Abstract
Because only pathologic examination can confirm the presence or absence of malignant disease in cancer patients, a certain rate of misinterpretation in any kind of imaging study is inevitable. For the accuracy of interpretation to be improved, determination of the nature, causes, and magnitude of this problem is needed. This study was designed to collect pertinent information from physicians referring patients for oncologic 18F-FDG PET/CT.
Methods
A total of 662 referring physicians completed an 11-question survey focused on their experience with the interpretation of oncologic 18F-FDG PET/CT studies. The participants were oncologists (36.1%; n = 239), hematologists (14.5%; n = 96), radiation oncologists (7.4%; n = 49), surgeons (33.8%; n = 224), and other physicians (8.2%; n = 54). Questions were aimed at determining the frequency, nature, and causes of scan misinterpretations as well as potential solutions to reduce the frequency of misinterpretations.
Results
Perceived misinterpretation rates ranged from 5% to 20%, according to most (59.3%) of the participants; 20.8% of respondents reported rates of less than 5%. Overinterpretation rather than underinterpretation was more frequently encountered (68.9% vs. 8.7%, respectively). Limited availability of a patient’s history and limited experience of interpreters were the major contributors to this phenomenon, according to 46.8% and 26.7% of the participants, respectively. The actions most commonly suggested to reduce misinterpretation rates (multiple suggestions were possible) were the institution of multidisciplinary meetings (59.8%), the provision of adequate history when ordering an examination (37.4%), and a discussion with imaging specialists when receiving the results of the examination (38.4%).
Conclusion
Overinterpretation rather than underinterpretation of oncologic 18F-FDG PET/CT studies prevails in clinical practice, according to referring physicians. Closer collaboration of imaging specialists with referring physicians through more multidisciplinary meetings, improved communication, and targeted training of interpreting physicians are actions suggested to reduce the rates of misinterpretation of oncologic 18F-FDG PET/CT studies.
Keywords: overinterpretation, false-positive results, false-negative results, accuracy, pitfall
PET/CT has a well-documented role in the clinical management of oncology patients (1–3) and has been widely incorporated into clinical protocols and algorithms (4–6). The accurate interpretation of oncologic 18F-FDG PET/CT studies is critical for appropriate patient management. Although numerous studies have assessed the performance of 18F-FDG PET/CT, to our knowledge no study has analyzed the problem of misinterpretation of 18F-FDG PET/CT studies in clinical practice.
The idea for the present study was generated from the results of a recent survey of 961 referring physicians performed by our group (7). This survey revealed, among other issues, considerable concerns about the correct interpretation of oncologic 18F-FDG PET/CT studies. More specifically, 40.9% of the 961 participating referring physicians reported overinterpretation as a major concern with 18F-FDG PET/CT. Therefore, the present study was designed to better understand the nature of the problem and to explore potential solutions. We used a web-based survey as an effective and technically feasible way of collecting data from busy health care professionals (8,9).
MATERIALS AND METHODS
In this study, we used a web-based questionnaire for physicians who manage oncology patients. The study was initiated in June 2012 through an e-mail request for participation to corresponding authors of articles appearing in major clinical oncologic journals. E-mail addresses were collected from the PubMed database. The e-mail invitation asked recipients to complete an anonymous questionnaire, provided that they were physicians actively referring patients for oncologic 18F-FDG PET/CT. A web link was provided for direct access to the questionnaire.
The questionnaire consisted of 11 multiple-choice questions with an open text field for optional comments. The questionnaire was constructed with a commercially available platform (SurveyMonkey; http://www.surveymonkey.com/). The questions were developed by experienced multiinstitutional PET/CT imaging specialists and inquired about clinicians’ perspectives on the estimated rates and causes of misinterpretation of oncologic 18F-FDG PET/CT studies as well as possible actions to reduce this problem. Three of the questions were related to the participant’s specialty, experience with 18F-FDG PET/CT, and practice environment. The specific questions in the survey are shown in the Appendix.
All survey questions contained a text box for comments. For questions 3, 4, and 8, the answer options were sequenced randomly to avoid any potential bias. Multiple answers to these questions were allowed.
The survey remained open for participation for 8 wk after initiation. A single reminder to complete the survey was sent by e-mail 1–4 wk after the initial invitation. Repeat entries were prevented by a survey-incorporated denial of access for recipients who had already completed the survey. Ineligible participants (physicians in nonrelevant specialties who were not ordering 18F-FDG PET/CT examinations for their patients) were excluded from the analysis (n = 37).
