Lung transplantation represents the only definitive treatment for advanced, end-stage lung disease. The severe deficiency in donor organs, however, remains the most significant barrier to providing the procedure at many large centres. In the meantime, a mounting number of individuals die while waiting for suitable donors. Given the limited success of public education and awareness campaigns, exploring options for alternative donor pools and developing new technologies have become important goals. The authors of this article describe their experi -ence with a promising donor source and supporting technology.
Keywords: Donation after circulatory death, Ex vivo lung perfusion, Lung transplantation, Portable
Abstract
BACKGROUND:
Donation after circulatory death is a novel method of increasing the number of donor lungs available for transplantation. Using organs from donors after circulatory death has the potential to increase the number of transplants performed.
METHODS:
Three bilateral lung transplants from donors after circulatory death were performed over a six-month period. Following organ retrieval, all sets of lungs were placed on a portable ex vivo lung perfusion device for evaluation and preservation.
RESULTS:
Lung function remained stable during portable ex vivo perfusion, with improvement in partial pressure of oxygen/fraction of inspired oxygen ratios. Mechanical ventilation was discontinued within 48 h for each recipient and no patient stayed in the intensive care unit longer than eight days. There was no postgraft dysfunction at 72 h in two of the three recipients. Ninety-day mortality for all recipients was 0% and all maintain excellent forced expiratory volume in 1 s and forced vital capacity values post-transplantation.
CONCLUSION:
The authors report excellent results with their initial experience using donors after circulatory death after portable ex vivo lung perfusion. It is hoped this will allow for the most efficient use of available donor lungs, leading to more transplants and fewer deaths for potential recipients on wait lists.
Abstract
HISTORIQUE :
Un don après un décès circulatoire est une nouvelle méthode pour accroître le nombre de poumons pouvant être transplantés. L’utilisation d’organes de donneurs après un décès circulatoire pourrait accroître le nombre de transplantations.
MÉTHODOLOGIE :
Trois transplantations pulmonaires bilatérales de donneurs après un décès circulatoire ont été effectuées sur une période de six mois. Après le prélèvement, tous les poumons ont été placés sur un dispositif de perfusion ex vivo portable en vue d’être évalués et préservés.
RÉSULTATS :
La fonction pulmonaire est demeurée stable pendant la perfusion ex vivo portable, tandis que la pression partielle entre le ratio d’oxygène et la fraction d’oxygène dans l’air inspiré s’est améliorée. Aucun receveur n’a été sous ventilation mécanique plus de 48 heures et n’est demeuré aux soins intensifs plus de huit jours. Deux des trois receveurs ne présentaient pas de dysfonction au bout de 72 heures. Aucun n’était décédé au bout de 90 jours, et tous ont conservé d’excellentes valeurs de volume expiratoire maximal par seconde et de capacité vitale forcée.
CONCLUSION :
Les auteurs ont rendu compte d’excellents résultats après leur expérience initiale auprès de donneurs après un décès circulatoire et une perfusion ex vivo portable. On espère que cette technique favorisera l’utilisation la plus efficace possible des poumons de donneurs, suscitera plus de transplantations et réduira les décès de receveurs potentiels sur la liste d’attente.
Lung transplantation (LTx) remains the only treatment for advanced end-stage lung disease from a variety of etiologies. A profound deficiency in donor organs remains the greatest challenge in providing LTx to patients at many large centres (1). As more patients are referred for LTx without the necessary donor lungs available, there is a growing rate of deaths on recipient wait lists (2). To increase the donor pool, solutions such as increasing awareness through public education may prove to be effective. However, technologies that maximize use of the scarce donor pool remain the best option for increasing rates of LTx, ultimately decreasing the number of deaths for recipients on wait lists.
One of the technologies that has emerged is ex vivo lung perfusion (EVLP). The technique of EVLP was originally developed as a method of assessing donor lung function from donors after circulatory death (DCD) before transplantation (3). EVLP for DCD lungs was further investigated by a Toronto (Ontario) group (4), who demonstrated that extended-criteria lungs, including DCD donors, could be assessed and treated using EVLP to achieve similar early outcomes as conventionally selected lungs when transplanted. EVLP has the potential to increase the number of organs available for LTx, leading to a rise in the number of transplants being performed (5).
Compared with neurological declaration of death, another way to increase the donor pool is using controlled DCD donors (Maastricht category III) (6,7), which includes patients with poor prognosis from nonsurvivable injuries who have treatment withdrawn, resulting in cardiac arrest.
