Abstract
Background
Interpretation of Lachman testing when evaluating the status of the anterior cruciate ligament (ACL) typically includes a numerical expression classifying the amount of translation (Grade I, II, III) in addition to a categorical modifier (Grade A [firm] or B [absent]) to describe the quality of the passive anterior tibial translation's endpoint. Most clinicians rely heavily on this tactile sensation and place value in this judgment in order to render their diagnostic decision; however, the reliability and accuracy of this endpoint assessment has not been well established in the literature.
Purpose
The purpose of this study was to determine the intertester reliability of endpoint classification during the passive anterior tibial translation of a standard Lachman test and evaluate the classification's ability to accurately predict the presence or absence of an ACL tear.
Study design
Prospective, blinded, diagnostic reliability and accuracy study.
Methods
Forty‐five consecutive patients with a complaint of knee pain were independently evaluated for the endpoint classification during a Lachman test by two physical therapists before any other diagnostic assessment. The 21 men and 24 women ranged in age from 20 to 64 years (mean +/‐ SD age, 40.7 +/‐ 14) and in acuity of knee injury from 30 to 365 days (mean +/‐ SD, 238 +/‐157).
Results
17 of the 45 patients had a torn ACL. The agreement between examiners on A versus B endpoint classification was 91% with a kappa coefficient of 0.72. In contrast, classification agreement based on the translational amount had an agreement of 65% with a weighted kappa coefficient of 0.52. The sensitivity of the endpoint grade alone was 0.81 with perfect specificity resulting in a positive likelihood ratio of 6.2 and a negative likelihood ratio of 0.19. The overall accuracy of the Lachman test using the endpoint assessment grade alone was 93% with a number needed to diagnose of 1.2.
Conclusions
Nominal endpoint classification (A or B) from a Lachman test is a reliable and accurate reflection of the status of the ACL. The true dichotomous nature of the test's interpretation (positive vs. negative) is well‐served by the quality of the endpoint during passive anterior tibial translation.
Level of Evidence
2
Keywords: ACL, anterior cruciate ligament, diagnosis, knee, Lachman test, reliability, sensitivity, specificity
Introduction
Physical examination of patients with knee injuries frequently involves assessment of ligamentous stability. One of the most common ligamentous injuries of the knee is to the anterior cruciate ligament (ACL) and the early recognition of the pathology is crucial in dictating the course of care in order to optimize outcomes. The Lachman test is characterized as the most direct and definitive evaluative technique used to determine the status of the ACL and is best performed prior to the onset of the patient's pain, swelling, and guarding.1-4
The Lachman test is the clinical examination gold standard for diagnosing this injury because of its well‐established sensitivity, specificity, and likelihood ratios; however, many clinicians also assign a categorical grade (modifier) to describe the endpoint of the passive anterior tibial translation. Traditionally, a grade of A is given when the endpoint is perceived to be “firm” while a grade of B is given if the endpoint is felt to be soft, absent, or ill‐defined. In fact, during instrumented arthrometry with a KT‐1000 ™, it has been suggested that the difference in the amount of translation that occurs between a 15 and 20‐lb stress (compliance index) is an objective measure of this phenomenon.5 However, the reliability, accuracy, and clinical utility of this assessment has not been subjected to critical investigation in the literature.
Previous authors have generally shown a suspect level of intra‐ and inter‐tester reliability in classifying the endpoint sensation of anterior tibial movement felt by the examiner. Based on the poor kappa values in a study evaluating endpoint agreement between an orthopedic surgeon and athletic trainers, Hurley et al6-7 concluded that that interpretation of manual clinical examination procedures is technique dependent, somewhat subjective, and open to bias and misinterpretation. Similarly, Cooperman et al8 found intertester agreement on judgments of tibial translation endpoint to be between 60 and 71% with kappa coefficients ranging from 0.19‐0.42 indicating moderate concurrence. When analyzed by discipline, physical therapists had an intertester kappa coefficient range of 0.02 to 0.69 with 53‐84% agreement. In contrast, orthopedic surgeons had kappa values of 0.38 ‐ 0.61 with an agreement range of 68‐81%. Limitations to these studies included inconsistent methods of conducting the test and limited expertise of the examiners. While examiners had appropriate qualifications and credentials, the significant improvement in second trials and/or the limited variability in their interpretation of results would hint at their relative inexperience with this specific type of testing.