RESULTS
Of the 699 respondents who completed the survey, 662 (94.7%) were eligible for inclusion. Of the eligible participants’ responses, 47.3% (n = 313) were from Europe, 35.0% (n = 232) were from North America, 12.4% (n = 82) were from Asia, 3.1% (n = 21) were from Australia and New Zealand, 1.1% (n = 7) were from Africa, and 1.1% (n = 7) were from South America. Of the 662 participants, 36.1% (n = 239) were oncologists, 33.8% (n = 224) were surgeons, 14.5% (n = 96) were hematologists, 7.4% (n = 49) were radiation oncologists, and 7.7% (n = 51) had various clinical specialties. Three of the participants (0.5%) did not declare their specialty.
Most of the respondents (85.8%; 568/662) indicated that they practiced medicine in an academic environment, 6.5% (43/662) practiced in a nonacademic environment public hospital, 5.0% (33/662) were in private practice, and 2.7% (18/662) refrained from answering this question. Most of the respondents (95.6%; 633/662) indicated that they were ordering 18F-FDG PET/CT examinations at the time that they responded to the survey. For each question, there were a limited number of participants who did not provide a response.
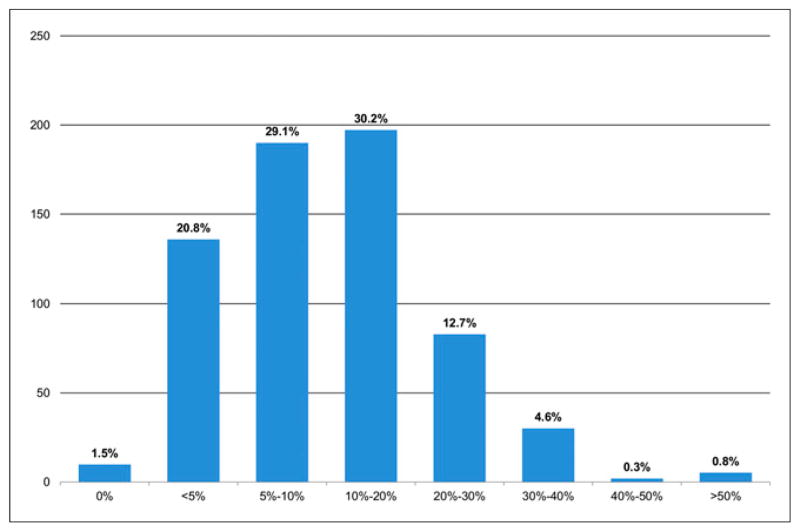
A total of 197 of 653 respondents (30.2%) estimated that misinterpretations occurred in 10%–20% of all cases, whereas 29.1% reported misinterpretation rates of 5%–10% (question 1; Fig. 1). Thus, 59.3% of respondents estimated that misinterpretation rates ranged from 5% to 20%. A total of 136 of 653 respondents (20.8%) estimated that misinterpretation rates were less than 5%, whereas 12.7% (83/653) thought that the rates were 20%–30%. Very few respondents (4.6%; 30/653) indicated that 18F-FDG PET/CT misinterpretations were very frequent, at 30%–40%.
FIGURE 1.
Responses to question 1: What is your estimation of the percentage of 18F-FDG PET/CT studies that are misinterpreted by the radiologists/nuclear medicine physicians reporting the scan results?
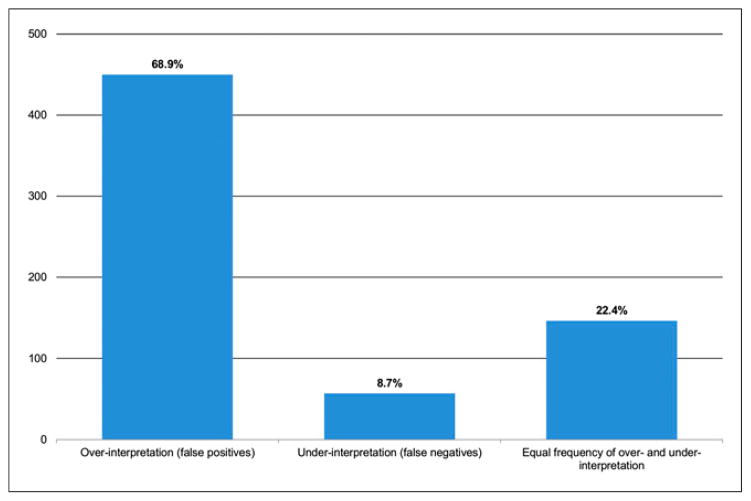
The answers to the question regarding over-versus under-interpretation (question 2; Fig. 2) suggested that PET/CT studies most frequently resulted in overinterpretation, as indicated by 450 of 653 respondents (68.9%). In contrast, only 146 of 653 participants (22.4%) responded that overinterpretation and underinterpretation occurred at similar rates, whereas only 57 of 653 respondents (8.7%) were predominantly concerned about underinterpretation of 18F-FDG PET/CT studies.
