Abstract
Background
Non‐specific low back pain is a common condition often without a clear mechanism for its presentation. Recently more attention has been placed on the hip and its potential contributions to non‐specific chronic low back pain (NSCLBP). Emphasis in research has mainly been placed on motor control, strength and endurance factors in relation to NSCLBP. Limited focus has been placed on hip mobility and its potential contribution in subjects with NSCLBP.
Purpose/Aim
The aim of this study was to compare passive ROM in hip extension, hip internal rotation, hip external rotation and total hip rotation in active subjects with NSCLBP to healthy control subjects. The hypothesis was that active subjects with NSCLBP would present with decreased total hip ROM and greater asymmetry when compared to controls.
Design
Two group case controlled
Setting
Clinical research laboratory
Participants
30 healthy subjects without NSCLBP and 30 active subjects with NSCLBP. Subjects categorized as NSCLBP were experiencing pain in the low back area with or without radicular symptoms of greater than three months duration.
Main Outcome Measure
Passive hip extension (EXT), hip internal rotation (IR), hip external rotation (ER) and total hip rotation ROM. A digital inclinometer was used for measurements.
Results
There was a statistically significant difference (p<0.001) in hip passive extension ROM between the control group and the NSCLBP group bilaterally. Mean hip extension for the control group was 6.88 bilaterally. For the NSCLBP group, the mean hip extension was ‐4.28 bilaterally. This corresponds to a difference of means between groups of 10.88. There was no statistically significant differences (p>0.05) in hip IR, ER, or total rotation ROM between groups.
Conclusions
The results of this study indicate that a significant difference in hip extension exists in active subjects with NSCLBP compared to controls. It may be important to consider hip mobility restrictions and their potential impact on assessment of strength in NSLBP subjects. Future studies may be needed to investigate the relationship between measurements and intervention strategies.
Level of Evidence
2b
Keywords: Hip extension, hip mobility, hip rotation, inclinometer, non‐specific low back pain
Introduction
Low back pain is a common condition with a lifetime prevalence in the general population ranging up to 84%, with prevalence of chronic low back pain noted at approximately 23%.1 The condition is also common amongst both adolescent and adult athletes.2‐4 In spite of the significant resources that have been utilized to treat this condition, it appears that current approaches have resulted in less than satisfactory outcomes for pain and function.5 One reason for such poor outcomes may be a limited understanding of a clear causative mechanism for this condition. Secondary to this limited knowledge regarding the mechanism of injury, this condition is generally referred to as non‐specific chronic low back pain (NSCLBP).6
The majority of the literature on low back pain continues to focus on anatomical and biomechanical/motor control abnormalities or dysfunction in the trunk and or spine regions without regard to other potential contributors to the condition.7‐9 There has recently been an increased interest in the possibility of hip involvement contributing to clinical conditions involving NSCLBP.10‐12 This attention on the hip is often focused upon motor control, strength and endurance deficits of the gluteus maximus and medius muscles.13‐15 Less emphasis appears to be placed on mobility or range of motion (ROM) of the hip joint itself. Of the studies examining hip ROM in relation to low back pain, many have focused primarily upon transverse and not sagittal or frontal plane motion.16‐18 Findings from these studies have noted significant asymmetry in hip internal rotation (IR) or external rotation (ER) and total rotation (TR) in subjects with low back pain as opposed to subjects without low back pain. The subjects in these reports participated in rotation dependent sports, that included golf, tennis and racquetball.19,20
Hip extension is another essential motion for proper loading and function of the lumbar spine and hip. It has been noted that normal hip extension mobility is imperative for normal mechanical load distribution in the hip and for efficient metabolic demands in standing.21 A decrease in hip extension, for example occurring due to shortening of the hip flexors, may result in an external flexor torque at the hip. This could result in an increased metabolic cost as a result of extensor muscles of the hip attempting to prevent collapse of hip and knee into full flexion.21 Theoretically it is possible that hip flexor shortening may result in an increased activation of low back musculature, with resultant increased internal moment, to keep the trunk in an upright position during standing and walking. Excessive activation of lumbar spine extensors may lead to early onset fatigue and decreased protection from shearing and torsional loads to lumbar spine, as well as impaired postural control strategies.22 Additionally, it has been demonstrated that in subjects with longstanding hip fusions that an excessive anterior pelvic tilt occurs during gait to compensate for lack of hip extension.23 This provides further evidence to suggest that lack of normal hip extension may alter the timing mechanism and motor activation of the lumbar spine. The role that mobility of hip abduction, adduction and flexion plays in the condition of NSCLBP appears to be limited based on current understandings of the condition and lack of significant investigation of issue.