DCD donation has the potential to dramatically change the field of solid-organ transplantation by increasing donor availability, ultimately leading to fewer deaths in patients waiting for an organ to become available (7). We describe our experience with LTx from DCD donors via normothermic EVLP on a portable device.
METHODS
Study design
From November 2013 to April 2014, three LTx using lungs from DCD donors were performed at the University of Alberta (Edmonton, Alberta). The present study involved a single-institution retrospective cohort with the intention of analyzing various parameters of the DCD lungs pre- and post-LTx, as well as evaluating the overall outcome of the transplant.
Donors and recipients
The lungs used in these cases were all donated after circulatory death. They were provided through the Human Organ Procurement and Exchange (HOPE) program. Donor arterial blood gases (ABGs) were drawn to determine partial pressure of oxygen/fraction of inspired oxygen (PF) ratios before the lungs were placed on EVLP. In addition, radiographic imaging and bronchoscopy were performed to inspect for edema, hemorrhage and possible signs of infection.
All recipients were deemed eligible for LTx due to end-stage pulmonary disease. All recipients gave informed consent and the procedure was approved by the Research Ethics Management Online. Recipient charts were evaluated for cause of end-stage pulmonary disease, length of intensive care unit stay post-transplant, PF ratios post-transplant and complications such as primary graft dysfunction.
LTx protocol
A protocol for DCD organ procurement has been established at the authors’ institution. Donors who do not meet neurological declaration of death criteria and who have a grave prognosis with no further treatment options leading to withdrawal of life-sustaining therapy (WLST) are considered for DCD donation. The decision for WLST is made by the attending intensivist and subsequently confirmed by a second intensivist with no involvement of transplant physicians. Consent is then obtained from the family to withdraw support after which they may request organ and/or tissue donation. WLST occurs by extubating the patient, ceasing inotropic support and providing comfort care. Arterial line and electrocardiographic monitoring is left in place to allow for continuous documentation of vital signs. The warm ischemic time begins when the mean arterial pressure is <55 mmHg and/or the oxygen saturation is <70% and ends at the time of aortic cannulation in the operating room. A 5 min ‘hands off’ period of pulselessness according to arterial line and electrical asystole by electrocardiography is required. The family is permitted to stay with their loved one until the end of the 5 min ‘hands off’ period, at which time the patient is declared dead. The donor is then transferred to the operating room for organ recovery.
Median sternotomy was performed, followed by standard retrieval techniques. The donor lungs were then placed on an EVLP device (Organ Care System [OCS] Lung; Transmedics Inc, USA) and perfused according to manufacturer specifications (8). The device flows at 40% of maximal cardiac output at approximately 2 L/min to 2.5 L/min and ventilates room air into the lungs. While on the device, the lungs are perfused with a cellular Perfadex (XVIVO, Sweden)/OCS solution with the addition of three units of packed red blood cells for a target hematocrit of 20%.
RESULTS
Over the span of six months, three LTx were performed using Maastricht category III (6) DCD donors. Table 1 lists the characteristics of each recipient. All recipients were diagnosed with end-stage lung disease and were deemed suitable LTx candidates.
TABLE 1.
Recipient characteristics
| Recipient | Age, years | Sex | Height, cm | Weight, kg | Diagnosis |
|---|---|---|---|---|---|
| 1 | 69 | Male | 170 | 88 | COPD |
| 2 | 29 | Female | 170 | 64 | Cystic fibrosis |
| 3 | 64 | Male | 172 | 57 | COPD |
COPD Chronic obstructive pulmonary disease
Donor characteristics are summarized in Table 2. Causes of death varied between donors; however, no donor lungs faced active pneumonia. Final PF ratios were calculated from arterial blood gases found in donor charts and can be used as a starting point to follow lung oxygenation capacity throughout the procedure. Donors 1 and 3 had PF ratios of 283 and 269, respectively. Donor 2 had a relatively higher PF ratio of 336. Additionally, donor 2 had been given tissue plasminogen activator while on EVLP as therapy for a pulmonary embolus, the cause of death for the donor. The warm ischemic time for all three sets of donor lungs was <30 min.
TABLE 2.