FIGURE 2.
Responses to question 2: In your experience, when an 18F-FDG PET/CT study is misinterpreted, is the reason most often overinterpretation (false-positive results), underinterpretation (false-negative results), or an equal frequency of overinterpretation and underinterpretation?
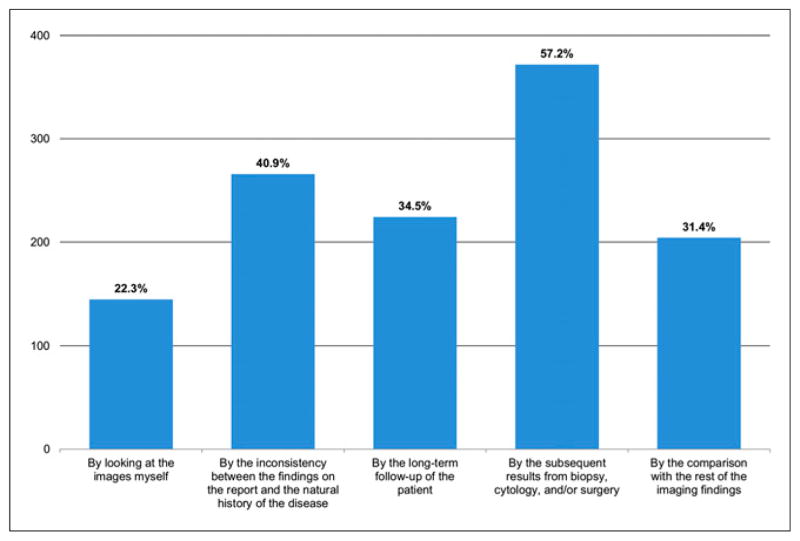
Question 3 inquired about how participants recognized the misinterpretation of 18F-FDG PET/CT studies (Fig. 3). Multiple answers to this question were allowed. Most respondents indicated that either subsequent results of cytology, biopsy, or surgery (57.2%; 372/650) or inconsistencies between the reported findings and the natural course of the disease (40.9%; 266/650) usually prompted them to consider that the PET interpretation was incorrect. A significant number (34.5%; 224/650) of respondents indicated that long-term follow-up commonly led to the conclusion of misinterpretation, whereas comparison of the reported 18F-FDG PET/CT results with other imaging findings was another commonly reported (31.4%; 204/650) way of recognizing misinterpretation. Only 145 of 650 respondents (22.3%) stated that they usually noted inconsistencies by personally reviewing the 18F-FDG PET/CT images.
FIGURE 3.
Responses to question 3: In what way(s) do you most often recognize misinterpretation of 18F-FDG PET/CT imaging studies?
