Abstract
AIM
To assess the outcomes of combined 23-gauge sutureless vitrectomy and clear corneal phacoemulsification with intraocular lens implantation for rhegmatogenous retinal detachment (RRD) repair.
METHODS
This was a retrospective, consecutive, non-comparative, interventional case series of 30 eyes of 30 patients who underwent combined sutureless vitrectomy and clear corneal cataract surgery for the repair of RRD. The principal outcome measures were primary anatomical success rate, reasons for redetachment, final visual acuity, and surgical complications.
RESULTS
Primary reattachment was achieved in 27 eyes (90.0%). The reasons for redetachment (3 eyes, 10%) were incomplete laser retinopexy, persistent chronic subretinal fluid, and proliferative vitreoretinopathy, respectively. The logarithm of the minimum angle of resolution visual acuity (mean±SD) improved from 0.76±0.74 preoperatively to 0.21±0.37 6 months' postoperatively (P<0.0001). Postoperative hypotony was not detected, but 1 eye (3.3%) had increased intraocular pressure (30mmHg) with spontaneous resolution. No endophthalmitis developed during follow-up. Macular pucker was detected in 3 eyes (10.0%).
CONCLUSION
Combined 23-gauge sutureless vitrectomy and clear corneal phacoemulsification with intraocular lens implantation for RRD repair was proven safe and effective. It may provide not only the known advantages of conventional combined surgery, but also additional advantages such as less conjunctival fibrosis and the maintenance of stable intraocular pressure with low risks of postoperative hypotony and intraocular pressure elevation.
Keywords: clear corneal phacoemulsification, combined 23-guage sutureless vitrectomy, rhegmatogenous retinal detachment
INTRODUCTION
Transconjunctival 25- or 23-gauge sutureless vitrectomy has been popularized for pars plana vitrectomy as minimally invasive vitreoretinal surgery [1]–[3]. Recent studies have demonstrated that 25- or 23-gauge vitrectomy is a feasible treatment for rhegmatogenous retinal detachment (RRD) and compares favorably with conventional 20-gauge vitrectomy[4]–[8]. Additionally, it may offer the advantages of a sutureless approach such as faster visual rehabilitation, less conjunctival fibrosis, and enhanced patient comfort.
With the advent of modern instrumentation and surgical techniques, combined cataract, and vitreoretinal surgery has increased in popularity in recent years[9]–[13]. Especially in the management of primary RRD, the combined surgery offers advantages to both the patient and the surgeon such as reduced cost, immediate visual recovery, avoiding the need for cataract surgery in the vitrectomized eye, good access to the vitreous base, and more complete vitrectomy[14]. Therefore, a more thorough vitreous shaving and a larger gas fill in pseudophakic eyes as compared to phakic eyes may result in superior anatomic and functional outcomes.
Although the combined surgery technique is being increasingly accepted as an effective and safe procedure in selected patients with RRD[5],[14] and clear corneal phacoemulsification has become a common approach for cataract surgery, there have been few reports regarding the results and complications of combined transconjunctival sutureless vitrectomy and clear corneal cataract surgery in patients with RRD. Herein, we present the outcomes of combined 23-gauge sutureless vitrectomy and clear corneal phacoemulsification with intraocular lens implantation for RRD and visually significant cataract.
SUBJECTS AND METHODS
Subjects
This was a retrospective, consecutive, non-comparative, interventional case series of consecutive patients who underwent combined 23-gauge sutureless vitrectomy and clear corneal cataract surgery for the repair of RRD. All cases were patients with both primary RRD and lens opacity, and all patients were informed of the option of vitrectomy or scleral buckling for the repair of RRD. Exclusion criteria were any previous intraocular surgery including vitrectomy and proliferative vitreoretinopathy grade C or worse. From March 2009 to February 2011, the combined surgery was carried out on 30 eyes of 30 patients. All procedures were conducted by a single physician (D.H.N.). The follow-up period was at least 6mo.