Donor characteristics
| Donor | Age, years | Sex | Height, cm | Weight, kg | Cause of death | Active PNA | Final PaO2/FiO2 |
|---|---|---|---|---|---|---|---|
| 1 | 60 | Male | 170 | 75 | IS | No | 283 |
| 2 | 29 | Female | 169 | 109 | PE | No | 336 |
| 3 | 55 | Male | 174 | 80 | HT | No | 269 |
FiO2 Fraction of inspired oxygen; HT Head trauma; IS Ischemic stroke; PaO2 Partial pressure of oxygen; PE Pulmonary embolism; PNA Pneumonia
Following organ procurement, lungs were connected to the portable OCS device to initiate EVLP. During this time, the device continually monitored lung function parameters including pulmonary artery pressure (PAP), pulmonary vascular resistance and the peak airway pressure. Figures 1, 2 and 3 represent the lung function parameters that were monitored for donor lung set 1, 2 and 3, respectively. All lung function parameters remained stable for the entirety of each EVLP. The variability in PAP in Figure 1 can be attributed to adjustments to the flow rate on the device. The fluctuations to the peak airway pressure in all three figures are the result of adjustments to the tidal volume and positive end-expiratory pressure made on the device. Physiological parameters, such as PAP and pulmonary vascular resistance, may be lower than in vivo as a result of the flow rate on the device being approximately 40% of maximal cardiac output. However, the trends in these parameters are important in determining function, especially when correlated with the PF ratios.
Figure 1).
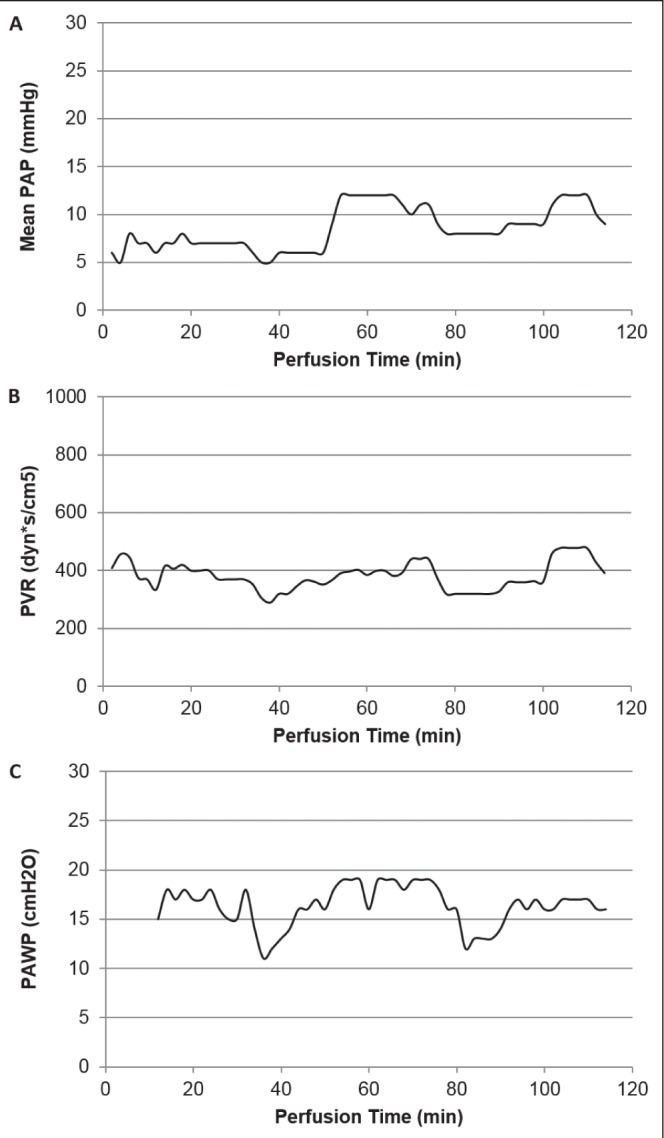
Function during ex vivo lung perfusion in donor lungs for prospective recipient 1. Continuous ex vivo monitoring of pulmonary artery pressure (PAP) (A), pulmonary vascular resistance (PVR) (B) and peak airway pressure (PAWP) (C)
Figure 2).