Peeler et al9 also evaluated the reliability of Lachman testing in patients with arthroscopically confirmed ACL tears. They found therapists rely heavily on the findings of this test but only have moderate (Po = 0.55) agreement with primary care physicians and poor (Po = 0.32) agreement with orthopedic surgeons. The authors of this study did not specifically detail the translational quantity or quality rationale behind assigning a grade of positive or negative to the test's outcome. In a systematic review of the inter‐rater reliability for determining the endpoint to physiological knee movements, Currier et al10 and Hayes et al11 reported relatively low kappa values, ranging from ‐0.01 – 0.31 for knee flexion and 0.25 – 0.43 for knee extension. These studies evaluated intertester agreement for the resistance met at the end‐range of physiological, sagittal plane knee motions using a greater number of descriptors (normal, empty, stiff, or loose) as opposed to the dichotomous terms of firm or soft endpoint that is typically assigned to the ligamentous restraint offered at end‐range joint translation.
Despite this relatively poor level of agreement many clinicians utilize the tactile quality of the endpoint sensation felt during the passive tibial translation inherent to the traditional Lachman test. Because of the variance in the amount of translation between individuals, the abruptness of the translation's stopping point can be quite useful and may be predictive. In fact, Callaghan et al12 suggest that an absent or soft endpoint indicates the lack of anterior restraint, whereas a firm endpoint signifies a normal ACL. A firm endpoint in the presence of increased translation may represent a partial tear or a tear of the ACL's posterolateral bundle.13-15
Although both manual and instrumented assessments of tibial translation can provide relevant information, only the manual knee examination allows the examiner to “feel” the endpoint of motion. This is an important element of the evaluative process particularly in cases where there is significant inherent laxity of the uninvolved extremity. The general “rule of thumb” for interpreting ligamentous stability is to place more value on the quality of motion and endpoint distinctiveness as compared to the amount of laxity present.7 The characteristic firm endpoint is evidence of the normal check‐reign function of the ligamentous stabilizer while the presence of a soft or mushy endpoint indicates that the primary stabilizer has failed and joint stability is now the responsibility of secondary stabilizers. However, this assessment is somewhat subjective and dependent upon the examiner's skill and experience.7,16 A summary of the findings from the previous literature can be found in Table 1.
TABLE 1.
Literature Review Summary of Examiner Reliability and Accuracy of Lachman Testing for ACL status
| Study | Clinician | Agreement | Reliability (k) | Sensitivity |
|---|---|---|---|---|
| Hurley, 2002 | Athletic Trainers | 42‐83% | ‐ 0.40 ‐ 0.56 | 0.67 |
| Cooperman, 1990 | Physical Therapists | 53‐84% | 0.02 ‐ 0.69 | |
| Orthopedic Surgeons | 68‐81% | 0.38 ‐ 0.61 | ||
| Peeler, 2010 | Therapists vs. Primary Care Physicians: | Po = 0.55 | ||
| Therapists vs. Orthopedic Surgeons: | Po = 0.32 | |||
| Currier, 2007 | Physical Therapists | 0.25 ‐ 0.31 | ||
| Hayes, 2001 | Physical Therapists | ‐0.01 ‐ 0.43 |
k = kappa coefficient; Po – phi coefficient of association
The purpose of this study was to determine the intertester reliability of endpoint classification of passive anterior tibial translation and evaluate the classification's ability to accurately predict the presence or absence of an ACL tear. The hypothesis for this study was that reliance solely on endpoint feel of passive anterior tibial translation may yield reliable results and be accurate in detecting the presence or absence of a torn ACL.
METHODS
The reliability and accuracy of detecting the quality of the anterior translation endpoint during the Lachman test was evaluated on a sample of consecutive patients referred from the emergency room of a county teaching hospital to the orthopedic surgery sports medicine service for definitive evaluation of a painful knee. Patients between the ages of 18 and 64 with knee pain complaint rated verbally as under 8/10 on a numerical rating scale and possessing at least 20‐120˚ of range of motion were eligible for study inclusion. The study was approved by the institutional review boards at Parkland Health and Hospital System and the University of Texas Southwestern Medical Center in Dallas, TX. All patients agreed via informed consent to participate in the investigation. Study exclusion criteria were the suspicion of a fracture based on the Ottawa knee rule, 3,17 previous knee joint arthroplasty, suspicion of posterior cruciate ligament (PCL) involvement, knee surgery in the previous six months, the presence of serious underlying non‐mechanical pathology, or systemic illness.
The examination was conducted independently by two licensed physical therapists before any other diagnostic evaluation was performed, including injury history interview or review of previously conducted radiographic or magnetic resonance images. Therefore, the examiners had minimal previous knowledge regarding the patient's condition and complaint. The testing was conducted with each examiner blind to the other's findings. One physical therapist (EPM) had 34 years’ experience with evaluating knee stability and the other (DQM) was an orthopedic physical therapy resident with 1 year of experience. Two, 1‐hour training sessions for both examiners was conducted prior to data collection to enhance consistency in testing and interpretation.