Surgical Procedure
Almost all patients underwent general anesthesia, although retrobulbar anesthesia was applied in some cases. An AMO Sovereign cataract surgical system (AMO, USA) and a DORC Associate 2500 vitrectomy system (DORC, Zuidland, Netherlands) were used. The procedure was initiated with conjunctival displacement, an oblique beveled scleral wound and insertion of the microcannulas (DORC, Zuidland, Netherlands) as described by Eckardt[3]. A 3.0-mm clear corneal wounds for cataract surgery were created at the 10-o'clock position and capsulorhexis of the anterior capsule was conducted. After phacoemulsification and the implantation of a hydrophobic acrylic lens (Tecnis®, AMO, USA), balanced salt solution mixed with 1:100 000 epinephrine was intracamerally injected to maintain the pupil dilatation. To prevent anterior chamber collapse during the vitreoretinal procedures, the clear corneal wound was sutured using 10-0 nylon. The suture was removed 7d postoperatively.
A hand-held light probe and the noncontact wide-angle viewing system (BIOM 3, Oculus, Wetzlar, Germany) was utilized to achieve visualization during vitrectomy. Complete removal of the posterior vitreous and extensive shaving of the vitreous base under scleral indentation was routinely performed. Scleral depression was performed by an assistant to relieve traction and to shave the peripheral vitreous thoroughly. Care was taken to remove any vitreous traction on both retinal breaks and the vitreous base. In intraocular pressure (IOL)-implanted eyes after cataract surgery, lens opacities did not impair the operative window and limit access to the peripheral retina and anterior vitreous. Therefore, there was no need to bend or change the 23-gauge instruments during the vitreous base shaving procedure.
Retinal breaks were marked with endodiathermy to make localization easy after a fluid-air exchange. The surgeon preferred to create a new retinotomy around the optic disc for internal drainage of viscous subretinal fluid in all cases because it might be more effective with no use of perfluorocarbon. The retinotomy site was indicated by endodiathermy and then opened with intraocular scissors or a soft-tipped extrusion cannula. The subretinal fluid was evacuated through the retinotomy with a soft-tipped extrusion cannula or a vitrectomy probe, after which the detached retina was reattached following a complete fluid-air exchange. Retinal breaks were usually treated under air with an endolaser photocoagulation, but cryotherapy was used in cases of superior breaks anterior to the equator. For the prevention of postoperative retinal detachment, inferior 180° laser retinopexy was applied up to the ora serrata including the posterior margin of the vitreous base, while cryotherapy retinopexy was conducted around the superior sclerotomy sites (10- and 2-o'clock).
At the end of surgery, eyes were flushed with 40 mL of mix of 12%-20% C3F8. In some cases, 1300 centistokes silicone oil was injected, which were long-term tamponade determined necessary because of giant tear or wide retinal dialysis, or patient unable to bear prone position. Even though fluid blebs or subconjunctival air were detected after microcannula removal, we neither sutured any scleral wounds nor injected any additional tamponade into vitreous cavity. Patients underwent prone positioning for 7-10d, except patient unable to bear prone position with silicone oil tamponade.
Outcome Measures
The main outcome measures were primary reattachment rate, reasons for redetachment, final visual acuity, and surgical complications.
Patients were evaluated at postoperative day 1, 7, and 14, and then every month thereafter. Primary reattachment was defined as the complete reattachment of the retina when all of the gas or silicone oil had disappeared. The cause of redetachment was determined by operative findings at the time of reoperation. Logarithm of the minimum angle of resolution (logMAR) equivalents were used to evaluate visual acuity measured by Snellen chart. Corneal topography (Orbscan topography system II) were used to obtain simulated keratometric readings, and surgically induced astigmatism (SIA) was calculated[13]. Hypotony and IOP elevation were defined as IOP of <6 mm Hg and >30 mm Hg, respectively. Intraoperative and postoperative complications were evaluated. Statistical analyses were conducted via Wilcoxon's signed rank test.
RESULTS
The baseline demographics of the enrolled patients are summarized in Table 1. The study population included 17 men and 13 women, with an average age (mean±SD) of 52.4±11.4.
Table 1. Patient demographics.
| Demographics | Values |
| Number of eyes (number of patients) | 30 (30) |
| Mean age, a (range) | 52.4±11.4 (27-75) |
| Sex (%) | |
| M | 17 (56.7) |
| F | 13 (43.3) |
| Lens status (%) | |
| Cortical opacity | 15 (50.0) |
| Nuclear sclerosis | 4 (13.3) |
| Posterior subcapsular opacity | 3 (10.0) |
| Combined cataract | 8 (26.7) |
| Preoperative refraction, diopter (range) | -3.07±4.09 (+4.00 to -13.25) |
| Axial length, mm (range) | 25.1±2.0 (21.9-30.2) |
Characteristics of Primary Rhegmatogenous Retinal Detachment
Duration of symptoms (floater, visual field loss, visual loss) (days, mean±SD) was 14.1±17.0. Nineteen eyes (63.3%) presented with macula-off retinal detachment, and 6 eyes (20.0%) were diagnosed with inferior RRD. The extent of retinal detachment in clock hours (mean±SD) was 5.6±2.6, and the number of retinal breaks (mean±SD) was 1.6±0.9 (Table 2).
