Abstract
AIM: To describe the electrocardiographic (ECG) phenomena characterized by T-wave inversion in the precordial leads in adults and to highlight its differential diagnosis.
METHODS: A retrospective chart review of 8 adult patients who were admitted with ECG T-wave inversion in the anterior chest leads with or without prolongation of corrected QT (QTc) interval. They had different clinical conditions. Each patient underwent appropriate clinical assessment including investigation for myocardial involvement. Single and multimodality non-invasive, semi-invasive and invasive diagnostic approach were used to ascertain the diagnosis. The diagnostic assessment included biochemical investigation, cardiac and abdominal ultrasound, cerebral and chest computed tomography, nuclear medicine and coronary angiography.
RESULTS: Eight adult subjects (5 females) with a mean age of 66 years (range 51 to 82) are analyzed. The etiology of T-wave inversion in the precordial leads were diverse. On admission, all patients had normal blood pressure and the ECG showed sinus rhythm. Five patients showed marked prolongation of the QTc interval. The longest QTc interval (639 ms) was found in the patient with pheochromocytoma. Giant T-wave inversion (≥ 10 mm) was found in pheochromocytoma followed by electroconvulsive therapy and finally ischemic heart disease. The deepest T-wave was measured in lead V3 (5 ×). In 3 patients presented with mild T-wave inversion (patients 1, 5 and 4 mm), the QTc interval was not prolonged (432, 409 and 424 msec), respectively.
CONCLUSION: T-wave inversion associated with or without QTc prolongation requires meticulous history taking, physical examination and tailored diagnostic modalities to reach rapid and correct diagnosis to establish appropriate therapeutic intervention.
Keywords: T-wave inversion, Coronary angiography, Pulmonary computed tomography angiography, Magnetic resonance imaging, Differential diagnosis
Core tip: Myriad of clinical conditions have been described in association with T-wave inversion in the anterior precordial leads. T-wave inversion associated with or without corrected QT prolongation may be encountered in a variety of clinical conditions. In the reversible (dynamic) types such as vascular coronary, cerebral and pulmonary disorders; metabolic disturbances and acute adrenergic stress cardiomyopathy; resolution of T-wave inversion may occur after days, weeks, months or years following the index event. Tailored diagnostic approach should be conducted avoiding overuse of diagnostic methods. Specific tailored therapeutic interventions were undertaken when high index of clinical suspicion was raised towards certain disease entity.
INTRODUCTION
T-wave inversion is found in 1% of patients admitted to the coronary care unit[1] and in 14% of patients presented with unstable angina[2]. It has been stated that T-wave inversion in right precordial leads is relatively rare (0.5%) in the general population and not associated with adverse outcome[3]. The tendency to inversion of T-wave declines with increasing age. Normally in females, the T-wave in V3 may be shallowly inverted. But in adult males, it is considered pathologic if the T-wave is inverted in V3-6[4]. The T-wave in V1 may be inverted normally at any age and in V2 it is sometimes normally negative[5].
Generally, the T-waves are negative in leads aVR, V1 and III. Giant T-wave inversion in the precordial leads are seen in different pathologies, such as anterior myocardial wall ischemia in patients with acute coronary syndrome, apical hypertrophic cardiomyopathy, cerebral and pulmonary disorders and post-pacing or tachyarrhythmia states.
The definite diagnosis in the presence of inverted T-wave can usually be assessed by meticulous history taking including family history of sudden cardiac death or arrhythmias, physical examination as well as appropriate non-invasive, semi-invasive or invasive diagnostic investigations. This current review, will focus on T-wave inversion in the anterior chest wall leads and discuss its differential diagnosis with emphasis on the non-coronary non-cardiac disorders.
Diagnostic approach should be tailored according to the clinical presentation, medical and family history. We present a Dutch case series of eight patients with T-wave inversion in the precordial leads due to different etiologies and the literature is briefly reviewed.
MATERIALS AND METHODS
The study was reviewed and approved by the Hospital Group Twente, Institutional Review Board. All study participants provided verbal informed consent.
Eight representative adult patients were identified and evaluated. In all patients, physical examination, electrocardiography and transthoracic echocardiography (TTE) were routinely performed. When necessary for adequate clarification of the clinical presentation, tailored diagnostic methods were undertaken in the individual patient at the clinician’s discretion [TTE, n = 8; coronary angiography “coronary angiography (CAG)”, n = 7; magnetic resonance imaging "magnetic resonance imaging (MRI)", n = 3; perfusion-ventilation scan, n = 2; computed tomography “computed tomography (CT)” abdomen, n = 1; CT brain, n = 1; CT thoracic aorta, n = 1; 123Iodine-metaiodibenzylguanidine (MIBG) scan, n = 1 and DOPA- positron emission tomography (PET), n = 1].
Diagnostic criteria
The diagnostic criteria included presentation with T-wave inversion in the anterior chest leads on the admission ECG.
Definitions
Electrocardiography: The admission ECGs were analyzed using standard criteria for measurements of T-wave axis, T-wave amplitude and QT interval. ECGs were analyzed for the presence of Left ventricular hypertrophy (LVH) using the Sokolow criteria[6].
T-wave negativity: was defined as a voltage of giant negative T-wave ≥ 10 mm in any of the leads[7-9], deep ≥ 5 mm[8] and mild 1-3 mm[8].
Corrected QT prolongation: Corrected QT (QTc) interval for heart rate was performed in V2 and was defined as QTc > 450 msec. according to Bazett[10] and Ahnve[11].
Measured serum biomarkers were creatine kinase and cardiac troponin T.
Transthoracic echocardiography: Left ventricular (LV) wall thickness as well as septal thickness were measured according to the established standards and guidelines of the American College of Cardiology/American Heart Association/European Society of Cardiology[12,13]. LVH was defined as a LV wall thickness > 13 mm.
Radionuclide studies: Radionuclide imaging and positron emission tomography: One patient (patient 7) underwent 123I-MIBG and dihydroxyphenylalanine-Positron Emission tomography (DOPA-PET) scanning. In 2 patients, pulmonary perfusion/ventilation scintigraphy were performed.
Computed tomography: Abdominal, cerebral and thoracic aorta CT scanning were performed in one patient each.
Pulmonary computed tomography angiography (PCTA) was performed in one patient.
Coronary angiography contrast angiography was performed in standard views via the femoral approach.
Follow-up: Follow-up was obtained by direct contact with patients, their physicians or by chart review.
Statistical analysis
No statistical data are available.
RESULTS
A total of 8 adult patients presented with chest pain and negative T-wave in the anterior chest wall leads on the admission ECG were identified (Figures 1-8).
Figure 1.
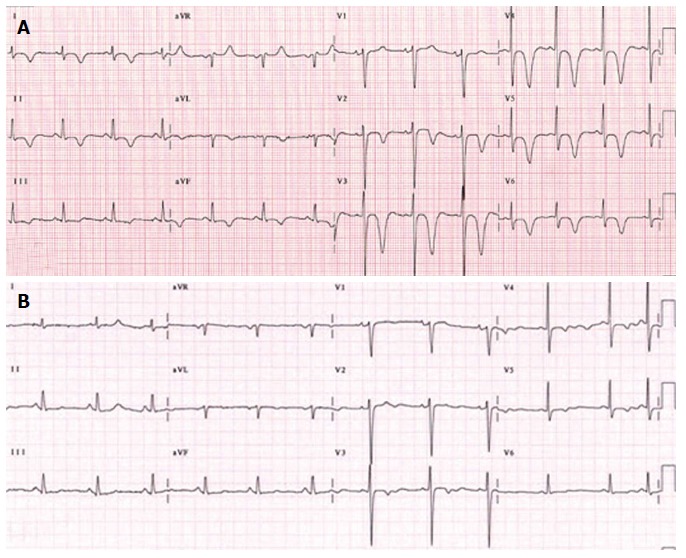
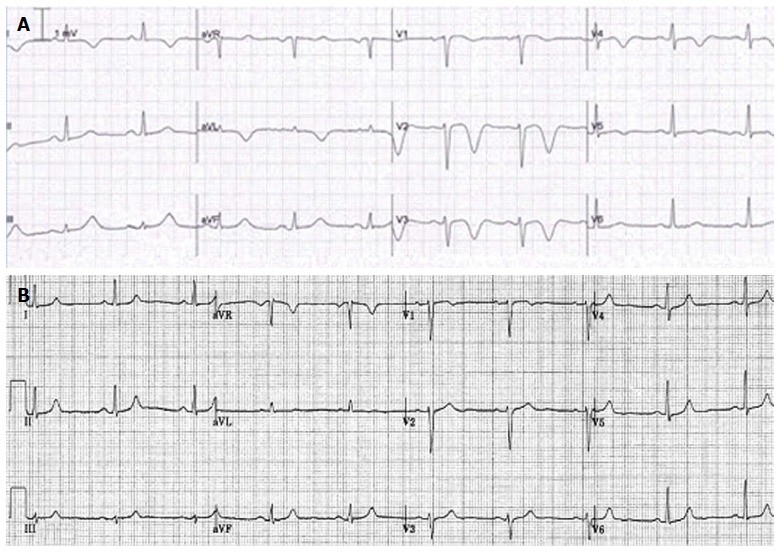
Patient 1. A: An electrocardiographic (ECG) tracing, illustrating the negative T-wave in the precordial leads V2-6, of a 51-year-old-female patient presented with palpitation following electroconvulsive therapy for her depression. In 2001, she underwent catheter ablation for atrioventricular nodal reentry tachycardia. She complained of palpitation after a shock of electroconvulsive therapy for treatment of depression. Post-electroconvulsive therapy, the ECG showed giant T-wave inversion in the precordial leads. The cardiac enzymes were minimally raised. Takotsubo cardiomyopathy is suggested due to emotional stress and electrical shock. Transthoracic echocardiography demonstrated apical hypokinesia and basal normokinesia with trivial valvular regurgitation without massive pericardial effusion. The estimated right ventricular systolic pressure was 35 mmHg. Coronary angiography and cardiac magnetic resonance imaging demonstrated normal findings. Medical treatment with beta blocker was initiated and the symptoms disappeared and (B) the ECG returned to base line in 2 wk time. The antidepressant drug was not discontinued.
