Abstract
Background
Road traffic injuries (RTIs) are a major public health concern in Libya. In the light of the armed conflict in Libya that broke out on February 2011 and the subsequent instability, the rate and pattern of RTIs was studied.
Methods
RTI patient data were gathered from Al-Jalaa hospital, the main trauma center in Benghazi, from 2010 to 2011. Various parameters [i.e. age, gender, nationality, method of entry, receiving department, intensive care unit (ICU) admission, duration of stay, method of discharge, and fatalities] were compared with data from the previous year (2010), and statistical analyses were performed (t-test, chi-square, and Poisson regression).
Results
During the conflict period, 15.8% (n=2,221) of hospital admissions were RTIs, that is, a rate of 6.08 RTI cases per day, levels not seen for 5 years (t=−5.719, p<0.001). The presence of armed conflict was found to have caused a significant 28% decrease in the trend of RTIs over the previous 10 years (B=−0.327, CI=−0.38–−0.28, p<0.001). February and March, the peak period of active combat in Benghazi, witnessed the lowest number of RTIs during the conflict period. The average age of an RTI decreased to 28.35±16.3 years (t=−7.257, p<0.001) with significantly more males (84.1%, n=1,755) being affected (χ2=4.595, p=0.032, df=1). There was an increase in the proportion of younger aged patients (from 0 to 29 years) (χ2=29.874, p<0.001, df=8). More patients required admission to the ICU (χ2=36.808, p<0.001, df=8), and the mortality of an RTI increased to 5.2% (n=116) (χ2=48.882, p<0.001, df=6).
Conclusion
There were fewer RTIs during the conflict period; however, those that occurred had higher morbidity and mortality. The profile of an RTI victims also changed to an increased prominence of young males and motorcyclists. Further research is required to propose and analyze possible interventions.
Keywords: road traffic accidents, road traffic injuries, motor vehicle, trauma, armed conflict, mortality, morbidity, Benghazi, Libya
The epidemiology of road traffic crashes has attracted considerable attention, especially in high-income countries. Less is known about road traffic accidents in low- and middle-income countries. Road traffic injuries (RTIs) have always been a major public health concern in Libya (1–4) – having the third highest per capita mortality from road traffic accidents worldwide.
The civil unrest witnessed in a number of low- and-middle-income countries inadvertently offered an additional perspective to road safety, as little research is available on the incidence of RTIs in times of war and civil unrest (5, 6). In February 2011, civilian protests in Libya quickly escalated to a full-scale armed conflict.
This study aims at determining the impact of armed conflict, and subsequent post-conflict conditions, on the pattern of RTIs in Libya.
Methods
Study population
Libya is a North African country with a population of approximately 6 million. Benghazi is the second largest city in Libya and the principal city of the eastern region with a population of slightly over 670,000.
Ethical approval
This study has been approved by the Biostatistics Department at Al-Jalaa hospital as well as by the Ethical Committee at the corresponding author's university. All data were anonymized, and only the variables under study were collected.
Data
Patient data were gathered retrospectively from the Biostatistics Department of Al-Jalaa hospital in Benghazi, Libya. This principal health care center receives the overwhelming majority of trauma and other emergency cases in eastern Libya. It is the oldest surgical hospital in the country and was established during the Italian colonization.
During the Libyan conflict, Al-Jalaa hospital received the vast majority of patients with war injuries. Despite financial and material shortages, the hospital remained functional during this period and continues providing quality services (7).
The collected data covers details of all patients who were received during January 1, 2010, to December 31, 2011. Total numbers of RTI hopitalizations, by sex, over the period 2001–2010 were available from a previous study (1). Records were subsequently filtered to include only RTIs (motor vehicle collisions). The parameters available were age, gender, nationality, method of entry, receiving department, intensive care unit (ICU) admission, duration of stay, method of discharge, and outcome (death). Hospital resources at Al-Jalaa hospital are limited and as such, only those who are severely injured are admitted to the ICU. Due to these strict admission criteria, ICU admission was used as an indicator of severity of injury.