Table 2. Characteristics of primary rhegmatogenous retinal detachment.
| Characteristics | Values |
| Symptom duration, d (range) | 14.1±17.0 (1-90) |
| Extent of detachment, clock hours (range) | 5.6±2.6 (1-12) |
| Macula status (%) | |
| Attached | 11 (36.7) |
| Detached | 19 (63.3) |
| Number of retinal breaks (range) | 1.6±0.9 (1-4) |
| Location of retinal breaks (%) | |
| Superotemporal quadrant | 22 (73.3) |
| Superonasal quadrant | 10 (33.3) |
| Inferotemporal quadrant | 4 (13.3) |
| Inferonasal quadrant | 2 (6.7) |
| Morphology of retinal breaks (%) | |
| Horse shoe | 18 (60.0) |
| Round | 11 (36.7) |
| Giant | 1 (3.3) |
Intraocular Tamponade
Tamponade with gas (12%-18% C3F8) was employed in 24 eyes (80.0%), silicone oil in 4 eyes (13.3%), and air in 1 eye (3.3%). In cases which long-term tamponade was not required, a minimal air exchange was used in 1 eye (3.3%) to prevent postoperative hypotony.
Anatomical Outcomes
Primary reattachment was achieved in 27 eyes (90.0%). In three eyes (10.0%), anatomical success was not achieved after primary surgery. The reasons for failure to achieve anatomical success after primary surgery were incomplete laser retinopexy, persistent chronic subretinal fluid, and proliferative vitreoretinopathy, respectively. Re-operation was conducted in these 2 eyes, whereas one patient refused it. During the second vitrectomies, we noticed almost naïve conjunctivae. Final anatomical success was achieved in all 29 eyes (Tables 3, 4).
Table 3. Baseline characteristics of 3 patients with primary anatomical failure after primary vitrectomy and cataract surgery.
| Patient No. | Symptom duration, day | Preoperative refraction | Axial length (mm) | Extent of detachment, clock hours | Macula status | Number of retinal breaks | Location of retinal breaks |
| 1 | 21 | +0.25 D | 23.34 | 5 | Detached | 2 | Superotemporal |
| 2 | 8 | -3.75 D | 26.96 | 5 | Detached | 1 | Superotemporal |
| 3 | 15 | +4.00 D | 23.65 | 6 | Detached | 1 | Inferotemporal |
Table 4. Surgical characteristics of 3 patients with primary anatomical failure after primary vitrectomy and cataract surgery.
| Patient No. | Tamponade | Surgical complication | Duration to failure | Reason for failure | Reoperation |
| 1 | Gas | None | 26 | Persistent chronic SRF | Vitrectomy, scleral encircling |
| 2 | Gas | None | 24 | Incomplete laser retinopexy | Vitrectomy |
| 3 | Gas | None | 21 | PVR | Refused |
SRF: Subretinal fluid; PVR: Proliferative vitreoretinopathy.
Visual Acuity
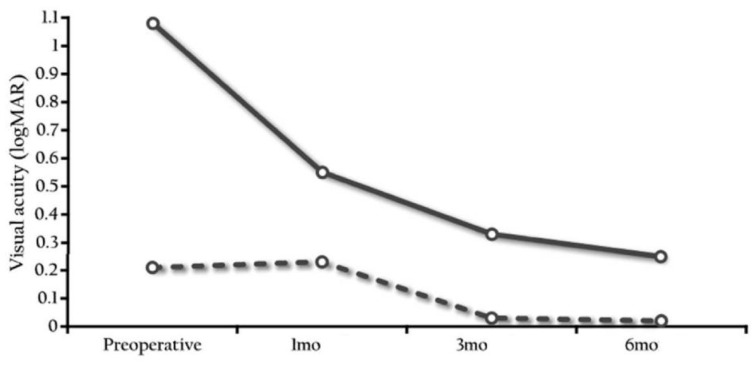
At each follow-up point, the logMAR visual acuity was improved from baseline in total 30 eyes. In 19 eyes with preoperative detached macula, improvement of visual acuity from baseline was showed at postoperative 3 and 6mo, while in 11 eyes with preoperative attached macula, visual improvement was presented at postoperative 1, 3, and 6mo. Preoperative logMAR visual acuity was showed significant difference between preoperative detached and attached macula, whereas this was not observed at postoperative 6 months (Table 5, Figure 1).