A great number of musculoskeletal changes occur during the aging process. This includes decreased hip extension ROM during gait and with clinical testing as observed with instrumented gait analysis.24 Currently, a dearth of normative data exists for what constitutes normal ROM of the hip within differing subsets of the human population. Existing information consists of an assortment of different testing positions, genders, active versus passive testing and use of different numbers of examiners during testing.25‐27 Some studies are limited to young healthy athletic subjects who may not be reflective of the general or the aging athletic population.28,29
The purpose of this study was to compare passive ROM in hip extension, hip internal rotation and external rotation and total hip rotation in healthy subjects to active subjects with non‐specific chronic low back pain. Further, the current study will contribute additional data for what constitutes normal passive hip ROM. This will assist in clinical decision making and to help determine if significant differences exist between the groups examined. The authors hypothesized that active subjects with NSCLBP would have less total hip ROM and greater asymmetry than healthy subjects.
METHODS
The study utilized a sample of convenience of 30 volunteer subjects without NSCLBP (13 males and 17 females; mean ± SD age 34.0 ± 13.1 years; height, 171.5 ± 11.9 cm; mass, 71.9 ± 13.9 kg) and 30 subjects with a diagnosis of NSCLBP (14 males and 16 females; age 45.0 ± 12.0 years; height, 170.5 ± 8.3 cm; mass, 71.1 ± 12.8 kg). Subjects were recruited through local medical and recreational facilities. All subjects were included if they reported no history of surgery to spine, hips, knees, or history of neurological insult to the musculoskeletal system and had not experienced acute pain (defined as within previous two weeks) of the hips, low back or knees. Subjects categorized as active with NSCLBP met the criteria above in addition to experiencing pain in the low back area with or without radicular symptoms of greater than three months duration.30 Subjects were considered active if they participated in some form of recreational sport or regular exercise routine a minimum of three days a week. All subjects were informed of the purpose of the study and signed an informed consent document prior to data collection. The human subject's review board at Western Washington University approved the protocol for the study.
Study Design
All data collection took place in a research institution and all testing was completed in a single session by the primary investigator. The investigator is a licensed physical therapist with 20 years of experience in the musculoskeletal practice environment. During evaluation, the investigator measured EXT, IR and ER of both left and right hip. A digital inclinometer (Digital Protractor Pro 3600, Miutoyo America, Aurora, Illinois) with an accuracy of 0.18 was used to measure hip ROM of all subjects in this study. This digital inclinometer has been found to possess good reliability and concurrent validity with the universal goniometer which is the standard tool in clinical practice.31 The reliability of the device in previous work on hip ROM was noted to be 0.90.32 No practice or warm up was performed prior to measurements.
During EXT measurement, the subjects were positioned supine and a modified Thomas test was performed. The modified Thomas test, typically a test for length of hip flexors to measure hip extension PROM, has been found to possess good reliability.32‐34 The hip being measured was positioned at the end of the treatment table and the tested leg was then cantilevered over the edge of table with the end feel resulting from the effects of gravity. No manual contact was made with the tested leg. The opposite leg was held actively by the subjects with the hip and knee in a flexed position against the chest. Instructions were provided for subjects to pull their knee straight toward their head to avoid any abduction. In addition, subjects were provided both verbal and tactile feedback to maintain a neutral lumbar spine and pelvis throughout the evaluation, which was accomplished with consistency in keeping knee firmly against the chest. The inclinometer measurement was taken from the anterior mid femur position with midpoint between the greater trochanter and lateral femoral condyle. Measurements were recorded as a negative number if they were above the horizontal position (more flexed than neutral position) and a positive number if they fell below the horizontal position (more extended than neutral position).