The term ‘cold case’ for RTI patients refers either to a person who was involved in an accident but did not seek immediate medical attention until later or somebody who presented to the hospital earlier and then returned with additional relevant complaints.
Data from 2011 were considered to be from the ‘conflict period’ while data from 2010 was considered to be from the ‘non-conflict period’. January and early February of 2011 were also included as part of the ‘conflict period’ due to the abnormal security conditions that were present in the run-up to the war (the Egyptian and Tunisian revolutions).
Statistical methods
The collected data were imported into SPSS (version 18, Chicago) and summarized in the form of frequencies, means (with standard deviation) and were presented in table and chart format. Furthermore, student's t-tests and chi-square tests were used to compare continuous and categorical variables respectively. Poisson regression was used to determine the effect of the presence of armed conflict on the incidence rate of RTIs over the period 2001–2011, adjusting for sex, taking the logarithm of the population as an offset. The 2006 Libyan census and annual growth rate estimates were used to determine the population of Benghazi for the study years. The study uses trend analysis initially to determine the effect of armed conflict on the incidence rate (per 100,000 population) of RTIs. After establishing that 2010 is within the normal prewar trend, it is used as the reference for comparison with the conflict year (i.e. 2011) in a case-control manner. These two methods of analysis (i.e. trend and case-control) allow us to ascertain that 2011 is really ‘off-trend’ and displays an abnormal pattern from previous years.
Results
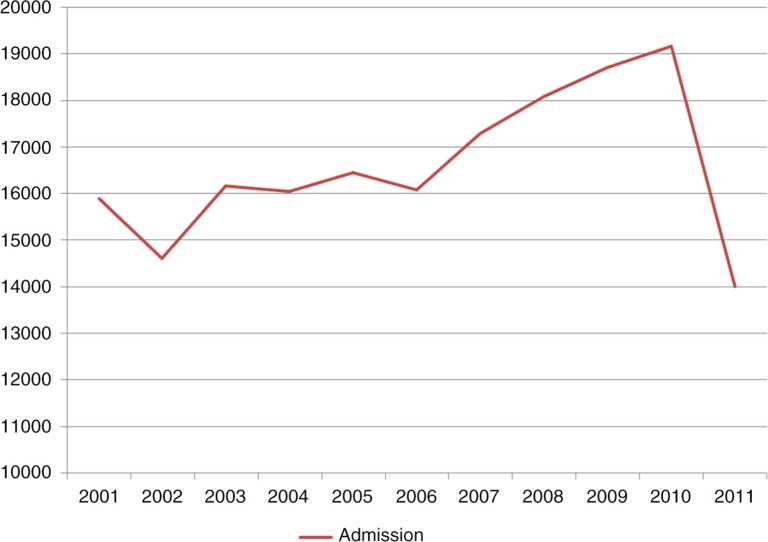
In 2011, Al-Jalaa hospital had received 13,995 cases from various parts of Libya (primarily Benghazi and eastern Libya). Figure 1 shows the trend of admissions for the period between 2001 and 2011. Overall, 40.9% (n=7,846) of patients in 2010 presented to the hospital as elective (non-emergency) cases, whereas that figure decreased in 2011 to 29.0% (n=4053) (χ2=35.792, p<0.001, df=1).
Fig. 1.
Graphical depiction of the total number of patients admitted to Al-Jalaa hospital from 2001 to 2011.
