Abstract
Purpose
To evaluate the outcomes of rigid ureterorenoscopy (URS) for renal pelvic stones (RPS) sized 1 to 2 cm and to determine the predictive factors for the requirement for flexible URS (F-URS) when rigid URS fails.
Materials and Methods
A total of 88 patients were included into the study. In 48 patients, the RPS were totally fragmented with rigid URS and F-URS was not required (group 1). In 40 patients, rigid URS was not able to access the renal pelvis or fragmentation of the stones was not completed owing to stone position or displacement and F-URS was utilized for retrograde intrarenal surgery (RIRS) (group 2). The predictive factors for F-URS requirement during RIRS for RPS were evaluated. Both groups were compared regarding age, height, sex, body mass index, stone size, stone opacity, hydronephrosis, and previous treatments.
Results
The mean patient age was 48.6±16.5 years and the mean follow-period was 39±11.5 weeks. The overall stone-free rate in the study population was 85% (75 patients). In groups 1 and 2, the overall stone-free rates were 83% (40 patients) and 87% (35 patients), respectively (p>0.05). The independent predictors of requirement for F-URS during RIRS were male gender, patient height, and higher degree of hydronephrosis.
Conclusions
Rigid URS can be utilized in selected patients for the fragmentation of RPS sized 1 to 2 cm with outcomes similar to that of F-URS. In case of failure of rigid URS, F-URS can be performed successfully in this group of patients.
Keywords: Kidney pelvis, Ureteroscopy, Urolithiasis
INTRODUCTION
Extracorporeal shock wave lithotripsy (ESWL) is established as the least invasive treatment option for the treatment of upper urinary tract stones. Previously, the European Association of Urology guidelines recommended ESWL as the first-line therapy for the treatment of renal calculi<20 mm [1]. However, with advancements in ureterorenoscopy (URS), improvements in deflection mechanisms, miniaturization of scopes, and the development of digital URS, flexible URS is also considered an acceptable option for these patients [2]. This improvement in technology may extend the indications of flexible URS to cases of ESWL-percutaneous lithotripsy (PNL) failure, obesity, and musculoskeletal deformity.
Although the current literature emphasizes flexible URS, rigid URS is still used for both distal and proximal ureteral stones. The existing literature has demonstrated rigid URS as a safe and effective treatment for proximal ureteral stones [3,4]. Although rigid URS is not used in renal stones owing to limited maneuverability and difficult access to middle and lower calyces, in some patients, rigid URS can be used to approach the kidney without any difficulty. The advantage of rigid URS in these patients is the larger working channel and thus larger working equipment. Additionally, better visualization can be obtained owing to higher irrigation flow.
In this study, we evaluated the outcomes of rigid URS for renal pelvic stones (RPS) sized 1 to 2 cm and determined the predictive factors for the requirement for flexible URS in patients in whom rigid URS failed.
MATERIALS AND METHODS
The clinical data of patients who underwent active intervention for treatment of RPS between January 2010 and December 2012 were reviewed, and patients with RPS of 1 to 2 cm in length and who underwent retrograde intrarenal surgery (RIRS) were included in the study. Ethical board approval was obtained for the study. Patients with caliceal stones, congenital anomalies, ureteropelvic junction obstruction, or ureteral strictures were excluded from the study.
Preoperative laboratory tests included urinalysis, serum creatinine, and complete blood count. Urinary ultrasonography was performed in all patients. For radiological investigation, intravenous urography or noncontrast computerized tomography was performed. Preoperatively, prophylactic intravenous antibiotics (cephazolin 1 g intravenously) were given to all patients. A course of antibiotics was continued in the postoperative period for 24 hours. RIRS was performed under general anesthesia.
Initially, patients were placed in a dorsal lithotomy position. The bladder was entered with a 22-Fr cystoscope and the ureter orifice was cannulated with an 0.038-mm guidewire through a balloon dilatator and the orifice was dilated (UroMax Ultra High Pressure Balloon Catheter, Boston Scientific, Marlborough, MA, USA). Before insertion of the ureteral sheath, URS was performed by use of a 9.5-Fr rigid URS to evaluate the presence of any stricture and to avoid any ureteral trauma related to blind insertion of the ureteral sheath. This may also mediate the dilation of the ureter and facilitate the passage of subsequent ureteral sheaths. The RPS accessed by use of rigid URS were fractured with a holmium-yttrium aluminium garnet laser with an energy setting of 0.6 to 0.8 J and a rate of 8 to 10 Hz if possible.