For IR and ER measurements, the subjects were positioned in the prone position on the treatment table and the following standard protocol was used.32 The investigator passively flexed both the knees to 90 degrees while both hips were positioned in neutral for measuring hip internal rotation. Next, the investigator instructed the subjects to relax, allowing the shank of both legs to rotate outward for IR until reaching passive end feel of joint motion under the effects of gravity. For ER, the investigator passively flexed one knee to 90 degrees and then instructed the subject to relax, allowing the shank to rotate towards the midline and leg crossed over midline until reaching passive end feel as per effects of gravity. The non‐ measured leg was positioned in extension on the table. The subject's pelvis was stabilized by the investigator's assistant during hip ER measures in order to prevent pelvic rotation. Additionally, the subjects that displayed with greater ER (motion blocked by presence of opposite leg) had their non‐tested leg abducted slightly to allow for full measurement. Measurements with the inclinometer were taken with device placed at midline of medial shaft of tibia between the medial malleoli and medial tibial condyle.
Each measurement was performed three times and the mean of the three measurements was calculated and recorded. Total hip range of motion was calculated as the sum of internal and external hip rotation. The order of the hip ROM measurements was randomized for each subject. In addition, the inclinometer measurements were verbally given by the investigator and recorded by an assistant.
Statistical Analyses
Statistics were run for all data using SPSS 22. For each direction of motion (extension, external rotation, and internal rotation), a two‐way mixed analysis of variance (ANOVA) was conducted to determine the effects of side (left vs. right) and group (control vs. NSCLBP) on hip ROM. In addition, a two‐way mixed ANOVA was run to determine the effects of side and group on total hip ROM. Simple effects analyses were conducted for significant interaction effects. Alpha level was set to p < 0.05.
RESULTS
Hip Extension
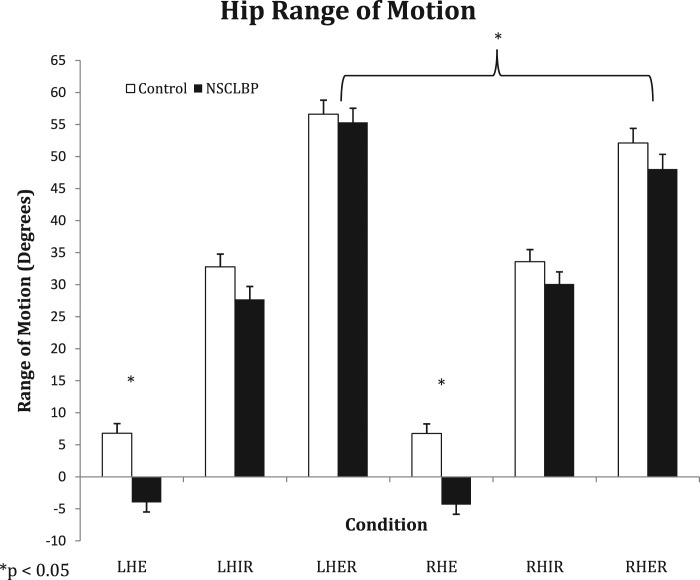
Hip extension ROM was significantly greater in the control group (6.78 ± 7.188) compared to the NSCLBP group (‐4.16 ± 8.818) (F [1, 58] = 29.19, p < .001, η2=.335) (Figure 1). There was no significant main effect of side on hip extension ROM (F[1, 58] = .191, p = .664), and no significant side by group interaction effect on hip extension ROM (F [1, 58] = .122, p = .728).
Figure 1.
Left Hip Extension (LHE), Left Hip Internal Rotation (LHIR), Left Hip External Rotation (LHER), Right Hip Extension (RHE), Right Hip Internal Rotation (RHIR), Right Hip External Rotation. * p < 0.05
Hip External Rotation
Hip external rotation showed no difference between groups (F[1, 58] = .850, p = .360). External rotation was significantly greater in both groups on the left side (55.97 ± 11.848) than the right (50.08 ± 12.378), F[1, 58] = 21.79, p < .001 (Figure 1). There was no side by group interaction effect on hip external rotation mediating the effect of side (F[1, 58] = 1.23, p = .272).
Hip Internal Rotation
There was no significant effect of group on hip internal rotation (F [1, 58] = 2.55, p = .116). Internal rotation ROM was significantly greater in the right (31.84 ± 10.41º) than the left hip (30.25 ± 11.00º) (F[1, 58] = 4.51, p = .038) (Figure 1). There was no side by group interaction effect on hip internal rotation ROM (F [1, 58] = 1.11, p = .297).