After enrollment, each patient was brought to a private examination room where the testing was conducted. Weight‐bearing ambulation without an assistive device to the examination room satisfied one of the items of the Ottawa knee rules. Active knee flexion to at least 90 degrees and palpation for reproduction of pain complaint was conducted at the patella and fibular head in order to complete the Ottawa knee rule algorithm. If there were no adverse signs according to the knee rule the examiners proceeded to screen for PCL injury. PCL injury evaluation was conducted via visual and palpatory assessment of a tibial sag sign with knee flexed at 90 degrees. If the tibial plateau did not appear to be at least one centimeter (cm) anterior to the femoral condyle, a quadriceps active drawer test was applied to rule in PCL injury. The palpatory loss of the tibia‐femur step‐off relationship has been shown to be a sensitive (0.90) and specific (0.99) means by which to detect the presence of a PCL injury.18 The quadriceps active drawer test is performed by the patient gently contracting the quadriceps with the knee flexed at 90° and foot stabilized on the treatment plinth. The posterior displacement of the tibia will be reduced with this isometric contraction in the presence of a PCL tear. The specificity of this maneuver has been reported to be 96% and the sensitivity 53%.18-19 All preliminary exclusion tests were performed by the examiner who first performed the stability assessment and confirmed by the therapist with 34 year's experience (EPM).
Following PCL screening, each examiner independently assessed the patient for the quality of their anterior translation endpoint, amount of anterior displacement, and response to a pivot shift maneuver. The results of the Lachman test (quality and quantity of anterior translation) were classified by the criteria outlined in Table 2.1 If the movement of the tibia on the femur came to a sudden stop the result was described as an A, if not, the endpoint was classified as a B. The results of the pivot shift examination were not allowed to alter the previously recorded results of the Lachman test. The order for which of the examiners conducted the patient's ligamentous evaluation first was randomized. At the conclusion of the manual examination each patient was evaluated with the KT‐1000™ arthrometer (MEDmetric, San Diego, CA) to record the millimeters of anterior translation at 15, 20, and 30 pounds (6.8, 9.1, and 13.6 kg) of force by a single examiner (DQM). The KT‐1000™ is a mechanical joint arthrometer allowing for stabilization of the femur with concurrent instrumented assessment of the amount of the tibial translation when an anterior displacement force is applied to the proximal end of the lower leg. This device has been shown to be an accurate and appropriate gauge of sagittal plane tibial displacement in a research setting.20 Previous studies at the authors’ facility have shown that the examiners involved in the study have good test‐retest reliability in performing the KT‐1000™ examination with an intraclass correlation coefficient (3,1) of .90, .82, .88, and .78 at 15 pounds (6.8 kg), 20 pounds (9.1 kg), 30 pounds (13.6 kg), and at a manually applied maximal force.3 This reliability data is consistent with values reported in other studies.21-22
TABLE 2.
Test Grading Criteria for Lachman Testing Classification
| Translation Grade | Operational Definition |
|---|---|
| I | < 5 mm translation |
| II | 5 – 10 mm translation |
| III | > 10 mm translation |
| Endpoint Grade | Operational Definition |
| A | Firm, sudden endpoint to passive anterior translation of tibia on a fixed femur |
| B | Absent, ill‐defined, or softened endpoint to passive anterior translation of tibia on a fixed femur |
Ligamentous Testing Description
For all patients the uninvolved knee was evaluated first in order to establish a baseline by which the contralateral knee could be judged. The test was performed with the patient lying supine on a firm examination table and the knee flexed to 20‐30 degrees. Care was taken to ensure the both knees were in the same degree of flexion during the physical examination procedure. The examiner's upper hand stabilized the unsupported distal thigh, while the lower hand, with the thumb on the anterior joint line, and the fingers feeling to ensure that the hamstrings were relaxed, pulled the tibia forward with approximately 30 lbs of force. Based on palpatory, tactile, and visual sense, the examiner provided a numerical and letter grade based on the operational definitions recommended by Lubowitz et al2 and provided in Table 2. This classification was determined prior to testing for a pivot shift so as to not bias the findings of the examiners.
After each examiner had rendered their separate decision on the status of the ACL they compared their findings. In four patients, the examiners had different endpoint interpretations of the test. In these instances, it was determined a priori to defer to the judgment of the more experienced examiner for the diagnostic accuracy portion of the study.
The pivot shift test was also conducted with the patient in a supine position in a standard manner. The examiner graded the pivot shift as positive if the there was a “jump” or dramatic clunk as the tibiofemoral relationship reduced within the target range. Alternatively, a negative test was recorded if the there was a smooth tibiofemoral glide or “guarded” if the patient could not adequately relax their hamstrings to allow a passive assessment.