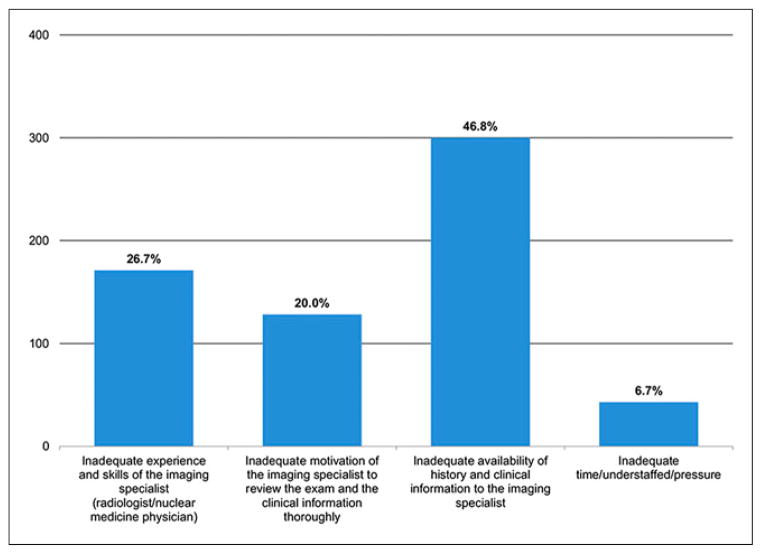
A total of 300 of 641 respondents (46.8%) thought that a lack of adequate history and clinical information was a common cause of 18F-FDG PET/CT misinterpretation (question 4; Fig. 4). “Inadequate experience and skills of the imaging specialist” was mentioned by 171 of 641 participants (26.7%) as another common cause for misinterpretation. “Inadequate motivation of the imaging specialist” (20.0%; 128/641) and “inadequate time/understaffed/pressure” (6.7%; 43/641) accounted for the rest of the responses. In this question, 90 of 641 respondents (14.0%) also commented (in the open text field for optional comments) that misinterpretation was expected as an inherent limitation of the imaging technique.
FIGURE 4.
Responses to question 4: In your experience, misinterpretation of 18F-FDG PET/CT studies is most often a result of … (choices were given on potential causes of misinterpretation).
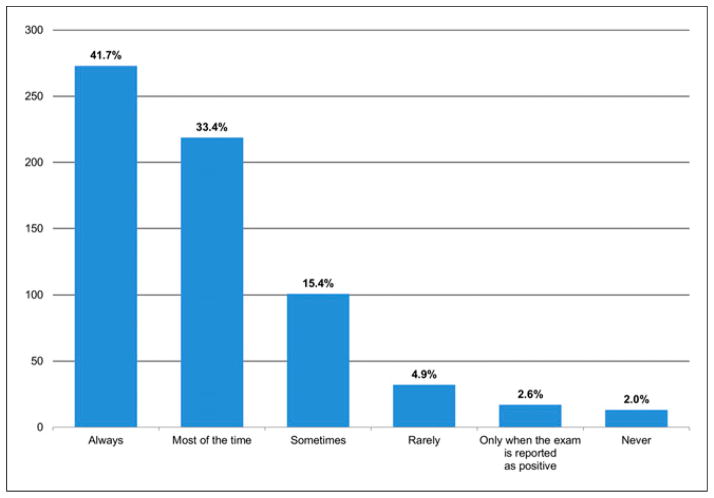
About 75% of the participating referring physicians stated that they “always” (41.7%; 273/655) or “most of the time” (33.4%; 219/655) reviewed their patients’ 18F-FDG PET/CT images (question 5; Fig. 5). Totals of 15.4% (101/655) responded with “sometimes,” 4.9% (32/655) responded with “rarely,” and 2.6% (17/655) responded with “only when the exam is reported as positive.” Only 2.0% (13/655) indicated that they never reviewed the 18F-FDG PET/CT images.
FIGURE 5.
Responses to question 5: How often do you review the 18F-FDG PET/CT images yourself?
