Abstract
Aim
This systematic review aimed at examining the best available evidence on the effectiveness of community-based nutrition education in improving the nutrition status of under five children in developing countries.
Methods
A systematic search of the literature was conducted utilising the following data bases: Cumulative Index to Nursing and Allied Health Literature (CINAHL), EMBASE, Medline, and Web of Knowledge. 9 studies were identified for the critical appraisal process. The Joanna Briggs Institute (JBI) critical appraisal check-list for experimental studies was utilised and two reviewers conducted the appraisal process independently. 7 studies were included for this review and data was extracted using the JBI data extraction form for experimental studies. The extracted data was heterogeneous as such narrative synthesis was conducted.
Results
The nutritional status of children in all studies improved and this was evidenced by increases in weight, height, mid upper arm circumference and reduced morbidity. Key messages about education were age at introduction of complementary foods, nutrition value on different types of feeds found locally and frequency of feeding the children. However, there were varied results regarding the effects of the intervention on the nutrition status of children. This was attributed by differences in implementers' characteristics, different intervention strategy and intensity, difference in age of the children at enrolment, pre-existing children's growth and nutritional status and follow-up periods. In addition to home visiting, conducting group meetings of care givers and community leaders, providing education twice a week and use of cooking demonstrations have shown that they produce highly significant findings.
Conclusion
The evidence from the identified studies suggests that community- based nutrition education improves the nutrition status of under-five children in developing countries.
Background
The prevalence of childhood malnutrition remains high in the developing world1. Malnutrition rate is high between the ages of 6 to 24 months because breast milk alone is not enough to meet the nutritional needs of the child and other foods are introduced2. World Health Organisation (WHO)3 defines complimentary feeding as the introduction of other foods and/ or energy containing liquids to young children in addition to breast milk. While some studies indicate that complementary feeding can be introduced at 4 months4,5 WHO6, recommends that children should be introduced to complementary foods at 6 months. The food that is given should be safe, adequate and appropriate to prevent growth faltering in under-five children thereby reducing childhood deaths.4 One of the major causes of malnutrition in young children in developing countries is poor feeding practices such as: introducing complimentary foods at an early or late stage, restriction in food selection and giving children poor quality and insufficient amounts of complimentary foods.6,7,8,9 It is argued that poor feeding practices are associated with caregivers poor knowledge, lack of information and their being restricted by traditional beliefs10. Poverty is another major cause and affects food choices1 With poverty, caregivers tend to give children the food that is available regardless of its nutrition value11 Shortage of health-care providers, HIV and AIDS and few health care facilities are some of the contributing factors to malnutrition. In developing countries there is critical shortage of health-care providers12. This has been made worse by the accelerating labour migration which is causing loss of nurses and doctors from countries that can least afford the brain drain13. There is also an increase in disease burden due to HIV and AIDS and as a result more of these health-care workers are based in the health care facility with few in the community. Consequently, primary care activities are not given a priority. There are a few health care facilities which are located very far from people and as such most people go to the hospital when they perceive an illness to be serious. As a result, health workers are mostly busy attending to serious cases and do not give much attention to preventive services such as health education. These factors provide a threat to the attainment of health-related millennium development goals number 4 and 6, which aim to reduce child mortality and combat HIV/ AIDS, malaria and other communicable diseases respectively3. It is against this background that numerous strategies have been put in place to reduce the prevalence rate of malnutrition in children. These strategies are: provision of supplementary feeding, fortified foods, immunisations and nutrition education1,14. To combat malnutrition it has been recommended by many researchers that nutrition intervention should be accessible, sustainable, culturally sensitive and integrated with local resources7,15,16. One such intervention is the training of some community members to provide nutrition education to care-givers in their villages to prevent and improve childhood under-nutrition. This systematic review will therefore evaluate the best available evidence on the effectiveness of community-based nutrition education in improving the nutrition status of under-five children in developing countries.
