Abstract
Background:
The uterus continues to contract after childbirth. The pain caused by the contractions of the uterus can be as severe as labor pain. The study was aimed to evaluate the effects of ice massage applied to the large intestine 4 (LI4) on postpartum pain during the active phase of labor.
Materials and Methods:
The study was designed as a randomized controlled trial with three groups and carried out in two stages. The study sample comprised of 150 pregnant women, who were referred to a maternity hospital. In the experimental group, ice massage was applied to LI4 during four contractions within the active phase of labor. In the placebo group, pressure was applied to LI4 using silicone balloons and the third group was the control group. The Visual Analog Scale (VAS) and The McGill (Melzack) Pain Questionnaire (MPQ) were compared among the experimental, placebo, and control groups.
Results:
The mothers in the ice application group had the lowest mean VAS score. It was determined that ice massage applied to LI4 during the active phase of labor did not lead to any statistical differences in mothers in the first 24 hours postpartum in terms of the characteristics of the pain with MPQ and VAS.
Conclusions:
In the study, the perception of pain was tried to be minimized by applying pressure with ice balloons to LI4. However, although the application was determined to have made no difference in the pain intensity, the mothers’ statements in the ice application group suggested that they felt more comfortable than did the mothers in the other groups.
Keywords: Hegu, ice massage, large intestine meridian point 4, postpartum pain
INTRODUCTION
The International Association for the Study of Pain's widely used definition states: Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.[1] Usually, pain is a signal of a potential threat, which should be diminished or eliminated. Furthermore, childbirth pain differs from other types of pain with respect to its positive outgrowth; a child is born.[2] Pain in the immediate postpartum period arises from laceration and stretching of the perineum. The pain also arises from episiotomy, incision, postpartum uterine contractions, hemorrhoids, breast engorgement, and the stretching of the nipple.[3,4] The uterus continues to contract after childbirth. Pain caused by the contractions of the uterus can be as severe as labor pain. On account of oxytocin secretion, the pain becomes very severe in nursing mothers.[3,4,5]
On account of the properties and subjectivity of pain, the most reliable indicator used for the assessment of pain is the patient's description of it in her own words. Even as pain is assessed, the intensity, type, property, location and time, and factors reducing or increasing the pain must be known.[6] On the other hand, there is no specific instrument designed to measure the contraction pain experienced during labor, but in several studies the Visual Analog Scale (VAS) has been used.[7,8,9]
There has been enormous growth in complementary alternative medicine (CAM) research in the past decade within the framework of traditional Chinese medicine. The stimulation of acupuncture points in this treatment is a method of initiating, controlling or accelerating body functions by stimulating the energy channels beneath the skin's surface and rebalancing the body's energy (Qi) to restore health.[10,11] Pressure on the acupuncture points can also be exerted with fingers, tennis balls, towels, and the like.[12,13] In this study, the Large Intestine 4 (LI4) (hegu) was used. As the upper portion of the uterus is encircled by the colon at full-term pregnancy, the location of LI4 is a point where the energy flow of the meridian is closest to the skin and can be easily stimulated with pressure, needles or extreme cold.[10]
The review of studies conducted on the applications to LI4 revealed a pilot study, which was developed on the basis of Dr. Melzack's use of ice massage of LI4, to reduce dental pain after Aleda Erskine linked dental pain, child-birth pain, and myocardial infarction under the category of acute clinical pains.[10] The review also revealed that there were other studies conducted to evaluate the effect of ice massage on eliminating pain in young women with dysmenorrhea.[14,15] In a study conducted on relieving labor pain, the researcher performed ice massage of the energy meridian LI4 during each contraction.[10,16,17]
The database on VAS showed a mean reduction in pain of 25.15. This mean score could be considered statistically significant, despite the small number of participants. In the same study, the effectiveness of ice massage applied to the energy meridian points in order to reduce pain during labor contractions was evaluated as well.[10] Chung et al. (2003), performed a study to determine the effects of pressure applied to LI4 and BL67 on labor pain and uterine contractions and the differences between acupressure, effleurage, and control groups, and they observed that the relief of labor pain was higher in women in the acupressure group.[18] Another study was designed to assess the effects of noninvasive electroacupuncture at LI4 on labor pain and stress-hormone responses to that pain.[19] Furthermore, in order to reduce the perception of labor pain, ice massage was applied to LI4 and no difference was determined between the groups, in terms of the pain level.[9] However, according to the results of some studies, the pain decreased after ice massage application.[13] According to Melzack's hypothesis, the efficacy of ice massage was due to engaging the gate control system of pain rather than eliminating the source of the pain.[10,16]
This present study was designed to evaluate, with MPQ, the effect of cold applied to LI4 during the labor process on postpartum pain.
MATERIALS AND METHODS
Study design
The study was designed as a randomized, clinical, controlled trial.