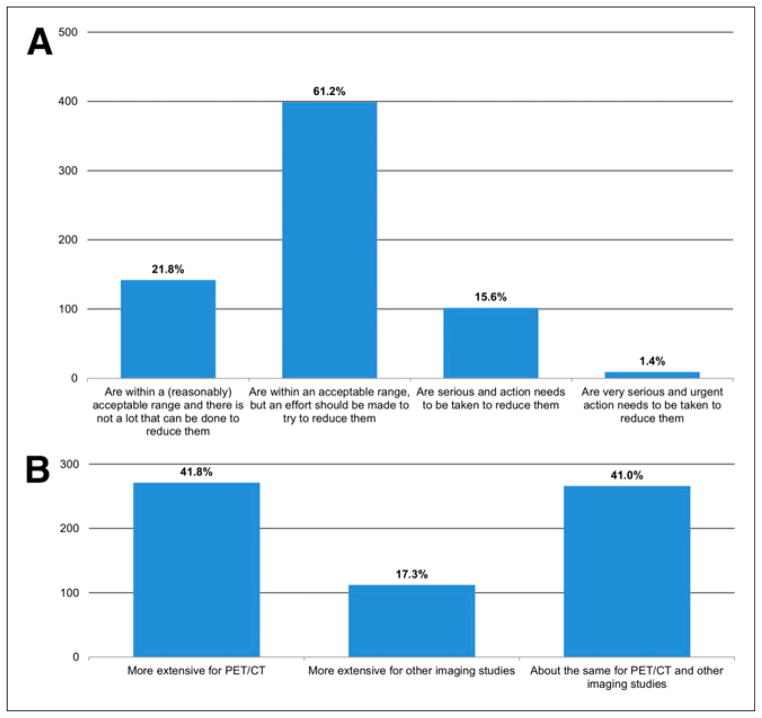
With regard to the consequences of 18F-FDG PET/CT misinterpretation (question 6; Fig. 6A), most of the participants (83.0%; 541/652) believed that these are within an acceptable range. A total of 15.6% (102/652) stated that the consequences are serious and that action needs to be taken to reduce the rates of misinterpretation, whereas very few (1.4%; 9/652) thought that “urgent” action is needed. Among the 541 participants who answered that the consequences of 18F-FDG PET/CT misinterpretation are within an acceptable or expected range, 26.2% (142/541) thought that not much can be done to reduce the rates of misinterpretation, and 73.8% (399/541) indicated that an effort should be made to reduce the rates.
FIGURE 6.
(A) Responses to question 6: In your opinion, the consequences of 18F-FDG PET/CT misinterpretation are … (choices were given about the seriousness of the consequences of 18F-FDG PET/CT misinterpretation and the importance of reducing misinterpretation). (B) Responses to question 7: Misinterpretation of 18F-FDG PET/CT studies in comparison with misinterpretation of other imaging studies (CT, MR imaging, ultrasound) is … (choices were given about which is more extensive in clinical practice).
A total of 41.0% (266/649) of respondents thought that the magnitude of 18F-FDG PET/CT misinterpretation was about equal to that of other imaging studies (question 7; Fig. 6B). Nearly the same fraction of respondents (41.8%; 271/649) believed that misinterpretation was more extensive for 18F-FDG PET/CT, whereas 17.3% (112/649) indicated the opposite.
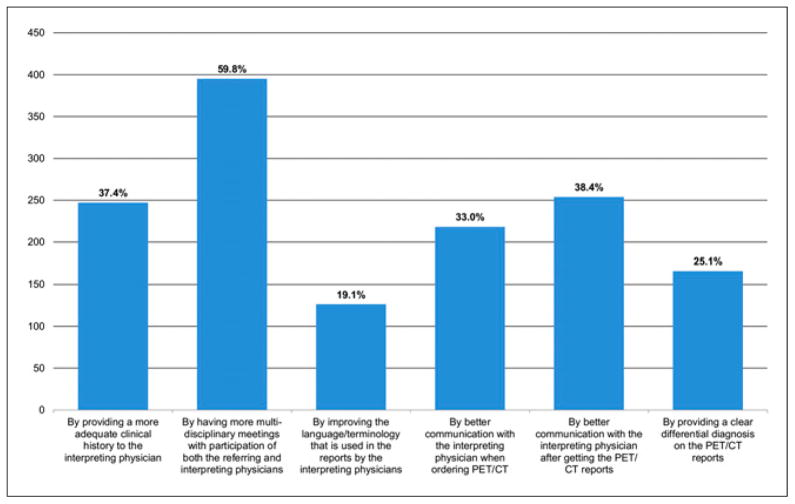
Question 8 asked for suggestions for reducing the rates of misinterpretation and the consequences of misinterpretation (question 8; Fig. 7). Possible responses consisted of 6 randomly arranged choices, and an open text field was available for providing other potential solutions. Most of the respondents (59.8%; 395/661) selected “by having more multidisciplinary meetings with participation of both the referring and interpreting physicians” as an answer. The second most popular selection was “by better communication with the interpreting physician after getting the PET/CT reports” (38.4%; 254/661), and the next most popular selection was “by providing a more adequate clinical history to the interpreting physician” (37.4%; 247/661). “By better communication with the interpreting physician when ordering PET/CT” was another frequent choice (33.0%; 218/661). “By providing a clear differential diagnosis on the PET/CT reports” (25.1%; 166/661) and “by improving the language/terminology that is used in the reports by the interpreting physicians” (19.1%; 126/661) were less frequent responses. The few additional comments (n = 67) provided were rather random, with most of them (n = 35) suggesting better standardization of the ordering and interpretation process.
