Abstract
Purpose
To determine effectiveness of Valsalva maneuver and standing position on scrotal color Doppler ultrasound (CDU) for the varicocele diagnosis.
Materials and Methods
We reviewed the physical examination and CDU finding in 87 patients who visited National Police Hospital from January 2011 to April 2014. Diameters of pampiniform plexus were measured bilaterally during resting and Valsalva maneuver in the supine position and standing position. We calculated the ratio of mean of maximal vein diameter (mMVD) during resting and Valsalva maneuver (resting-Valsalva ratio) and compared in the both position.
Results
In the resting and supine position, mMVD of varicocele testis units were 1.8 mm, 2.1 mm, 2.6 mm (grades I, II, III, respectively), and that of normal testis units (NTU) 1.2 mm. During Valsalva maneuver in the supine position, mMVD were 3.0 mm, 3.4 mm, 4.2 mm (grades I, II, III) vs 1.8 mm (NTU) (p=0.007, p<0.001, p<0.001, respectively). Average of resting-Valsalva ratio in the supine position were 0.69, 0.74, 0.74 (grades I, II, III) and 0.67 (NTU). Whereas in the resting and standing position, mMVD were 2.8 mm, 3.3 mm, 3.8 mm (grades I, II, III) and 1.8 mm (NTU) (p=0.002, p<0.001, p<0.001). During Valsalva maneuver in the standing position, mMVD were 5.0 mm, 5.8 mm, 6.6 mm (grades I, II, III) and 2.5 mm (NTU) (p=0.002, p<0.001, p<0.001). And average resting-Valsalva ratio were 0.76, 0.90, 0.71 (grades I, II, III) and 0.26 (NTU), which showed significant differences from all grades (p<0.001, p<0.001, p<0.001).
Conclusions
It is suggested that the standing position and Valsalva maneuver during CDU could improve diagnostic ability for varicocele. Resting-Valsalva ratio in the standing position could be a new diagnostic index for varicocele diagnosis using CDU.
Keywords: Doppler ultrasonography, Valsalva maneuver, Varicocele
INTRODUCTION
Varicocele is characterized by retrograde flow in testicular veins pathophysiologically and is manifested clinically by abnormal tortuosity and dilatation of the spermatic veins and pampiniform plexus [1,2,3]. It affects 15% of the general population and is especially common among teenagers and young adults [4]. The clinical relevance of varicocele is based on its symptoms being related to scrotal venous stasis and the potential association with male infertility [5]. Physical examination is still the standard diagnostic method for varicocele, but it is usually difficult to estimate the existence of varicocele by use of physical examination alone. Some varicoceles are impalpable and asymptomatic and are diagnosed only with ultrasound evaluation owing to thick scrotal skin and a strong cremasteric reflex [6,7]. Several authors have examined groups of patients with a diagnosis of varicocele to establish qualitative and quantitative color Doppler ultrasonography (CDU) criteria [6,8,9,10,11,12,13,14,15], but the criteria were heterogeneous and poorly defined from a quantitative point of view. Furthermore, physical examination for diagnosis of varicocele is generally performed with the patient in the standing position, but some studies examined CDU for patients in the supine position [6,10,12,15] and some studies did so for patients in the standing position [8,9,11,13,14].
In this study, we proposed to assess the effectiveness of the Valsalva maneuver and the standing position on CDU for varicocele diagnosis and to devise a new index that can improve existing diagnostic criteria of CDU for varicocele.
MATERIALS AND METHODS
We reviewed the findings of a physical examination and CDU for 87 patients who visited National Police Hospital for varicocelectomy with complaints of scrotal pain, painful swelling, or infertility and were clinically diagnosed with varicocele from January 2011 to April 2014. After obtaining approval from the Institutional Review Board (IRB) of National Police Hospital, we retrospectively reviewed the imaging findings and clinical records (IRB approval No. 116222-201409-HR-006). None of the patients had a previous history of genitourinary trauma or surgery. The age of the patients ranged from 19 to 65 years (mean age, 22.34±3.86 years).
Patients were examined in a warm room after standing for 5 minutes and varicocele was graded by physical examination in a standing position according to the system of Dubin and Amelar as follows: grade I, palpable only with Valsalva maneuver; grade II, palpable without the Valsalva maneuver; and grade III, visible from a distance [16].