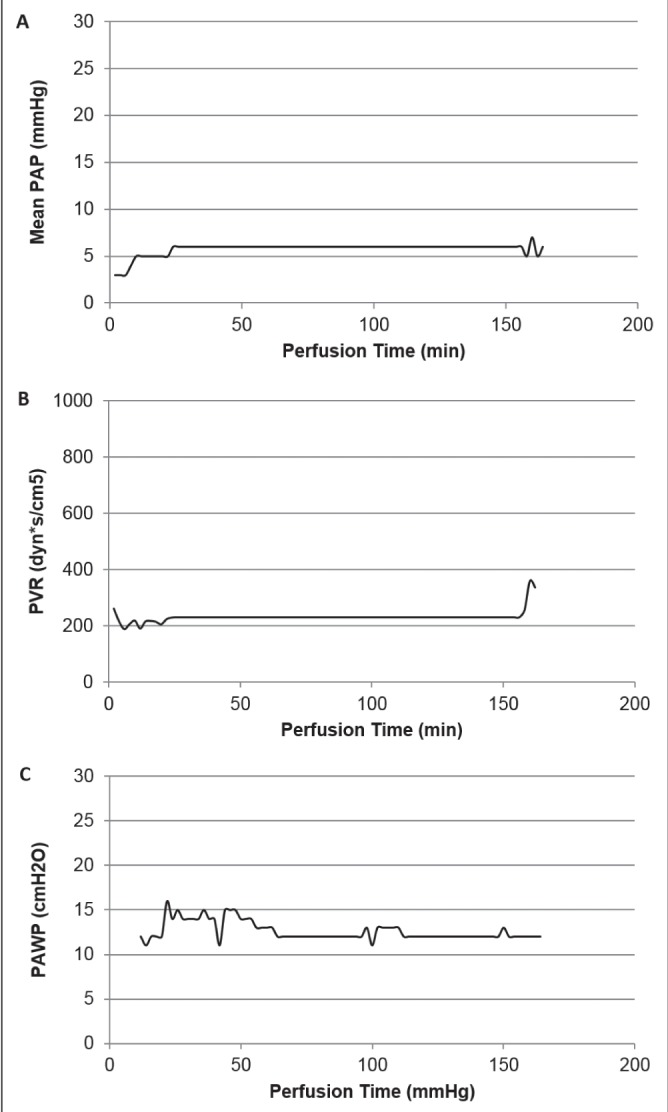
Function during ex vivo lung perfusion in donor lungs for prospective recipient 2. Continuous ex vivo monitoring of pulmonary artery pressure (PAP) (A), pulmonary vascular resistance (PVR) (B) and peak airway pressure PAWP) (C)
Figure 3).
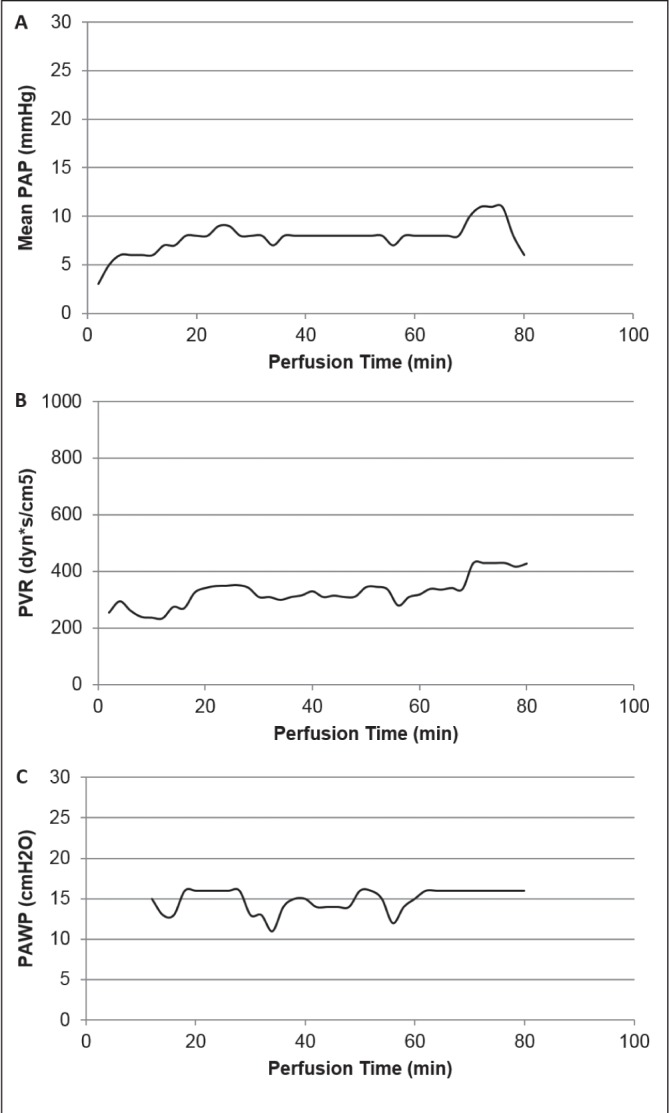
Function during ex vivo lung perfusion in donor lungs for prospective recipient 3. Continuous ex vivo monitoring of pulmonary artery pressure (PAP) (A), pulmonary vascular resistance (PVR) (B) and peak airway pressure (PAWP) (C)
ABGs were drawn from the pulmonary venous return line while the lungs were on the OCS device. Final PF ratios after EVLP are shown in Table 3, along with a comparison with the values before organ procurement. In all cases, the final PF ratio showed improvement after the period of EVLP. Mechanical circulatory support, including extracorporeal membranous oxygenation and cardiopulmonary bypass, was not required at any time in any of the cases.