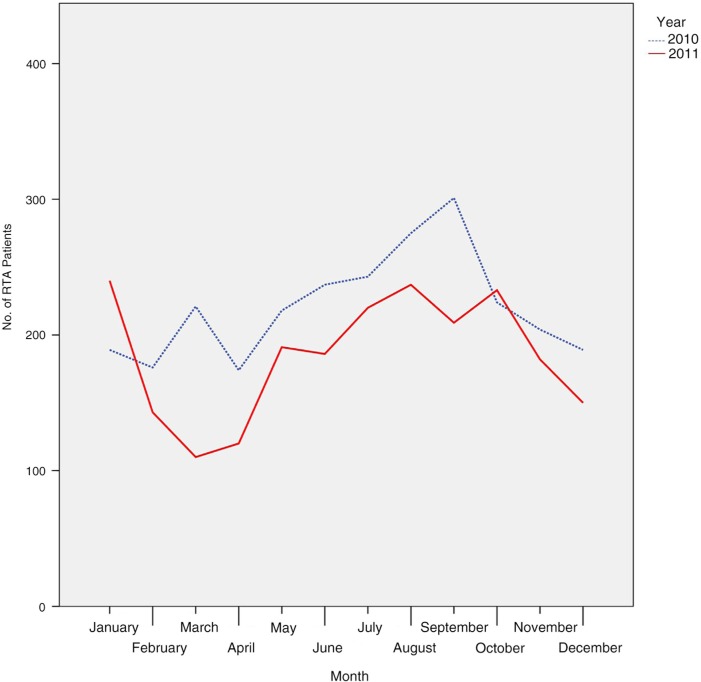
Among the patients received during the conflict period, 15.8% (n=2,221) were RTIs, that is, a rate of 6.08 RTI cases per day (a drop compared to previous years) (t=−5.719, p<0.001). February and March showed the lowest levels of RTIs during the conflict period (Fig. 2).
Fig. 2.
The number of road traffic accidents plotted against the months in 2010 and 2011.
In addition to a decrease in the number of RTI patients, the crude incidence rate was also affected (Table 1). There was found to be a statistically significant decrease by 28% in the rate of RTIs during the war (B=0.327, CI= 0.28–0.38, p<0.001). Libyan nationals comprised 94.6% (n=2,102) of the RTI victims while non-nationals formed the remaining 5.4% (n=119). There was a significant decrease in the number of non-Libyans who were involved in RTIs (χ2=34.731, p<0.001, df=1).
Table 1.
Comparison between 2010 and 2011 on gender of patients, state of entry, nationality, and age distribution of patients
| 2010 | 2011 | |||
|---|---|---|---|---|
| n | % | n | % | |
| Gender (χ 2=4.595, p=0.032, df=1) | ||||
| Male | 2,167 | 81.7 | 1,755 | 84.1 |
| Female | 486 | 18.3 | 333 | 15.9 |
| State of entry (χ 2=35.792, p<0.001, df=1) | ||||
| Cold case | 502 | 18.9 | 280 | 12.6 |
| Emergency | 2,151 | 81.1 | 1,941 | 87.4 |
| Nationality (χ 2=34.731, p<0.001, df=1) | ||||
| Libyan | 2,390 | 90.1 | 2,102 | 94.6 |
| Foreigner | 263 | 9.9 | 119 | 5.4 |
| Age distribution (year) (χ2=29.874, p<0.001, df=8) | ||||
| 0–9 | 276 | 10.4 | 266 | 12.0 |
| 10–19 | 340 | 12.8 | 346 | 15.6 |
| 20–29 | 781 | 29.4 | 703 | 31.7 |
| 30–39 | 544 | 20.5 | 433 | 19.5 |
| 40–49 | 311 | 11.7 | 225 | 10.1 |
| 50–59 | 189 | 7.1 | 116 | 5.2 |
| 60–69 | 131 | 4.9 | 74 | 3.3 |
| 70–79 | 60 | 2.3 | 44 | 2.0 |
| 80 and up | 21 | 0.8 | 14 | 0.6 |
Our study found that 64.7% (n=1,436) of the injured patients were from Benghazi. Al-Marj (11.9%, n=264) – around 100 km to the east – and Al-Wahat (7.2%, n=161) – around 100 km to the southwest – contributed the largest proportion of RTI cases from the rural areas.
The average age of an RTI patient in Jalaa was 28.35±16.3 years – compared to 30.86±16.9 years in 2010 (t=−7.257, p<0.001). This is reflected in the increase in the proportion of younger aged patients (from 0 to 29 years) (χ2=29.874, p<0.001, df=8).