Figure 8.
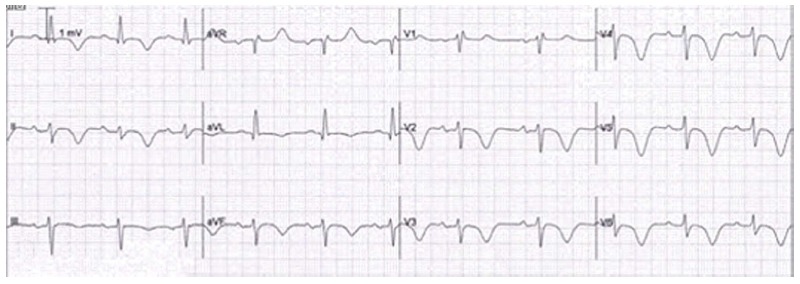
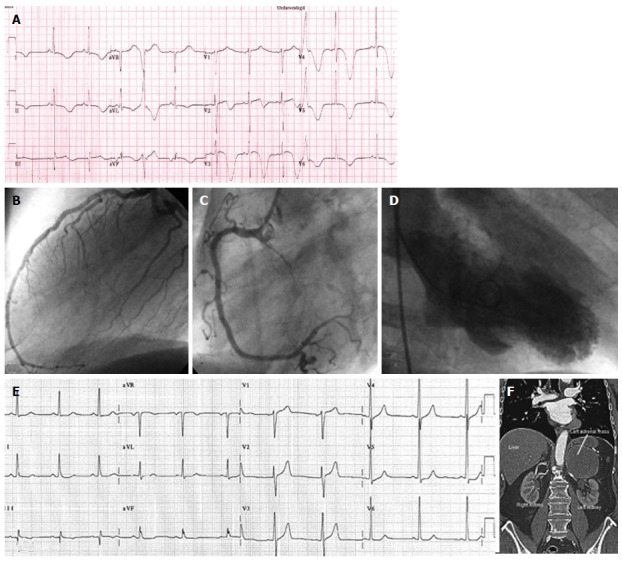
Patient 8. Electrocardiographic (ECG) tracing, demonstrating negative T-wave in the precordial leads V1-5, microvoltage in the standard leads and an Epsilon wave (arrow) which can be appreciated on magnification of ECG lead V2, of a 73-year-old man, amateur marathon runner after successful resuscitation for OHCA due to ventricular fibrillation. His coronary angiography and transthoracic echocardiography were normal. Genetic counseling revealed mutation 1238C > A (Tyr616X) in the plakophilline2 gen, compatible with AC. He refused implantable cardioverter defibrillator implantation and remained on medical treatment including class III antiarrhythmic drug. He was advised to refrain from marathon running and other strenuous exercise.
Figure 2.
Patient 2. An electrocardiographic (ECG) tracing, illustrating the negative T-wave with minimal ST segment elevation in the precordial leads V1-4, of a 82-year-old-female patient presented with acute coronary syndrome due to non ST elevation myocardial infarction. Her previous medical history included hormonal substitution for hypothyroidism, ablatio retinae, polymylagia rheumatica, arterial hypertension, mild concentric left ventricular hypertrophy, aortic valvular stenosis with a peak gradient of 18 mmHg and mild aortic regurgitation grade 2/4. In 2011, analysis with ambulatory ECG recording for a syncopal attack revealed no abnormalities. Transthoracic echocardiography demonstrated apicoinferior hypokinesia. The patient was treated medically and remained free of symptoms. Her maintenance drug therapy consisted of BB, aspirin (ASA), clopidogrel, Angiotensin-II antagonist, prednisolon, diuretic and statin.
Figure 3.
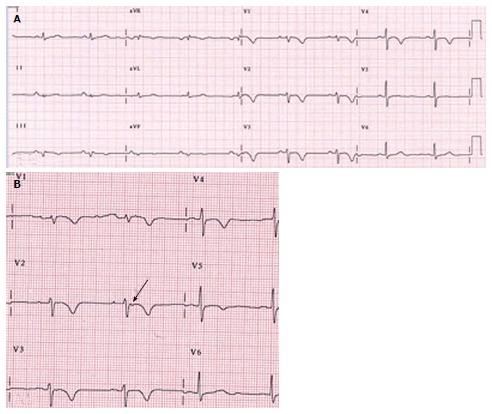
Patient 3. An electrocardiographic (ECG) tracing, illustrating the negative T-wave in the precordial leads V2-6, of a 72-year-old-woman who underwent 6 mo earlier direct current electric cardioversion for persistent atrial fibrillation. Her concomitant medical history includes temporal arteritis, carotid endarterectomy and cluster headache. She presented with abnormal rest ECG during out-patient follow-up. Her spouse died 2 wk prior to presentation. The cardiac markers were minimally elevated. The diagnosis of Takotsubo cardiomyopathy was strongly suggested as the emotional stress may have been the trigger. Transthoracic echocardiography depicted biventricular normokinesia with hypertrophic LV. Pulmonary perfusion-ventilation scintigraphy, Coronary angiography and cardiac MRI were all normal. She did well on pharmacological treatment with oral vit K antagonist, class 3 antiarrhythmic drug, anti-depressive drug and diuretics. The ECG alterations returned to baseline over a 6 mo period.
Figure 4.
Patient 4. A: An electrocardiographic (ECG) tracing, demonstrating negative T wave in the precordial leads V2-5, of a 69-year female patient with past medical history of transient ischemic attack two years previously, presented with interscapular pain. She had no emotional or physical stress. Normal results were found on transthoracic echocardiography, perfusion-ventilation scintigraphy, Coronary angiography and cardiac MRI. Brain CT scan revealed mild cerebral atrophy and minimal ischemic changes; B: The ECG showed spontaneous regression in 2 mo time. The etiology of the negative T wave inversion remains undetermined. Her medical regimen included aspirin, beta blocker, statin and diuretic.
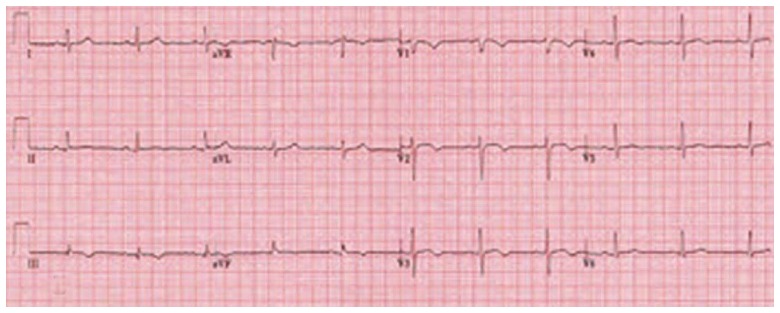
Figure 5.
Patient 5. An electrocardiographic (ECG) tracing, showing negative T wave in the precordial leads V1-3 and S1 Q3 T3, of a 55-year obese male patient without antecedent medical history presented with chest pain and minimally elevated serum cardiac biomarkers. Transthoracic echocardiography revealed dilated and hypokinetic RV with pulmonary hypertension and distended inferior caval vein. Coronary angiography was normal and pulmonary CT angiography confirmed the clinical diagnosis showing massive bilateral pulmonary embolism with central and peripheral localization. A continuous positive airway pressure was implemented for newly detected severe obstructive sleep apnea syndrome. He was successfully treated with medical regimen and on follow-up he became asymptomatic and the abnormal ECG findings gradually disappeared.
Figure 6.
Patient 6. An electrocardiographic (ECG)tracing, showing voltage criteria for left ventricular hypertrophy with ST depression and negative T wave in the precordial and inferior leads V3-6, of a 52-year female patient with non-obstructive hypertrophic cardiomyopathy (thickness of septum 20 mm and posterior wall of 24 mm without septal anterior movement or obstruction of outflow tract). Normal coronary arteries were found on coronary angiography. She refused genetic counseling and invasive intervention. She was treated medically with beta blocker.
Clinical features
On presentation, the blood pressure was normal in all patients and all were in sinus rhythm (Table 1). Cerebral pathology was excluded by the absence of neurological signs. No neurological deficits were found.
Table 1.