Methods
A comprehensive and systematic search of CINAHL, EMBASE, MEDLINE, PubMed and Web of Knowledge was undertaken utilising synonyms of the following key terms: Children, Community- based nutrition education and Nutrition Status. Search strings were created by combining the Boolean operators OR and AND. The search included studies with the following qualities: randomised controlled trials, quasi experimental studies, primary research from peer- reviewed journals, studies that used nutrition education or counselling as interventions The interventions were delivered within the community or at home to groups or individual care takers by health-care providers and trained community members and/ or peer counsellors. Before the implementation of the intervention, the implementers should have received training on nutrition content The studies should have been written in the English language, conducted in developing countries and whose outcomes were increase in weight and height. The review excluded studies that evaluated the effectiveness of provision of supplementary or complementary feeding; those that combined the interventions of education and provision of supplementary feeding, systematic reviews, studies that looked at education provided at a health facility and those that looked at education provided to children at school. The search identified 5,074 articles for review. After reading the topic and abstract, 38 articles were identified. Full text articles assessed for eligibility were 25. After removing duplicates and systematic reviews, 9 studies were identified and appraised by two reviewers for methodological quality using the standardised critical appraisal instrument for Experimental Studies from the Joanna Briggs Institute. This process resulted in 7 studies for inclusion in this review (figure 1).
Fig 1.
Literature search and study identification
These findings show that community-based nutrition education is effective in improving the nutrition status of under-five children in developing countries. This is evidenced by the increase in weight18,21, length,8 weight and height,10,20 weight, height and Mid Upper Arm Circumference19 weight and reduced morbidity.17
Discussion
Results from this review suggest that nutrition education provided to care-givers in their homes or community improves the nutrition status of under-five children in developing countries. To produce highly significant results, findings from this review suggest conducting group meetings of care givers and community leaders, providing education at frequent intervals for example twice a week and use of cooking demonstrations in addition to home visiting. Providing nutrition training to implementers prior to implementation of the study helped them to demonstrate higher levels of nutrition knowledge and counselling skills which they previously lacked22. This helped them to provide relevant nutritional education to care givers hence significant results were produced. However, this review has found varied results regarding the effects of the intervention on the nutrition status of children. The possible reasons for the difference are: different intervention strategy and intensity, difference in age of the children at enrolment, pre-existing children's growth and nutritional status. This was also previously reported in7 where they looked at effectiveness of educational interventions for improving complementary feeding practices. The difference with this review is the setting in which the implementation was conducted. In7 the interventions were delivered in various settings including the hospital while this review concentrated on educational interventions delivered in the community or home. In addition, implementers for studies in this systematic review had different characteristics. In 8 studies health-care providers and nutrition workers implemented the intervention. In 17 studies the implementers were graduate-level health assistants,18 used community health workers 21 used mentor mothers and 10,19,20 had trained community members and/ or peer counsellors. Health care providers, nutrition workers, graduate-level health assistants and community health workers may have had good understanding of nutrition as a subject and experience in community teaching compared to community members and peer counsellors. These implementers were able to disseminate information to the intervention group in a simple way hence results of their studies were highly significant. Comparing children of different nutritional status would not bring the same effect of the intervention because malnourished children usually present with other medical conditions due to reduced immunity and as such, their appetite is reduced and they would not eat well compared to normal children. Even when the malnourished child eats well, the nutrients will be used to treat or rehabilitate the condition first and then later for catch up growth23. Having children of different nutritional status in the same study meant that the nutrition education was the same yet they had different nutritional needs. This might mean that the care-givers followed the advice that they were given, only that it did not suit their children's needs. In this case the nutrition status of malnourished children would not improve at the same rate as that of normal children.
Implication for clinical practice
Children of different nutritional status should not be given the same nutrition information because they have different nutritional needs. Therefore, the education content should aim to target the audience. The education can also be more or less effective depending on the circumstance. With shortage of health care workers, utilising trained local people to provide nutrition counselling has shown to be effective. Instead of just asking any volunteer to provide nutrition education, it is necessary to consider care givers whose children are well nourished but living under the same conditions to act as mentors to other community members. By doing this it will be easy for the care-givers to change their behaviour since they will be encouraged by people whom they know and they will be able to understand that it is possible to have well-nourished children even in poor conditions.
Limitations
This review included studies published in peer- reviewed journals only. Studies published in non-English language were not included and as such only seven articles were included, of which six are from Asia and one from Africa. This has brought bias as the small number of studies and countries does not provide a good representation of all developing countries. There may be a lot of unpublished work which has not been included in this review and this has contributed to publication bias.