Participants
The study sample comprised of 150 pregnant women, who presented to a general maternity hospital in Izmir to deliver their babies and met the study criteria. The pregnant women were divided into three groups: Ice application group (experimental) (n = 50), silicone application group (placebo) (n = 50), and control group (n = 50). Of the women, those who had full-term pregnancy, single fetus, 4–8 cm cervical dilatation, with regular contractions, no pregnancy complications systemic non-neurological illness or contraction abnormalities, and who agreed to participate in the study were included in the study.
Forms
The data were collected with the following three forms: (1) The Socio-demographic, and Intrapartum and Postpartum Follow-up Questionnaire, (2) The Visual Analog Scale (VAS), to determine the level of pain, (3) The McGill (Melzack) Pain Questionnaire (MPQ).
The visual analog scale
It is a single-item scale and used to measure perceived pain. It is a continuous scale comprised of a horizontal or vertical line, usually 10 cm (100 mm) in length. For pain intensity, the scale is most commonly anchored by ‘no pain’ (score of 0) and ‘pain as bad as it could be’ or ‘worst imaginable pain’ (score of 100 (100-mm scale)).[6,20,21]
McGill pain questionnaire
The reason why the MPQ was preferred in this study was that it was the most widely examined multidimensional method of pain assessment, that its validity and reliability had been tested the most, and it was the most widely used pain assessment tool. The MPQ was developed by Melzack and Torgerson in 1971. The validity and reliability study of the Turkish version of the MPQ was conducted by Kuguoğlu, et al. in 1998. The Cronbach alpha value obtained from the original tool was 0.98.[22] In this study, the Cronbach alpha value was calculated as 0.82. The MPQ was administered by the researchers to the patients who agreed to participate in 15- to 20-minute interviews.
The MPQ has four sections. The first section has statements about the location of the pain, the second has statements describing the pain, the third assesses the duration of the pain, and the fourth assesses the severity of the pain.[6,22,23,24]
Instruments
Ice balloons
Ice balloons were prepared to perform cold application in the experimental group. The ice balloons were first filled with about 30 cc of water and then frozen. In the study, a different ice balloon was used for each hand of the pregnant women. To ensure patient safety, the balloons were wrapped with gauze.
Silicone balloons
In the placebo group, balloons similar to ice balloons but filled with silicone were used. As in the experimental group, in the placebo group too, a different silicone balloon was used for each hand of the pregnant women. To ensure patient safety, the balloons were wrapped with gauze. The purpose of using silicone balloons in the placebo group was to determine whether the pressure or the cold affected the LI4 Silicone balloon time of pressure was performed for eight contractions as intermittent (Mean = 30.38 ± 7.72 minutes).
The standardization of all the balloons used throughout the study was ensured by the researcher.
Procedures
The study, carried out in two stages, was comprised of three groups. The first stage of the study was conducted during the active phase of labor, whereas, the second stage was carried out in the postpartum period. In the first group (the experimental group), ice massage was applied to LI4 during four contractions within the active phase (after 4 cm cervical dilatation) of labor (mean 31.04 ± 11.19 minutes). In the second group (the placebo group), pressure was applied to LI4 using silicone balloons (mean 30.38 ± 7.72 minutes). In the control group, the routine birth protocol was implemented.
THE FIRST STAGE
In all the three groups, external fetal monitoring (EFM) was used to monitor contractions and fetal heart rates during the applications. At the end of the application, the duration, frequency, and severity of the contractions in the pregnant women were assessed. The research data were collected from the patients in the three groups. They are as follows:
A- Ice and silicone balloon application groups
Labor pain was measured with VAS before the ice and silicone balloon massages were applied to LI4 (beginning of the application)
LI4 (located between the thumb and index finger) of the pregnant woman was determined [Figure 1]
Ice and silicone balloons wrapped with gauze were applied to LI4 between the start and end of each contraction
During the contraction, the pregnant women were asked to hold the ice or silicone balloon in their hands
Between contractions, the applications were suspended
As the next contraction started, the pregnant women were again asked to hold the ice or silicone balloon in their hands
During each of the four contractions, ice or silicone balloons were applied to the same hand. At the end of each contraction, the pain scores of the pregnant women were determined with VAS
At the same time, the duration and severity of the contractions in the patients were assessed with electronic fetal monitoring.
Figure 1.
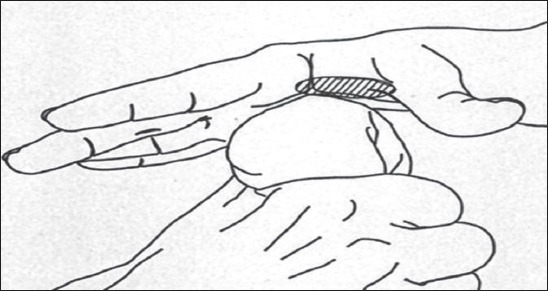
Ice balloon application to LI4
B-Control group
The pregnant women in this group underwent only routine interventions. The women in this group did not use any special technique for pain. Each woman's vital signs, contractions, cervical dilatation, and descent of the baby were followed.