Total Hip Rotation ROM
There was nearly a significant effect of group on total hip ROM, with the NSCLBP group having insignificantly lower ranges of motion (80.61 ± 14.898) than controls (87.54 ± 14.818) (F [1, 58] = 3.55, p = .065). Total ROM was significantly lower on the right side (81.92 ± 15.538) than the left (86.22 ± 14.178) (F [1, 58] = 15.59, p < .001). These were not mediated by a side by group interaction (F [1, 58] = .312, p = .579).
DISCUSSION
The primary purpose of this study was to compare passive hip ROM in controls and active subjects with NSCLBP. The current data demonstrated a significant difference in hip extension only. The control group on average demonstrated 10° greater hip extension than the NSCLBP population. These findings suggest that hip extension should be evaluated in active subjects with NSCLBP during clinical assessment.
Hip extension measurements in the clinical setting tend to raise concerns in terms of validity of true hip measurements. The concerns are generally centered on the ability to separate out contributions of the hip from the lumbo‐pelvic region. Additional concerns may be in the validity of measurement devices utilized in the clinical setting. Measurements are often taken with a universal goniometer in the clinical setting as compared to a biomechanics lab that may use three dimensional (3D) analysis. This has recently been addressed by Moreside and McGill who examined 77 healthy young males and assisted in the establishment of normative data for hip extension, external and internal rotation ROM. Importantly, they compared 3D video based measurements with standard goniometer for hip extension and found a high correlation between the measurements (r2 =.88).35 This provides increased validity for use of common clinical tools in assessing hip ROM. The inclinometer used in this study has been found to be a valid and reliable tool for assessing hip ROM.32
Several studies have noted a relationship between low back pain and tightness of the anterior hip region. Pattelma et al noted that subjects with both sub‐acute low back pain and chronic low back pain had significantly shortened hip flexors than those without low back pain.36 Others have also noted a correlation between low back pain and short hip flexors in subjects ranging from young elite golfers to people who were employed in fields involving at least moderate physical effort and experienced chronic or recurrent low back pain.37,38 These findings are consistent with the current results where we noted on average a difference of 10° between those with NSCLBP and controls. When individuals lack appropriate hip extension during gait they may compensate through mechanisms such as excessive anterior pelvic tilt with resultant increased lumbar lordosis.23 This compensation could potentially lead to overuse, fatigue and altered motor activation patterns in the lumbar spine and hip region. A decrease in normal lumbo‐pelvic motion may result in other structures compensating for the lack of potential and elastic strain energy that normally occurs with stretching of the anterior hip region during terminal stance phase of gait. The lack of passive stretching may result in the need to excessively recruit contractile agents in a manner that may not be energy efficient.39 Interestingly, the authors of a recent study demonstrated that increases in passive hip ROM in extension and rotation through selected interventions did not result in a carryover into functional movement patterns in normal healthy males.40 The possibility is raised that additional interventions in conjunction with stretching may be necessary to create functional changes in individuals.
The current study's findings were not in agreement with other literature in regards to total hip ROM. Van Dillen et al noted in a study of 48 subjects with low back pain (LBP) a significant decrease in total hip ROM and asymmetry in rotation as compared to controls.19 The results of the current study showed no differences in total ROM. The VanDillen et al LBP group consisted of young athletes and may not be comparable to this study's sampled population which differed in mean age by approximately 20 years. What is particularly noteworthy is the large difference in total ROM and hip ER data collected in the present study. This study measured a total hip ROM of 89.78 on left and 85.78 on right in the control group. Three other studies that specifically recorded this data had values ranging between 60.268and 77.18 in controls.18,19,41 Total mean ROM measurements for subjects in the current study with LBP were 83.18 for left hip and 78.28 for right hip. This contrasted with Barbee‐Ellison et al and Van Dillen et al that recorded values ranging between a low of 51.558 and a high of 69.668 in subjects with LBP. These noted differences may be the result of the present study utilizing a digital inclinometer as compared to photographic method (use of digital camera to capture measures for objective analysis), or a universal goniometer and fluid filled goniometer used in above studies.19,41,42 It may also have been the result of differing criteria in what constitutes pelvic stabilization. As noted previously, all efforts were made to prevent compensatory movement of the pelvis during this study.