Demographic features, clinical presentations, diagnostic modalities and management
| Case/ gender/ age | Clinical presentation | ECG (SR) T-wave inversion | QTc (msec) | Associated disorders | TTE | Diagnostic modalities | Management | Condition |
| 1- F51 | Palpitation | 15 mm in V2-6 | 452 | AVNRT Depression | Apical hypokinesia | TTE CAG MRI | MM | Post-ECT. TTC (electrical stress) |
| 2-F82 | Chest pain | 10 mm in V1-4 | 484 | Mild AS PG 18 mmHg | Apicoinferior hypokinesia LVH | TTE | MM | NSTEMI |
| 3-F72 | Abnormal rest ECG | 5 mm in V2-6 | 553 | PAF 2011 Temporal arteritis Carotid endarterectomy Cluster headache | LVH | TTE CAG PV scan MRI | MM | TTC (emotional stress, spouse died 2 wk earlier) |
| 4-F69 | Inter-scapular pain | 9 mm in V2-5 | 520 | TIA 2010 | Normal | TTE CAG PV scan MRI CT brain | MM | Undetermined |
| 5-M55 | Chest pain | 1 mm in V1-3 S1 Q3 T3 | 432 | - | Dilated hypokinetic RV ePAP 75-80 mmHg | TTE CAG PCTA | MM | Pulmonary embolism |
| 6-F52 | Fatigue | 5 mm in V3-6 | 409 | - | LVH | TTE CAG | MM | HCM |
| 7-M76 | Left abdominal pain and psychomotor agitation | 20 mm in V2-6 | 639 | IMI 1990 PCI RCA 1990 and 2004 PCI LAD 1991 | Apical Hypokinesia LVH | TTE CAG CT thoracic aorta Ultrasound abdomen CT abdomen 123I-MIBG DOPA-PET Pathology | Surgical left adrennalectomy MM | TTC. Pheochromocytoma (hormonal stress) |
| 8-M73 | VF, OHCA | Epsilon V2 4 mm in V1-5 | 424 | Negative family history | RV dilatation | TTE CAG Genetic counseling | MM, AAD Refused ICD implantation Advise to refrain from strenuous exercise | ARVC/D |
AAD: Antiarrhythmic drug; ARVC/D: Arrhythmogenic right ventricular cardiomyopathy/dysplasia; AS: Aortic valvular stenosis; AVNRT: Atrioventricular nodal reentry tachycardia; BB: Beta blocker; CAD: Coronary artery disease; CAG: Coronary angiography; ECT: Electroconvulsive therapy; MM: Medical management; CRB: Calcium reentry blocker; CT: Computed tomography; ePAP: Estimated pulmonary artery pressure; F: Female; HCM: Hypertrophic cardiomyopathy; IMI: Inferior myocardial infarction; LAD: Left anterior descending coronary artery; LVH: Left ventricular hypertrophy; M: Male; MRI: Magnetic resonance imaging; NSTEMI: Non ST elevation myocardial infarction; OHCA: Out of hospital cardiac arrest; PAF: Persistent atrial fibrillation; PCI: Percutaneous coronary intervention; PCTA: Pulmonary computed tomography angiography; PET-CT: Positron emission tomography-computed tomography; PG: Peak gradient; PV scan: Perfusion-ventilation scan; RCA: Right coronary artery; RV: Right ventricle; SR: Sinus rhythm; TIA: Transient ischemic attack; TTC: Takotsubo cardiomyopathy; TTE: Transthoracic echocardiography; VF: Ventricular fibrillation; ECG: Electrocardiographic.
All patients had on physical examination no neurological abnormalities. One patient known with a previous transient ischemic attack showed a complete recovery. Of the 8 patients, one presented with abnormal rest ECG, three with chest pain, one with palpitation, one with fatigue, one with left abdominal pain and psychomotor agitation and one with out-of-hospital cardiac arrest (OHCA).
None of the patients, except one (patient 8) performed endurance sports activities all had no family history of sudden cardiac death or arrhythmias.
Electrocardiography
The admission ECGs were analyzed using standard criteria for measurements of T-wave amplitude and QTc interval. Giant T-wave inversion (≥ 10 mm) was found in the patients with pheochromocytoma (20 mm) followed by electroconvulsive therapy (15 mm) then ischemic heart disease (10 mm). Deep T-wave inversion (≥ 5 mm) was detected in three and mild (1-3 mm) in two of the patients. The deepest T-wave was measured in lead V3 (5 ×), V4 (2 ×) and V2 (1 ×). Epsilon wave was present in one patient with arrhythmogenic right ventricular cardiomyopathy/dysplasia (ARVC/D) (patient 8) (Figure 8B). Electrocardiographic criteria for left ventricular hypertrophy was found in 4 patients (patients 2, 3, 6 and 7).
In 3 patients diagnosed with pulmonary embolism (PE) (patient 5), LVH (patient 6) and ARVC/D (patient 8) presented with mild T wave inversion (1, 5 and 4 mm), the QTc interval was not prolonged (432, 409 and 424 msec), respectively.
Corrected QT prolongation
Corrected QT prolongation defined as QTc > 450 msec. measured in lead V2. The corrected QT interval exceeded 450 ms in 5 (452-639) with a mean of 530 ms and it was not prolonged in 3 (409, 424 and 432 ms) of the patients. The amplitude of the inverted T-wave varied significantly with the maximum negative T-wave amplitude ranging from one to 20 mm. A gradual complete resolution of the T-wave inversion and QT prolongation occurred in 5 of the patients.
Other ECG findings were as follow: two patients (patients 2 and 3) showed first degree AV block, one patient (patient 8) revealed microvoltage in the standard and limb leads, negative T wave in I and aVL in 2 patients (patients 4 and 7), negative T wave in leads I, II, III, aVL and aVF in (patients 1 and 3), negative T wave in II, III and aVF without (patient 5) or with (patient 6) ST segment depression.
Serum biomarkers
Cardiac troponin T were assessed. Myocardial infarction was ruled out in 7 patients. One (patient 2) with non ST elevation myocardial infarction (NSTEMI) showed typical biomarker rise and fall course with markedly elevation of troponin level. Mild elevation of troponin value was found in 4 patients (patients 3, 4, 5 and 7). No elevation was detected in 3 patients (patients 1, 6 and 8).
Transthoracic echocardiography
Transthoracic echocardiography was performed in all patients. Mild and moderate tricuspid regurgitation was detected in 6 (patients 1, 3, 4, 5, 6 and 7) and one (patient 2) of the patients, respectively. In 3 patients (patients 2, 3 and 7) trivial aortic regurgitation was present. Mild and moderate mitral regurgitation was demonstrated in 4 (patients 3, 4, 5 and 7) and 3 (patients 1, 2 and 6) patients, respectively. Dilatation of the right ventricle (RV) was demonstrated in one patient (patient 8). In five patients (patients 1, 2, 3, 4 and 5) the estimated RV systolic pressure was 35, 28, 35, 32 and 59 mmHg, respectively. Echocardiographic criteria for LVH was found in 4 patients (patients 2, 3, 6 and 7). Apical hypokinesia was detected in two patients (patients 1 and 7).
Cardiac magnetic resonance imaging
Cardiac magnetic resonance imaging was performed in three patients (patients 1, 3 and 4). All had normal findings.
Pulmonary computed tomography angiography
Pulmonary computed tomography angiography was performed in one patient (patient 5). Tailored individual diagnostic investigation was performed. In 2 patients (patients 3 and 4), pulmonary perfusion/ventilation scintigraphy were performed and pulmonary embolism was ruled out.
Computed tomography
Abdominal CT scan was performed in one which revealed an abdominal mass in the left adrenal region, a CT scan of the thoracic aorta excluding acute aortic dissection (patient 7) and brain CT scan in another (patient 4) showing mild atrophy and minimal ischemic changes.
Radionuclide imaging and positron emission tomography
One patient (patient 7) underwent 123I-MIBG scan and DOPA-PET scanning. This revealed MIBG uptake in the left adrenal region and a solitary lesion was detected at the left adrenal area with central necrosis with DOPA-PET scanning.
Coronary angiography
Seven patients underwent selective contrast angiography which revealed non-obstructive coronary artery disease in one patient and normal coronary arterial tree in 6 patients.
Follow-up: Follow-up was obtained by direct contact with patients, general practitioner, their physicians or by chart review.
DISCUSSION
In middle-aged subjects, T-wave inversion in the precordial leads is relatively rare in the general population occurring in 0.5% (54/10899[3] of the subjects. T-wave inversion in the anterior chest wall leads is relatively common in children and adolescents[9] but infrequently found in healthy adults and is considered as “normal variants”[4]. This pattern is more common in young females and young adults (1%-3%)[14,15]. The prevalence was associated with gender difference, which was higher (0.9%) in women than in men (0.1%)[3].
Primary and secondary T-wave abnormalities
Primary T-wave abnormalities (ischemia or injury) are due to alterations in myocardial cellular electrophysiology and secondary T-wave abnormalities (bundle branch block or ventricular Hypertrophy) are subsequent to alterations of sequence of ventricular activation.
Differential diagnosis of T-wave inversion
In the 1960s of last century, Jacobson and Schrire described the differential diagnosis of T-wave inversion that included heart block, ischemic heart disease, bradycardia, right ventricular hypertrophy, right bundle branch block, metabolic disturbances, changes during diagnostic coronary angiography and cerebral disturbances[16]. Nowadays, the current differential diagnosis of T-waves inversion has expanded including, besides the abovementioned citations of Jacobson and Schrire, LV anterior wall ischemia, acute central nervous system disorders, acute adrenergic stress (Takotsubo cardiomyopathy “TTC”)[17,18], pulmonary edema[19,20], antiarrhythmic drug effects[21], pulmonary embolism[22], cardiac memory secondary to transient tachycardia[8], post-ventricular pacing states[23], idiopathic[24] or in relation to cocaine use[25,26]. In a recent review, reversible or permanent inverted T-waves were found in 38% of patients with congenital coronary artery-ventricular multiple micro-fistulas (MMFs)[27]. Hence, congenital MMFs may be included in the differential diagnosis of anterior chest wall T-wave inversion.
Transient and permanent T-wave inversion
Transient T-wave inversion may occur in the following conditions: Acute coronary syndrome[1], cardiac memory T-wave[8,23], cardiogenic non-ischemic pulmonary edema[19], gastroenteritis[28], post maxillofacial surgery[29], subarachnoid hemorrhage[30], electroconvulsive therapy[31-33], Takotsubo cardiomyopathy[18,34], pheochromocytoma[35] and indeterminate origin[24]. On the other hand, permanent T-wave inversion may accompany a variety of disorders associated with LV or RV cardiomyopathy such as apical hypertrophic cardiomyopathy (AHCM)[4,7,36,37] and arrhythmogenic right ventricular cardiomyopathy/dysplasia[38-41].