For 17 patients the gold standard for diagnostic accuracy was direct arthroscopic visualization of the ACL at the time of surgery. For the 28 patients for whom direct visual evidence through the arthroscope was not available, each patient's ACL status was categorized as intact or torn based on a cluster of clinical findings. To be classified as having a torn ACL, the patient had to have at least 2 of the 3 following findings: 1) a positive MRI; 2) excessive laxity on KT‐1000™ examination which was defined as more than 3 mm greater translation on the involved side during the instrumented assessment with the 30 lb (13.6 kg) and/or manual maximum test as compared to the uninvolved side; and 3) a positive finding on a subsequent independent and comprehensive knee ligamentous evaluation conducted by a physician who was blind to the original examiners’ findings and the patient's condition. If less than two of these findings were positive the patient's ACL status was classified as normal.
Fellowship trained orthopedic surgery and radiology investigators not involved in conducting the Lachman tests interpreted the MRI images and/or evaluated the ACL under arthroscopic visualization. No adverse events were reported for any of the patients during the index testing or evaluation of the reference standards.
Statistical Analysis
Cohen kappa (k) coefficients and percent agreement between examiners were used as estimates of inter‐rater reliability for endpoint classification. A weighted analysis for the k value was used to evaluate the inter‐rater reliability for the 3‐point ordinal classification on the amount of anterior translation on all subjects. Secondary to an anticipated high agreement rate in the gold standard group and a low prevalence of an intact ACL in patients who went on to surgery to address their knee complaint, a less divergent perspective of agreement, Gwet's AC1, was also calculated.24 The k value is a chance‐adjusted measure of agreement. A k of 0.00 represents agreement equivalent with random chance alone, whereas a k of 1.00 represents perfect agreement. A negative k represents worse than what would be expected due to chance alone, whereas a k of –1.00 represents complete discordance between observers. Analysis was performed using Agree‐Stat 2011 (Advanced Analytics, LLC, Gaithersburg, Maryland). Kappa values were interpreted according to the guidelines proposed by Landis and Koch.23 Excellent agreement is described for values between 0.81 and 1.00, good for values between 0.61 and 0.80, moderate for values between 0.41 and 0.60, fair for values between 0.21 and 0.40, and poor for values under 0.20.
A 2x2 contingency table protocol was used to evaluate the sensitivity, specificity, positive and negative predicative values, and likelihood ratios based solely on the endpoint translation classification of the Lachman test. Sensitivity represents the % of true positives in all patients with the reference injury and specificity represents the % of true negatives. Consequently, index tests with high sensitivity are thought to be effective at ruling out the presence of the injury while tests with high specificity are effective at ruling in the injury. Positive and negative predictive values reflect the percentage of time that a positive or negative test (respectively) accurately captures the diagnosis. Exact binomial confidence intervals for the positive and negative predictive values were determined by the Clopper‐Pearson method through an on‐line calculator at http://statpages.org/ctab2x2.html. Positive and negative likelihood ratios reflect changes in the post‐test probability when the index test is positive or negative (respectively). The confidence intervals for the sensitivity, specificity, and likelihood ratios were computed via an on‐line calculator at http://www.pedro.org.au/english/downloads/confidence‐interval‐calculator/ using the Wilson score method. The number needed to diagnose was derived from the formula 1/[sensitivity – (1/specificity)] and represents the number of tests that need to be performed to gain a positive response for the presence of the injury. There is no clear method for calculating the confidence intervals for this statistical measure.
RESULTS
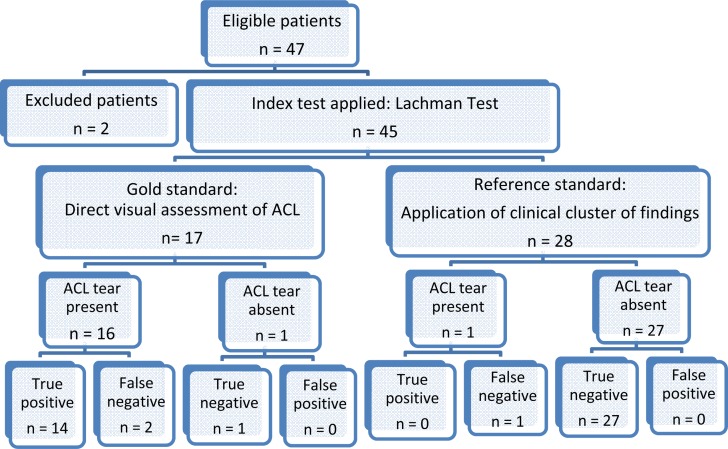
The Lachman test was prospectively evaluated on 47 consecutive patients between September of 2013 and February of 2014; however, only 45 of them were included in the study. Two patients were excluded whose pain level and guarding prevented anterior tibial translation assessment. Demographic information is presented in Table 3. Figure 1 summarizes the flow of the patients through the study. For 17 of the 45 patients the gold standard of arthroscopic direct visualization was used to classify the status of the ACL. In this subset of patients, 16 individuals had a torn ACL and one had an intact ACL. For the remaining 28 patients a clinical consensus of their imaging results, joint arthrometry examination, and clinical evaluation was used as the reference standard in determining which nominal description would be used to classify their actual physical finding. In this subset of patients there was one individual with a torn ACL and 27 with a normal ACL.