Most of the injured (84.1%, n=1,755) during the conflict were males, a higher proportion than during the preconflict period (χ2=4.595, p=0.032, df=1). These figures are presented in further detail in Table 2.
Table 2.
Determination of the incidence rates (per 100,000 population) for road traffic injuries from 2001 to 2011 in Libya
| Male | Female | Overall | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n | Incidence rate | n | Incidence rate | n | Incidence rate | |
| 2001 | 1,313 | 417.1 | 300 | 101.6 | 1,613 | 264.4 |
| 2002 | 1,349 | 420.0 | 332 | 110.2 | 1,681 | 270.0 |
| 2003 | 1,564 | 477.2 | 376 | 122.3 | 1,940 | 305.4 |
| 2004 | 1,695 | 506.8 | 359 | 114.4 | 2,054 | 316.9 |
| 2005 | 1,758 | 515.2 | 422 | 131.8 | 2,180 | 329.6 |
| 2006 | 1,801 | 517.2 | 385 | 117.8 | 2,186 | 323.9 |
| 2007 | 1,934 | 544.5 | 438 | 131.4 | 2,372 | 344.5 |
| 2008 | 2,037 | 562.3 | 454 | 133.6 | 2,491 | 354.7 |
| 2009 | 2,107 | 570.2 | 476 | 137.3 | 2,583 | 360.6 |
| 2010 | 2,167 | 574.9 | 486 | 137.4 | 2,653 | 363.1 |
| 2001–2010 (preconflict) | 17,725 | 513.5 | 4,028 | 124.4 | 21,753 | 325.2 |
| 2011 (conflict) | 1,755 | 456.5 | 333 | 92.3 | 2,088 | 280.2 |
Most RTI patients were admitted to the Department of Orthopedics (45.6%, n=1,012) followed by the Department of Neurosurgery (25.9%, n=575). When compared to the previous year, there were significantly more admissions to the ICU. In 2010, 6.7% (n=177) of RTI cases were admitted to the ICU, whereas in 2011 that number rose to 8.7% (n=193) (χ2=36.808, p<0.001, df=8).
The vast majority of cases were received as emergency cases (87.4%, n=1,941) as opposed to cold cases (12.6%, n=280). There was an increase in emergency RTIs during the conflict period (χ2=35.792, p<0.001, df=1). During the conflict period, there was an increase in same-day discharge (i.e. No Stay) from 7.3% (n=194) in 2010 to 10.9% (n=243) (χ2=22.268, p<0.001, df=4). A linear-by-linear association showed that the primary difference between the duration of stay is focused on the ‘No Stay’ subsect (χ2=4.538, p=0.033, df=4) with no difference existing for the other period categories between the 2 years.
Vehicle occupants (drivers and passengers) formed the bulk of RTI patients (73.6%, n=1,633). More passengers but fewer drivers and pedestrians were admitted to the hospitals during the conflict period. Moreover, a strong increase in motorcycle injuries was observed (χ2=11.2, p=0.024, df=4).
When the method of discharge was analyzed, it was observed that the majority of discharges were scheduled to be followed on an outpatient basis (77.4%, n=1,719). Fatalities had increased from 4.3% in 2010 to 4.7% (n=106) in 2011. Also, startling increases were seen in the proportion of absconded (runaway) patients, from 3.28% (in 2010) to 5.2% during the conflict (Table 3). Patients who were referred from other hospitals (either within or outside Benghazi) increased in proportion between 2010 (1.8%, n=48) and 2011 (4.3%, n=95) (χ2=48.882, p<0.001, df=6).
Table 3.