THE SECOND STAGE
Before the women in all the three groups were discharged from the hospital, after giving birth, the Postpartum Follow–up Questionnaires were filled out, and their pain levels were assessed with VAS and MPQ.
Data analysis
The data obtained were analyzed by the Statistical Package for Social Science for Windows (SPSS 16.0). The frequency and percentage values of the group variables, the means, and standard deviations of the numeric variables were calculated. The One-Way Analysis of Variance (ANOVA) and the Chi-square test were used to determine the difference between the groups. For detailed analysis, the Scheffe Test was used in this study, and a P < 0.05 was considered to be statistically significant.[25]
Permissions and ethics
Permissions were obtained from the Scientific Ethics Committee of the Ege University School of Nursing before the study and then, during the data collection phase, from the Provincial Health Directorate of the Ministry of Health and the Chief Physician of the hospital. Written informed consents of the mothers who participated in the study were obtained before the study was conducted.
RESULTS
The study was designed to evaluate the effect of ice massage applied to LI4 during the active phase of labor on postpartum pain with MPQ in the second stage of the two-stage research. The postpartum interview was done with the mothers about 17.57 ± 6.52 hours after childbirth before they were discharged from the hospital. The mean of the mothers’ ages was 23.86 ± 4.38 years.
The pregnant women included in all the three groups of the study were alike in terms of age, number of pregnancies, cervical dilatation at the beginning of the application, and time of postpartum interviews (P > 0.05).
Of the mothers, 97.3% suffered postpartum pain. All the mothers in the control group and 94.0% of the mothers in the ice application group had postpartum pain. Although the mothers in the silicone application group had the lowest mean VAS score and the control group the highest mean VAS score, the difference between the groups was not statistically significant (P > 0.05) [Table 1].
Table 1.
The mothers’ postpartum pain status and pain intensity
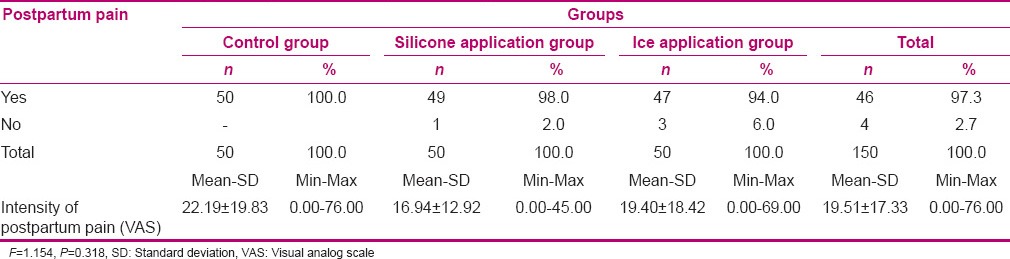
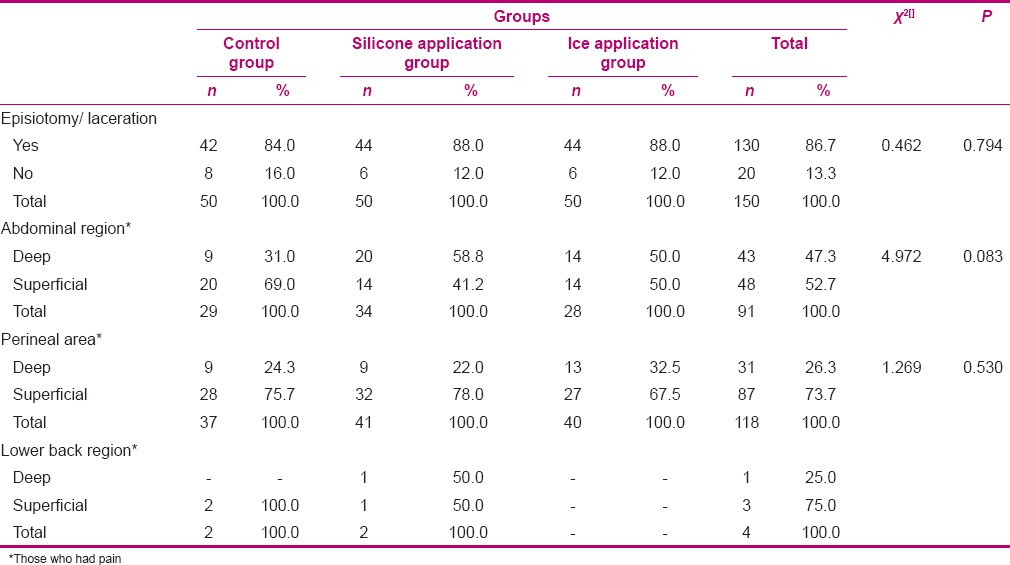
Table 2 shows the distribution of episiotomy/laceration and postpartum pain suffered by the mothers in terms of the characteristics of the pain. It was determined that 52.7% of the mothers with abdominal pain, 73.7% of the mothers with perineal pain, and 75.0% of the mothers with lower back pain described the pain as ‘superficial’. There was no statistically significant difference between the groups in terms of the characteristics of postpartum pain (P > 0.05). Of the mothers, 86.7% suffered episiotomy/laceration. The incidence rate of episiotomy/laceration was similar in all the three groups (P > 0.05). None of the mothers was determined for breast pain.