If renal pelvic access was not mediated, the stone could not be observed by rigid URS, or fragmentation of the stone was not completed owing to stone position or displacement, a ureteral sheath was placed over the previously inserted guidewire. A 7.5-Fr f lexible ureteroscope was passed into the upper urinary tract through the ureteral sheath (Karl Storz Endoscopy, Tuttlingen, Germany). The stone was fragmented with similar laser energy settings and f ibers. Following lithotripsy, a double-J stent was placed. Fragments smaller than 2 mm were left to pass and larger ones were retrieved. The double-J stent was removed at 1 month postoperatively, and stone status was evaluated at the end of the third month with ultrasonography and direct x-ray. Stone-free status was defined as no residual fragments.
In 48 patients, the RPS were totally fragmented with rigid URS and flexible URS was not required (group 1). In 40 patients, rigid URS could not access the renal pelvis or fragmentation of the stone was not completed owing to the stone position or displacement and flexible URS was used for RIRS (group 2). Age, height, sex, body mass index, stone size, stone opacity, hydronephrosis, and previous treatments were compared between the two groups.
Statistical analysis was done by using SPSS ver. 15 (SPSS Inc., Chicago, IL, USA). Categorical variables were compared with the chi-square test and continuous variables were compared with the t-test. We performed Cox regressıon analysis to detect predictors. A p-value less than 0.05 was considered statistically significant.
RESULTS
On retrospective analysis, there were 88 patients: 48 males and 40 females. The mean patient age was 48.6±16.5 years, and the mean follow-up time was 39±11 weeks. Patient and stone demographics are shown in Table 1. The mean stone size was 14.59±4.31 mm.
Table 1.
Comparison of the patients in groups 1 and 2
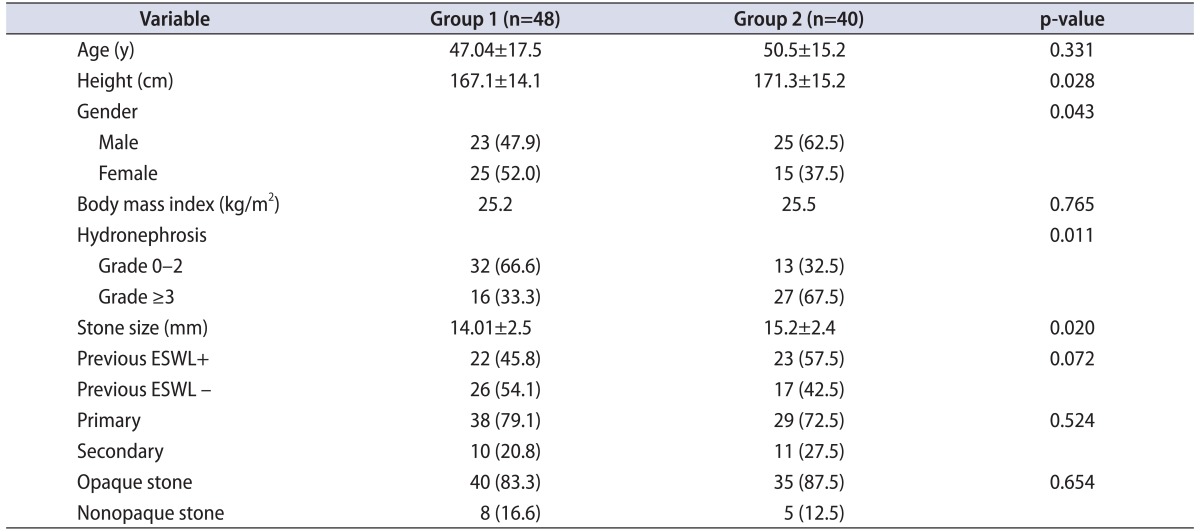
Values are presented as mean±standard deviation or number (%).
Group 1, renal pelvic stone (RPS) were totally fragmented with rigid ureteroscopy (URS); group 2, flexible URS was required to fragment the RPS; ESWL, extracorporeal shock wave lithotripsy.