Non-coronary cardiac and non-cardiac disorders
Several non-coronary cardiac and non-cardiac disorders have been associated with the development of T-wave inversion. Among the Non-coronary cardiac disorders: are pericarditis, myocarditis, cardiac metastasis, athletic heart syndrome, AHCM[4], hypertrophic cardiomyopathy[37], post-tachycardia and right ventricular pacing (cardiac memory)[8,23].
Prognosis
In the middle-aged population, inverted T-wave in the right precordial leads V1-3 was associated with good prognosis in contrast to inverted T-wave in leads other than V1-3 which predicted adverse outcomes such as increased risk of hospitalization due to congestive heart failure and coronary artery disease[3]. Fisch et al[42], stated that inverted shallow asymmetric T-wave with the descending limb longer than the abruptly ascending limb seen in middle-aged women are not associated with cardiac disease.
Non-coronary non-cardiac disorders
Non-coronary non-cardiac disorders (T-wave wide asymmetric and associated with prolonged QT interval) include severe brain injury (subarachnoid hemorrhage “SAH”, intracranial hemorrhage)[30,43], traumatic head injury, maxillofacial surgery[29], bilateral carotid endarterectomy, after vagotomy, cocaine abuse[44], flecainide use[21], pheochromocytoma[45] and gastrointestinal emergencies (perforated ulcer, acute pancreatitis and acute cholecystitis)[28,46-49].
Transient T-wave inversion
Acute coronary syndrome[1]: T-wave inversion in the precordial leads have been reported since 1982 as narrow, sharp, and symmetrical waves; the so called “coronary type” reflecting high-grade stenosis of the proximal left anterior descending coronary artery due to regional delay in ventricular repolarization as generally found in ischemic heart disease[50,51]. In this condition, T-wave inversion may persist for days or weeks.
Cardiac memory pattern: Memory T wave was first presented by Chatterjee et al[52], in 1969 in 94% of patients with intermittent right ventricular pacing. Transient T-wave inversion occurring after conversion to sinus rhythm from tachycardia or artificial pacing which is caused by abnormal ventricular activation. This pattern of transient T-wave inversion in the precordial leads is associated with tall T-wave in leads I and aVL and are common in patients with permanent pacemakers or ensue after recovery from ventricular or supraventricular tachycardia[23]. It is a diagnosis of exclusion. This pattern of T-wave inversion in RV pacing is caused by dyssynchronous LV activation and involvement of potassium ion channels are postulated to be the key issues in its pathogenesis[53].
Electroconvulsive therapy: ECT may induce ECG changes with simultaneous echocardiographic regional wall motion abnormalities especially when arterial blood pressure and heart rate are markedly elevated[54]. It has been reported that transient T wave inversion Occurs in 4% of the patients undergoing ECT[55]. Transient T-wave inversion, not associated with cardiac abnormalities, has been reported due to increased sympathetic stimulation associated with ECT[31,32]. Conversely, Tuininga reported two cases of T-wave inversion following ECT with significant obstructive coronary artery disease requiring anti-anginal therapy and percutaneous coronary intervention[33]. It was recommended that further investigation to rule out significant coronary artery disease should be performed especially in patients with cardiovascular risk factors. Moreover, transient T-wave inversion has been reported after electroconvulsive therapy but not following transthoracic direct current electrical cardioversion for treatment of atrial fibrillation[56]. In representative case (patient 1), the findings of CAG and cardiac MRI were normal.
Cardiac sarcoidosis: Cardiac sarcoidosis (CS) is a systemic inflammatory disease with unknown etiology characterized with non-caseating granulomas in multiple organ systems and may be associated with negative T-wave in the anterior precordial leads.
Subarachnoid hemorrhage: In the 1960s, electrocardiographic changes mimicking myocardial ischemia and infarction associated with spontaneous intracranial hemorrhage have been reported[57]. Reversible T-wave abnormalities accompanied with prolongation of QT interval were found in 32% of patients with SAH[30]. ECG changes and arrhythmias occurred within the first 48 h after SAH[43,58]. The postulated pathogenesis is cardiomyocytolysis due to excessive sympathetic stimulation. Possible mechanisms[30] are autonomic neural stimulation from the hypothalamus and elevated levels of circulating catecholamine. The care of patients with subarachnoid hemorrhage has improved dramatically over the last few decades. These gains are the result of improved microsurgical, endovascular, and medical management techniques. This intensive management subjects patients to multiple radiographic studies and thus increased radiation exposure. Thus, tailored diagnostic modalities are required for early and correct establishment of the diagnosis. This to avoid over exposure to ionizing radiation and other invasive procedures. T-wave abnormalities in patients suffering SAH are subsequent to TTC secondary to elevated levels of circulating catecholamine and excessive sympathetic stimulation[29].
Pulmonary embolism: Acute pulmonary embolism may occasionally result in reversible deep T-wave inversion with QT interval prolongation[59]. T-wave inversion associated with PE was first described in 1938 by Love et al[60]. T-wave inversion in the precordial leads have been noticed in a moderate-size PE[61], partially occlusive[22] and non-occlusive[23] PE. Precordial T-wave inversion was the most common abnormal ECG finding (68%), this anterior wall ischemic pattern was found in 85% of massive PE and in 19% of mild-moderate PE followed by S1 Q3 T3 pattern detected in 54% of the patients[62]. The proposed mechanisms include RV strain and decreased perfusion of LV anterior wall caused by hypotension consequent to pulmonary embolism[63]. The above mentioned findings were present in the patient with PE (patient 5).
Diagnostic workup for T-wave inversion should always focus on the most likely causes and patient individually tailored diagnostic program should be followed. This to avoid and to limit unnecessary radiation exposure including diagnostic invasive cardiac catheterization.
Pulmonary edema: T wave inversion in the precordial leads has rarely been reported: Possible postulated mechanisms are: an acute rise in the cardiac sympathetic tone either via an increased sympathetic discharge from the central nervous system or through subendocardial ischemia due to elevated wall stress, high end-diastolic pressure and decreased coronary arterial blood flow and the electrical heterogeneity in the ventricular wall[19].
Pheochromocytomas: Pheochromocytomas are catecholamine secreting tumours that arise from the chromaffin cells of the adrenal gland. Biochemical diagnosis is established by measuring plasma free metanephrins or nor-metanephrin levels. Localization of the tumour is reached by performing computed tomography or magnetic resonance imaging scans and specifically using metaiodibenzylguanidine scan. The latter is considered the gold standard. Finally, it is confirmed by histopathologic examination[64]. Occasionally, pheochromocytoma may resemble acute coronary syndrome[35,65]. Pheochromocytoma-related cardiomyopathy has incidentally been reported with inverted takotsubo contractile pattern[45]. In patient No. 7, diagnosed with pheochromocytoma (Figure 7F) presented with chest pain and psychomotor agitation, showed periodic fluctuations of blood pressure and ECG abnormalities mimicking acute coronary syndrome (Figure 7A) without significant obstructive coronary artery disease (CAD) on his CAG (Figure 7B and C).
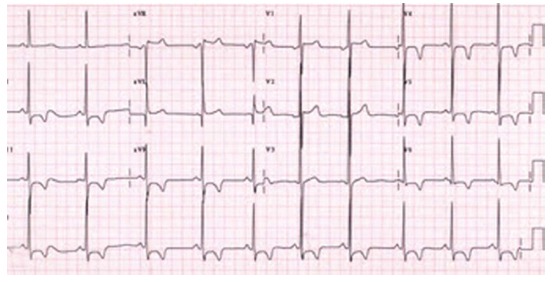
Figure 7.
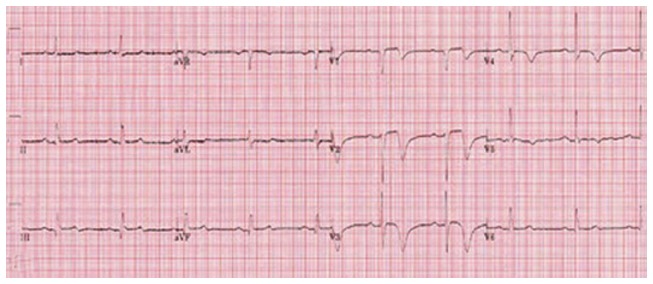
Patient 7. A: An electrocardiographic (ECG) tracing, showing giant T wave inversion in the precordial leads V2-6, of a 76-year Caucasian male with a past medical history of an old inferior myocardial infarction, percutaneous coronary intervention of the right coronary artery (RCA) and left anterior descending coronary artery, acutely presented with left abdominal pain, psychomotor unrest, diaphoresis and blood pressure difference between the right and left arm. Acute aortic dissection was excluded as well as recurrent MI. Coronary angiography frame of (B) the left coronary artery and (C) the RCA depicting no significant stenosis of the arterial tree. Serum cardiac markers were slightly elevated. Echocardiographic (hypokinesia of the mid and apical regions and hyperkinesia of the basal segments) findings and (D) ventriculography (apical ballooning) were all compatible with Takotsubo cardiomyopathy; E: Base line ECG. The abdominal ultrasound and (F) CT demonstrated a pheochromocytoma in the left adrenal region which was confirmed with 123I-MIBG scan and dihydroxyphenylalanine-Positron Emission tomography and proved by pathological results. Plasma and urine metanephrin and normetanephrin were highly elevated. After removal of the hormonally active tumor, the patient became symptom free and the ECG normalized. The medical treatment continued including calcium reentry blocker, beta blocker, aspirin, angiotensin converting enzyme inhibitor, statin and an α-blocker.