Given the fact that clear agreement on the diagnosis of NSCLBP remains elusive at this point, it is important to consider all potential anatomical structures in the region as a potential contributor to the condition. This would include the sacroiliac joint (SIJ) which is intricately linked to the lumbar spine through a vast network of both contractile and non‐contractile elements. Cibulka noted that subjects with LBP and evidence of sacroiliac joint (SIJ) dysfunction had significantly greater hip ER than hip IR ROM unilaterally.43 This was in opposition to those without SIJ dysfunction who demonstrated with bilaterally greater hip ER than hip IR ROM. Additionally, Cibulka noted that asymmetries in hip rotation may result in significant differences in muscle strength of hip rotator muscles.44 Both of these studies indicate that asymmetry in hip ER between groups could result in changes in motor control and increased loading of lumbo‐pelvic structures. Flynn et al found that a difference in hip rotation was one of five predictive variables that relates to successful short‐term improvement with spinal manipulation in patients with nonradicular low back pain.17 It was observed that manipulation was more likely to contribute to a successful outcome if hip IR was greater than 358. The data in the current study demonstrated no difference in IR/ER ROM between or within groups.
Study Limitations
The main limitation during data collection was potential for alterations of stabilization of the pelvis during measurements. As other authors have noted, stabilizing the pelvis during the modified Thomas test, and for passive hip ROM in general, is very important in order to achieve consistency during hip measurement and limit lumbar spine involvement.33,45 All efforts were made to limit this involvement and it was felt that verbal and tactile cues given to subjects was sufficient to achieve this goal. Additionally, the main investigator was not blinded to the subjects' condition, which had the potential to bias measurements. Another potential limitation may be in the average age difference of 11 years between the NSCLBP group vs control group (mean age of 34 versus mean age of 45 respectively). Future studies may consider age matching subjects. Lastly, the subjects were not required to complete a low back disability score questionnaire or pain scale to quantify their low back pain. This may have helped to determine if significant differences existed between individuals before the study was conducted. The authors believe that the criteria utilized in the study were sufficient in assessing what is examined in the common clinical practice.
CONCLUSION
The results of this study indicate that active subjects presenting with NSCLBP had significantly less passive hip extension than controls, when measured using the Thomas test. There were no significant differences noted in total hip rotation ROM nor hip IR/ER between groups. These findings suggest that passive hip extension may be an important variable that should be included within the clinical examination of active subjects with NSCLBP. It may be important to consider hip mobility restrictions and their potential impact on assessment of strength and possible SIJ involvement. Future studies may be needed to investigate the relationship between measurements and intervention strategies.
REFERENCES>
- 1.Walker BF The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J of Spinal Diord. 2000;13(3):205‐217. [DOI] [PubMed] [Google Scholar]
- 2.Schmidt CP Zwingenberger S Walther A, et al. Prevalence of low back pain in adolescent athletes ‐ an epidemiological investigation. Int I Sports Med. 2014;35(8):684‐689. [DOI] [PubMed] [Google Scholar]
- 3.Van Hilst J Hilgersom NF Kuilman MC Kuijer PP Frings‐Dresen MH Low back pain in young elite field hockey players, football players and speed skaters: Prevalence and risk factors. J Back Musculoskelet Rehabil. 24 2014. [DOI] [PubMed] [Google Scholar]