TABLE 3.
Demographic Data
| Characteristic | |
|---|---|
| Age [(mean years ± SD (range)] | 40.7 ± 14 (20‐64) |
| Side of Involvement (frequency) | 20 right; 25 left |
| Gender (frequency) | 21 male; 24 female |
| BMI [(mean ± SD (range)] | 30.9 ± 6.0 (20.9 – 48.1) |
| Mean Days since Injury [(mean days ± SD (range)] | 238 ± 157 (30 – 365) |
| Thigh circumference [(mean cm ± SD (range)] | 44.0 ± 6.6 (35.5 – 60) |
Figure 2.
Flow chart of eligible patients
The two examiners agreed on the A/B classification of the Lachman test 91% of the time with a Cohen's kappa coefficient value of 0.72 (95% CI 0.50‐0.95), indicating good agreement. For the classification on excessive translation (Grades I‐III), the two examiners agreed on the Lachman finding 65% of the time with a free margin kappa coefficient of 0.42 and a weighted kappa value of 0.52 indicating moderate agreement (Table 4). For the seventeen patients with the gold standard of direct visual evidence of an ACL tear, the examiners agreed on the endpoint classification 76% of the time (13 of 17) but the Cohen kappa value dropped to ‐0.09 indicating an agreement worse than expected by chance. However, the more appropriate alternate agreement coefficient, Gwet's AC1, rendered a kappa value of 0.70. .There was perfect concordance on endpoint (A or B) classification for the patient's categorized by the clinical cluster in contrast with a 63% agreement and kappa value of 0.16 – 0.25 when using translation grade criteria.
TABLE 4.
Intertester agreement and kappa coefficient values for the Lachman test
| All Patient Values n= 45 | Gold Standard Values n= 17 | Clinic Reference Standard Values n= 28 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Diagnostic Parameters | % Agreement | Kappa Coefficient (95% CI) | Gwet AC1* Kappa Coefficient (95% CI) | % Agreement | Kappa Coefficient (95% CI) | Gwet AC1 Kappa Coefficient (95% CI) | % Agreement | Kappa Coefficient | Gwet AC1 Kappa Coefficient |
| A/B Endpoint Classification | 91 | 0.72 (0.50‐0.95) | 0.81 (0.65 – 0.98) | 76 | −0.09 (0.50‐0.95) | 0.70 (0.37‐0.1.0) | 100 | 1.00 | 1.00 |
| Weighted Kappa Coefficient (95% CI) | Weighted Kappa Coefficient (95% CI) | Weighted Kappa Coefficient (95% CI) | |||||||
| I‐II‐III Translation Classification | 65 | 0.42 (0.16‐0.66) | 0.52 (0.29‐0.77) | 71 | 0.52 (0.10‐0.94) | 0.45 (0.00‐1.00) | 63 | 0.16 (0.00‐0.50) | 0.25 (0.00‐0.59) |
After blinded classification, the examiners met regarding the four patients in which they disagreed on endpoint classification and came to concurrence based on the senior examiner's expertise and experience. Overall, the examiners agreed on a rating of the Lachman endpoint as an A in 31 patients and B in 14.
Seventeen of the 45 patients in this study had a torn ACL resulting in a prevalence of 38%. Fourteen of the sixteen patients with an ACL tear identified by surgical observation were classified as an abnormal endpoint (B) resulting in a sensitivity of 0.88 (95% CI = 0.82 ‐ 0.88) (Table 5). All 27 of the patients classified as an intact ACL by the clinical cluster rule were classified as having a normal endpoint (A) during Lachman testing (Table 6). In the other two patients there was one true negative confirmed during surgery and one false negative based on the cluster criteria. For all patients’, regardless of means of classification, the sensitivity of endpoint classification was 0.81 (95% CI = 0.63 – 0.81) with perfect specificity yielding a positive likelihood ratio of infinity (95% CI = 6.2 ‐ ∞) and a negative likelihood ratio of 0.19 (95% CI = 0.19 – 0.41) (Table 7). In contrast, likelihood ratios based on the on the amount of translation classification were computed based on the classification of Grade I as an intact ACL and Grade II or III as a torn ACL. Using this dichotomy the sensitivity of the Lachman test was 0.94 (95% CI = 0.73 ‐1.00) but the specificity dropped to .83 (95% CI = 0.71 – 0.86) yielding a positive likelihood ratio of 5.4 (95% CI = 2.6 – 7.1) and a negative likelihood ratio of 0.08 (95% CI – 0.004 – 0.38) (Table 8). The overall accuracy of a soft endpoint classification was 93% accurate at predicting a torn ACL.