TABLE 3.
Intraoperative data
| Recipient | Final donor PaO2/FiO2 ratio | Diagnosis | Warm ischemic time, min | ECMO (at any time) | Cardiopulmonary bypass | |
|---|---|---|---|---|---|---|
|
| ||||||
| Before harvest | On OCS Lung* | |||||
| 1 | 283 | 341 | Chronic obstructive pulmonary disease | 15 | No | No |
| 2 | 336 | 486 | Cystic fibrosis | 16 | No | No |
| 3 | 269 | 576 | Chronic obstructive pulmonary disease | 23 | No | No |
OCS Lung Organ Care System, Transmedics Inc, USA. ECMO Extracorporeal membranous oxygenation; FiO2 Fraction of inspired oxygen; PaO2 Partial pressure of oxygen
Postoperative data are summarized in Table 4. Mechanical ventilation was discontinued within 48 h for each recipient and no patient stayed in the intensive care unit longer than eight days. Primary graft dysfunction (PGD) scores were detemined based on PF ratios obtained from postoperative ABG values and radiographic imaging to investigate for abnormalities. Recipients 2 and 3 showed an improvement in PGD score, reaching an ideal score of 0 in 72 h. They had uneventful postoperative courses and were discharged home within one month of transplantation. Recipient 1 remained at a PGD score of 3 at 72 h and also experienced prolonged postoperative delirium. Despite the development of prolonged PGD, the authors believe that LTx was justified given the suitable objective assessment of the donor lungs during EVLP. Additionally, this patient was able to recover and was successfully discharged home. The 90-day mortality rate was 0% for all recipients.
TABLE 4.
Postoperative data
| Recipient | Diagnosis | Mechanical ventilation, h | ICU stay, days | PGD grade | ||
|---|---|---|---|---|---|---|
|
| ||||||
| 0 h | 24 h | 72 h | ||||
| 1 | COPD | 17 | 6 | 3 | 3 | 3 |
| 2 | Cystic fibrosis | 33 | 5 | 3 | 0 | 0 |
| 3 | COPD | 40 | 8 | 2 | 2 | 0 |
COPD Chronic obstructive pulmonary disease; ICU Intensive care unit. PGD Postgraft dysfunction (Grade 0: Partial pressure of oxygen/fraction of inspired oxygen [PF] ratio >300 and normal chest x-ray, Grade 1: PF ratio >300 and diffuse infiltrates, Grade 2: PF ratio 200–300 and diffuse infiltrates, Grade 3: PF ratio <200 and diffuse infiltrates)
Table 5 provides midterm follow-up data for each patient. All patients are alive and maintain excellent forced expiratory volume in 1 s and forced vital capacity values, reflecting healthy lung function post-transplantation.
TABLE 5.
Midterm follow-up
| Recipient | Dx | Follow-up, months | Best FEV1 | Best FVC | Status |
|---|---|---|---|---|---|
| 1 | COPD | 7.9 | 70% predicted | 85% predicted | Alive |
| 2 | CF | 6.8 | 74% predicted | 77% predicted | Alive |
| 3 | COPD | 3.4 | 77% predicted | 66% predicted | Alive |
CF Cystic fibrosis; COPD Chronic obstructive pulmonary disease; Dx Diagnosis; FEV1 Forced expiratory volume in 1 s; FVC Forced expiratory volume
DISCUSSION
Currently, the level of donor lungs that are suitable for LTx is insufficient to ameliorate the growing transplant wait list. As a result, individuals on wait lists are faced with an increased risk for death, and it is imperative that a solution to this deficiency is pursued. Our centre’s experience with DCD lungs has yielded promising results, suggesting that this method is a viable alternative to increase the donor pool.