The overall stone-free rate was 85% (75 patients) in the study population. In groups 1 and 2, the overall stone-free rates were 83% (40 patients) and 87% (35 patients), respectively. Three flexible URS and 2 ESWL procedures were performed as secondary procedures in group 1, and three ESWL procedures were performed as secondary procedures in group 2. After the secondary procedures, the stone-free rates were 89% and 92%, respectively. This difference was not statistically significant (p>0.05). Postoperatively, there were 3 minor complications. One patient in group 2 had significant bleeding and this resolved without any intervention and transfusion was not required. Two patients had postoperative fever >38℃ and intravenous antibiotics were given.
The comparison of groups 1 and 2 according to patient and stone characteristics is summarized in Table 2. The male-to-female ratio, patient length, degree of hydronephrosis, and mean stone size were significantly higher in group 2. The independent predictors for requirement of flexible URS during RIRS were male gender, patient height, and higher degree of hydronephrosis (Table 2).
Table 2.
Results of the multivariate analysis according to requirement for flexible URS during RIRS
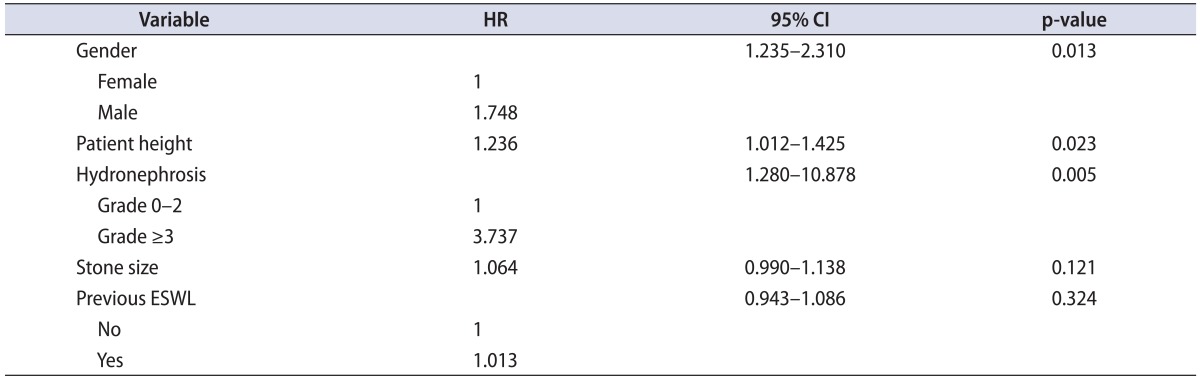
URS, ureteroscopy; RIRS, retrograde intrarenal surgery; HR, hazard ratio; CI, confidence interval; ESWL, extracorporeal shock wave lithotripsy.
DISCUSSION
Gradual technological advances have modified the management of upper urinary tract stones. Initially, PNL, ESWL, and URS reduced the role of open surgery in these patients. The introduction of ESWL in the early 1980s and developments in technique and equipment put ESWL at the top of the treatment algorithm. Although ESWL is still the first-line and established option for upper urinary tract stones sized <2 cm, the status of RIRS and PNL as primary treatment options is becoming more prominent [5]. PNL was developed as the standard procedure for large renal stones. Although PNL has high success rates, it is associated with an increased risk of complications such as renal parenchymal and adjacent organ injuries [6].
RIRS became possible because of constant technical improvements in flexible URS and intracorporeal lithotripsy. This advancement allows access and treatment of calculi in a single procedure and prevents PNL-related complications such as bleeding, visceral injury, and urine leakage. Especially, inserting an access sheath to ease the passing of a flexible ureteroscope and the use of a holmium laser to fragment the stone renders RIRS an outpatient procedure [7,8]. The high stone-free and low retreatment rates after flexible URS [9,10] seem to establish flexible URS as equivalent or superior to ESWL for treating renal stones <2 cm. The American Urological Association guidelines state that the stone-free rate is higher with flexible URS than with ESWL in patients with nonstaghorn renal stones. This difference increases with stones >1 cm; URS can achieve success rates of 86%, whereas SWL results in only 67% of patients being deemed stone-free [6].