Table 5. Changes of visual acuity from baseline to 6 months in preoperative detached and attached macula.
| Visual acuity (logMAR) | Total (30 eyes) | Preoperative detached macula (19 eyes) | Preoperative attached macula (11 eyes) | P |
| Preoperative (±SD) | 0.76±0.74 | 0.21±0.26 | 1.08±0.74 | 1< 0.001 |
| Postoperative 1mo (±SD) | 0.42±0.45 | 0.23±0.28 | 0.55±0.50 | 10.061 |
| 2P | 0.003 | 0.461 | 0.002 | |
| Postoperative 3mo (±SD) | 0.20±0.37 | 0.03±0.53 | 0.33±0.46 | 10.010 |
| 2P | 0.001 | 0.027 | 0.003 | |
| Postoperative 6mo (±SD) | 0.14±0.31 | 0.02±0.03 | 0.25±0.39 | 10.051 |
| 2P | 0.001 | 0.018 | 0.003 |
LogMAR: logarithm of the minimum angle of resolution; SD: standard deviation. 1Mann Whitney U test; 2Wilcoxon signed rank test.
Figure 1. Changes of visual acuity from baseline to 6mo in preoperative detached and attached macula.
Full line represents sequential changes of visual acuity in 19 eyes with preoperative detached macula, and dotted line in 11 eyes with preoperative attached macula.
Intraocular Pressure
The preoperative IOP (mmHg, mean±SD) was 11.4±3.7. The postoperative IOP was 12.3±4.5, 13.1±5.2, and 12.7±3.1 at 1, 3, and 6mo, respectively.
Postoperative Astigmatism
The SIA (diopter, mean±SD) was 0.77±0.55 at 1mo postoperatively and gradually decreased to 0.61±0.55 at 3mo and 0.57±0.49 at 6mo (Table 6). Amplitudes and changes in SIA in our study were comparable with those in previous reports[13],[15].
Table 6. Changes in surgically induced astigmatism (SIA) (diopter) at each postoperative period.
| Postoperative period (mo) | SIA (diopter) |
| 1 | 0.77±0.55 |
| 3 | 0.61±0.55 |
| 6 | 0.57 ± 0.49 |
SD: Standard deviation.
x±s
Intraoperative and Postoperative Complications
Intraoperatively, iatrogenic retinal break (1 eye, 3.3%) and suprachoroidal effusion (1 eye, 3.3%) were developed. Tear of the posterior capsule was absent. Conversion into conventional 20-gauge vitrectomy was not noted.
Postoperatively, posterior capsule opacification occurred in 4 eyes (13.3%), IOL decentration in 1 eye (3.3%), and hyphema in 2 eyes (6.6%). Duration from primary surgery to posterior capsule opacification (days, mean±SD) was 54.7±50.1. No endophthalmitis developed during follow-up in any cases. Postoperative hypotony was not detected in our series, but 1 eye with silicone oil tamponade (3.3%) evidenced increased IOP (30 mm Hg) at postoperative day 2. The eye had normal IOP within 2 days after treatment with IOP-lowering agents. Macular pucker was identified in 3 eyes (10.0%), including 1 eye with silicone oil tamponade (Table 7).
Table 7. Intraoperative and postoperative complications.
| Complications | No. of patients (%) |
| Intraoperative | |
| Iatrogenic retinal break | 1 (3.3) |
| Suprachoroidal effusion | 1 (3.3) |
| Posterior capsular tear | 0 (0) |
| Postoperative | |
| Posterior capsule opacification | 4 (13.3) |
| IOL decentration | 1 (3.3) |
| Vitreous hemorrhage | 0 (0) |
| Hyphaema | 2 (6.6) |
| Hypotony (<6 mm Hg) | 0 (0) |
| Increased IOP (>30 mm Hg) | 1 (3.3) |
| Endophthalmitis | 0 (0) |
| Macular epiretinal membrane | 3 (10.0) |
| Redetachment | 3 (10.0) |
IOL: Intraocular lens; IOP: Intraocular pressure.