DCD donors have been used for numerous other types of solid organ transplant, from kidney and liver to lung (9–13). The experience with DCD organs has been largely positive, with post-transplant outcomes comparable with donors after brain death (DBD). DCD utilization initially lagged behind DBD primarily due to the conservative practices of many transplant teams; however, DCD utilization has increased dramatically in the past decade, resulting in more transplantations being performed at various centres (10,14). In Ontario, there has been an increase in deceased donor rates of 25% as a result of increased DCD activity (15).
Numerous centres around the world have reported on their experiences with LTx using DCD donors (16–20). These reports provide support for the use of DCD lungs for transplantation, with post-transplant outcomes comparable with DBD transplantation (4,21–23).
By combining EVLP technology and DCD lungs, we may be able to expand the donor pool even further. Having the ability to assess DCD lungs in addition to neurological declaration of death lungs before transplantation allows for a more informed clinical decision that may lead to successful transplantation with lungs that traditionally would not be used. The use of EVLP for DCD lungs has also shown promising results in early animal studies (24). Our experience, along with that of the Toronto group (4), represents one of the few cases utilizing DCD lungs undergoing EVLP and is the only reported case in performing EVLP on a portable device with DCD lungs.
EVLP also has the distinct advantage of being able to provide personalized therapy to donor lungs before transplantation. Studies assessing the benefits of interleukin-10 therapy and the use of tissue plasminogen activator have been published (25,26).
Considering the overall LTx process, procurement and transport of the lungs to the transplant centre causes a window of cold ischemic time to occur. Ischemic time has been shown to correlate with increased postgraft dysfunction in the donor lungs (27). Furthermore, the development of higher levels of PGD causes increased mortality in the short term (<30 days) and in the long term (>1 year) (28). Using the technique of portable EVLP, we were able to perfuse the lungs at normothermic conditions early in the process, thus significantly reducing ischemic times. As a result, our technique has the potential to reduce the damage associated with PGD and increase short- and long-term survival rates of lung recipients. The Transmedics OCS Lung device used in these cases is currently being evaluated for efficacy compared with current standard of care in the INSPIRE trial (NCT01630434) (29). Despite our success with immediate EVLP with DCD lungs, there is literature suggesting that a delayed EVLP strategy with a period of cold ischemic time may also be appropriate (30). The ideal protocol continues to be investigated with opportunity for both immediate and delayed EVLP.
Regarding the University of Alberta Hospital Transplant Program specifically, our centre is the most geographically isolated thoracic transplantation program in the world, with a catchment area >6 million km2 serving >7 million Canadians. The geographical isolation and large catchment area involved with this transplant program creates a demand for more effective methods of preserving lungs as they are transported large distances with long ischemic times, and possibly treating them on their way to the centre for transplant. Currently, our centre is only able to accept 27% of all lung donation offers and, consequently, the death rate on the wait list is 33%. Thus, the use of a portable EVLP system, such as the TransMedics OCS device, is a novel improvement to the transplant protocol implemented in centres with large catchment areas, with the ability to significantly reduce the ischemic time of the donor lung, leading to improved graft survival.
The combination of including DCD lungs in the donor pool along with using EVLP will effectively complement the implementation of Bill 207, the Human Tissue and Organ Donation Amendment Act of Alberta. This bill essentially increases the number of opportunities that Albertans will have to agree to organ donation, with the mandate to expand the donor pool in the aforementioned catchment area. Using portable EVLP, lungs donated from areas further away from the centre will be able to be maintained at a high quality, and any required treatments can be started on the way to the transplant centre. Overall, the donor pool will be expanded and any damage to the lungs based on transport time will be mitigated.
Therefore, the implementation of this technology with DCD donors to increase the virtual pool of donor organs represents a significant investment back into the public as the awareness for donation increases (Bill 207) in parallel with an increased donor utilization rate.
CONCLUSION
Our experience with lung transplantation from DCD donors has been largely positive. Although only a small number of LTx using DCD donors have been completed at our institution, we believe that a significant increase in the number of transplants being performed can be achieved through using this group of donors. By using portable EVLP to assess these lungs before transplant, we are able to significantly reduce ischemic times, continuously monitor and evaluate the lungs and apply novel therapeutics to improve lung function. Ultimately this will enable the most efficient utilization of available donor lungs, leading to more transplants and fewer recipient deaths on the wait list.
Acknowledgments
The authors acknowledge the Human Organ Procurement and Exchange (HOPE) program for their contributions to this work. They also acknowledge the University Hospital Foundation (UHF).
Footnotes
AUTHOR CONTRIBUTIONS: Sabin Bozso: composed manuscript and performed data collection; Vishnu Vasanthan: composed manuscript and performed data collection; Jessica Luc: performed data collection; Katie Kinaschuk: performed data collection; Darren Freed: edited manuscript and provided intellectual content; Jayan Nagendran: corresponding author who performed the case and supervised manuscript preparation and data collection.