Table 2.
Distribution of Episiotomy/laceration, postpartum pain suffered by the Mothers in terms of the characteristics of the pain
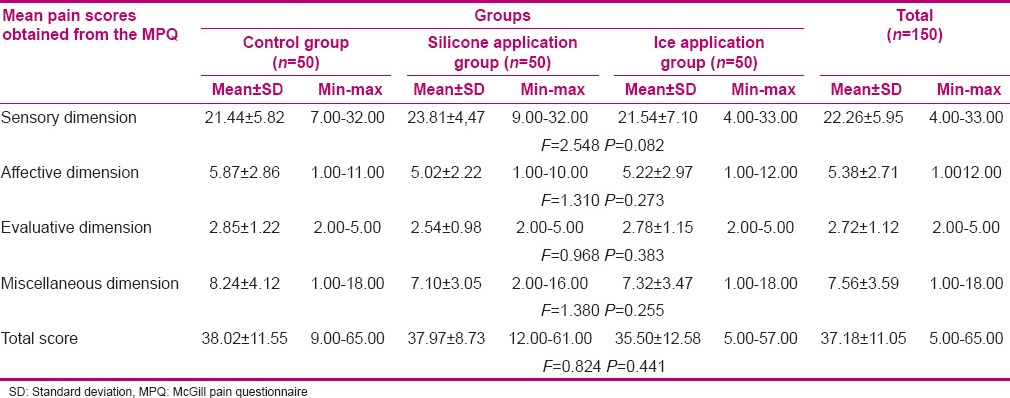
Assessment of postpartum pain with MPQ is given in Table 3. Based on this assessment, it was determined that ice massage applied to LI4 during the active phase of labor did not lead to any statistical differences in mothers in the first 24 hours postpartum, in terms of the characteristics of the pain (P > 0.05). However, there were statistically significant differences between the groups based on the assessment carried out with items 14 and 19 of the MPQ, which were used to evaluate the perceptual and miscellaneous dimensions of pain (P < 0.05). Based on the fourteenth item, most of the mothers in the ice application and control groups described the pain as ‘cruel,’ whereas, most of the mothers in the silicone application group described it as ‘punishing’. Based on the nineteenth item, the mothers in the silicone and ice application groups mostly described the pain as ‘cool’.
Table 3.
Distribution of patients’ words descriptors of postpartum pain
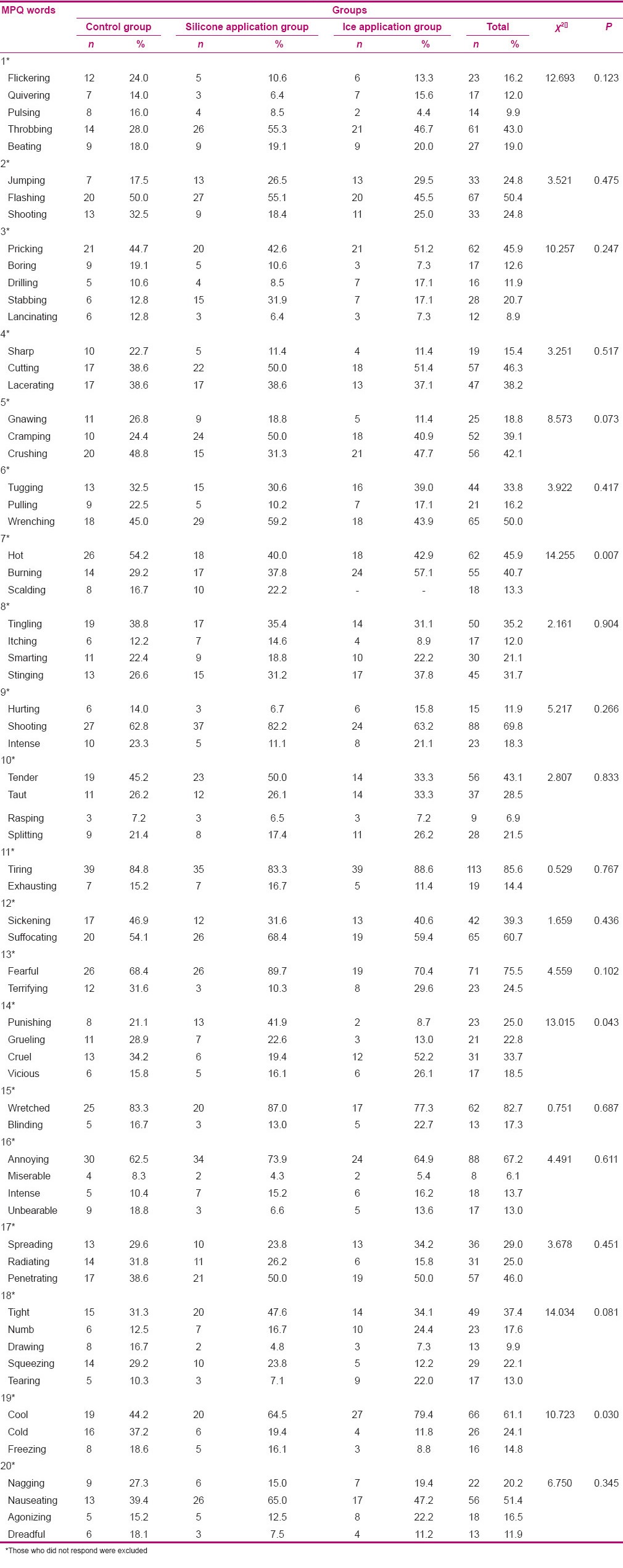
Table 4 shows the mean postpartum pain scores obtained by the mothers from the MPQ. When the groups were compared in terms of the mothers’ perception of postpartum pain for the sensory, affective, evaluative, and miscellaneous dimensions, the differences between the groups were not statistically significant (P > 0.05). The total mean MPQ score was 37.18 ± 5.11 (Min. = 5.00 Max. = 65.00). When the groups were compared in terms of total scores obtained from the second part of the MPQ, no statistically significant difference was determined between the groups (P > 0.05).
Table 4.
Comparison of the mean postpartum pain scores mothers obtained from the MPQ
DISCUSSION
In the first part of the study, a reduction was determined in labor pain perceived by the pregnant women who had ice application to LI4 during the active phase of labor. Although the difference between the groups in terms of the duration of labor was not significant, the women in the ice application group had the shortest duration of labor (4.88 ± 2.47 hours).[9]
Previous studies carried out in Turkey on postpartum care mostly focused on alternative postpartum applications,[26,27,28] adaptation to motherhood,[29] factors affecting postpartum comfort, and determination of postpartum health needs.[30,31] Previous studies have examined associations between physical symptoms after childbirth. Therefore, there is a need to conduct studies to assess postpartum pain. We described discomfort with particular attention to postpartum pain.