Comparison between 2010 and 2011 on duration, role in the accident, method of discharge, and receiving department
| 2010 | 2011 | |||
|---|---|---|---|---|
| n | % | n | % | |
| Duration (χ2=22.268, p<0.001, df=4) | ||||
| No Stay | 194 | 7.3 | 243 | 10.9 |
| 1–7 days | 1,755 | 66.2 | 1,402 | 63.1 |
| 8–14 days | 402 | 15.2 | 349 | 15.7 |
| 15–29 days | 211 | 8.0 | 149 | 6.7 |
| 30+ days | 91 | 3.4 | 78 | 3.5 |
| Role (χ2=11.2, p=0.024, df=4) | ||||
| Pedestrian | 677 | 25.5 | 521 | 23.5 |
| Driver | 915 | 34.5 | 761 | 34.3 |
| Passenger | 1,002 | 37.8 | 872 | 39.3 |
| Motorcycle | 41 | 1.5 | 58 | 2.6 |
| Bicycle | 18 | 0.7 | 9 | 0.4 |
| Method of discharge (χ2=48.882, p<0.001, df=6) | ||||
| Transferred to another hospital | 47 | 1.8 | 95 | 4.3 |
| LAMA | 243 | 9.2 | 169 | 7.6 |
| Absconded | 87 | 3.3 | 116 | 5.2 |
| Discharged to attend OPD | 2,146 | 80.9 | 1,719 | 77.4 |
| Expired | 115 | 4.3 | 106 | 4.8 |
| Unspecified | 1 | 0.0 | 7 | 0.3 |
| Refused admission | 14 | 0.5 | 9 | 0.4 |
| Department (χ2=36.808, p<0.001, df=8) | ||||
| Chest Surgery | 114 | 4.3 | 85 | 3.8 |
| General Surgery | 246 | 9.3 | 132 | 5.9 |
| Hand Surgery | 2 | 0.1 | 1 | 0.0 |
| ICU | 179 | 6.7 | 193 | 8.7 |
| Neurosurgery | 690 | 26.0 | 575 | 25.9 |
| Oromaxillofacial Surgery | 76 | 2.9 | 79 | 3.6 |
| Orthopedic Surgery | 1,211 | 45.6 | 1,012 | 45.6 |
| Plastic Surgery | 135 | 5.1 | 137 | 6.2 |
| Unspecified | 0 | 0.0 | 7 | 0.3 |
Discussion
During the conflict period, RTIs decreased to levels not seen since 5 years (on par with 2006). The residents of Benghazi presumably decreased their movements within the city due to security concerns giving rise to fewer motor vehicle accidents. This is supported by the fact that February and March [the peak period of active combat in Benghazi (7)] witnessed the lowest number of RTIs during the conflict period. Prominent events (i.e. dates) during the Libyan conflict were found to have influenced the admission rate of certain conditions [i.e. gunshot injuries (7), abortions (8), and preterm delivery(9)].
The average age of an RTI patient was found to have decreased significantly during the conflict. Presumably, younger people remained active outside their homes (as either pedestrians or drivers), whereas the older age group and women may well have been able to reduce exposure to violence by limiting their movements. Motorcycle injuries were also much more common during the war, further substantiating the notion that the increased presence of young people on the roads was an important factor behind the changes seen in RTIs during the conflict period.
Regardless of the presence/absence of armed conflict, the Department of Orthopedics followed by the Department of Neurosurgery were the two most common destinations for RTI patients in the hospital. Compared to the prewar period, more patients required the services of a neurosurgeon (10). An even more striking feature in 2011 was the sharp increase in ICU admissions, suggesting that while the absolute number of RTIs may have decreased, the severity of the cases had risen.
Hospital resources in Al-Jalaa hospital are limited, and ICU admission is reserved only for the severely injured. As long as the patient was not in a life-threatening situation, they would be managed within the departments or as outpatients. Therefore, ICU admission was used as an indicator of injury severity.
In addition to the increased ICU admission during the conflict, several other findings support the notion that more patients presented to the hospital with severe injuries. The outcomes of patients, notably fatalities, involved in an RTI worsened. Moreover, a greater proportion of the RTI cases presented as emergencies rather than as cold cases. Also, more RTI patients were being sent to Al-Jalaa hospital from the rural areas during the war. This would suggest that these injuries were too serious for the healthcare services in the smaller town/cities and required more advanced facilities in Benghazi.