All CDU studies were performed by three experienced physicians using the same equipment (7.5-Mhz electronic linear probe, Prosound alpha5 SV, Aloca Co., Tokyo, Japan). We placed the transducer transversely on the bilateral scrotal surface with the patients in a supine position with the abdomen and chest elevated to about 15°, followed by the same measurement with the patient in a standing position. Diameters of the largest vein in the pampiniform plexus were measured bilaterally during resting and during a Valsalva maneuver in the supine position followed by same examination with the subjects standing (Fig. 1). We calculated the ratio of mean maximal vein diameter (mMVD) during resting to that during the Valsalva maneuver (resting-Valsalva ratio), and the ratios were compared between the two positions (Fig. 1).
Fig. 1.
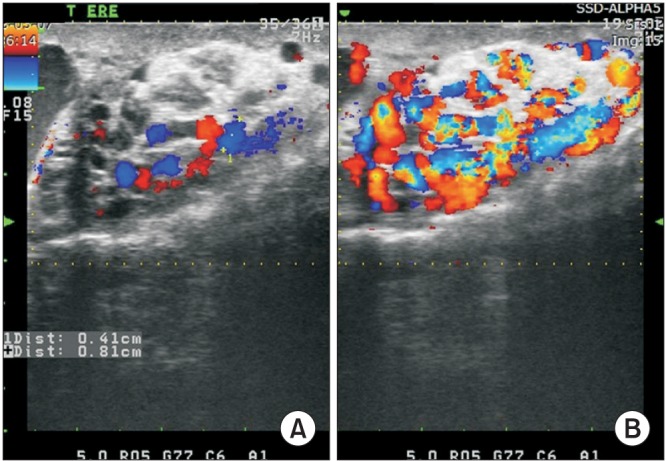
Color Doppler ultrasonography of varicocele. Maximal venous diameters in the pampiniform plexus were measured during resting (A) and during a Valsalva maneuver (B) in the standing position.
The data were analyzed by using the t-test with a personal computer and the SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA). We compared the mMVD of normal testis units versus that of grades I, II, and III varicocele testis units and the mMVD of each varicocele unit in the supine position during rest and during the Valsalva maneuver, followed by the same comparisons in the standing position. Resting-Valsalva ratios were compared in both positions in the same way. A two-tailed p-value less than 0.05 was considered to be statistically significant.
RESULTS
Of a total 87 patients, 76 patients had left varicoceles and 11 patients had bilateral varicoceles upon physical examination. Among the 76 patients with left unilateral varicocele, 7 patients had grade I (9%), 40 patients had grade II (53%), and 29 patients had grade III (38%) on physical examination, respectively. The 11 patients with bilateral varicoceles were identified as follows: 2 patients with grade II (18%) and 9 patients with grade III (82%; right grade I, 7; grade II, 3; grade III, 1). Among the physical parameters of the 174 testis units in 87 patients, 77 testis units were normal testis units with no varicocele (44%), 13 units were grade I (7%), 45 units were grade II (26%), and 39 units were grade III (22%), respectively.
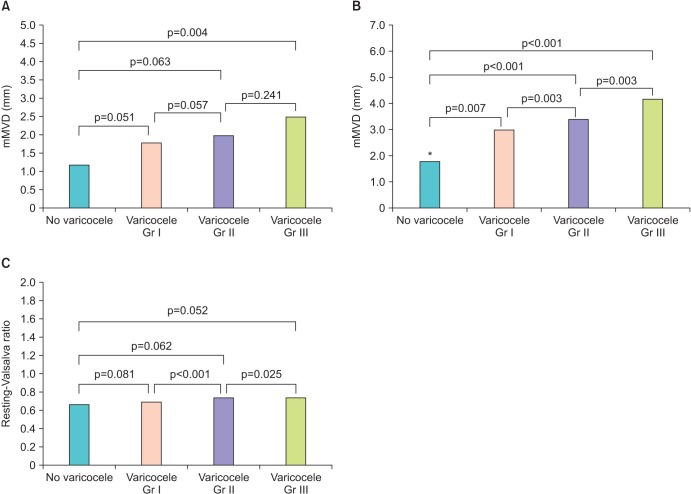
By use of scrotal CDU in the supine position at rest, the mMVD of varicocele testis units was 1.8 mm (grade I), 2.0 mm (grade II), and 2.5 mm (grade III), respectively, and that of normal testis units was 1.2 mm. Compared with normal testis units, only grade III varicoceles showed a significant difference (p=0.004). In the supine position during the Valsalva maneuver, mMVD was 3.0 mm (grade I), 3.4 mm (grade II), and 4.2 mm (grade III) and that of normal testis units was 1.8 mm (p=0.007, p<0.001, p<0.001, respectively). The average resting-Valsalva ratio in the supine position was 0.69, 0.74, and 0.74 for grades I, II, and III, respectively, and 0.67 for normal testis units. There were no significant differences between the normal and varicocele unit groups (Fig. 2).