It has been reported that postpartum pain develops due to uterine involution, perineal episiotomy/laceration, and fatigue experienced by the mother during labor.[24] Even as the incidence of pain due to episiotomy in women who had vaginal delivery was 28% in one study,[30] it was 30.4% in another study.[31]
A painful perineum was frequently reported by women with an assisted vaginal delivery (77% among primiparas and 52% among multiparas), and by primiparas with a spontaneous vaginal delivery (73%, with 28% describing it as major).[32] Pain and discomfort related to perineal trauma have been reported to interfere with women's daily activities, postpartum, such as, sitting, walking, or lifting the baby. Besides, neck and shoulder pain, low back pain, and dyspareunia came third in ranking, being listed by 28 – 29% of the women.[33]
A majority of the mothers, in all the groups (86.7%), who had episiotomy/laceration, suffered severe pain in the perineum and had abdominal pain due to rapid uterine involution during the early postpartum period, which suggested that it was a normal process.
In their literature review, Niven and Murphy-Black (2000) report that that postpartum pain is not forgotten immediately,[34] and that the anxiety and stress experienced by women and negative attitudes displayed by the clinical staff during labor cause the women to recall the pain for a long time.[35]
In this study, the incidence of abdominal and perineal pain in the early postpartum period was high, but the women describing it as superficial was noteworthy because it indicated that postpartum pain was temporary and did not affect the mother's life much. However, more mothers in the ice application balloon group described pain in their perineal area as ‘deep,’ as against those in the other groups. This was because, in this group, the episiotomy rate was thought to be high.
Of the mothers who stated that they had pain during the interviews held after birth, those in the silicone application group had lower VAS pain scores than did those in the other groups, but the scores in the other two groups were not high either. But, Kaviani et al. (2012), Both acupressure and ice massage led to reduced pain intensity in labor.[36] In addition, when the pain was assessed with the four dimensions of the MPQ, it was observed that the mothers described their pain as ‘throbbing’, ‘reflective’, ‘prickling’, ‘cutting’, ‘crushing’, ‘twisting’, ‘searing’, ‘shooting’, and ‘tender’ for the sensory dimension. As a large number of the mothers had episiotomy/laceration, it was an expected phenomenon that the pain felt was ‘pulsating or cutting’ in nature. It was also expected that the pain would be ‘searing or shooting’ in nature because of wound healing. For the affective dimension, the mothers described their postpartum pain using expressions such as, ‘exhausting’, ‘suffocating’, ‘terrifying’, ‘unbearable,’ and ‘wretched’.