Further Research
Further research conducted in other developing countries would be of great help in concluding that community-based nutrition education is effective in improving the nutrition status of under-five children. The research should consider all the three nutritional indices which are: weight- for- age, weight- for-height and height- for- age. It should also be conducted on a large scale to allow in-depth analysis of the findings. Data of malnourished children should be analysed differently so as to understand the effects of the intervention on malnourished children22.
Conclusion
Evidence from the identified studies in this review suggests that community- based nutrition education improves the nutrition status of under-five children in developing countries.
Table 1.
Characteristics of included studies
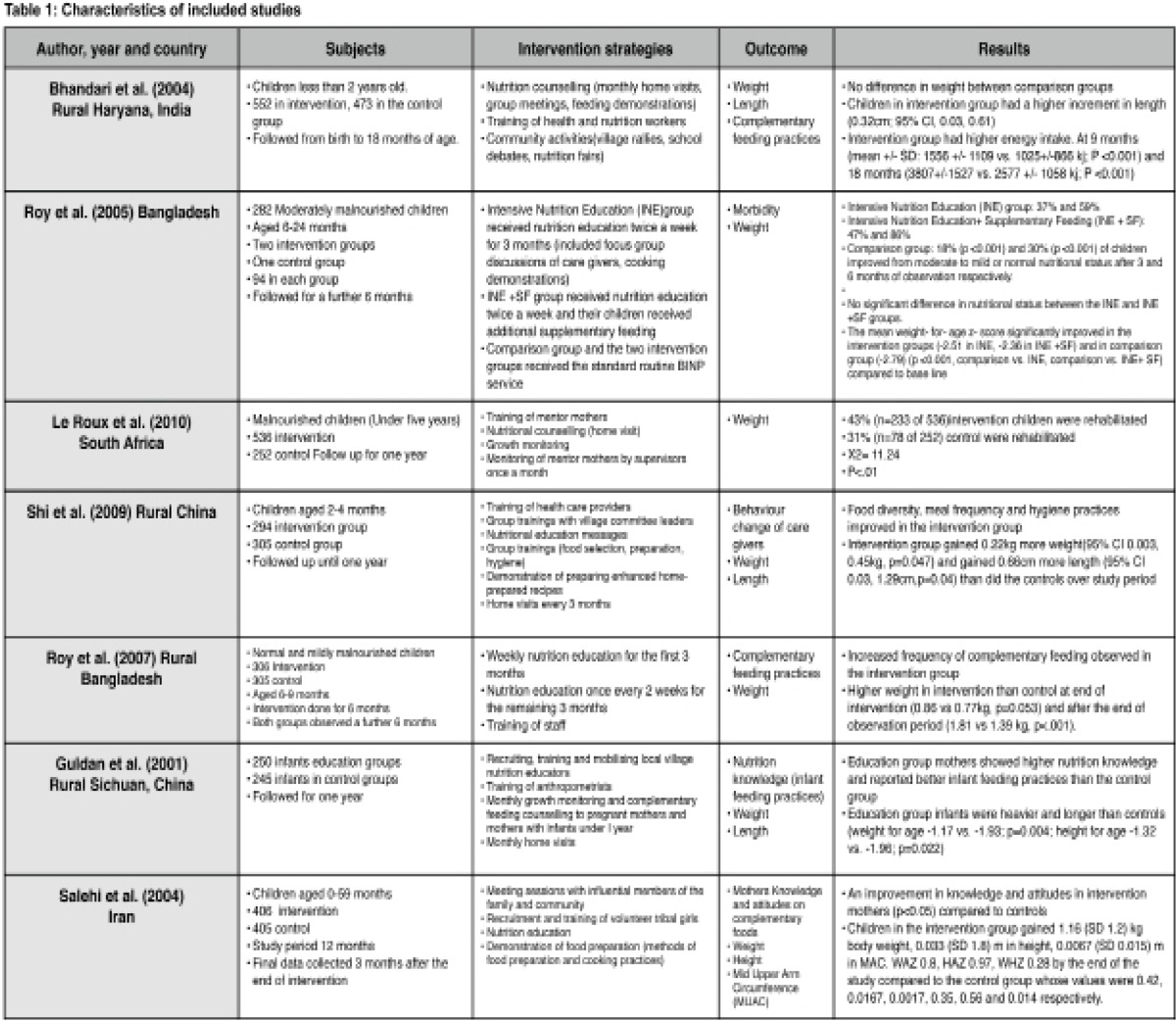 |
Table 2.