Fig. 2.
(A) Mean maximal vein diameter (mMVD) of varicocele testis units upon scrotal color Doppler ultrasonography in the supine position at rest. (B) mMVD of varicocele testis units upon scrotal color Doppler ultrasonography in the supine positing during a Valsalva maneuver. (C) Average resting-Valsalva ratio [=(mMVD during Valsalva-mMVD during resting)/mMVD during resting] in the supine position. Gr, grade. *mMVD of no varicocele units (mm)=1.8±0.9.
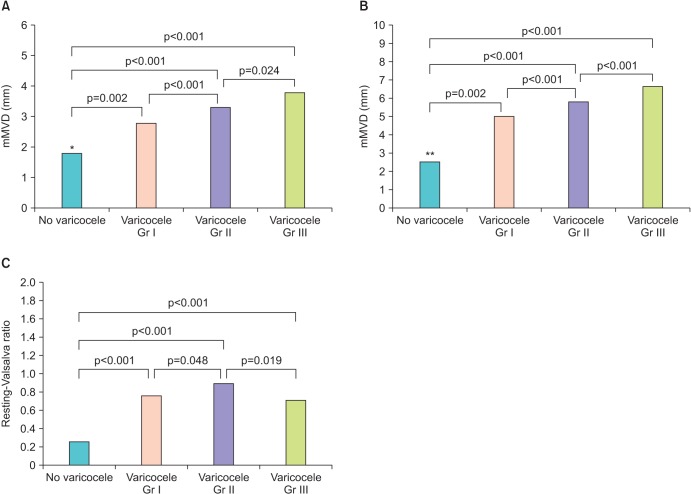
In the standing position at rest, mMVD was 2.8 mm, 3.3 mm, and 3.8 mm for grades I, II, and III, respectively, and 1.8 mm for normal testis units (p=0.002, p<0.001, p<0.001, respectively). In the standing position during a Valsalva maneuver, mMVD was 5.0 mm, 5.8 mm, and 6.6 mm for grades I, II, and III, respectively, and 2.5 mm for normal testis units (p=0.002, p<0.001, p<0.001, respectively). Average resting-Valsalva ratios were 0.76, 0.90, and 0.71 for grades I, II, and III, respectively, and 0.26 for normal testis units, which showed a significant difference for all grades (p<0.001, p<0.001, p<0.001, respectively) (Fig. 3).
Fig. 3.
(A) Mean maximal vein diameter (mMVD) of varicocele testis units upon scrotal color Doppler ultrasonography in the standing position at rest. (B) mMVD of varicocele testis units upon scrotal color Doppler ultrasonography in the standing position during a Valsalva maneuver. (C) Average resting-Valsalva ratio in the standing position. Gr, grade. *mMVD of no varicocele units (mm)=1.8±1.2. **mMVD of no varicocele units (mm)=2.5±0.3.
DISCUSSION
Varicocele is an abnormal degree of venous dilatation in the pampiniform plexus due to reflux of blood resulting from the absence or incompetency of the valves within the spermatic vein [17,18]. Clinical suspicion of a varicocele depends on the expertise of the evaluating physician. Physical examination is the standard diagnostic method for clinical varicocele. However, clinical examination is subjective, may be associated with significant interphysician variability, and has a limited capacity to detect blood flow changes. Furthermore, physical examination alone may be inadequate to diagnose small or subclinical varicoceles, which are also considered to have significant pathophysiological potential. Testicular venography is the most reliable method for the detection of small varicoceles, but it has several disadvantages including a morbidity rate of 0.5% to 1.0% owing to contrast medium injection, high cost, and inappropriateness for routine use because it is limited to embolization procedures [19].