- 4.Hoskins W Pollard H Daff C, et al. Low back pain status in elite and semi‐elite Australian football codes: a cross‐sectional survey of football (soccer), Australian rules rugby league, rugby union and non‐athletic controls. BMC Musculoskeletal Disord. 2009;10:38. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5.Wand BM O'Connell NE Chronic non‐specific low back pain ‐ sub‐groups or a single mechanism? BMC Musculoskeletal Disord. 2008;9:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balague F Mannion AF Pellise F Cedraschi C Non‐specific low back pain. Lancet. Feb 4 2012;379(9814):482‐491. [DOI] [PubMed] [Google Scholar]
- 7.D'Hooge R Hodges P Tsao H Hall L Macdonald D Danneels L Altered trunk muscle coordination during rapid trunk flexion in people in remission of recurrent low back pain. J Electromyogr Kinesiol. 2013;23(1):173‐181. [DOI] [PubMed] [Google Scholar]
- 8.MacDonald D Moseley GL Hodges PW People with recurrent low back pain respond differently to trunk loading despite remission from symptoms. Spine. Apr 1 2010;35(7):818‐824. [DOI] [PubMed] [Google Scholar]
- 9.Hosseinifar M Akbari M Behtash H Amiri M Sarrafzadeh J The effects of stabilization and Mckenzie exercises on transverse abdominis and multifidus muscle thickness, pain, and disability: A randomized controlled trial in nonspecific chronic low back pain. J Phys Ther Sci. 2013;25(12):1541‐1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leinonen V Kankaanpaa M Airaksinen O Hanninen O Back and hip extensor activities during trunk flexion/extension: effects of low back pain and rehabilitation. Arch Phys Med Rehabil. 2000;81(1):32‐37. [DOI] [PubMed] [Google Scholar]
- 11.Mok NW Brauer SG Hodges PW Hip strategy for balance control in quiet standing is reduced in people with low back pain. Spine. Mar 15 2004;29(6):E107‐112. [DOI] [PubMed] [Google Scholar]
- 12.Harris‐Hayes M Sahrmann SA, Van Dillen LR Relationship between the hip and low back pain in athletes who participate in rotation‐related sports. J Sports Rehabil. 2009;18(1):60‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kendall KD SC Ferber R The relationship between hip‐abductor strength and the magnitude of pelvic drop in patients with low back pain. J Sports Rehabil. 2010;19(4):422‐435. [DOI] [PubMed] [Google Scholar]
- 14.Kankaanpaa M Taimela S Laaksonen D Hanninen O Airaksinen O Back and hip extensor fatigability in chronic low back pain patients and controls. Arch Phys Med Rehabil. 1998;79(4):412‐417. [DOI] [PubMed] [Google Scholar]
- 15.Vogt L Pfeifer K Banzer W Neuromuscular control of walking with chronic low‐back pain. Man Ther. 2003;8(1):21‐28. [DOI] [PubMed] [Google Scholar]
- 16.Harris‐Hayes M, Van Dillen LR The inter‐tester reliability of physical therapists classifying low back pain problems based on the movement system impairment classification system. Pm R. 2009;1(2):117‐126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flynn T Fritz J Whitman J, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short‐term improvement with spinal manipulation. Spine. 15 2002;27(24):2835‐2843. [DOI] [PubMed] [Google Scholar]
- 18.Barbee‐Ellison JB RS, Sahrmann SA. Patterns of hip rotation range of motion: comparisons between healthy subjects and patients with low back pain. Phys Ther.1990;70:537–41. 1990;70:537‐541. [DOI] [PubMed] [Google Scholar]
- 19.Van Dillen LR Bloom NJ Gombatto SP Susco TM Hip rotation range of motion in people with and without low back pain who participate in rotation‐related sports. Phys Ther Sport. 2008;9(2):72‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vad VB Bhat AL Basrai D Gebeh A Aspergren DD Andrews JR Low back pain in professional golfers: the role of associated hip and low back range‐of‐motion deficits. Am J Sports Med. 2004;32(2):494‐497. [DOI] [PubMed] [Google Scholar]
- 21.DAN. Kinesiology of the Musculoskeletal System. 2nd ed. St. Louis, Missouri: 2010. [Google Scholar]
- 22.Johanson e BS Janssens L Pijnes M Claeys K Paasuke M The effect of acute back muslce fatigue on postural control strategy in people with and without recurrent low back pain. Eur Spine J. 2011;20(12):152‐159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thambyah A, Hee HT, Das De S, Lee SM Gait adaptations in patients with longstanding hip fusion. J Orthop Surg (Hong Kong). 2003;11(2):154‐158. [DOI] [PubMed] [Google Scholar]
- 24.Kerrigan DC Lee LW Collins JJ Riley PO Lipsitz LA Reduced hip extension during walking: healthy elderly and fallers versus young adults. Arch Phys Med Rehabil. 2001;82(1):26‐30. [DOI] [PubMed] [Google Scholar]