Pheochromocytomas are rare neuroendocrine tumours with a highly variable clinical presentation but most commonly presenting with bouts of headaches, sweating, palpitation and hypertension. Imaging techniques such as CT or MRI and functional assessments using 123I-MIBG are applied to localize biochemically active tumors. In our patient (patient 7), full recovery occurred after left adrenalectomy was successfully performed in an academic hospital. The deepest T-wave inversion (Figure 7A) was found in this patient.
Takotsubo cardiomyopathy: TTC in relation to neurohormonal active adrenal tumor pheochromocytoma or after pulmonary resection for bilateral non-small cell lung neoplasms has rarely been reported[45,66]. TTC accounts for 2% of total hospital admissions for suspected acute coronary syndrome[67]. It Accounts for approximately 1% of admissions for suspected acute myocardial infarction in Japan[68]. Satoh et al[69] and Dote and associates first described this syndrome in Japanese patients[70]. In 2001, Tsuchihashi et al[17] reported on cardiomyopathy with apical ballooning mimicking acute myocardial infarction (MI) without obstructive epicardial CAD, 97% of patients demonstrated T-wave inversion in the precordial leads with female predominance (86%). They observed that in 70% of the subjects there was a preceding heavy psychological or physical stress[17]. While the pathogenesis of TTC is not fully understood and remains to be elucidated, several hypotheses, including multivessel epicardial coronary artery spasm, storm of catecholamine excess and coronary microvascular disorder have been proposed[17,71,72]. In a comparison between patients with acute MI and heart failure and patients admitted with a LV systolic dysfunction after sudden emotional stress (95% female subject), Wittstein et al[18], found CAD in only 5% in the latter group with significantly higher plasma catecholamine levels suggesting a relation between an exaggerated sympathetic stimulation and transient LV dysfunction[18]. The following criteria are required for establishing the diagnosis TTC; transient LV systolic dysfunction frequently emerging following a stressful trigger, not associated with significant obstructive CAD, novel ECG changes with ST-segment elevation or T-wave inversion usually accompanied with slightly elevation of cardiac markers and no signs of myocarditis and pheochromocytoma[73-75]. Occasionally, in the hyperacute phase of TTC, transient J wave may precede T-wave inversion[72]. Diagnostic work-up may include history, ECG, echocardiography, CAG, ventriculography and less frequent Cardiac magnetic resonance imaging[76]. Cardiac MRI has been useful to differentiate stress TTC from anterior ST-Elevation MI with segmental wall necrosis, by absence of late enhancement in the former condition on delayed image sequence. Other pivotal MRI findings for the diagnosis of TTC are diffuse edema of the left ventricular apical or mid wall associated with akinesia or hypokinesia and absence of perfusion defects[34]. Furthermore, T2-weighted MRI delineated the ECG characterizations (dynamic negative T waves and QTc prolongation) in TCC, resembling the ischemic-like Wellens’ ECG pattern, correlating with the apicobasal gradient of myocardial edema, reflecting the edema-induced transient apicobasal inhomogeneity[77]. Recently, positron emission tomography computed tomography has been used to differentiate takotsubo cardiomyopathy TTC from acute coronary syndrome[78]. TTC may occur subsequent to aneurysmal subarachnoid hemorrhage[79]. The relation between TTC and SAH is well known. Many reports have shown the reversible pattern of T-wave inversion associated with SAH[29,78].
Athletic heart: In 1899, Henschen[80] described cardiac enlargement in cross-country skiers. Several ECG changes have been observed in athletes engaged in high intensity dynamic endurance sport activities which may mimic pathological and structural heart diseases. Among others, T-wave inversion in the precordial leads and relative bradycardia were reported[81]. Echocardiographic features of athletic left ventricular hypertrophy may include mild concentric LVH, mild LV dilatation, normal diastolic filling and normal systolic function[82]. It is important to distinguish between physiological adaptive ECG changes and pathological ECG abnormalities to prevent unnecessary distress [83,84]. Regression of LVH occurs when athletes decide to decondition. Some authors consider this adaptation of endurance sports athletic heart as pathologic since LVH regresses on cessation of endurance training in a similar response to a successful treatment of aortic stenosis or arterial hypertension[85].
Permanent T-wave inversion
Arrhythmogenic right ventricular hypertrophy was first described by Dalla volta et al[86] in 1961 in Italy and it was brought comprehensively under attention by Frank et al[87] in 1978. They reported individuals with extending fibro-fatty non-ischemic changes of the right ventricle. Sudden death may be the first sign of disease[88]. Prevalence is 1/5000 individuals[89]. They have an autosomal dominant or recessive mode of inheritance with incomplete penetrance. ARVC/D affects mainly the right ventricular myocardium characterized with progressive fibro-fatty replacement and infiltration of the RV myocardium and is considered a major cause of sudden arrhythmic death. Recently, involvement of the left ventricle at a later stage may be associated with severe manifestation and carry a worse prognosis[90]. It has been suggested by Gallo et al[91] and others for the implementation of a broader term as arrhythmogenic cardiomyopathy (AC)[91,92]. In AC, two major criteria or one major and 2 minor criteria are required to establish the diagnosis[38]. T wave inversion may be the first presentation[3]. Recently, in 2010, the revised task force criteria and guidelines for the clinical diagnosis of AC have been updated and T-wave inversion in the right precordial leads V1-3 or beyond was upgraded to a major criterion, in subjects > 14 years of age in the absence of complete right bundle branch block[93], as was found in patient No. 8. The 12-lead ECG demonstrated abnormal changes in 90% of the cases with T-wave inversion in V1-3 and sometimes across V6 as the most common finding[38]. Right precordial T-wave inversions were present in 48%-85% of suspected subjects and Epsilon wave (terminal notch in the QRS complex due to slowed intraventricular conduction) was found in 8%-33% of patients with AC[38-40] as was the case in patient No. 8. In subjects with AC, global and or regional dysfunction and structural alterations may be detected by echocardiography, angiography, radionuclide scintigraphy or MRI. Cardiac MRI has a high negative predictive value with sensitivity of 100% and specificity of 87%[94]. Mutations in the genes responsible for coding of connecting proteins, called desmosomes are the culprit. In the Dutch population, a founder mutation of p.Arg79X in plakophillin-2 (PKP2) gen with the same desmosome gene mutation in AC has been described[95]. Analysis of DNA in patient No. 8, showed a mutation of plakophillin-2 gen (1248C>A Tyr 616X). Rarely, cardiac sarcoidosis may mimic AC[96].
Apical hypertrophic cardiomyopathy[4,7,36,37]: It Is also called (Yamaguchi syndrome) and is considered a rare variant of hypertrophic cardiomyopathy. In the majority of cases (93%) of AHCM, negative T-wave in the precordial leads is the most frequent finding[7]. Its prevalence (15%) in Japan is high in comparison to the United States (3%)[97] and in Europe (< 5%)[98]. Giant negative T-wave exceeding 10 mm is found in 47% of patients with AHCM[7]. Typical findings were first described by Sakamoto in 1976[99] and Yamaguchi et al[100] in 1979. In the retrospective study of Eriksson et al[7], T-wave inversion was found in (98/105) 93% of the patients. Apical wall thickness of 15 mm was based on TTE or MRI measurements. The T-wave inversion is permanent without tendency for recovery. The permanent ECG features of AHCM are among others giant negative T waves in the precordial leads, ST depression and negative U waves in II, III, aVF, V4-V6, a prolonged QTc and tallest R wave in V4; however, these permanent features may vary over time[101].
Awareness of the differential diagnosis of T-wave inversion in the precordial leads will help trainees and physicians to discern different entities and will prevent some patients from undergoing unnecessary invasive investigations and procedures. Tailored individual diagnostic investigation was performed and specific diagnostic tools were undertaken when high index of clinical suspicion was raised towards a certain disease entity.
COMMENTS
Background
Myriad of clinical conditions have been described in association with T-wave inversion in the precordial leads. T-wave inversion associated with or without corrected QT prolongation may be encountered in a variety of clinical conditions.
Research frontiers
In patients with T-wave inversion in the precordial leads, tailored diagnostic approach should be conducted avoiding overuse of diagnostic methods. Specific tailored diagnostic modalities and directed therapeutic interventions may be undertaken when high index of clinical suspicion is raised towards certain disease entity.
Innovations and breakthroughs
This study is a retrospective analysis of patients presented with T-wave inversion in the anterior chest leads. The T-wave inversion may be accompanied with or without QTc prolongation. Classification has been made into reversible and irreversible types to facilitate its differential diagnostic approach.
Applications
Awareness of the differential diagnosis of T-wave inversion in the precordial leads will help trainees and physicians to discern different entities and will prevent some patients from undergoing unnecessary invasive investigations and procedures.
Peer review
In this paper, authors report the various clinical conditions of patients with T wave inversion in the anterior chest wall leads. This review article is interesting and very educational.
Footnotes
Ethics approval: The study is reviewed and approved by the Hospital Group Twente, Institutional Review Board. Verbal consent was taken from the patients and ethical clearance and permission to publish the cases is obtained from the Hospital Group Twente, Institutional Review Board.
Informed consent: All study participants provided verbal informed consent.
Conflict-of-interest: The authors declare no conflict of interest.