DISCUSSION
While scleral buckling and 20-gauge pars plana vitrectomy have been the standard treatments for RRD, recent years have witnessed a gradual increase in the application of sutureless vitrectomy for the repair of RRD[4]–[8]. Furthermore, since a combined approach (vitrectomy and cataract surgery) has advantages including more complete vitrectomy and obviation of the need for cataract surgery in the vitrectomized eye, combined sutureless vitrectomy and cataract surgery has recently become popular in patients with RRD. It is also well known that the most commonly adopted approach for cataract surgery is clear corneal phacoemulsification.
Crystalline lens may pose an anatomic obstacle to intraoperative maneuvers during vitrectomy, and complete removal of the basal vitreous gel surrounding the sclerotomy sites may be compromised in phakic eyes[16]. In vitrectomy for RRD, vitreous base dissection and scrupulous identification of all retinal breaks are crucial for anatomic and functional successes. The vitrectomy should be complete because incomplete or partial vitrectomy could cause residual vitreous traction-related problems such as secondary retinal breaks and retinal detachment. After vitrectomy, there is predictable worsening of lens opacities, specifically early feathering of the posterior capsule and late nuclear sclerosis. Therefore, we routinely perform vitreous base dissection in pseudophakic eyes or eyes that undergo a combined cataract surgery during primary RRD vitrectomy.
We must be aware of the potential complications of combined phacoemulsification and sutureless vitrectomy surgery for the treatment of RRD. Intraoperatively, the posterior capsule could be accidentally ruptured by sharp instruments such as an inserter during the insertion of the microcannula or the phaco tip during phacoemulsification[10]. We have not observed any such cases. Suprachoroidal retention of fluid or hemorrhage may be another intraoperative complication of 23-gauge sutureless vitrectomy[12],[17]. One case of suprachoroidal fluid was detected in current case series.
Increased risks for hypotony and associated endophthalmitis following sutureless vitrectomy have been reported[18],[19]. Especially when occurring after RRD surgery, hypotony can induce a reduction in the volume of intraocular tamponade. Additionally, during the transition from the scleral tunnel to clear corneal incision phacoemulsification, increased rates of endophthalmitis were reported[20],[21]. However, current reports showed that the risks of endophthalmitis associated with sutureless vitrectomy or clear corneal cataract surgery have decreased over time, and the incidence of endophthalmitis was similar between the newly introduced procedures and conventional standard surgeries[22]–[25]. Therefore, whether combining clear corneal cataract surgery and sutureless vitrectomy increases this risk has yet to be clearly determined. In the current study involving combined surgery, we observed no postoperative hypotony and no endophthalmitis, even though suturing was not conducted for any sclerotomy sites. We reported previously that both a combined surgery (phacovitrectomy) and a partial or minimal fluid-air exchange at the end of surgery in eyes with diabetic retinopathy may prevent or compensate for sutureless vitrectomy-related wound leakage or IOP decrease[13],[26],[27]. The absence of postoperative hypotony in our series can support these prior findings, as both combined surgery and intraocular tamponade with gas, silicone oil, or air were conducted in all cases of RRD.
Early IOP elevation following pars plana vitrectomy is a frequently encountered complication, and occurs in 13-56% of cases[28],[29]. Additionally, patients treated for RRD are at high risk for IOP elevation and should be followed closely[30],[31]. Possible mechanisms of IOP elevation after RRD vitrectomy include intraocular gas expansion, inflammation, silicone oil complications, pupillary block, or excess aqueous humor production. However, 23-gauge sutureless vitrectomy is known to reduce the risk of extremely high pressure, as the ports allow small amounts of gas to leak out when the IOP rises but the ports remain sealed. The 23-gauge sutureless system is reportedly associated with a lower risk of IOP elevation than the 20-gauge suture or 25-gauge sutureless systems[7],[32]. Similarly, this study, which used 23-gauge vitrectomy, resulted in IOP elevation in only 1 of 30 eyes.