The mothers described their postpartum pain as ‘miserable’ for the evaluative dimension of the MPQ, and as ‘penetrating’, ‘nuisance’, ‘shivering’, and ‘disturbing’ for the miscellaneous dimension of the MPQ.
In a study conducted to evaluate the sensory dimension of the MPQ during both stages of labor, the pain was described as ‘cramping’, ‘pulling’, ‘stabbing,’ and ‘cutting’.[37] In another study conducted to investigate ‘cultural differences regarding labor pain’, the participants described pain as, ‘burning’, ‘piercing’, ‘cramping’, ‘sharp’, ‘stabbing’, ‘severe’, ‘tiring’, ‘exhausting,’ and ‘tense’.[38,39] In this study, no statistically significant difference was determined between the groups in terms of the sensory dimension of pain (P > 0.05), which indicated that applying ice massage during the active phase of labor had no effect on reducing postpartum pain.
Acupressure is pressure with fingers or small beads on acupuncture points. It is used for labor pain. As acupressure can be done, with minimal instruction, by the woman's partner, it may be desired by some laboring women.[13] Comparison of mean pain intensity pre intervention with the mean pain intensity post intervention in the ice massage group showed a significant difference in the labor. A significant difference was also observed in the acupressure group between pain intensity half-an-hour post intervention.[40] However, there are no published trials of its efficacy in relieving postpartum pain. Furthermore, randomized clinical trials are needed to investigate this further. Many non-pharmacological methods help reduce labor pain, but they are not widely used.[13]
The mothers’ description of pain as ‘steady’, ‘intermittent’, and ‘temporary’ indicates that the pain is temporary and manageable in nature. During the same interview, the mothers described their ‘worst’ pain as ‘severe’ and least pain as ‘mild’. This is similar to the result of the research literature.[34]
In Eisenach et al.'s study (2008), 66% of the patients reported that their pain interfered with one or more of their daily activities – walking, mood, sleep, relations with others or ability to concentrate. The delivery mode was meaningfully related to acute pain after delivery. Based on this study, nearly 500,000 American women may experience severe acute pain after childbirth annually.[41]
CONCLUSIONS
In the study, pain suffered by mothers during labor and early postpartum period was assessed and it was attempted to minimize their perception of pain by applying pressure with ice balloons to LI4. However, although the application was determined to make no difference in pain intensity, the mothers’ statements in the ice application group suggested that they felt more comfortable than did the mothers in the other groups.
The characteristics of the pain the mothers had during the early postpartum period have been assessed with the MPQ. As the VAS is used in pain assessment more widely, studies conducted with the MPQ do not have much coverage in the literature. Even as pain was assessed with the MPQ during the early postpartum period, the mothers were given explanations and metaphors were used. Therefore, the scale was not practical to use.
Recommendation
All pregnant women should be informed about labor pain and the pain assessment process during antenatal follow-ups and pain descriptors should be determined too. In addition, during labor and the postpartum period, the mothers’ pain should be routinely assessed and interventions to reduce pain should be achieved
Acupressure should also be achieved by applying other materials to LI4 to effectively use this acupressure point, and cold application should be maintained during the whole course of labor and its effectiveness should be evaluated. In addition, it was recommended that similar studies be performed with larger sample groups, a longer duration of pressure, and other acupunture points, which could diminish pain.
Limitations
The study had some limitations:
During the data collection phase, 225 pregnant women were contacted, but the data evaluated were collected from 150 pregnant women. Of the mothers, those who had inadequate antenatal follow-ups, and the weights of whose fetuses were not measured, and those who gave birth by Cesarean section, due to obstetric reasons, were excluded from the study. Those about whom no data were collected, because they were discharged from the hospital at their own request, were also excluded from the study. Other data about them were not taken into account either
The ice application method was used only during the active phase of labor so that time spent on this method was limited
In addition, the mothers had difficulty understanding the terms used in the MPQ. Therefore, the researcher had to clarify what some of the terms meant, which suggested that when the data were collected with the MPQ, face-to-face interviews were preferred
Evaluating the characteristics of pain proved to be difficult because perception and expression of pain varied from one person to another.
ACKNOWLEDGEMENT
I would like to extend my sincere thanks to Prof. Dr. Umran Sevil, who supported the project, to Assoc. Prof. Timur Köse who performed the statistical analyzes and to all the midwives and physicians working in the hospital where the study was conducted. This article was derived from a Doctorate thesis with project number 2005/ASYO/002, Ege University Scientific Research Projects Directorate, Izmir, Turkey.
Footnotes
Source of Support: This study was supported by the ‘Ege University Scientific Research Projects Directorate,’ as a project, dated and numbered 2005/ASYO/002
Conflict of Interest: Nil.