Data sharing: Technical appendix, statistical code, and dataset available from the corresponding author at salah.said@gmail.com. Informed consent, neither verbal nor written, was obtained for data sharing but the presented data are anonymized and risk of identification is negligible.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: October 28, 2014
First decision: November 27, 2014
Article in press: January 12, 2015
P- Reviewer: Cheng XW, Kato M S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
References
- 1.Fisher M, Lichstein E, Hollander G, Greengart A, Shani J. Giant T-wave inversion in patients with acute coronary insufficiency. Chest. 1992;101:935–937. doi: 10.1378/chest.101.4.935. [DOI] [PubMed] [Google Scholar]
- 2.de Zwaan C, Bär FW, Janssen JH, Cheriex EC, Dassen WR, Brugada P, Penn OC, Wellens HJ. Angiographic and clinical characteristics of patients with unstable angina showing an ECG pattern indicating critical narrowing of the proximal LAD coronary artery. Am Heart J. 1989;117:657–665. doi: 10.1016/0002-8703(89)90742-4. [DOI] [PubMed] [Google Scholar]
- 3.Aro AL, Anttonen O, Tikkanen JT, Junttila MJ, Kerola T, Rissanen HA, Reunanen A, Huikuri HV. Prevalence and prognostic significance of T-wave inversions in right precordial leads of a 12-lead electrocardiogram in the middle-aged subjects. Circulation. 2012;125:2572–2577. doi: 10.1161/CIRCULATIONAHA.112.098681. [DOI] [PubMed] [Google Scholar]
- 4.MacKenzie R. Giant negative T waves. J Insur Med. 2004;36:153–157. [PubMed] [Google Scholar]
- 5.Marriott HJL. Practical electrocardiography. 7th ed. Baltimore/London: Williams & Wilkins; 1983. [Google Scholar]
- 6.Sokolow M, Lyon TP. The ventricular complex in right ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J. 1949;38:273–294. doi: 10.1016/0002-8703(49)91335-6. [DOI] [PubMed] [Google Scholar]
- 7.Eriksson MJ, Sonnenberg B, Woo A, Rakowski P, Parker TG, Wigle ED, Rakowski H. Long-term outcome in patients with apical hypertrophic cardiomyopathy. J Am Coll Cardiol. 2002;39:638–645. doi: 10.1016/s0735-1097(01)01778-8. [DOI] [PubMed] [Google Scholar]
- 8.Hanna EB, Glancy DL. ST-segment depression and T-wave inversion: classification, differential diagnosis, and caveats. Cleve Clin J Med. 2011;78:404–414. doi: 10.3949/ccjm.78a.10077. [DOI] [PubMed] [Google Scholar]
- 9.Rautaharju PM, Surawicz B, Gettes LS, Bailey JJ, Childers R, Deal BJ, Gorgels A, Hancock EW, Josephson M, Kligfield P, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part IV: the ST segment, T and U waves, and the QT interval: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009;53:982–991. doi: 10.1016/j.jacc.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 10.Bazett HC. An analysiss of time relations of electrocardiograms. Heart. 1920;7:353–370. [Google Scholar]
- 11.Ahnve S. Correction of the QT interval for heart rate: review of different formulas and the use of Bazett’s formula in myocardial infarction. Am Heart J. 1985;109:568–574. doi: 10.1016/0002-8703(85)90564-2. [DOI] [PubMed] [Google Scholar]
- 12.Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989;2:358–367. doi: 10.1016/s0894-7317(89)80014-8. [DOI] [PubMed] [Google Scholar]
- 13.Maron BJ, McKenna WJ, Danielson GK, Kappenberger LJ, Kuhn HJ, Seidman CE, Shah PM, Spencer WH, Spirito P, Ten Cate FJ, et al. American College of Cardiology/European Society of Cardiology Clinical Expert Consensus Document on Hypertrophic Cardiomyopathy. A report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the European Society of Cardiology Committee for Practice Guidelines. Eur Heart J. 2003;24:1965–1991. doi: 10.1016/s0195-668x(03)00479-2. [DOI] [PubMed] [Google Scholar]
- 14.Marcus FI. Prevalence of T-wave inversion beyond V1 in young normal individuals and usefulness for the diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia. Am J Cardiol. 2005;95:1070–1071. doi: 10.1016/j.amjcard.2004.12.060. [DOI] [PubMed] [Google Scholar]
- 15.Pelliccia A, Culasso F, Di Paolo FM, Accettura D, Cantore R, Castagna W, Ciacciarelli A, Costini G, Cuffari B, Drago E, et al. Prevalence of abnormal electrocardiograms in a large, unselected population undergoing pre-participation cardiovascular screening. Eur Heart J. 2007;28:2006–2010. doi: 10.1093/eurheartj/ehm219. [DOI] [PubMed] [Google Scholar]
- 16.Jacobson D, Schrire V. Giant T wave inversion. Br Heart J. 1966;28:768–775. doi: 10.1136/hrt.28.6.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsuchihashi K, Ueshima K, Uchida T, Oh-mura N, Kimura K, Owa M, Yoshiyama M, Miyazaki S, Haze K, Ogawa H, et al. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris-Myocardial Infarction Investigations in Japan. J Am Coll Cardiol. 2001;38:11–18. doi: 10.1016/s0735-1097(01)01316-x. [DOI] [PubMed] [Google Scholar]
- 18.Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP, Gerstenblith G, Wu KC, Rade JJ, Bivalacqua TJ, Champion HC. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352:539–548. doi: 10.1056/NEJMoa043046. [DOI] [PubMed] [Google Scholar]
- 19.Littmann L. Large T wave inversion and QT prolongation associated with pulmonary edema: a report of nine cases. J Am Coll Cardiol. 1999;34:1106–1110. doi: 10.1016/s0735-1097(99)00311-3. [DOI] [PubMed] [Google Scholar]
- 20.Pascale P, Quartenoud B, Stauffer JC. Isolated large inverted T wave in pulmonary edema due to hypertensive crisis: a novel electrocardiographic phenomenon mimicking ischemia? Clin Res Cardiol. 2007;96:288–294. doi: 10.1007/s00392-007-0504-1. [DOI] [PubMed] [Google Scholar]
- 21.Said SA, Somer ST, Oude Luttikhuis HA. Flecainide-induced JT prolongation, T wave inversion and ventricular tachycardia during treatment for symptomatic atrial fibrillation. Int J Cardiol. 1994;44:285–287. doi: 10.1016/0167-5273(94)90293-3. [DOI] [PubMed] [Google Scholar]
- 22.Pillarisetti J, Gupta K. Giant Inverted T waves in the emergency department: case report and review of differential diagnoses. J Electrocardiol. 2010;43:40–42. doi: 10.1016/j.jelectrocard.2009.08.048. [DOI] [PubMed] [Google Scholar]
- 23.Littmann L, Fertman AF. Large T-wave inversion in a patient with a pacemaker. Arch Intern Med. 2011;171:1314; discussion 1315–1316. doi: 10.1001/archinternmed.2011.358. [DOI] [PubMed] [Google Scholar]
- 24.Corbella F, Dragonetti L, Rivas C, Eyheremendy E, Acunzo R. Giant negative T waves of indeterminate origin. Rev Argent Cardiol. 2009;2:131–134. [Google Scholar]
- 25.Dhawan SS. Pseudo-Wellens’ syndrome after crack cocaine use. Can J Cardiol. 2008;24:404. doi: 10.1016/s0828-282x(08)70608-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zimmerman FH, Gustafson GM, Kemp HG. Recurrent myocardial infarction associated with cocaine abuse in a young man with normal coronary arteries: evidence for coronary artery spasm culminating in thrombosis. J Am Coll Cardiol. 1987;9:964–968. doi: 10.1016/s0735-1097(87)80256-5. [DOI] [PubMed] [Google Scholar]
- 27.Said SA, Schiphorst RH, Derksen R, Wagenaar L. Coronary-cameral fistulas in adults (first of two parts) World J Cardiol. 2013;5:329–336. doi: 10.4330/wjc.v5.i9.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rott D, Leibowitz D, Weiss AT. Giant precordial T wave inversion in a patient with gastroenteritis. Case Rep Vasc Med. 2011;2011:942045. doi: 10.1155/2011/942045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim Y, Shibutani T, Hirota Y, Hori T, Matsuura H. Giant negative T waves after maxillofacial surgery. Anesth Prog. 1992;39:28–35. [PMC free article] [PubMed] [Google Scholar]
- 30.Chatterjee S. ECG Changes in Subarachnoid Haemorrhage: A Synopsis. Neth Heart J. 2011;19:31–34. doi: 10.1007/s12471-010-0049-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Narasimhan S. Electroconvulsive therapy and electrocardiograph changes. J Postgrad Med. 2008;54:228–229. doi: 10.4103/0022-3859.41810. [DOI] [PubMed] [Google Scholar]
- 32.Cockey GH, Conti CR. Electroconvulsive therapy-induced transient T-wave inversions on ECG. Clin Cardiol. 1995;18:418–420. doi: 10.1002/clc.4960180711. [DOI] [PubMed] [Google Scholar]
- 33.Tuininga YS. ECG changes after electroconvulsive therapy, cause or consequence? Neth Heart J. 2012;20:129–131. doi: 10.1007/s12471-011-0167-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fernández-Pérez GC, Aguilar-Arjona JA, de la Fuente GT, Samartín M, Ghioldi A, Arias JC, Sánchez-González J. Takotsubo cardiomyopathy: assessment with cardiac MRI. AJR Am J Roentgenol. 2010;195:W139–W145. doi: 10.2214/AJR.09.3369. [DOI] [PubMed] [Google Scholar]