FIGURE 7.
Responses to question 8: In what way(s) should the medical community try to reduce the misinterpretation of 18F-FDG PET/CT studies as well as the consequences of these misinterpretations?
DISCUSSION
In the present study, a survey of global practitioners using oncologic 18F-FDG PET/CT was used to collect opinions about the nature, magnitude, and causes of 18F-FDG PET/CT misinterpretation. We also solicited suggestions for reducing the problem. The collective experiences of referring physicians with oncologic 18F-FDG PET/CT are important because they illustrate problems encountered with 18F-FDG PET/CT reports in routine clinical practice. Awareness of these problems is a prerequisite for improvement and for oncologic 18F-FDG PET/CT to reach its maximum potential.
The survey suggested (question 2; Fig. 2) that overinterpretation rather than underinterpretation constitutes the main source of errors in oncologic 18F-FDG PET/CT reporting. According to clinicians’ experiences (question 4; Fig. 4), this problem originates not only from inevitable technical limitations but also from inadequate correlation with a patient’s clinical history and from the limited experience or motivation of the interpreting physician. The collective responses also showed (question 6; Fig. 6A) that even though the consequences of misinterpretation are estimated to be within a (reasonably) acceptable range, the medical community still believes that some action is required to reduce the rates of misinterpretation. Suggested solutions mostly favored better communication between referring and interpreting physicians (question 8; Fig. 7).
The perceived frequency and nature of 18F-FDG PET/CT misinterpretation, to the best of our knowledge, have not been investigated in the past, although causes for false-positive results (e.g., inflammatory processes, therapy-related changes, attenuation artifacts, and injection-induced radioactive clot) and false-negative results (e.g., partial-volume effect and low 18F-FDG affinity of tumors) in 18F-FDG PET/CT imaging have been widely discussed in the published medical literature (10–17). Furthermore, although in clinical practice oncology patients undergoing 18F-FDG PET/CT are heterogeneous, most clinical trials or retrospective studies have explored the performance of 18F-FDG PET/CT in very specific subgroups of patients and diseases. The lack of cumulative data on the overall performance of oncologic 18F-FDG PET/CT makes it difficult to appreciate the current status of this technique in clinical practice and to estimate the perceived sense of reliability of 18F-FDG PET/CT among referring physicians.
The reported frequency of 18F-FDG PET/CT misinterpretation (question 1; Fig. 1) may not accurately depict the actual extent of the problem; nevertheless, it reflects the perception of ordering clinicians. Therefore, it provides insights into the confidence of physicians using scan reports to make critical treatment decisions (e.g., surgical approach, type of chemotherapy regimen, radiation therapy planning, and additional workup). Interestingly, 59.3% of the respondents estimated misinterpretation rates of 5%–20%. These values correlate well with the 80%–95% accuracy of 18F-FDG PET/CT reported in most studies for a wide variety of cancers (5,18).
The fact that 20.8% of participating physicians thought that misinterpretation rates were less than 5% likely reflects the general acceptance of 18F-FDG PET/CT as the oncology imaging modality of choice. However, 12.7% of respondents estimated the misinterpretation rates to be 20%–30%, and 5.7% estimated the rates to be more than 30%; these results suggested that a significant number of physicians have some reservations about 18F-FDG PET/CT imaging.
Reassuringly, the overall magnitude and impact of the problem of 18F-FDG PET/CT misinterpretation do not seem to concern the medical community (question 6; Fig. 6). Only 17.0% (111/652) of physicians considered this a serious problem. Nevertheless, most of the participants (76.8%; 501/652) thought that some action should be taken to reduce the rates of misinterpretation.
Almost 8 times as many participants (68.9% vs. 8.7%) considered overinterpretation rather than underinterpretation to be the most frequently encountered problem (question 2; Fig. 2). This observation implies a significant concern about false-positive results rather than false-negative results in 18F-FDG PET/CT reports. False-positive results are caused by the non–cancer-specific kinetics of the 18F-FDG tracer (e.g., inflammation and infection) or, less frequently, by artifacts (e.g., attenuation artifacts, misregistration, and injection-induced 18F-FDG clot). Careful consideration of available information regarding a patient’s clinical status and history as well as diligent analysis of the distinctive features of image abnormalities should significantly reduce the likelihood of an 18F-FDG PET/CT examination being overinterpreted.