TABLE 5.
A/B Classification: 2 x 2 contingency table for patients who had direct visualization of anterior cruciate ligament status during surgical intervention
| Condition according to Gold Standard: Arthroscopic Visualization | ||||
|---|---|---|---|---|
| Positive | Negative | Totals | ||
| Condition according to A/B Endpoint Classification | Positive | 14 | 0 | 14 |
| Negative | 2 | 1 | 3 | |
| Totals | 16 | 1 | 17 | |
TABLE 6.
A/B Classification: 2 x 2 contingency table for patients for whom a clinical cluster of tests was used for the reference standard
| Condition according to Reference Standard: Clinical Cluster* | ||||
|---|---|---|---|---|
| Positive | Negative | Totals | ||
| Condition according to A/B Endpoint Classification | Positive | 0 | 0 | 0 |
| Negative | 1 | 27 | 28 | |
| Totals | 1 | 27 | 28 | |
To be classified as having a torn ACL, the patient had to have at least 2 of the 3 following findings: 1) a positive MRI; 2) excessive laxity (> 3mm) on KT‐1000™ examination; and 3) a positive finding on a subsequent independent and comprehensive knee ligamentous evaluation conducted by a
TABLE 7.
Lachman Endpoint A/B Classification: 2 x 2 contingency table for all patients
| Condition according to Reference or Gold Standard for all Subjects | ||||
|---|---|---|---|---|
| Positive | Negative | Totals | ||
| Condition according to A/B Endpoint Classification | Positive (B) | 13 | 0 | 13 |
| Negative (A) | 3 | 29 | 32 | |
| Totals | 16 | 29 | 45 | |
DISCUSSION
In a patient presenting with a possible injury to the ACL it is important to know the accuracy of the tests used to establish a diagnosis. Traditionally, the interpretation of the Lachman test reflects on both the quantity and quality of the tibial anterior translation on a fixed femur. The results of this study provide evidence that the quality aspect of the endpoint feel is a reliable finding, even in examiners with significant differences in experience, and can be used as a part of the comprehensive clinical examination to judge the ACL's ability to resist anterior tibial translation. In fact, it appears that the “soft” or “B” endpoint may be a pathognomonic finding relative to a torn ACL. It appears that the tactile sense of an abrupt halt to the passive anterior translation of the tibia on the femur represents a healthy, intact ACL whereas the soft, elastic sense represents the secondary stabilizers stopping the motion in absence of an intact ACL. This information may be as, if not more, useful than the amount of translation that is detected during the examination.
To further illustrate this point a post‐hoc analysis of the information used to determine the ACL's status was conducted. Using the endpoint classification criteria in isolation resulted in a sensitivity of 82% (three false negatives) and 100% specificity (no false positives). In contrast, if solely using the compliance index derived from the KT‐1000 evaluation to detect the status of the ACL, the sensitivity dropped to 53% (8 false negatives) and specificity to 92% (two false positives). The operational definition of the compliance index used for this analysis was a difference of greater than 1.5 mm in anterior translation between the 15 and 20 pound stress points during the Lachman test.5 Additionally, had the KT‐1000 data regarding the translation difference between knees had been applied to the operational definition of the Lachman grading scale the accuracy would have again dipped dramatically as seven subjects with torn ACLs had less than a 5 mm difference and the other 10 had between 5 and 10 mm of difference. None of the subjects with a torn ACL showed a KT‐1000 difference of greater than 10 mm in anterior translation. These finding support the notion that the interpretation of the “endpoint” results in a more accurate determination of the ligament's status than does the estimation of the amount of translation that is present during the examination technique.
The findings from this study are in contrast to the findings of Hurley et al6-7,25, Cooperman et al8, and Peeler et al9. It is unclear as to why these examiners had much less reliable impressions of the knee's anterior tibial translation. Possible explanations could include inconsistency in technique, unclear operational definitions and distinctions between soft and firm endpoints, and underutilization of the multiple sensory sources inherent to rendering the categorical assignment. While the examiners in the current study were blind to all relevant patient history and physical exam findings they were able to see the patient (age, athletic demeanor, knee morphology) and were allowed to utilize multiple sensory sources such as visual appreciation of the patellar tendon slope and tactile proprioceptive sense to arrive at their conclusion. Additionally, while not controlling for meniscal injury the authors did exclude patients with suspicion of a torn posterior cruciate ligament that may have displayed an exaggerated anterior translation from a posteriorly displaced position. The authors were not able to confirm that scarring of a torn ACL to the PCL presents in a unique manner (increased translation but firm, delayed endpoint) as suggested by Dhillon et al26 as there were not any subjects with tears with the finding of an abnormally reattached ACL. Finally, while the authors had numerous subjects with osteoarthritic knees, none of the patients had Kellgren Lawrence scores of greater than 2 or the presence of large or multiple osteophytes which could have confounded the clarity of the endpoint classification.27 In fact, two of the three false negatives were in patients with more advanced arthritic findings. Other commonalities in the patients with a false negative were bilateral excessive laxity to anterior tibial translation, complex meniscal pathologies, and one patient that had a healed, partial tear of the ACL. The patient with the partial tear may have had the “delayed” firm endpoint but was classified by the examiners as a 2A yet grouped with the “torn” ACL cohort.