- 35.Hsu CT, Chen CY. A Patient with Pheochromocytoma Showing Periodic Fluctuations of Blood Pressure and Electrocardiographic Abnormalities Mimicking Acute Coronary Syndrome. J Emerg Crit Care Med. 2009;20:25–32. [Google Scholar]
- 36.Webb JG, Sasson Z, Rakowski H, Liu P, Wigle ED. Apical hypertrophic cardiomyopathy: clinical follow-up and diagnostic correlates. J Am Coll Cardiol. 1990;15:83–90. doi: 10.1016/0735-1097(90)90180-w. [DOI] [PubMed] [Google Scholar]
- 37.Yusuf SW, Bathina JD, Banchs J, Mouhayar EN, Daher IN. Apical hypertrophic cardiomyopathy. World J Cardiol. 2011;3:256–259. doi: 10.4330/wjc.v3.i7.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Francés RJ. Arrhythmogenic right ventricular dysplasia/cardiomyopathy. A review and update. Int J Cardiol. 2006;110:279–287. doi: 10.1016/j.ijcard.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 39.Nasir K, Bomma C, Tandri H, Roguin A, Dalal D, Prakasa K, Tichnell C, James C, Spevak PJ, Marcus F, et al. Electrocardiographic features of arrhythmogenic right ventricular dysplasia/cardiomyopathy according to disease severity: a need to broaden diagnostic criteria. Circulation. 2004;110:1527–1534. doi: 10.1161/01.CIR.0000142293.60725.18. [DOI] [PubMed] [Google Scholar]
- 40.Cox MG, van der Smagt JJ, Wilde AA, Wiesfeld AC, Atsma DE, Nelen MR, Rodriguez LM, Loh P, Cramer MJ, Doevendans PA, et al. New ECG criteria in arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circ Arrhythm Electrophysiol. 2009;2:524–530. doi: 10.1161/CIRCEP.108.832519. [DOI] [PubMed] [Google Scholar]
- 41.Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, Calkins H, Corrado D, Cox MG, Daubert JP, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Circulation. 2010;121:1533–1541. doi: 10.1161/CIRCULATIONAHA.108.840827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fisch C. The abnormal ECG in the absence of cardiac disease. ACC Current Journal Review. 1997:69–73. [Google Scholar]
- 43.Kukla P, Jastrzebski M, Praefort W. J-wave-associated ventricular fibrillation in a patient with a subarachnoid haemorrhage. Europace. 2012;14:1063–1064. doi: 10.1093/europace/eur410. [DOI] [PubMed] [Google Scholar]
- 44.Ramirez FD, Femenía F, Simpson CS, Redfearn DP, Michael KA, Baranchuk A. Electrocardiographic findings associated with cocaine use in humans: a systematic review. Expert Rev Cardiovasc Ther. 2012;10:105–127. doi: 10.1586/erc.11.152. [DOI] [PubMed] [Google Scholar]
- 45.Sanchez-Recalde A, Costero O, Oliver JM, Iborra C, Ruiz E, Sobrino JA. Images in cardiovascular medicine. Pheochromocytoma-related cardiomyopathy: inverted Takotsubo contractile pattern. Circulation. 2006;113:e738–e739. doi: 10.1161/CIRCULATIONAHA.105.581108. [DOI] [PubMed] [Google Scholar]
- 46.Khairy P, Marsolais P. Pancreatitis with electrocardiographic changes mimicking acute myocardial infarction. Can J Gastroenterol. 2001;15:522–526. doi: 10.1155/2001/604386. [DOI] [PubMed] [Google Scholar]
- 47.Ito M, Hatta K, Miyakawa K, Miyauchi K, Arai H. Prolonged and fluctuating giant T-wave inversion after electroconvulsive therapy. J ECT. 2007;23:194–197. doi: 10.1097/YCT.0b013e31806ad234. [DOI] [PubMed] [Google Scholar]
- 48.Lowenstein L, Hussein A. [Transient ischemic ECG changes in a patient with acute cholecystitis without a history of ischemic heart disease] Harefuah. 2000;138:449–450, 518. [PubMed] [Google Scholar]
- 49.Migliore F, Zorzi A, Marra MP, Basso C, Corbetti F, De Lazzari M, Tarantini G, Buja P, Lacognata C, Thiene G, et al. Myocardial edema underlies dynamic T-wave inversion (Wellens’ ECG pattern) in patients with reversible left ventricular dysfunction. Heart Rhythm. 2011;8:1629–1634. doi: 10.1016/j.hrthm.2011.04.035. [DOI] [PubMed] [Google Scholar]
- 50.de Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103:730–736. doi: 10.1016/0002-8703(82)90480-x. [DOI] [PubMed] [Google Scholar]
- 51.Rhinehardt J, Brady WJ, Perron AD, Mattu A. Electrocardiographic manifestations of Wellens’ syndrome. Am J Emerg Med. 2002;20:638–643. doi: 10.1053/ajem.2002.34800. [DOI] [PubMed] [Google Scholar]
- 52.Chatterjee K, Harris AM, Davies JG, Leatham A. T-wave changes after artificial pacing. Lancet. 1969;1:759–760. doi: 10.1016/s0140-6736(69)91758-9. [DOI] [PubMed] [Google Scholar]
- 53.Rosen MR, Cohen IS. Cardiac memory ... new insights into molecular mechanisms. J Physiol. 2006;570:209–218. doi: 10.1113/jphysiol.2005.097873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Messina AG, Paranicas M, Katz B, Markowitz J, Yao FS, Devereux RB. Effect of electroconvulsive therapy on the electrocardiogram and echocardiogram. Anesth Analg. 1992;75:511–514. doi: 10.1213/00000539-199210000-00008. [DOI] [PubMed] [Google Scholar]
- 55.O’Brien KE, Pastis N, Conti JB. Diffuse T-wave inversions associated with electroconvulsive therapy. Am J Cardiol. 2004;93:1573–1574. doi: 10.1016/j.amjcard.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 56.Van Gelder IC, Crijns HJ, Van der Laarse A, Van Gilst WH, Lie KI. Incidence and clinical significance of ST segment elevation after electrical cardioversion of atrial fibrillation and atrial flutter. Am Heart J. 1991;121:51–56. doi: 10.1016/0002-8703(91)90954-g. [DOI] [PubMed] [Google Scholar]
- 57.CROPP GJ, MANNING GW. Electrocardiographic changes simulating myocardial ischemia and infarction associated with spontaneous intracranial hemorrhage. Circulation. 1960;22:25–38. doi: 10.1161/01.cir.22.1.25. [DOI] [PubMed] [Google Scholar]
- 58.Di Pasquale G, Pinelli G, Andreoli A, Manini G, Grazi P, Tognetti F. Holter detection of cardiac arrhythmias in intracranial subarachnoid hemorrhage. Am J Cardiol. 1987;59:596–600. doi: 10.1016/0002-9149(87)91176-3. [DOI] [PubMed] [Google Scholar]
- 59.Punukollu G, Gowda RM, Khan IA, Wilbur SL, Vasavada BC, Sacchi TJ. QT interval prolongation with global T-wave inversion: a novel ECG finding in acute pulmonary embolism. Ann Noninvasive Electrocardiol. 2004;9:94–98. doi: 10.1111/j.1542-474X.2004.91528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Love Jr WS, Brugler GW, Winslow N. Electrocardiographic studies in clinical and experimental pulmonary embolization. Arch Intern Med. 1938;11:2109–2123. [Google Scholar]
- 61.Sarin S, Elmi F, Nassef L. Inverted T waves on electrocardiogram: myocardial ischemia versus pulmonary embolism. J Electrocardiol. 2005;38:361–363. doi: 10.1016/j.jelectrocard.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 62.Ferrari E, Imbert A, Chevalier T, Mihoubi A, Morand P, Baudouy M. The ECG in pulmonary embolism. Predictive value of negative T waves in precordial leads--80 case reports. Chest. 1997;111:537–543. doi: 10.1378/chest.111.3.537. [DOI] [PubMed] [Google Scholar]
- 63.DACK S, MASTER AM. Acute coronary insufficiency due to pulmonary embolism. Am J Med. 1949;7:464–477. doi: 10.1016/0002-9343(49)90396-4. [DOI] [PubMed] [Google Scholar]
- 64.Mehta N, Paniker V, Shah A. MIBG negative pheochromocytoma. J Assoc Physicians India. 2010;58:198–199. [PubMed] [Google Scholar]
- 65.Menke-van der Houven van Oordt CW, Twickler TB, van Asperdt FG, Ackermans P, Timmers HJ, Hermus AR. Pheochromocytoma mimicking an acute myocardial infarction. Neth Heart J. 2007;15:248–251. doi: 10.1007/BF03085991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Toyooka S, Akagi S, Furukawa M, Nakamura K, Soh J, Yamane M, Oto T, Miyoshi S. Takotsubo cardiomyopathy associated with pulmonary resections after induction chemoradiotherapy for non-small cell lung cancer. Gen Thorac Cardiovasc Surg. 2012;60:599–602. doi: 10.1007/s11748-012-0058-7. [DOI] [PubMed] [Google Scholar]
- 67.Azzarelli S, Galassi AR, Amico F, Giacoppo M, Argentino V, Tomasello SD, Tamburino C, Fiscella A. Clinical features of transient left ventricular apical ballooning. Am J Cardiol. 2006;98:1273–1276. doi: 10.1016/j.amjcard.2006.05.065. [DOI] [PubMed] [Google Scholar]
- 68.Sharkey SW, Lesser JR, Zenovich AG, Maron MS, Lindberg J, Longe TF, Maron BJ. Acute and reversible cardiomyopathy provoked by stress in women from the United States. Circulation. 2005;111:472–479. doi: 10.1161/01.CIR.0000153801.51470.EB. [DOI] [PubMed] [Google Scholar]