Results
|
Characteristics of implementers |
|
| Training |
|
| Nutrition education |
|
|
Mode of intervention delivery |
|
| Study period | |
| Setting |
|
| Outcome description |
Acknowledgements
I would like to thank Judith Carrier for her guidance and support. This work was supported by funding from the Government of Malawi through University of Malawi. The funding was granted to the first author as part of Masters studies.
Conflicts of interest
There are no financial and non-financial conflicts of interest in this review
Authors' Contributions
Maureen D. Juma Majamanda developed a protocol for this review, conducted the search strategy, appraisal of studies, data extraction and data synthesis under the supervision of Judith Carrier. Tiwonge Mbeya Munkhondia conducted the appraisal of studies. All contributed to the editing of this manuscript.
References
- 1.Imdad A, Yakoob MY, Bhutta ZA. Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health. 2011;11(Suppl 3):S25. doi: 10.1186/1471-2458-11-S3-S25. http://dx.doi.org/:10.1186/1471-2458-11-S3-S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shrimpton R, Victoria CG, de Onis M, Lima RC, Blossner M, Clugston G. Worldwide timing of growth faltering: Implications for nutritional interventions. Journal of the American Academy of Paediatrics. 2001;107(5):e75. doi: 10.1542/peds.107.5.e75. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organisation, author. Complementary Feeding. 2011. [5/06/2011]. http://www.who.int/nutrition/topics/complementary_feeding/en/index.html.
- 4.Brown KH, Duggan C, Watkins J, Walker WA. Nutrition in Pediatrics: Basic Science & Clinical Applications. 4th edn. BC Decker Inc.; 2008. Chapter 36. Complementary feeding; pp. 411–116. [Google Scholar]
- 5.Duijts L, Jaddoe VWV, Hofman A, Moll HA. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Paediatrics. 2010;126(1):e18–e25. doi: 10.1542/peds.2008-3256. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organisation, author. Report of Informal Meeting to Review and Develop Indicators for Complementary Feeding. Washington D.C: 2002. [Google Scholar]
- 7.Shi L, Zhang J. Recent evidence of the effectiveness of educational interventions for improving complementary feeding practices in developing countries. Journal of Tropical Paediatrics. 2010;57(2):91–98. doi: 10.1093/tropej/fmq053. [DOI] [PubMed] [Google Scholar]
- 8.Bhandari N, Mazumder S, Bahl R, Martines J, Black RE, Bhan MK. An educational intervention to promote appropriate complementary feeding practices and physical growth in infants and young children in rural Haryana, India. The Journal of Nutrition. 2004;134:2342–2348. doi: 10.1093/jn/134.9.2342. [DOI] [PubMed] [Google Scholar]
- 9.Dewey KG, Brown KH. Update on technical issues concerning complementary feeding of young children in developing countries and implications for intervention programs. Food and Nutrition Bulletin. 2003;24(1):5–28. doi: 10.1177/156482650302400102. [DOI] [PubMed] [Google Scholar]
- 10.Guldan GS, Fan HC, Ma X, Ni ZZ, Xiang X, Tang MZ. Culturally Appropriate Nutrition Education Improves Infant Feeding and Growth in Rural Sichuan, China. Journal of Nutrition. 2000;130:1204–1211. doi: 10.1093/jn/130.5.1204. [DOI] [PubMed] [Google Scholar]
- 11.Vorster HH, Kruger A. Poverty, malnutrition, under-development and cardiovascular disease: A South African perspective. Cardiovascular Journal of Africa. 2007;18(5):321–324. [PMC free article] [PubMed] [Google Scholar]
- 12.Task Force on Health Systems Research, author. Informed choices for attaining the millenium development goals: Towards an international cooperative agenda for health systems research. Lancet. 2004;364:997–1003. doi: 10.1016/S0140-6736(04)17026-8. http://dx.doi.org/10.1016/S0140-6736(04) 17026-8. [DOI] [PubMed] [Google Scholar]