The most commonly observed adverse events were posterior capsule opacification (4 eyes, 13.3%), macular epiretinal membrane (3 eyes, 10%), and redetachment (3 eyes, 10%). A high risk of posterior capsule opacification after combined surgery with intraocular gas or silicone oil tamponades has been noted in previous studies[14]. The relatively low rate of posterior capsule opacification in our combined surgery, even with intraocular tamponade and postoperative prone position, may be related to the surgeon-controlled-endoillumination-guided irrigation and aspiration which made the posterior capsule polishing nearly complete[33]. In pseudophakic eyes, the ability to achieve a meticulous anterior vitreous removal and a complete gas fill is known to be better than in phakic eyes. In our series using combined sutureless vitrectomy and cataract surgery, the rates of retinal redetachments including newly diagnosed retinal breaks or proliferative vitreoretinopathy were less than in eyes using no combined sutureless vitrectomy[4],[8].
Although vitreoretinal surgeons must be familiar with clear corneal cataract surgery, our experience with 23-gauge sutureless vitrectomy combined with clear corneal phacoemulsification for simultaneous RRD and cataract was rather encouraging. The incidence rates of postoperative hypotony and IOP elevation were remarkably low, and the rates of other complications were comparable to those associated with conventional phacovitrectomy. This combined surgery may have not only the known advantages of conventional combined surgery, but also additional ones, such as less conjunctival fibrosis and faster visual rehabilitation. The maintenance of a stable IOP with a low risk of IOP fluctuation and almost naïve conjunctiva may constitute additional and outstanding advantages of combined sutureless vitrectomy with cataract surgery in eyes with RRD.
The limitations of this study include the fact that this was a retrospective, noncomparative study and that it employed a small number of patients. Further long-term studies with a comparative group will be necessary to confirm the safety and efficacy of combined 23-gauge sutureless vitrectomy and clear corneal cataract surgery in eyes with RRD.
Acknowledgments
Conflicts of Interest: Moon H, None; Sohn HJ, None; Lee DY, None; Lee JY, None; Nam DH, None.
REFERENCES
- 1.Fujii GY, De Juan E, Jr, Humayun MS, Chang TS, Pieramici DJ, Barnes A, Kent D. Initial experience using the transconjunctival sutureless vitrectomy system for vitreoretinal surgery. Ophthalmology. 2002;109(10):1814–1820. doi: 10.1016/s0161-6420(02)01119-3. [DOI] [PubMed] [Google Scholar]
- 2.Fujii GY, De Juan E, Jr, Humayun MS, Pieramici DJ, Chang TS, Awh C, Ng E, Barnes A, Wu SL, Sommerville DN. A new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgery. Ophthalmology. 2002;109(10):1807–1812. doi: 10.1016/s0161-6420(02)01179-x. [DOI] [PubMed] [Google Scholar]
- 3.Eckardt C. Transconjunctival sutureless 23-gauge vitrectomy. Retina. 2005;25(2):208–211. doi: 10.1097/00006982-200502000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Lai MM, Ruby AJ, Sarrafizadeh R, Urban KE, Hassan TS, Drenser KA, Garretson BR. Repair of primary rhegmatogenous retinal detachment using 25-gauge transconjunctival sutureless vitrectomy. Retina. 2008;28(5):729–734. doi: 10.1097/IAE.0b013e318162b01c. [DOI] [PubMed] [Google Scholar]
- 5.Tsang CW, Cheung BT, Lam RF, Lee GK, Yuen CY, Lai TY, Lam DS. Primary 23-gauge transconjunctival sutureless vitrectomy for rhegmatogenous retinal detachment. Retina. 2008;28(8):1075–1081. doi: 10.1097/IAE.0b013e31817b98ba. [DOI] [PubMed] [Google Scholar]