REFERENCES
- 1.International Association for the Study of Pain: Pain Definitions IASP Taxonomy. [Last accesed on 2014 Apr 12]. Available from: https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698 .
- 2.Flink IK, Mroczek MZ, Sullivan MJL, J, Linton SJ. Pain in childbirth and postpartum recovery – The role of catastrophizing. Eur J Pain. 2009;13:312–6. doi: 10.1016/j.ejpain.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Ergin AB, Ozdamar D. Postpartum Dönem ve Ağrı [Postpartum period and pain] In: Sirin A, Kazlak O, editors. Doğum Ağrısı ve Yönetimi [Labour Pain and Management] Istanbul: BEDRAY Publishing; 2008. pp. 145–65. [Google Scholar]
- 4.Taskýn L. Doğum ve Kadın Saılığı Hem şireliği [Labour and Women Health Nursing], V.Edit. Ankara, Sistem Printing. 2012:230–2. [Google Scholar]
- 5.Lowdermilk DL, Perry SE, Bobak IM. 6th ed. United States: Mosby Inc; 1997. Maternity Women's Health Care. [Google Scholar]
- 6.Aslan FE. Ağrı Değerlendirmesi ve Ölçümü [Pain Assessment and Measurement] In: Aslan FE, editor. Agrı Dogası ve Kontrolü [Nature and Control of Pain] Istanbul: Avrupa Tıp Publishing; 2006. pp. 68–99. [Google Scholar]
- 7.Melzack R. The McGill Pain Questionnaire: Major properties and scoring methods. Pain. 1975;1:277–99. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- 8.Lee MK, Chang SB, Kang DH. Effects of SP6 acupressure on labor pain and length of delivery time in women during labor. J Altern Complement Med. 2004;10:959–65. doi: 10.1089/acm.2004.10.959. [DOI] [PubMed] [Google Scholar]
- 9.Ozturk Can H, Saruhan A. Studyýng the effect of ice-massage applied to hands of pregnant women to reduce the perceived labor pains. J Res Dev Nurs. 2008;10:18–37. [Google Scholar]
- 10.Waters BL, Raisler J. Ice Massage for the reduction of labor pain. J Midwifery Womens Health. 2003;48:317–21. doi: 10.1016/s1526-9523(03)00277-0. [DOI] [PubMed] [Google Scholar]
- 11.Tournaire M, Theau-Yonneau A. Complementary and alternative approaches to pain relief during labor. Evid Based Complement Alternat Med. 2007;4:409–17. doi: 10.1093/ecam/nem012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gentz BA. Alternative therapies for the management of pain ın labor and delivery. Clin Obstet Gynecol. 2001;44:704–32. doi: 10.1097/00003081-200112000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Simkin P, Bolding A. Update on nonpharmacologic approaches to relieve labor pain and prevent suffering. J Midwifery Womens Health. 2004;49:489–504. doi: 10.1016/j.jmwh.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 14.Chen HM, Chen CH. Effects of acupressure on menstrual distress in adolescent girls: A comparison between Hegu–Sanyinjiao Matched Points and Hegu, Zusanli single point. J Clin Nurs. 2010;19:998–1007. doi: 10.1111/j.1365-2702.2009.02872.x. [DOI] [PubMed] [Google Scholar]
- 15.Wu LL, Su CH, Liu CF. Effects of noninvasive electro acupuncture at Hegu (LI4) and Sanyinjiao (SP6) acupoints on dysmenorrhea: A randomized controlled trial. J Altern Complement Med. 2012;18:137–42. doi: 10.1089/acm.2010.0506. [DOI] [PubMed] [Google Scholar]
- 16.Ysmael FT, Bejoc JA, Elizon LG, Alforque JM. Hoku cryokinetics fort he reduction of pain during the active phase of labor. Asian J Health. 2012;2:54–71. [Google Scholar]
- 17.Cho SH, Lee H, Ernst E. Acupuncture for pain relief in labour: A systematic review and meta-analysis. BJOG. 2010;117:907–20. doi: 10.1111/j.1471-0528.2010.02570.x. [DOI] [PubMed] [Google Scholar]
- 18.Chung UL, Hung LC, Kuo SC, Huang CL. Effects of LI4 and BL67 acupressure on labor pain and uterine contractions ın the first stage of labor. J Nurs Res. 2003;11:251–60. doi: 10.1097/01.jnr.0000347644.35251.c1. [DOI] [PubMed] [Google Scholar]
- 19.Mucuk S, Baser M, Ozkan T. Effects of noninvasive electroacupuncture on labor pain, Adrenocorticotropic Hormone, and Cortisol. Altern Ther Health Med. 2013;19:26–30. [PubMed] [Google Scholar]
- 20.Cline ME, Herman J, Shaw ER, Morton RD. Standardization of the visual analogue scale. Nurs Res. 1992;4:378–80. [PubMed] [Google Scholar]