- 25.Roach KE Miles TP Normal hip and knee active range of motion: the relationship to age. Phys Ther. 1991;71(9):656‐665. [DOI] [PubMed] [Google Scholar]
- 26.Nussbaumer S, Leunig M, Glatthorn JF, Stauffacher S, Gerber H, Maffiuletti NA Validity and test‐retest reliability of manual goniometers for measuring passive hip range of motion in femoroacetabular impingement patients. BMC Musculoskeletal Disord. 2010; 11:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Simoneau GG Hoenig KJ Lepley JE Papanek PE Influence of hip position and gender on active hip internal and external rotation. J Orthop Sports Phys Ther. 1998;28(3):158‐164. [DOI] [PubMed] [Google Scholar]
- 28.Harvey D Assessment of the flexibility of elite athletes using the modified Thomas test. Br J Sports Med. 1998;32(1):68‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang SS Whitney SL Burdett RG Janosky JE Lower extremity muscular flexibility in long distance runners. J Orthop Sports Phys Ther. 1993;17(2):102‐107. [DOI] [PubMed] [Google Scholar]
- 30.Koes BW, van Tulder MW, Thomas S Diagnosis and treatment of low back pain. BMJ. 17 2006;332(7555):1430‐1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Franettovich MM McPoil TG Russell T Skardoon G Vicenzino B The ability to predict dynamic foot posture from static measurements. J Am Podiatr Med Assoc. 2007;97(2):115‐120. [DOI] [PubMed] [Google Scholar]
- 32.Roach S San Juan JG Suprak DN Lyda M Concurrent validity of digital inclinometer and universal goniometer in assessing passive hip mobility in healthy subjects. Int J Sports Phys Ther. 2013;8(5):680‐688. [PMC free article] [PubMed] [Google Scholar]
- 33.Kendall FP McCreary EK Kendall HO Muscles, testing and function. 3rd ed. Baltimore: Williams & Wilkins; 1983. [Google Scholar]
- 34.Bartlett MD Wolf LS Shurtleff DB Stahell LT Hip flexion contractures: a comparison of measurement methods. Arch Phys Med Rehabil. 1985;66(9):620‐625. [PubMed] [Google Scholar]
- 35.Moreside JM McGill SM Quantifying normal 3D hip ROM in healthy young adult males with clinical and laboratory tools: hip mobility restrictions appear to be plane‐specific. Clin Biomech (Bristol, Avon). Oct;26(8):824‐829. [DOI] [PubMed] [Google Scholar]
- 36.Paatelma M Karvonen E Heiskanen J Clinical perspective: how do clinical test results differentiate chronic and subacute low back pain patients from “non‐patients”? J Man Manip Ther. 2009;17(1):11‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Evans K Refshauge KM Adams R Aliprandi L Predictors of low back pain in young adult golfers: a preliminary study. Phys Ther Sports. 2005;6:122‐130. [Google Scholar]
- 38.Mellin G Correlations of hip mobility with degree of back pain and lumbar spinal mobility in chronic low‐back pain patients. Spine. June 1988;13(6):668‐670. [PubMed] [Google Scholar]
- 39.Gracovetsky SA Iacono S Energy transfers in the spinal engine. J Biomed Eng. April 1987;9(2):99‐114. [DOI] [PubMed] [Google Scholar]
- 40.Moreside JM MS Improvements in hip flexibility do not transfer to mobility in fucntional movement patterns J Strength Cond Res. 2013;27(10):2635‐2643. [DOI] [PubMed] [Google Scholar]
- 41.Kouyoumdjian P Coulomb R Sanchez T Asencio G Clinical evaluation of hip joint rotation range of motion in adults. Orthop Traumatol Surg Res. 2012;98(1):17‐23. [DOI] [PubMed] [Google Scholar]
- 42.Barbee‐Ellison JB RS, Sahrmann SA . Patterns of hip rotation range of motion: comparisons between healthy subjects and patients with low back pain. . Physical Ther. 1990;70:537–541. [DOI] [PubMed] [Google Scholar]
- 43.Cibulka MT Sinacore DR Cromer GS Delitto A Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint regional pain. Spine. May 1 1998;23(9):1009‐1015. [DOI] [PubMed] [Google Scholar]
- 44.Cibulka MT Strube MJ Meier D, et al. Symmetrical and asymmetrical hip rotation and its relationship to hip rotator muscle strength. Clin Biomech (Bristol, Avon). 2010;25(1):56‐62. [DOI] [PubMed] [Google Scholar]
- 45.Nussbaumer S Leunig M Glatthorn JF Stauffacher S Gerber H Maffiuletti NA Validity and test‐retest reliability of manual goniometers for measuring passive hip range of motion in femoroacetabular impingement patients. BMC Musculoskeletal Disord. 2010;11:194. [DOI] [PMC free article] [PubMed] [Google Scholar]