- 6.Bourla DH, Bor E, Axer-Siegel R, Mimouni K, Weinberger D. Outcomes and complications of rhegmatogenous retinal detachment repair with selective sutureless 25-gauge pars plana vitrectomy. Am J Ophthalmol. 2010;149(4):630–634. doi: 10.1016/j.ajo.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 7.Kunikata H, Nishida K. Visual outcome and complications of 25-gauge vitrectomy for rhegmatogenous retinal detachment; 84 consecutive cases. Eye (Lond) 2010;24(6):1071–1077. doi: 10.1038/eye.2010.41. [DOI] [PubMed] [Google Scholar]
- 8.Romano MR, Das R, Groenwald C, Stappler T, Marticorena J, Valldeperas X, Wong D, Heimann H. Primary 23-gauge sutureless vitrectomy for rhegmatogenous retinal detachment. Indian J Ophthalmol. 2012;60(1):29–33. doi: 10.4103/0301-4738.90487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soheilian M, Mirdehghan SA, Peyman GA. Sutureless combined 25-gauge vitrectomy, phacoemulsification, and posterior chamber intraocular lens implantation for management of uveitic cataract associated with posterior segment disease. Retina. 2008;28(7):941–946. doi: 10.1097/IAE.0b013e31816ed5c7. [DOI] [PubMed] [Google Scholar]
- 10.Sisk RA, Murray TG. Combined phacoemulsification and sutureless 23-gauge pars plana vitrectomy for complex vitreoretinal diseases. Br J Ophthalmol. 2010;94(8):1028–1032. doi: 10.1136/bjo.2009.175984. [DOI] [PubMed] [Google Scholar]
- 11.Heath G, Rahman R. Combined 23-gauge, sutureless transconjunctival vitrectomy with phacoemulsification without face down posturing for the repair of idiopathic macular holes. Eye(Lond) 2010;24(2):214–220. doi: 10.1038/eye.2009.292. [DOI] [PubMed] [Google Scholar]
- 12.Sood V, Rahman R, Denniston AK. Phacoemulsification and foldable intraocular lens implantation combined with 23-gauge transconjunctival sutureless vitrectomy. J Cataract Refract Surg. 2009;35(8):1380–1384. doi: 10.1016/j.jcrs.2009.02.047. [DOI] [PubMed] [Google Scholar]
- 13.Lee DY, Jeong HS, Sohn HJ, Nam DH. Combined 23-gauge sutureless vitrectomy and clear corneal phacoemulsification in patients with proliferative diabetic retinopathy. Retina. 2011;31(9):1753–1758. doi: 10.1097/IAE.0b013e31820d4057. [DOI] [PubMed] [Google Scholar]
- 14.Smith M, Raman SV, Pappas G, Simcock P, Ling R, Shaw S. Phacovitrectomy for primary retinal detachment repair in presbyopes. Retina. 2007;27(4):462–467. doi: 10.1097/01.iae.0000243066.19645.de. [DOI] [PubMed] [Google Scholar]
- 15.Park DH, Shin JP, Kim SY. Surgically induced astigmatism in combined phacoemulsification and vitrectomy; 23-gauge transconjunctival sutureless vitrectomy versus 20-gauge standard vitrectomy. Graefes Arch Clin Exp Ophthalmol. 2009;247(10):1331–1337. doi: 10.1007/s00417-009-1109-3. [DOI] [PubMed] [Google Scholar]
- 16.Schiff WM, Barile GR, Hwang JC, Tseng JJ, Cekiç O, Del Priore LV, Chang S. Diabetic vitrectomy: influence of lens status upon anatomic and visual outcomes. Ophthalmology. 2007;114(3):544–550. doi: 10.1016/j.ophtha.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 17.Ooto S, Kimura D, Itoi K, Mukuno H, Kusuhara S, Miyamoto N, Akimoto M, Takagi H. Suprachoroidal fluid as a complication of 23-gauge vitreous surgery. Br J Ophthalmol. 2008;92(10):1433–1434. doi: 10.1136/bjo.2007.133462. [DOI] [PubMed] [Google Scholar]
- 18.Kunimoto DY, Kaiser RS, Wills Eye Retina Service Incidence of endophthalmitis after 20- and 25-gauge vitrectomy. Ophthalmology. 2007;114(12):2133–2137. doi: 10.1016/j.ophtha.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 19.Scott IU, Flynn HW, Jr, Dev S, Shaikh S, Mittra RA, Arevalo JF, Kychenthal A, Acar N. Endophthalmitis after 25-gauge and 20-gauge pars plana vitrectomy: incidence and outcomes. Retina. 2008;28(1):138–142. doi: 10.1097/IAE.0b013e31815e9313. [DOI] [PubMed] [Google Scholar]
- 20.Lundström M, Wejde G, Stenevi U, Thorburn W, Montan P. Endophthalmitis after cataract surgery: a nationwide prospective study evaluating incidence in relation to incision type and location. Ophthalmology. 2007;114(5):866–870. doi: 10.1016/j.ophtha.2006.11.025. [DOI] [PubMed] [Google Scholar]