Although flexible URS is a safe and efficacious method for the treatment of RPS, this treatment modality is not free from disadvantages. The small size of the working channels allows only the use of small stone extractors and laser f ibers, which may prolong the operation. Additionally, reduced irrigation during the operation may impair the surgeon's vision [11]. Access to a lower-pole stone and durability of the ureteroscopes are other disadvantages. The introduction of smaller sized ureteroscopes with larger working channels, greater active deflection angles, and smaller sized laser fibers (200 µm) has facilitated access of URS to the lower pole [12]. Although these technological advancements enhance the utility of flexible URS, the small size and complex construction of these devices makes them more fragile. Sung et al. [13] stated that long, small-diameter ureteroscopes have increased mobility and ease of passage and improved access to the collecting system; however, these same characteristics render these ureteroscopes more susceptible to damage. In the study by Sung et al. [13], laser burns and overbending the URS were the main reasons for damage to the scopes. Carey et al. [14] demonstrated a mean of 40 to 48 uses before the need for initial repair of a new flexible ureteroscope. After the initial repair, the mean average use was 11.1 before the ureteroscope needed repair again. Consequently, Carey et al. [14] recommended consideration of the cost-effectiveness of maintaining previously used ureteroscopes or purchasing a new flexible ureteroscope.
In our clinical practice, we routinely perform rigid URS before flexible URS. Although rigid URS is ideally suited for the distal ureter because of its ease of use and excellent control of working elements, with enhancements and modifications in design, rigid ureteroscopes are now suitable for use in the upper ureter and renal pelvis as well [15]. In our study, 55% of the patients were treated by use of rigid URS without the need for f lexible URS. In 45% of the patients, flexible URS was needed owing to a small ureter diameter, shortness of the rigid ureteroscope, or kinking of the ureter. Additionally, when renal pelvic access was obtained with rigid URS, flexible URS was used to complete the procedure in patients with inadequate stone fragmentation owing to restricted maneuverability. The stone-free rates were similar in both groups after URS and secondary procedures. In males, tall patients, and patients with severe hydronephrosis, flexible URS was required more often. The length and angle of the urethra are the main reasons for the difficult access of rigid URS in males [16]. Additionally, patient height may also correlate with ureter length, and the length of the rigid ureteroscope can be insufficient in tall patients. In patients with severe hydronephrosis, stone displacement or migration of large fragments to other calices during stone fragmentation were the main reasons for performing flexible URS. Rigid URS reached the renal pelvis, but flexible URS was performed owing to stone migration and inadequate fragmentation as a result of limited maneuverability in a total of eight patients in group 2. Six of these patients (75%) had a hydronephrosis degree ≥3. In a recent study, Atis et al. [17] compared the outcomes and patient characteristics of 47 patients. In that study, the investigators performed semirigid URS in all of the patients and the pelvic stones were fragmented in 25 of 47 patients. In 22 patients, flexible URS was required for treatment of the stone. Those authors compared both groups according to patient and clinical factors. Although the male-to-female ratio was higher in their flexible URS group, similar to our study, this difference was not statistically significant.
In this study, we did not aim to compare the outcomes of rigid and flexible URS for RPS. Additionally, we do not recommend rigid URS as an alternative to flexible URS. According to our results, rigid URS can be utilized in selected patients in whom flexible URS was intended. By this means, application of flexible URS can be decreased and the costs owing to repair and purchase of new flexible ureteroscopes can be reduced. Furthermore, starting the procedure with rigid URS and proceeding to flexible URS may decrease the use and increase the availability of the ureteroscope. However, we do not recommend performing rigid URS in patients with difficult upper urinary tract access. In patients with easy upper urinary tract access, rigid URS may present a good option with a better visualization and larger working channel. According to the outcomes of our study, rigid URS is more reasonable in short female patients without severe hydronephrosis.
The main limitation of our study was its retrospective nature. We did not calculate the costs in the patients in order to obtain a cost-effectiveness evaluation. The lack of data on operative time is another limitation as an operative outcome. We did not use computed tomography as a follow-up modality to reduce the patients' exposure to radiation, which may have caused us to miss some residual stones.
CONCLUSIONS
Flexible URS and laser lithotripsy are first-line treatment options in patients with RPS. Although rigid URS is mostly used for ureteral stones, fragmentation of RPS can be achieved in selected patients. In the case of rigid URS failure, flexible URS can be successfully performed in these patients.
Footnotes
The authors have nothing to disclose.