Ultrasound technology has improved considerably in recent years. At present it allows the identification of minimal ectasia of the scrotal veins and minimal retrograde venous flow. Ultrasonography and particularly CDU appear to be the most reliable and practical methods for diagnosing subclinical varicocele. A widely accepted ultrasound criterion for diagnosis of varicocele is the existence of veins larger than 2 mm in diameter [3,10,20]. Gonda et al. [10] reported 95% sensitivity with a 2-mm cutoff for vein diameters. In a recent study, Lee et al. [21] reviewed previous studies and insisted that multiple veins >3.0 to 3.5 mm with concomitant reversal of flow after Valsalva maneuver is the most widely used criteria for diagnosing a varicocele on CDU. Nonetheless, they described that there is no clear-cut standardized size criterion, which may be not only a result of the lack of proper prospective trials, but also a manifestation of a spectrum phenomenon in which there is no clear discrete normal value. Caskurlu et al. [22] used CDU to analyze the diameter of the veins in the pampiniform plexus in patients with clinical or subclinical varicocele and in controls. Those authors suggested that venous diameter should not be used as a diagnostic criterion in patients without clinical signs of varicocele, but rather should be used to document and quantify pathology in patients with clinical varicocele [22].
CDU can be used to measure the size of the pampiniform plexus and blood flow parameters of the spermatic vein. However, the reliability of CDU to diagnose varicoceles remains controversial and the diagnostic criteria remain poorly def ined, with considerable variation between investigators. Reflux is an important criterion for the diagnosis of varicocele. The change in color is subjective and unreliable for the diagnosis of reflux in CDU examination and should be quantified with spectral Doppler analysis.
Varicocele may be diagnosed more reliably by quantifying the duration of reflux in spectral analysis. Studies have quantitatively classified the reflux in varicocele patients. A study by Kocakoc et al. [23] reported a 62.3% incidence of reflux in testicular veins with a diameter <3 mm. However, their measures were obtained only in the supine position. A new scoring system to improve CDU criteria to diagnose scrotal varicocele was proposed by Chiou et al. [15] by incorporating the maximal venous diameter, the presence of a venous plexus, the sum of diameters of veins in the plexus, and the change in flow on Valsalva maneuver. However, the clinical impact and reproducibility of this score must still be demonstrated.
An attempt to identify new criteria for the CDU diagnosis of subclinical varicocele was performed by Mihmanli et al. [24], although these criteria have not provided new information on the diagnosis of subclinical varicocele in infertile patients.
Cina et al. [5] reported that a scrotal diameter of up to 3.7 mm and a reflux lasting up to 3 seconds with a velocity of 0.1 m/s can be observed in healthy subjects and should not be interpreted as a certain sign of scrotal varicocele. Also, physical examination alone is not a highly reliable tool in the diagnosis of varicocele, and the use of venography is inappropriate for routine screening. Moreover, Cina et al. [5] insisted that a gold standard for detecting subclinical varicocele does not exist.
As enumerated above, CDU is a useful modality for scrotal varicocele diagnosis and has many merits, such as being a real-time, noninvasive, and relatively inexpensive technique. However, limitations do exist. We considered supplementing the varicocele diagnosis index by using CDU, with a focus on dilation of the pampiniform plexus in the standing position during a Valsalva maneuver.
In our study, in the supine position at rest, only mMVD of grade III varicocele testis units showed a significant difference with normal testis units. In the supine position during the Valsalva maneuver, all grades of varicocele testis units showed significant differences with normal testis units. This suggests that the Valsalva maneuver results in dilation of the pampiniform plexus in all grades of varicocele. However, the average resting-Valsalva ratio in the supine position had no significant meaning.
In the standing position, whether during rest or during the Valsalva maneuver, all grades of varicocele testis units showed significant differences with normal testis units. Also, the average resting-Valsalva ratio showed significant differences for all grades. This suggests that the detection of varicocele is more precise in the standing position, and the Valsalva maneuver has a greater role in dilation of the pampiniform plexus in the standing position than in the supine position. The resting-Valsalva ratio of normal testis units showed significant differences with the ratio of testis units of each grade of varicocele in the standing position. It seems that in the standing position, the Valsalva maneuver contributes to the dilatory effectiveness of the pampiniform plexus, thus increasing the resting-Valsalva ratio.