A second potential explanation for increased rural contribution among the RTIs would be that in the absence of air transport (during the no-fly zone), more traffic went by road. Additionally, as customs services were largely absent during the conflict, large numbers of used vehicles (mostly unfit for usage) were imported which increased the availability of vehicles in the rural areas (as well as the conflict zones), leading to more RTIs in the more distant rural areas.
During the conflict period, it was common that RTI patients would simply abscond from the hospital after being treated. This might indicate either wrongful action during the accident or fear of retribution from any injured party. There was a sharp increase in the rate of same-day discharge. This could be explained by the hospital's need to increase its turnover rate to accommodate the increasing burden of war injuries.
At the start of the uprising, there was a mass exodus of foreign nationals from Libya towards neighboring countries. Even though some returned later on, as parts of the country began to stabilize, a significant number did not to return.
As the study is an interrupted time-series rather than a randomized clinical trial, certain caveats seem appropriate. Data quality in Libya and elsewhere in the developing world is not always optimal. However, this limitation (misclassification, undercounting) affects both years and should have little impact on comparisons. The conflict situation may have compounded this problem in that patient files were sometimes left unattended for days when the administrative staff could not come to the hospital for security reasons. The first 2 months of 2011 were included within the conflict period, even though the actual fighting had commenced in mid-February, due to the abnormal security conditions that were present in the run-up to the war (the Egyptian and Tunisian revolutions).
Conclusion
The conflict in Libya changed a number of features in the normal pattern of RTIs. Quantitatively, there were less RTIs; however, those that occurred were significantly worse and with higher morbidity and mortality rates. The profile of an RTI victim has also changed to reflect an increased prominence of young males and motorcyclists. Further research is required to analyze road safety during times of strife and possible interventions that could be implemented.
Conflict of interest and funding
The authors state that there were no conflicts of interest in this study and no financial support was provided.
References
- 1.Bodalal Z, Bendardaf R, Ambarek M. A study of a decade of road traffic accidents in Benghazi-Libya: 2001 to 2010. PLoS One. 2012;7:e40454. doi: 10.1371/journal.pone.0040454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hamza M. A study of road accidents, causalities and their injury patterns in Libya. Newcastle, UK: Newcastle University; 2005. [Google Scholar]
- 3.Mekky A. Road traffic accidents in rich developing countries: the case of Libya. Accid Anal Prev. 1984;16:263–77. [Google Scholar]
- 4.World Health Organization. Global status report on road safety: time for action; Geneva: World Health Organization; 2009. [Google Scholar]
- 5.Richter E. Fewer injuries but more deaths from road accidents during the Persian Gulf War. Isr J Med Sci. 1991;27:631–5. [PubMed] [Google Scholar]
- 6.Ðurić P, Peek-Asa C. Economic sanctions, military activity, and road traffic crashes in Vojvodina, Serbia. Inj Prev. 2008;14:372–6. doi: 10.1136/ip.2008.019240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bodalal Z, Mansor S. Gunshot injuries in Benghazi-Libya in 2011: the Libyan conflict and beyond. Surgeon. 2013;11:258–63. doi: 10.1016/j.surge.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Bodalal Z, Agnaeber K, editors. The effect of armed conflict on spontaneous abortions in Benghazi–Libya. 14th World Congress on Controversies in Obstetrics, Gynecology & Infertility (COGI); Paris, France. 2012. [Google Scholar]
- 9.Bodalal Z, Agnaeber K, Nagelkerke N, Stirling B, Temmerman M, Degomme O. Pregnancy outcomes in Benghazi – Libya, before and during the armed conflict in 2011. East Mediterr Health J. 2014;20:11–16. [PubMed] [Google Scholar]
- 10.Bodalal Z, Alzunni B. The trends of neurological trauma in a decade of road traffic accidents: 2001 to 2010. PanArab J Neurosurg. 2013;17:1–14. [Google Scholar]