- 69.Satoh H, Tateishi H, Uchida T, et al. Takotsubo-type cardiomyopathy due to multivessel spasm. In: Kodama K, Haze K, Hon M, editors. Clinical aspects of myocardial injury. From ischemia to heart failure (in Japanese) Tokyo: Kagakuhyouronsya Co; 1990. pp. 56–64. [Google Scholar]
- 70.Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. [Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases] J Cardiol. 1991;21:203–214. [PubMed] [Google Scholar]
- 71.Kurisu S, Sato H, Kawagoe T, Ishihara M, Shimatani Y, Nishioka K, Kono Y, Umemura T, Nakamura S. Tako-tsubo-like left ventricular dysfunction with ST-segment elevation: a novel cardiac syndrome mimicking acute myocardial infarction. Am Heart J. 2002;143:448–455. doi: 10.1067/mhj.2002.120403. [DOI] [PubMed] [Google Scholar]
- 72.Zorzi A, Migliore F, Perazzolo Marra M, Tarantini G, Iliceto S, Corrado D. Electrocardiographic J waves as a hyperacute sign of Takotsubo syndrome. J Electrocardiol. 2012;45:353–356. doi: 10.1016/j.jelectrocard.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 73.Sharkey SW, Lesser JR, Maron MS, Maron BJ. Why not just call it tako-tsubo cardiomyopathy: a discussion of nomenclature. J Am Coll Cardiol. 2011;57:1496–1497. doi: 10.1016/j.jacc.2010.11.029. [DOI] [PubMed] [Google Scholar]
- 74.Akashi YJ, Goldstein DS, Barbaro G, Ueyama T. Takotsubo cardiomyopathy: a new form of acute, reversible heart failure. Circulation. 2008;118:2754–2762. doi: 10.1161/CIRCULATIONAHA.108.767012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Madhavan M, Rihal CS, Lerman A, Prasad A. Acute heart failure in apical ballooning syndrome (TakoTsubo/stress cardiomyopathy): clinical correlates and Mayo Clinic risk score. J Am Coll Cardiol. 2011;57:1400–1401. doi: 10.1016/j.jacc.2010.10.038. [DOI] [PubMed] [Google Scholar]
- 76.Fritz J, Wittstein IS, Lima JA, Bluemke DA. Transient left ventricular apical ballooning: magnetic resonance imaging evaluation. J Comput Assist Tomogr. 2005;29:34–36. doi: 10.1097/01.rct.0000148454.67697.42. [DOI] [PubMed] [Google Scholar]
- 77.Perazzolo Marra M, Zorzi A, Corbetti F, De Lazzari M, Migliore F, Tona F, Tarantini G, Iliceto S, Corrado D. Apicobasal gradient of left ventricular myocardial edema underlies transient T-wave inversion and QT interval prolongation (Wellens’ ECG pattern) in Tako-Tsubo cardiomyopathy. Heart Rhythm. 2013;10:70–77. doi: 10.1016/j.hrthm.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 78.Ghadri JR, Dougoud S, Maier W, Kaufmann PA, Gaemperli O, Prasad A, Lüscher TF, Templin C. A PET/CT-follow-up imaging study to differentiate takotsubo cardiomyopathy from acute myocardial infarction. Int J Cardiovasc Imaging. 2014;30:207–209. doi: 10.1007/s10554-013-0311-x. [DOI] [PubMed] [Google Scholar]
- 79.Kumar MA, Nakajl P, Radhakrishnan P, Sue R. Tako-tsubo cardiomyopathy occurring 12 days after aneurysmal subarachnoidal hemorrhage. Chest. 2012;142:393–395. [Google Scholar]
- 80.Henschen S. Skilanglauf und skiwettlauf. Eine medixzinische sport studie. Jena: Mitt Med Klin Uppsala; 1899. [Google Scholar]
- 81.Fagard R. Athlete’s heart. Heart. 2003;89:1455–1461. doi: 10.1136/heart.89.12.1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Maron BJ. Structural features of the athlete heart as defined by echocardiography. J Am Coll Cardiol. 1986;7:190–203. doi: 10.1016/s0735-1097(86)80282-0. [DOI] [PubMed] [Google Scholar]
- 83.Corrado D, Biffi A, Basso C, Pelliccia A, Thiene G. 12-lead ECG in the athlete: physiological versus pathological abnormalities. Br J Sports Med. 2009;43:669–676. doi: 10.1136/bjsm.2008.054759. [DOI] [PubMed] [Google Scholar]
- 84.Pelliccia A, Di Paolo FM, Quattrini FM, Basso C, Culasso F, Popoli G, De Luca R, Spataro A, Biffi A, Thiene G, et al. Outcomes in athletes with marked ECG repolarization abnormalities. N Engl J Med. 2008;358:152–161. doi: 10.1056/NEJMoa060781. [DOI] [PubMed] [Google Scholar]
- 85.McCann GP, Muir DF, Hillis WS. Athletic left ventricular hypertrophy: long-term studies are required. Eur Heart J. 2000;21:351–353. doi: 10.1053/euhj.1999.1783. [DOI] [PubMed] [Google Scholar]
- 86.Dalla volta S, Battaglia G, Zerbini E. “Auricularization’ of right ventricular pressure curve. Am Heart J. 1961;61:25–33. doi: 10.1016/0002-8703(61)90513-0. [DOI] [PubMed] [Google Scholar]
- 87.Frank R, Fontaine G, Vedel J, Mialet G, Sol C, Guiraudon G, Grosgogeat Y. Electrocardiology of 4 cases of right ventricular dysplasia inducing arrhythmia. Arch Mal Coeur Vaiss. 1978;71:963–972. [PubMed] [Google Scholar]
- 88.Thiene G, Nava A, Corrado D, Rossi L, Pennelli N. Right ventricular cardiomyopathy and sudden death in young people. N Engl J Med. 1988;318:129–133. doi: 10.1056/NEJM198801213180301. [DOI] [PubMed] [Google Scholar]
- 89.Norman MW, McKenna WJ. Arrhythmogenic right ventricular cardiomyopathy: perspectives on disease. Z Kardiol. 1999;88:550–554. doi: 10.1007/s003920050324. [DOI] [PubMed] [Google Scholar]
- 90.Saguner AM, Brunckhorst C, Duru F. Arrhythmogenic ventricular cardiomyopathy: A paradigm shift from right to biventricular disease. World J Cardiol. 2014;6:154–174. doi: 10.4330/wjc.v6.i4.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gallo P, d’Amati G, Pelliccia F. Pathologic evidence of extensive left ventricular involvement in arrhythmogenic right ventricular cardiomyopathy. Hum Pathol. 1992;23:948–952. doi: 10.1016/0046-8177(92)90410-5. [DOI] [PubMed] [Google Scholar]
- 92.Ackerman MJ, Priori SG, Willems S, Berul C, Brugada R, Calkins H, Camm AJ, Ellinor PT, Gollob M, Hamilton R, et al. HRS/EHRA expert consensus statement on the state of genetic testing for the channelopathies and cardiomyopathies: this document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA) Europace. 2011;13:1077–1109. doi: 10.1093/europace/eur245. [DOI] [PubMed] [Google Scholar]
- 93.Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, Calkins H, Corrado D, Cox MG, Daubert JP, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria. Eur Heart J. 2010;31:806–814. doi: 10.1093/eurheartj/ehq025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chellamuthu S, Smith AM, Thomas SM, Hill C, Brown PW, Al-Mohammad A. Is cardiac MRI an effective test for arrhythmogenic right ventricular cardiomyopathy diagnosis? World J Cardiol. 2014;6:675–681. doi: 10.4330/wjc.v6.i7.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.van der Zwaag PA, Cox MG, van der Werf C, Wiesfeld AC, Jongbloed JD, Dooijes D, Bikker H, Jongbloed R, Suurmeijer AJ, van den Berg MP, et al. Recurrent and founder mutations in the Netherlands: Plakophilin-2 p.Arg79X mutation causing arrhythmogenic right ventricular cardiomyopathy/dysplasia. Neth Heart J. 2010;18:583–591. doi: 10.1007/s12471-010-0839-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mohsen A, Panday M, Wetherold S, Jimenez A. Cardiac sarcoidosis mimicking arrhythmogenic right ventricular dysplasia with high defibrillation threshold requiring subcutaneous shocking coil implantation. Heart Lung Circ. 2012;21:46–49. doi: 10.1016/j.hlc.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 97.Kitaoka H, Doi Y, Casey SA, Hitomi N, Furuno T, Maron BJ. Comparison of prevalence of apical hypertrophic cardiomyopathy in Japan and the United States. Am J Cardiol. 2003;92:1183–1186. doi: 10.1016/j.amjcard.2003.07.027. [DOI] [PubMed] [Google Scholar]
- 98.Spirito P, Autore C. Apical hypertrophic cardiomyopathy or left ventricular non-compaction? A difficult differential diagnosis. Eur Heart J. 2007;28:1923–1924. doi: 10.1093/eurheartj/ehm266. [DOI] [PubMed] [Google Scholar]
- 99.Sakamoto T, Tei C, Murayama M, Ichiyasu H, Hada Y. Giant T wave inversion as a manifestation of asymmetrical apical hypertrophy (AAH) of the left ventricle. Echocardiographic and ultrasono-cardiotomographic study. Jpn Heart J. 1976;17:611–629. doi: 10.1536/ihj.17.611. [DOI] [PubMed] [Google Scholar]
- 100.Yamaguchi H, Ishimura T, Nishiyama S, Nagasaki F, Nakanishi S, Takatsu F, Nishijo T, Umeda T, Machii K. Hypertrophic nonobstructive cardiomyopathy with giant negative T waves (apical hypertrophy): ventriculographic and echocardiographic features in 30 patients. Am J Cardiol. 1979;44:401–412. doi: 10.1016/0002-9149(79)90388-6. [DOI] [PubMed] [Google Scholar]
- 101.Madias JE. Electrocardiogram in apical hypertrophic cardiomyopathy with a speculation as to the mechanism of its features. Neth Heart J. 2013;21:268–271. doi: 10.1007/s12471-013-0400-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