Interestingly, respondents in the United States (187/653) were even more concerned about overinterpretation (78.1%; 146/187) than those outside the United States (65.2%; 304/466), and the converse was true for responses regarding underinterpretation (3.2% [6/187] for U.S. respondents and 10.9% [51/466] for non–U.S. respondents, respectively). Therefore, it seems possible that the fear of litigation is an additional major cause of overcautious reporting (19).
The most important measure for improving oncologic 18F-FDG PET/CT reporting appears to be better communication (question 8; Fig. 7). Many participants suggested that referring physicians should provide a meaningful, well-structured clinical history when ordering an 18F-FDG PET/CT scan. This information would help interpreting physicians improve image interpretation. Along the same lines are the recommendations for more interaction of and cooperation between referring and interpreting physicians through direct communication before or after the scan or during multidisciplinary meetings.
A potential bias of the present study is the academic setting of most (85.8%) of the participating referring physicians, presumably a result of the method used to collect the contact details of the participating clinicians (through their scientific publications in oncology-related medical journals). Although the academic orientation of most of the participating physicians does not allow extrapolation of the survey results to the general medical community, the fact that clinical protocols for the management of cancer patients are generally uniform and used worldwide suggests that the survey results should be representative for the entire community of referring physicians.
CONCLUSION
Although the perceived oncologic 18F-FDG PET/CT misinterpretation rates and their consequences appear to be within a generally accepted range, there is a clear need for improvement. According to most respondents, improvement could be achieved through better communication of information about patients between referring and interpreting physicians. Targeted training of interpreting physicians and improved standardization of the exchange of information about patients could lead to improved accuracy of 18F-FDG PET/CT in oncology.
APPENDIX
List of Survey Questions
What is your estimation of the percentage of 18F-FDG PET/CT studies that are misinterpreted by the radiologists/nuclear medicine physicians reporting the scan results?
In your experience, when an 18F-FDG PET/CT study is misinterpreted, is the reason most often overinterpretation (false-positive results), underinterpretation (false-negative results), or an equal frequency of overinterpretation and underinterpretation?
In what way(s) do you most often recognize misinterpretation of 18F-FDG PET/CT imaging studies?
In your experience, misinterpretation of 18F-FDG PET/CT studies is most often a result of … (choices were given on potential causes of misinterpretation).
How often do you review the 18F-FDG PET/CT images yourself?
In your opinion, the consequences of 18F-FDG PET/CT misinterpretation are … (choices were given about the seriousness of the consequences of 18F-FDG PET/CT misinterpretation and the importance of reducing misinterpretation).
Misinterpretation of 18F-FDG PET/CT studies in comparison with misinterpretation of other imaging studies (CT, MR imaging, ultrasound) is … (choices were given about which is more extensive in clinical practice).
In what way(s) should the medical community try to reduce the misinterpretation of 18F-FDG PET/CT studies as well as the consequences of these misinterpretations?
What is your specialty?
Are you currently ordering 18F-FDG PET/CT examinations for your patients?
In what environment do you practice medicine?
Footnotes
DISCLOSURE
No potential conflict of interest relevant to this article was reported.
References
- 1.Hillner BE, Siegel BA, Liu D, et al. Impact of positron emission tomography/computed tomography and positron emission tomography (PET) alone on expected management of patients with cancer: initial results from the National Oncologic PET Registry. J Clin Oncol. 2008;26:2155–2161. doi: 10.1200/JCO.2007.14.5631. [DOI] [PubMed] [Google Scholar]
- 2.Tunis S, Whicher D. The National Oncologic PET Registry: lessons learned for coverage with evidence development. J Am Coll Radiol. 2009;6:360–365. doi: 10.1016/j.jacr.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Medicare & Medicaid Services. Decision memo for positron emission tomography (FDG) for solid tumors (CAG-00181R4) [Accessed October 29, 2014];Centers for Medicare & Medicaid Services website. http://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=263. Published June 11, 2013.
- 4.Royal College of Physicians and Royal College of Radiologists. [Accessed October 29, 2014];Evidence-based indications for the use of PET-CT in the UK. 2013 http://www.rcr.ac.uk/docs/radiology/pdf/2013_PETCT_RCP_RCR.pdf. Published 2013.