- 21.Nichamin LD, Chang DF, Johnson SH, Mamalis N, Masket S, Packard RB, Rosenthal KJ, American Society of Cataract and Refractive Surgery Cataract Clinical Committee ASCRS White Paper: What is the association between clear corneal cataract incisions and postoperative endophthalmitis? J Cataract Refract Surg. 2006;32(9):1556–1559. doi: 10.1016/j.jcrs.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 22.Hu AY, Bourges JL, Shah SP, Gupta A, Gonzales CR, Oliver SC, Schwartz SD. Endophthalmitis after pars plana vitrectomy a 20- and 25-gauge comparison. Ophthalmology. 2009;116(7):1360–1365. doi: 10.1016/j.ophtha.2009.01.045. [DOI] [PubMed] [Google Scholar]
- 23.Parolini B, Romanelli F, Prigione G, Pertile G. Incidence of endophthalmitis in a large series of 23-gauge and 20-gauge transconjunctival pars plana vitrectomy. Graefes Arch Clin Exp Ophthalmol. 2009;247(7):895–898. doi: 10.1007/s00417-009-1063-0. [DOI] [PubMed] [Google Scholar]
- 24.Chen JK, Khurana RN, Nguyen QD, Do DV. The incidence of endophthalmitis following transconjunctival sutureless 25- vs 20-gauge vitrectomy. Eye(Lond) 2009;23(4):780–784. doi: 10.1038/eye.2008.160. [DOI] [PubMed] [Google Scholar]
- 25.Oshika T, Hatano H, Kuwayama Y, Ogura Y, Ohashi Y, Oki K, Uno T, Usui N, Yoshitomi F. Incidence of endophthalmitis after cataract surgery in Japan. Acta Ophthalmol Scand. 2007;85(8):848–851. doi: 10.1111/j.1600-0420.2007.00932.x. [DOI] [PubMed] [Google Scholar]
- 26.Nam DH, Ku M, Sohn HJ, Lee DY. Minimal fluid-air exchange in combined 23-gauge sutureless vitrectomy, phacoemulsification, and intraocular lens implantation. Retina. 2010;30(1):125–130. doi: 10.1097/IAE.0b013e3181b4f26b. [DOI] [PubMed] [Google Scholar]
- 27.Lee JY, Jeong HS, Lee DY, Sohn HJ, Nam DH. Early postoperative intraocular pressure stability after combined 23-gauge sutureless vitrectomy and cataract surgery in patients with proliferative diabetic retinopathy. Retina. 2012;32(9):1767–1774. doi: 10.1097/IAE.0b013e3182475ad6. [DOI] [PubMed] [Google Scholar]
- 28.Anderson NG, Fineman MS, Brown GC. Incidence of intraocular pressure spike and other adverse events after vitreoretinal surgery. Ophthalmology. 2006;113(1):42–47. doi: 10.1016/j.ophtha.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 29.Yang HK, Woo SJ, Park KH, Park KH. Intraocular pressure changes after vitrectomy with and without combined phacoemulsification and intraocular lens implantation. Korean J Ophthalmol. 2010;24(6):341–346. doi: 10.3341/kjo.2010.24.6.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Muether PS, Hoerster R, Kirchhof B, Fauser S. Course of intraocular pressure after vitreoretinal surgery: is early postoperative intraocular pressure elevation predictable? Retina. 2011;31(8):1545–1552. doi: 10.1097/IAE.0b013e31820f4b05. [DOI] [PubMed] [Google Scholar]
- 31.Hasegawa Y, Okamoto F, Sugiura Y, Okamoto Y, Hiraoka T, Oshika T. Intraocular pressure elevation in the early postoperative period after vitrectomy for rhegmatogenous retinal detachment. Jpn J Ophthalmol. 2012;56(1):46–51. doi: 10.1007/s10384-011-0094-3. [DOI] [PubMed] [Google Scholar]
- 32.Misra A, Ho-Yen G, Burton RL. 23-gauge sutureless vitrectomy and 20-gauge vitrectomy: a case series comparison. Eye(Lond) 2009;23(5):1187–1191. doi: 10.1038/eye.2008.175. [DOI] [PubMed] [Google Scholar]
- 33.Kim KH, Sohn HJ, Song HJ, Lee DY, Nam DH. Surgeon-controlled-endoillumination-guided irrigation and aspiration during combined 23-gauge sutureless vitrectomy and cataract surgery in eyes with poor fundus reflex. J Cataract Refract Surg. 2010;36(12):2028–2031. doi: 10.1016/j.jcrs.2010.10.004. [DOI] [PubMed] [Google Scholar]