- 21.Watson JW. Sudbury, Massachusetts: Jones and Bartlett Publishers; 2003. Pain As A Symptom Outcome, Edit: Doran D. Nursing-Sensitive Outcomes State of The Science; pp. 177–209. [Google Scholar]
- 22.Kuguoglu SY, Aslan FE, Olgun N. Turkish adaptation of the McGill Melzack Pain Questionnaire (MPQ) Ağrı [Pain] 2003;15:47–51. [Google Scholar]
- 23.Mann E, Carr E. Oxford, UK: Blackwell; 2006. Pain management; pp. 1–21. [Google Scholar]
- 24.Melzack R. The McGill pain questionnaire. Anesthesiology. 2005;103:199–202. doi: 10.1097/00000542-200507000-00028. [DOI] [PubMed] [Google Scholar]
- 25.Aksakoglu G. Izmir: 2006. Sağlıkta Araştırma ve Çözümleme [Health Research and Analysis] pp. 215–58. Second Edit. [Google Scholar]
- 26.Egri G, Gölbası Z. Traditional postnatal ınfant-care practices of 15-49 years old married women. TAF Prev Med Bull. 2007;6:313–20. [Google Scholar]
- 27.Cakırer N, Calıskan ZI. Traditional beliefs and applications about pregnancy, birth and puerperium in Agilli Village of Nevsehir. TAF Prev Med Bull. 2010;9:343–8. [Google Scholar]
- 28.Bölükbası N, Erbil N, Altunbas H, Arslan Z. Traditional practices about child care of the mothers who owner 0-12 month baby. Int J Hum Sci. 2009;6:164–76. [Google Scholar]
- 29.Beydag KD. Adaptation to motherhood in the postpartum period and the nurse's role. TAF Prev Med Bull. 2007;6:479–84. [Google Scholar]
- 30.Pinar G, Dogan N, Algıer L, Kaya K, Cakmak F. Factors that affecting mothers’ postnatal comfort. Dicle Med J. 2009;36:184–90. [Google Scholar]
- 31.Gozum S, Kilic D. Health problems related to early discharge of Turkish women. Midwifery. 2005;21:371–8. doi: 10.1016/j.midw.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 32.Declercq ER, Cunningham DK, Johnson C, Sakala C. Mothers’ reports of postpartum pain associated with vaginal and cesarean deliveries: Results of a national survey. Birth. 2008;35:16–24. doi: 10.1111/j.1523-536X.2007.00207.x. [DOI] [PubMed] [Google Scholar]
- 33.Schytt E, Lindmark G, Waldenstrom U. Physical symptoms after childbirth: Prevalence and associations with self-rated health. BJOG. 2005;112:210–7. doi: 10.1111/j.1471-0528.2004.00319.x. [DOI] [PubMed] [Google Scholar]
- 34.Niven CA, Murphy-Black T. Memory for labor pain: A Review of the literature. Birth. 2000;27:244–53. doi: 10.1046/j.1523-536x.2000.00244.x. [DOI] [PubMed] [Google Scholar]
- 35.Stewart D. Psychiatric symptoms following attempted natural childbirth. Can Med Assoc J. 1982;127:713–6. [PMC free article] [PubMed] [Google Scholar]
- 36.Kaviani M, Ashoori M, Azima S, Rajaei Fard A, Hadian Fard MJ. Comparing the effect of two methods of acupressure and ice massage on the pain, anxiety levels and labor length in the point LI-4. J Shahid Sadoughi Univ Med Sci. 2012;20:220–8. [Google Scholar]
- 37.Brown ST, Champbell D, Kurts A. Characteristics of labor pain at two stages of cervical dilation. Pain. 1989;38:289–95. doi: 10.1016/0304-3959(89)90215-7. [DOI] [PubMed] [Google Scholar]
- 38.Callister LC, Khalaf I, Semenic S, Kartchner R, Julkunene KV. The pain of childbirth: Perception of culturally diverse women. Pain Manage Nurs. 2003;4:145–54. doi: 10.1016/s1524-9042(03)00028-6. [DOI] [PubMed] [Google Scholar]
- 39.Lim CED, Wilkinson JM, Wong WSF, Cheng NCL. Effect of acupuncture on induction of labor. J Altern Complement Med The Journal of Alternative and Complementary Medicine. 2009;15(11):1209–214. doi: 10.1089/acm.2009.0100. [DOI] [PubMed] [Google Scholar]
- 40.Hajiamini Z, Masoud SN, Ebadi A, Mahboubh A, Matin AA. Comparing the effects of ice massage and acupressure on labor pain reduction. Complement Ther Clin Pract. 2012;18:169–72. doi: 10.1016/j.ctcp.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 41.Eisenach JC, Pan PH, Smiley R, Lavand’homme P, Landau R, Houle TT. Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain. 2008;140:87–94. doi: 10.1016/j.pain.2008.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]