- 5.Podoloff DA, Ball DW, Ben-Josef E, et al. NCCN task force: clinical utility of PET in a variety of tumor types. J Natl Compr Canc Netw. 2009;7(suppl 2):S1–S26. doi: 10.6004/jnccn.2009.0075. [DOI] [PubMed] [Google Scholar]
- 6.PET Professional Resources and Outreach Source. [Accessed October 29, 2014];Part I: NCCN practice guidelines tabular summary (DD 3/20/13)—PET and PET/CT. http://snmmi.files.cms-plus.com/FileDownloads/Centers/NCCNPracticeGuidelinesI.pdf.
- 7.Karantanis D, Kalkanis D, Allen-Auerbach M, et al. Oncologic 18F-FDG PET/CT: referring physicians’ point of view. J Nucl Med. 2012;53:1499–1505. doi: 10.2967/jnumed.111.102228. [DOI] [PubMed] [Google Scholar]
- 8.Smith B, Smith TC, Gray GC, Ryan MA Millennium Cohort Study Team. When epidemiology meets the Internet: Web-based surveys in the Millennium Cohort Study. Am J Epidemiol. 2007;166:1345–1354. doi: 10.1093/aje/kwm212. [DOI] [PubMed] [Google Scholar]
- 9.Russell CW, Boggs DA, Palmer JR, Rosenberg L. Use of a Web-based questionnaire in the Black Women’s Health Study. Am J Epidemiol. 2010;172:1286–1291. doi: 10.1093/aje/kwq310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Long NM, Smith CS. Causes and imaging features of false positives and false negatives on F-PET/CT in oncologic imaging. Insights Imaging. 2011;2:679–698. doi: 10.1007/s13244-010-0062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang JM, Lee HJ, Goo JM, et al. False positive and false negative FDG-PET scans in various thoracic diseases. Korean J Radiol. 2006;7:57–69. doi: 10.3348/kjr.2006.7.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Truong MT, Viswanathan C, Carter BW, Mawlawi O, Marom EM. PET/CT in the thorax: pitfalls. Radiol Clin North Am. 2014;52:17–25. doi: 10.1016/j.rcl.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Karantanis D, Subramaniam RM, Mullan BP, Peller PJ, Wiseman GA. Focal F-18 fluorodeoxy-glucose accumulation in the lung parenchyma in the absence of CT abnormality in PET/CT. J Comput Assist Tomogr. 2007;31:800–805. doi: 10.1097/RCT.0b013e3180340376. [DOI] [PubMed] [Google Scholar]
- 14.Metser U, Even-Sapir E. Increased 18F-fluorodeoxyglucose uptake in benign, nonphysiologic lesions found on whole-body positron emission tomography/computed tomography (PET/CT): accumulated data from four years of experience with PET/CT. Semin Nucl Med. 2007;37:206–222. doi: 10.1053/j.semnuclmed.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 15.Truong MT, Erasmus JJ, Munden RF, et al. Focal FDG uptake in mediastinal brown fat mimicking malignancy: a potential pitfall resolved on PET/CT. AJR. 2004;183:1127–1132. doi: 10.2214/ajr.183.4.1831127. [DOI] [PubMed] [Google Scholar]
- 16.Kim BT, Kim Y, Lee KS, et al. Localized form of bronchioloalveolar carcinoma: FDG PET findings. AJR. 1998;170:935–939. doi: 10.2214/ajr.170.4.9530038. [DOI] [PubMed] [Google Scholar]
- 17.Berger KL, Nicholson SA, Dehdashti F, Siegel BA. FDG PET evaluation of mucinous neoplasms: correlation of FDG uptake with histopathologic features. AJR. 2000;174:1005–1008. doi: 10.2214/ajr.174.4.1741005. [DOI] [PubMed] [Google Scholar]
- 18.Antoch G, Saoudi N, Kuehl H, et al. Accuracy of whole-body dual-modality fluorine-18-2-fluoro-2-deoxy-D-glucose positron emission tomography and computed tomography (FDG-PET/CT) for tumor staging in solid tumors: comparison with CT and PET. J Clin Oncol. 2004;22:4357–4368. doi: 10.1200/JCO.2004.08.120. [DOI] [PubMed] [Google Scholar]
- 19.Imperato JP. The new medical malpractice crisis. N Engl J Med. 2003;349:912. doi: 10.1056/NEJM200308283490920. [DOI] [PubMed] [Google Scholar]