DISCLOSURES: The authors have no financial disclosures or conflicts of interest to declare.
REFERENCES
- 1.Yusen RD, Christie JD, Edwards LB, et al. The Registry of the International Society for Heart and Lung Transplantation: Thirtieth adult lung and heart-lung transplant report – 2013; Focus theme: Age. J Heart Lung Transplant. 2013;32:965–78. doi: 10.1016/j.healun.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Valapour M, Paulson K, Smith JM, et al. OPTN/SRTR 2011 annual data report: Lung. Am J Transplant. 2013;13(Suppl 1):149–77. doi: 10.1111/ajt.12024. [DOI] [PubMed] [Google Scholar]
- 3.Steen S, Liao Q, Wierup PN, Bolys R, Pierre L, Sjoberg T. Transplantation of lungs from non-heart-beating donors after functional assessment ex vivo. Ann Thorac Surg. 2003;76:244–52. doi: 10.1016/s0003-4975(03)00191-7. [DOI] [PubMed] [Google Scholar]
- 4.Cypel M, Yeung JC, Liu M, et al. Normothermic ex vivo lung perfusion in clinical lung transplantation. N Engl J Med. 2011;364:1431–40. doi: 10.1056/NEJMoa1014597. [DOI] [PubMed] [Google Scholar]
- 5.Valenza F, Rosso L, Coppola S, et al. Ex vivo lung perfusion to improve donor lung function and increase the number of organs available for transplantation. Transpl Int. 2014;27:553–61. doi: 10.1111/tri.12295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daemen JW, Kootstra G, Wijnen RM, Yin M, Heineman E. Nonheart-beating donors: The Maastricht experience. Clin Transpl. 1994:303–16. [PubMed] [Google Scholar]
- 7.Van De Wauwer C, Verschuuren EA, van der Bij W, Nossent GD, Erasmus ME. The use of non-heart-beating lung donors category III can increase the donor pool. Eur J Cardiothorac Surg. 2011;39:e175–80. doi: 10.1016/j.ejcts.2011.01.035. [DOI] [PubMed] [Google Scholar]
- 8.Warnecke G, Moradiellos J, Tudorache I, et al. Normothermic perfusion of donor lungs for preservation and assessment with the organ care system lung before bilateral transplantation: A pilot study of 12 patients. Lancet. 2012;380:1851–8. doi: 10.1016/S0140-6736(12)61344-0. [DOI] [PubMed] [Google Scholar]
- 9.Dominguez-Gil B, Haase-Kromwijk B, Van Leiden H, et al. Current situation of donation after circulatory death in European countries. Transpl Int. 2011;24:676–86. doi: 10.1111/j.1432-2277.2011.01257.x. [DOI] [PubMed] [Google Scholar]
- 10.Klein AS, Messersmith EE, Ratner LE, Kochik R, Baliga PK, Ojo AO. Organ donation and utilization in the United States, 1999–2008. Am J Transplant. 2010;10(4 Pt 2):973–86. doi: 10.1111/j.1600-6143.2009.03008.x. [DOI] [PubMed] [Google Scholar]
- 11.Morrissey PE, Monaco AP. Donation after circulatory death: Current practices, ongoing challenges, and potential improvements. Transplantation. 2014;97:258–64. doi: 10.1097/01.TP.0000437178.48174.db. [DOI] [PubMed] [Google Scholar]
- 12.Neyrinck A, Van Raemdonck D, Monbaliu D. Donation after circulatory death: Current status. Curr Opin Anaesthesiol. 2013;26:382–90. doi: 10.1097/ACO.0b013e328360dc87. [DOI] [PubMed] [Google Scholar]
- 13.Bellingham JM, Santhanakrishnan C, Neidlinger N, et al. Donation after cardiac death: A 29-year experience. Surgery. 2011;150:692–702. doi: 10.1016/j.surg.2011.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson RJ, Bradbury LL, Martin K, Neuberger J, UK Transplant Registry Organ donation and transplantation in the UK – the last decade: A report from the UK national transplant registry. Transplantation. 2014;97(Suppl 1):S1–S27. doi: 10.1097/01.TP.0000438215.16737.68. [DOI] [PubMed] [Google Scholar]
- 15.Hernadez-Alejandro R, Wall W, Jevnikar A, et al. Organ donation after cardiac death: Donor and recipient outcomes after the first three years of the Ontario experience. Can J Anaesth. 2011;58:599–605. doi: 10.1007/s12630-011-9511-9. [DOI] [PubMed] [Google Scholar]