There are limitations to this study design. Reflection from only two examiners on 45 consecutive patients with variable levels of injury acuity should only be considered a starting point in the discussion on Lachman grading and interpretation. The authors’ also acknowledge only partial blinding as the examiners could see the patient and their injured knee during the examination. By design, the applications and external validity of this study's findings should be quite broad. This study population represented a diverse population of knee pain complaints and would generally be considered to represent a chronologically older and more chronic status when compared to the typical population of patients with a primary concern of ACL deficiency. Additionally, this study does not offer significant diagnostic insight for the patient with partial tears of the ACL or in circumstances where ACL tear has scarred into the notch or PCL.
Based on the current findings the authors would propose that the two‐tier classification scheme (translation grade and endpoint quality) proposed by the American Medical Association28 over 40 years ago is unnecessarily complicated and may decrease reliability. Lachman testing can be reliably and accurately interpreted as either positive (“torn”) or negative (“intact”) based on the tibial translation endpoint. The amount of translation is not as reliable an assessment and does not change or add to the decision‐making in how to manage the patient's pathology. The vast majority of the patients (>80%) in this study could have been classified as either 1A (intact) or 2B (torn).
CONCLUSION
The results of this study indicate that the examiners were able to reliably detect and categorize the quality of endpoint to anterior tibial translation better than the actual magnitude of translation and the nature of the endpoint classification was very accurate in predicting the histological status of the anterior cruciate. In conjunction with the clinical or instrumented judgment of translation, the Lachman examination technique should highly value the identification of an abnormal endpoint in the determination of the status of the ACL. The dichotomous nature of the Lachman test, as was its original intent, is a reliable and reasonably accurate clinical test of the integrity of the ACL.29
REFERENCES
- 1.Benjaminse A Gokeler A van der Schans CP Clinical diagnosis of an anterior cruciate ligament rupture: a meta‐analysis. J Orthop Sports Phys Ther. 2006 May;36(5):267‐88. [DOI] [PubMed] [Google Scholar]
- 2.Lubowitz JH Benardini BJ Reid JB Current concepts review: comprehensive physical examination for instability of the knee. Am J Sports Med. 2008 Mar; 36(3):577‐94. [DOI] [PubMed] [Google Scholar]
- 3.Mulligan EP Harwell JL Robertson WJ Reliability and diagnostic accuracy of the Lachman test performed in a prone position. J Orthop Sports Phys Ther. 2011 Oct;41(10):749‐57. [DOI] [PubMed] [Google Scholar]
- 4.Scholten RJ Opstelten W van der Plas CG Bijl D Deville WL Bouter LM Accuracy of physical diagnostic tests for assessing ruptures of the anterior cruciate ligament: a meta‐analysis. J Fam Pract. 2003 Sep;52(9):689‐94. [PubMed] [Google Scholar]
- 5.Daniel DM Stone ML Sachs R Malcom L Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med. 1985 Nov‐Dec;13(6):401‐7. [DOI] [PubMed] [Google Scholar]
- 6.Hurley WL Agreement of clinical judgments of endfeel between 2 sample populations. J Sport Rehabil. 2002; 11:209‐223. [Google Scholar]
- 7.Hurley WL McGuire DT Influences of clinician technique on performance and interpretation of the Lachman test. J Athl Training. 2003. 38(1): 34‐43. [PMC free article] [PubMed] [Google Scholar]
- 8.Cooperman JM Riddle DL Rothstein JM Reliability and validity of judgments of the integrity of the anterior cruciate ligament of the knee using the Lachman's test. Phys Ther. 1990 Apr; 70(4): 225‐33. [DOI] [PubMed] [Google Scholar]
- 9.Peeler J Leiter J MacDonald P Accuracy and reliability of anterior cruciate ligament clinical examination in a multidisciplinary sports medicine setting. Clin J Sports Med. 2010. 20(2):80‐85. [DOI] [PubMed] [Google Scholar]
