38:69–73. doi: 10.1097/00126334-200501010-00013. [DOI] [PubMed] [Google Scholar]