- 16.Zych B, Popov AF, Amrani M, et al. Lungs from donation after circulatory death donors: An alternative source to brain-dead donors? Midterm results at a single institution. Eur J Cardiothorac Surg. 2012;42:542–9. doi: 10.1093/ejcts/ezs096. [DOI] [PubMed] [Google Scholar]
- 17.Mason DP, Murthy SC, Gonzalez-Stawinski GV, et al. Early experience with lung transplantation using donors after cardiac death. J Heart Lung Transplant. 2008;27:561–3. doi: 10.1016/j.healun.2008.01.023. [DOI] [PubMed] [Google Scholar]
- 18.Mason DP, Brown CR, Murthy SC, et al. Growing single-center experience with lung transplantation using donation after cardiac death. Ann Thorac Surg. 2012;94:406–11. doi: 10.1016/j.athoracsur.2012.03.059. [DOI] [PubMed] [Google Scholar]
- 19.Puri V, Scavuzzo M, Guthrie T, et al. Lung transplantation and donation after cardiac death: A single center experience. Ann Thorac Surg. 2009;88:1609–14. doi: 10.1016/j.athoracsur.2009.06.039. [DOI] [PubMed] [Google Scholar]
- 20.Cypel M, Sato M, Yildirim E, et al. Initial experience with lung donation after cardiocirculatory death in canada. J Heart Lung Transplant. 2009;28:753–8. doi: 10.1016/j.healun.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 21.Wigfield CH, Love RB. Donation after cardiac death lung transplantation outcomes. Curr Opin Organ Transplant. 2011;16:462–8. doi: 10.1097/MOT.0b013e32834a99ac. [DOI] [PubMed] [Google Scholar]
- 22.De Vleeschauwer SI, Wauters S, Dupont LJ, et al. Medium-term outcome after lung transplantation is comparable between brain-dead and cardiac-dead donors. J Heart Lung Transplant. 2011;30:975–81. doi: 10.1016/j.healun.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 23.Mason DP, Thuita L, Alster JM, et al. Should lung transplantation be performed using donation after cardiac death? The United States experience. J Thorac Cardiovasc Surg. 2008;136:1061–6. doi: 10.1016/j.jtcvs.2008.04.023. [DOI] [PubMed] [Google Scholar]
- 24.Nakajima D, Chen F, Yamada T, et al. Reconditioning of lungs donated after circulatory death with normothermic ex vivo lung perfusion. J Heart Lung Transplant. 2012;31:187–93. doi: 10.1016/j.healun.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 25.Cypel M, Liu M, Rubacha M, et al. Functional repair of human donor lungs by IL-10 gene therapy. Sci Transl Med. 2009;1:49. doi: 10.1126/scitranslmed.3000266. [DOI] [PubMed] [Google Scholar]
- 26.Machuca TN, Hsin MK, Ott HC, et al. Injury-specific ex vivo treatment of the donor lung: Pulmonary thrombolysis followed by successful lung transplantation. Am J Respir Crit Care Med. 2013;188:878–80. doi: 10.1164/rccm.201302-0368LE. [DOI] [PubMed] [Google Scholar]
- 27.Kuntz CL, Hadjiliadis D, Ahya VN, et al. Risk factors for early primary graft dysfunction after lung transplantation: A registry study. Clin Transplant. 2009;23:819–30. doi: 10.1111/j.1399-0012.2008.00951.x. [DOI] [PubMed] [Google Scholar]
- 28.Christie JD, Kotloff RM, Ahya VN, et al. The effect of primary graft dysfunction on survival after lung transplantation. Am J Respir Crit Care Med. 2005;171:1312–6. doi: 10.1164/rccm.200409-1243OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Warnecke G, Van Raemdonck D, Massard G, et al. The INSPIRE Lung international trial evaluating the impact of portable ex-vivo perfusion using the organ care system (OCS™) lung technology on routine lung transplant outcomes. J Heart Lung Transplant. 2014;33:S72. [Google Scholar]
- 30.Mulloy DP, Stone ML, Crosby IK, et al. Ex vivo rehabilitation of non-heart-beating donor lungs in preclinical porcine model: Delayed perfusion results in superior lung function. J Thorac Cardiovasc Surg. 2012;144:1208–15. doi: 10.1016/j.jtcvs.2012.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]