In this study, mMVD values of varicocele testis units were greater than and differed significantly from the values for normal testis units when the patients performed the Valsalva maneuver or were in the standing position. This finding suggests that only the standing position or Valsalva maneuver can distinguish between normal testis units and Varicocele testis units. However, the mMVDs of normal testis units during the Valsalva maneuver in the supine position and during resting and the Valsalva maneuver in the standing position were 1.8±0.9 mm, 1.8±1.2 mm, and 2.5±0.3 mm, respectively. Compared with the conventional cutoff value of varicocele diagnosis by mMVD, 2 mm [3,10,20], the mMVD of normal testis units was too close to the cutoff value. Thus, it is hard to differentiate between normal and varicocele testis units by use of mMVD. Using the cutoff value of mMVD >3 mm, when the mMVD of normal testis units by physical examination is over 3 mm, the resting-Valsalva ratio can help in the discrimination of varicocele. The resting-Valsalva ratio in the supine position does not discriminate significantly but in the standing position can be a useful diagnostic index for detecting varicocele and grading.
Several limitations of this study warrant mentioning. First, normal testis units were classified from varicocele patients by physical examination instead of in a normal population with no varicocele. Second, CDU and the resting-Valsalva ratio were not compared with the use of another varicocele diagnostic modality. In addition, this study did not give a concrete cutoff value of the resting-Valsalva ratio for varicocele diagnosis. Thus, further studies correlating CDU to assess the cutoff values of the resting-Valsalva ratio are needed and reproducibility should be verified by other studies.
CONCLUSIONS
CDU is a useful modality for scrotal varicocele diagnosis but limitations do exist. The detection of varicocele is more precise with the patient in the standing position, and the Valsalva maneuver has a greater role in dilation of the pampiniform plexus in the standing position than in the supine position. The resting-Valsalva ratio in the standing position could be a new and ancillary diagnostic index for varicocele diagnosis by use of scrotal CDU.
Footnotes
The authors have nothing to disclose.
References
- 1.Sigmund G, Gall H, Bahren W. Stop-type and shunt-type varicoceles: venographic findings. Radiology. 1987;163:105–110. doi: 10.1148/radiology.163.1.3547489. [DOI] [PubMed] [Google Scholar]
- 2.Cornud F, Belin X, Amar E, Delafontaine D, Helenon O, Moreau JF. Varicocele: strategies in diagnosis and treatment. Eur Radiol. 1999;9:536–545. doi: 10.1007/s003300050706. [DOI] [PubMed] [Google Scholar]
- 3.Arslan H, Sakarya ME, Atilla MK. Clinical value of power Doppler sonography in the diagnosis of varicocele. J Clin Ultrasound. 1998;26:229. doi: 10.1002/(sici)1097-0096(199805)26:4<229::aid-jcu13>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 4.Greenberg SH. Varicocele and male fertility. Fertil Steril. 1977;28:699–706. doi: 10.1016/s0015-0282(16)42669-5. [DOI] [PubMed] [Google Scholar]
- 5.Cina A, Minnetti M, Pirronti T, Vittoria Spampinato M, Canade A, Oliva G, et al. Sonographic quantitative evaluation of scrotal veins in healthy subjects: normative values and implications for the diagnosis of varicocele. Eur Urol. 2006;50:345–350. doi: 10.1016/j.eururo.2006.02.055. [DOI] [PubMed] [Google Scholar]
- 6.Kocakoc E, Serhatlioglu S, Kiris A, Bozgeyik Z, Ozdemir H, Bodakci MN. Color Doppler sonographic evaluation of interrelations between diameter, reflux and flow volume of testicular veins in varicocele. Eur J Radiol. 2003;47:251–256. doi: 10.1016/s0720-048x(02)00182-1. [DOI] [PubMed] [Google Scholar]
- 7.Kim WS, Choi DY, Han YT. Scrotal Doppler ultrasonography in the assessment of varicocele. Korean J Urol. 1998;39:1070–1076. [Google Scholar]