References
- 1.Turk C, Knoll T, Petrik A, Sarica K, Skolarikos A, Straub M, et al. Guidelines on urolithiasis. Arnhem (NL): European Association of Urology; 2015. [Google Scholar]
- 2.Busby JE, Low RK. Ureteroscopic treatment of renal calculi. Urol Clin North Am. 2004;31:89–98. doi: 10.1016/S0094-0143(03)00097-1. [DOI] [PubMed] [Google Scholar]
- 3.Karlsen SJ, Renkel J, Tahir AR, Angelsen A, Diep LM. Extracorporeal shockwave lithotripsy versus ureteroscopy for 5- to 10-mm stones in the proximal ureter: Prospective effectiveness patient-preference trial. J Endourol. 2007;21:28–33. doi: 10.1089/end.2006.0153. [DOI] [PubMed] [Google Scholar]
- 4.Kumar A, Nanda B, Kumar N, Kumar R, Vasudeva P, Mohanty NK. A prospective randomized comparison between shockwave lithotripsy and semirigid ureteroscopy for upper ureteral stones <2 cm: a single center experience. J Endourol. 2015;29:47–51. doi: 10.1089/end.2012.0493. [DOI] [PubMed] [Google Scholar]
- 5.Wen CC, Nakada SY. Treatment selection and outcomes: renal calculi. Urol Clin North Am. 2007;34:409–419. doi: 10.1016/j.ucl.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 6.Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, et al. 2007 guideline for the management of ureteral calculi. J Urol. 2007;178:2418–2434. doi: 10.1016/j.juro.2007.09.107. [DOI] [PubMed] [Google Scholar]
- 7.Kourambas J, Byrne RR, Preminger GM. Does a ureteral access sheath facilitate ureteroscopy? J Urol. 2001;165:789–793. [PubMed] [Google Scholar]
- 8.Gupta PK. Is the holmium:YAG laser the best intracorporeal lithotripter for the ureter? A 3-year retrospective study. J Endourol. 2007;21:305–309. doi: 10.1089/end.2006.0247. [DOI] [PubMed] [Google Scholar]
- 9.El-Nahas AR, Ibrahim HM, Youssef RF, Sheir KZ. Flexible ureterorenoscopy versus extracorporeal shock wave lithotripsy for treatment of lower pole stones of 10-20 mm. BJU Int. 2012;110:898–902. doi: 10.1111/j.1464-410X.2012.10961.x. [DOI] [PubMed] [Google Scholar]
- 10.Fabrizio MD, Behari A, Bagley DH. Ureteroscopic management of intrarenal calculi. J Urol. 1998;159:1139–1143. [PubMed] [Google Scholar]
- 11.Miernik A, Schoenthaler M, Wilhelm K, Wetterauer U, Zyczkowski M, Paradysz A, et al. Combined semirigid and flexible ureterorenoscopy via a large ureteral access sheath for kidney stones >2 cm: a bicentric prospective assessment. World J Urol. 2014;32:697–702. doi: 10.1007/s00345-013-1126-z. [DOI] [PubMed] [Google Scholar]
- 12.Bagley DH. Ureteroscopic surgery: changing times and perspectives. Urol Clin North Am. 2004;31:1–4. doi: 10.1016/S0094-0143(03)00088-0. [DOI] [PubMed] [Google Scholar]
- 13.Sung JC, Springhart WP, Marguet CG, L'Esperance JO, Tan YH, Albala DM, et al. Location and etiology of flexible and semirigid ureteroscope damage. Urology. 2005;66:958–963. doi: 10.1016/j.urology.2005.05.033. [DOI] [PubMed] [Google Scholar]
- 14.Carey RI, Gomez CS, Maurici G, Lynne CM, Leveillee RJ, Bird VG. Frequency of ureteroscope damage seen at a tertiary care center. J Urol. 2006;176:607–610. doi: 10.1016/j.juro.2006.03.059. [DOI] [PubMed] [Google Scholar]
- 15.Basillote JB, Lee DI, Eichel L, Clayman RV. Ureteroscopes: flexible, rigid, and semirigid. Urol Clin North Am. 2004;31:21–32. doi: 10.1016/S0094-0143(03)00094-6. [DOI] [PubMed] [Google Scholar]
- 16.Khairy-Salem H, el-Ghoneimy M, el-Atrebi M. Semirigid ureteroscopy in management of large proximal ureteral calculi: is there still a role in developing countries? Urology. 2011;77:1064–1068. doi: 10.1016/j.urology.2010.08.067. [DOI] [PubMed] [Google Scholar]
- 17.Atis G, Gurbuz C, Arikan O, Canat L, Kilic M, Caskurlu T. Ureteroscopic management with laser lithotripsy of renal pelvic stones. J Endourol. 2012;26:983–987. doi: 10.1089/end.2011.0664. [DOI] [PubMed] [Google Scholar]