- 13.Chen L, Evans T, Anand S, Boufford JI, Brown H, Chowdhury M, Cueto M, Dare L, Dussault G, Elzing G, Fee E, Habte D, Hanvoravongchai P, Jacobs M, Kurowski C, Michael S, Pablos-Mendez A, Sewankambo N, Solimano G, Stiwell B, Waal A, Wibulpolprasert S. Human Resources for Health: Overcoming the Crisis. The Lancent. 2004;364(9449):1984–1990. doi: 10.1016/S0140-6736(04)17482-5. [DOI] [PubMed] [Google Scholar]
- 14.Pelletier DL, Frongillo EA. Changes in child survival are strongly associated with changes in malnutrition in developing countries. Journal of Nutrition. 2003;133:107–119. doi: 10.1093/jn/133.1.107. [DOI] [PubMed] [Google Scholar]
- 15.Penny ME, Creed-Kanashiro HM, Roberts RC, Narro MR, Caulifield LE, Black RE. Effectiveness of an educational intervention delivered through the health services to improve nutrition in young children: A cluster randomised controlled trial. Lancet. 2005;365:1863–1872. doi: 10.1016/S0140-6736(05)66426-4. [DOI] [PubMed] [Google Scholar]
- 16.Kilaru A, Griffiths PL, Ganapathy S, Ghosh S. Community-based nutrition education for improving infant growth in rural Karnataka. Indian Paediatrics. 2005;42:425–432. [PubMed] [Google Scholar]
- 17.Roy SK, Jolly SP, Fuchs GJ, Mahmud Z, Gulshan A, Islam S, Shafique S, Akter SS, Chakraborty B. Intensive nutrition education with or without supplementary feeding improves the nutritional status of moderately- malnourished children in Bangladesh. Journal for Health Population and Nutrition. 2005;23(4):320–330. [PubMed] [Google Scholar]
- 18.Roy SK, Jolly SP, Shafique S, Fuchs GJ, Mahmud Z, Chakraborty B, Roy S. Prevention of malnutrition among young children in rural Bangladesh by a food-health-care educational intervention: A randomised, Controlled Trial. Food and Nutrition Bulletin. 2007;28(4):375–383. doi: 10.1177/156482650702800401. [DOI] [PubMed] [Google Scholar]
- 19.Salehi M, Kimiagar SM, Shahbazi M, Mehrabi Y, Kolahi AA. Assessing the impact of nutrition education on growth indices of iranian nomadic children: an application of a modified beliefs, attitudes, subjective- norms and enabling-factors model. British Journal of Nutrition. 2004;91:779–787. doi: 10.1079/BJN20041099. http://dx.doi.org/10.1079/BJN20041099. [DOI] [PubMed] [Google Scholar]
- 20.Shi L, Zhang J, Wang Y, Caulifield LE, Guyer B. Effectiveness of an educational intervention on complementary feeding practices and growth in rural china: A cluster randomised controlled trial. Public Health Nutrition. 2009;13(4):556–565. doi: 10.1017/S1368980009991364. [DOI] [PubMed] [Google Scholar]
- 21.Le Roux IM, Le Roux K, Comulada WS, Greco EM, Desmond KA, Mbewu N, Rotheram-Borus MJ. Home visits by neighbourhood mentor mothers provide timely recovery from childhood malnutrition in South Africa: Results from a Randomised Controlled Trial. Nutrition Journal. 2010;9:56. doi: 10.1186/1475-2891-9-56. http://dx.doi.org/10.1186/1475-2891-9-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pelto GH, Santos I, Goncalves H, Victoria C, Martines J, Habicht JP. Nutrition Counselling training changes Physician behaviour and improves care giver knowledge acquisition. Journal of Nutrition. 2004;134(2):357–362. doi: 10.1093/jn/134.2.357. [DOI] [PubMed] [Google Scholar]
- 23.Ashworth A, Ferguson E. Dietary Counselling in the Management of Moderately Malnourished Children: WHO Technical Background Paper. 2008. [28/08/2011]. http://www.who.int/nutrition/publications/moderate_malnutrition/MM_Background_paper3.pdf.