- 8.Wolverson MK, Houttuin E, Heiberg E, Sundaram M, Gregory J. High-resolution real-time sonography of scrotal varicocele. AJR Am J Roentgenol. 1983;141:775–779. doi: 10.2214/ajr.141.4.775. [DOI] [PubMed] [Google Scholar]
- 9.Rifkin MD, Foy PM, Kurtz AB, Pasto ME, Goldberg BB. The role of diagnostic ultrasonography in varicocele evaluation. J Ultrasound Med. 1983;2:271–275. doi: 10.7863/jum.1983.2.6.271. [DOI] [PubMed] [Google Scholar]
- 10.Gonda RL, Jr, Karo JJ, Forte RA, O'Donnell KT. Diagnosis of subclinical varicocele in infertility. AJR Am J Roentgenol. 1987;148:71–75. doi: 10.2214/ajr.148.1.71. [DOI] [PubMed] [Google Scholar]
- 11.Orda R, Sayfan J, Manor H, Witz E, Sofer Y. Diagnosis of varicocele and postoperative evaluation using inguinal ultrasonography. Ann Surg. 1987;206:99–101. doi: 10.1097/00000658-198707000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nashan D, Behre HM, Grunert JH, Nieschlag E. Diagnostic value of scrotal sonography in infertile men: report on 658 cases. Andrologia. 1990;22:387–395. doi: 10.1111/j.1439-0272.1990.tb02013.x. [DOI] [PubMed] [Google Scholar]
- 13.Eskew LA, Watson NE, Wolfman N, Bechtold R, Scharling E, Jarow JP. Ultrasonographic diagnosis of varicoceles. Fertil Steril. 1993;60:693–697. doi: 10.1016/s0015-0282(16)56224-4. [DOI] [PubMed] [Google Scholar]
- 14.Hoekstra T, Witt MA. The correlation of internal spermatic vein palpability with ultrasonographic diameter and reversal of venous flow. J Urol. 1995;153:82–84. doi: 10.1097/00005392-199501000-00029. [DOI] [PubMed] [Google Scholar]
- 15.Chiou RK, Anderson JC, Wobig RK, Rosinsky DE, Matamoros A, Jr, Chen WS, et al. Color Doppler ultrasound criteria to diagnose varicoceles: correlation of a new scoring system with physical examination. Urology. 1997;50:953–956. doi: 10.1016/S0090-4295(97)00452-4. [DOI] [PubMed] [Google Scholar]
- 16.Dubin L, Amelar RD. Varicocele size and results of varicocelectomy in selected subfertile men with varicocele. Fertil Steril. 1970;21:606–609. doi: 10.1016/s0015-0282(16)37684-1. [DOI] [PubMed] [Google Scholar]
- 17.Kim SW. Varicocele and male infertility. J Korean Med Assoc. 2012;55:37–46. [Google Scholar]
- 18.Beddy P, Geoghegan T, Browne RF, Torreggiani WC. Testicular varicoceles. Clin Radiol. 2005;60:1248–1255. doi: 10.1016/j.crad.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 19.Gat Y, Bachar GN, Zukerman Z, Belenky A, Gorenish M. Physical examination may miss the diagnosis of bilateral varicocele: a comparative study of 4 diagnostic modalities. J Urol. 2004;172(4 Pt 1):1414–1417. doi: 10.1097/01.ju.0000138540.57137.5f. [DOI] [PubMed] [Google Scholar]
- 20.Aydos K, Baltaci S, Salih M, Anafarta K, Beduk Y, Gulsoy U. Use of color Doppler sonography in the evaluation of varicoceles. Eur Urol. 1993;24:221–225. doi: 10.1159/000474298. [DOI] [PubMed] [Google Scholar]
- 21.Lee J, Binsaleh S, Lo K, Jarvi K. Varicoceles: the diagnostic dilemma. J Androl. 2008;29:143–146. doi: 10.2164/jandrol.107.003467. [DOI] [PubMed] [Google Scholar]
- 22.Caskurlu T, Tasci AI, Resim S, Sahinkanat T, Ekerbicer H. Reliability of venous diameter in the diagnosis of subclinical varicocele. Urol Int. 2003;71:83–86. doi: 10.1159/000071100. [DOI] [PubMed] [Google Scholar]
- 23.Kocakoc E, Kiris A, Orhan I, Bozgeyik Z, Kanbay M, Ogur E. Incidence and importance of reflux in testicular veins of healthy men evaluated with color duplex sonography. J Clin Ultrasound. 2002;30:282–287. doi: 10.1002/jcu.10068. [DOI] [PubMed] [Google Scholar]
- 24.Mihmanli I, Kurugoglu S, Cantasdemir M, Zulfikar Z, Halit Yilmaz M, Numan F. Color Doppler ultrasound in subclinical varicocele: an attempt to determine new criteria. Eur J Ultrasound. 2000;12:43–48. doi: 10.1016/s0929-8266(00)00102-6. [DOI] [PubMed] [Google Scholar]