- 10.Currier LL Froehlich PJ Carow SD McAndrew RK Cliborne AV Boyles RE Mansfield LT Wainner RS Development of a clinical prediction rule to identify patients with knee pain and clinical evidence of knee osteoarthritis who demonstrate a favorable short‐term response to hip mobilization. Phys Ther. 2007 Sep;87(9):1106‐19. [DOI] [PubMed] [Google Scholar]
- 11.Hayes KW Petersen CM Reliability of assessing end‐feel and pain and resistance sequence in subjects with painful shoulders and knees. J Orthop Sports Phys Ther. 2001 Aug;31(8):432‐45. [DOI] [PubMed] [Google Scholar]
- 12.Callaghan JJ Rosenberg AG Rubash HE Simonian PT Wickiewicz TL The Adult Knee. Lippincott Williams & Wilkins. Philadephia, 2003. [Google Scholar]
- 13.Dejour D Ntagiopoulos PG Saggin PR Panisset JC The diagnostic value of clinical tests, magnetic resonance imaging, and instrumented laxity in the differentiation of complete versus partial anterior cruciate ligament tears. Arthroscopy. 2013 Mar;29(3):491‐9. [DOI] [PubMed] [Google Scholar]
- 14.Furman W Marshall JL Girgis FG The anterior cruciate ligament. A functional analysis based on postmortem studies. J Bone Joint Surg Am. 1976 Mar;58(2):179‐85. [PubMed] [Google Scholar]
- 15.Petersen W Zantop T Partial rupture of the anterior cruciate ligament. Arthroscopy. 2006 Nov;22(11):1143‐5. [DOI] [PubMed] [Google Scholar]
- 16.Tsai AG Musahl V Steckel H Bell KM Zantop T Irrgang JJ Fu FH Rotational knee laxity: reliability of a simple measurement device in vivo. BMC Musculoskelet Disord. 2008 Mar. 18;9:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stiell IG Greenberg GH Wells GA McDowell I Cwinn AA Smith NA, et al. Prospective validation of a decision rule for the use of radiography in acute knee injuries. JAMA. 1996;275:611‐5. [PubMed] [Google Scholar]
- 18.Rubenstein RA Shelbourne KD McCarroll JR VanMeter CD Rettig AC The accuracy of the clinical examination in the setting of posterior cruciate ligament injuries. Am J Sports Med. 1994. 22(4):550‐557. [DOI] [PubMed] [Google Scholar]
- 19.Kopkow C Freiberg A Kirschner S Seidler A Schmitt J Physical examination tests for the diagnosis of posterior cruciate ligament rupture: a systematic review. J Orthop Sports Phys Ther. 2013 Nov;43(11):804‐13. [DOI] [PubMed] [Google Scholar]
- 20.Pugh L Mascarenhas R Arneja S Chin PY Leith JM Current concepts in instrumented knee‐laxity testing. Am J Sports Med. 2009 Jan;37(1):199‐210. [DOI] [PubMed] [Google Scholar]
- 21.Hanten WP Pace MB Reliability of measuring anterior laxity of the knee joint using a knee ligament arthrometer. Phys Ther. 1987;67:357‐59 PMID: 3823149 [DOI] [PubMed] [Google Scholar]
- 22.Wroble RR Van Ginkel LA Grood ES Noyes FR Shaffer BL Repeatability of the KT‐1000 arthrometer in a normal population. Am J Sports Med. 1990;18:396‐99. [DOI] [PubMed] [Google Scholar]
- 23.Landis JR Koch GG The measurement of observer agreement for categorical data. Biometric. 1977 Mar;. 33(1):159‐74. [PubMed] [Google Scholar]
- 24.Gwet KL Computing inter‐rater reliability and its variance in the presence of high agreement. Br J Math Stat Psychol. 2008 May;61(Pt 1):29‐48. [DOI] [PubMed] [Google Scholar]
- 25.Hurley WL Denegar C Buckley WE The relationship between grading and instrumented measurements of anterior knee joint laxity. J Sport Rehabil. 2008 Feb;17(1):60‐7. [DOI] [PubMed] [Google Scholar]
- 26.Dhillon AK Al‐Dadah O Servant CT Diagnostic accuracy of ACL tears according to tear morphology. Acta Orthop Belg. 2013 Feb;79(1):76‐82. [PubMed] [Google Scholar]
- 27.Johnson AJ Howell SM Costa CR Mont MA The ACL in the arthritic knee: how often is it present and can preoperative tests predict its presence? Clin Orthop Relat Res. 2013 Jan;471(1):181‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Medical Association. Standard nomenclature of athletic injuries. Chicago, American Medical Association, 1968. [Google Scholar]
- 29.Torg JS Conrad W Kalen V Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med. 1976 Mar‐Apr;4(2):84‐93. [DOI] [PubMed] [Google Scholar]