Abstract
Background:
Presently, using complementary therapy such as lavender oil has specific application in medicine. The purpose of this study was to investigate the effect of aromatherapy massage on the severity of primary dysmenorrhea in nursing and midwifery students of Islamic Azad University of Arsanjan, Iran.
Materials and Methods:
This study was performed using clinical trial method on 80 eligible students whose level of pain was measured by visual analogue scale (VAS) before the intervention. Each participant, in the first days of menstruation, randomly received two types of massage with lavender and placebo oil in two consecutive cycles of menstruation. Their level of pain was measured before and 30 min after the intervention. In this study, each group was considered as their self-control group in the next cycle. The data were analyzed by SPSS software.
Results:
A significant decrease in VAS score after lavender massage was detected in comparison with placebo massage. There was a statistically significant difference between VAS scores after and before placebo massage. In addition, statistically the effect of lavender massage on the severity of primary dysmenorrhea was higher than that of placebo massage (P < 0.001).
Conclusions:
Findings of this study showed that lavender oil massage decreases primary dysmenorrhea and it can be used as an effective herbal drug.
Keywords: Aromatherapy, dysmenorrhea, Iran, lavender oil, nursing
INTRODUCTION
One of the most common medical problems in gynecology is dysmenorrhea.[1] It is associated with menstrual pain and cramping centralized in the lower abdomen.[2] Dysmenorrhea is the most common periodical pain, and based on anatomic pathological conditions, it is divided into two types of primary and secondary.[1,3] These conditions come into existence at the time of first menstruation or shortly thereafter, last for 48-72 h, and are associated with cramps, nausea, vomiting, fatigue, loss of appetite, diarrhea, and headaches.[3,4] The second type is associated with painful menstruation caused by pathological problems in the pelvic region.[2,5]
In a longitudinal study conducted in the USA on 17-19-year-old students, 13% reported that they experience sever pain in more than half of their menstrual cycles, and in 42% of cases, at least one painful menstruation interfering with their activity had been reported. In another study on the prevalence of dysmenorrhea, 45% of the women studied were suffering from moderate to severe dysmenorrhea.[2] A survey in Iran reported a 71% incidence of primary dysmenorrhea and that 15% of students were absent from school 1-7 days per school year due to this problem.[6] In this regard, in the USA, the working hours lost due to dysmenorrhea is estimated at 600 million hours per year, equal to $2 billion per year.[7] Today, most women, in order to avoid multiple pregnancies, experience more menstruation; therefore, dysmenorrhea is more common than it had been previously.[1] Given that the majority of women are active in various social scenes, if they do not receive treatment, they will experience disabilities every month for 1-3 days.
It has been established that primary dysmenorrhea occurs only in periods when ovulation takes place and prostaglandins are produced.[2,5] In women whose prostaglandin concentrations reach their highest level, most severe menstrual pain is experienced.[1,5] Therefore, the first effective treatment is contraceptive pills in order to prevent ovulation. However, due to concerns about the side effects of these pills, most mothers are reluctant to use them for their young daughters. Furthermore, in order to inhibit ovulation, pills should be taken quite regularly throughout the course. In this case, many people suffer from the most common side effects of pills such as nausea, vomiting, breast enlargement, and spotting.[8,9] The second treatment for the alleviation of pain of primary dysmenorrhea is the use of prostaglandin inhibitor drugs. These synthetic drugs, especially in long-term prescriptions, cause ulcers, renal necrosis, and elevated concentrations of liver enzymes.[5,8,9]
Today, due to the effects of chemical drugs, the high economic cost of importing raw materials, and lack of desire of young girls to use hormonal drugs to reduce pain, use of medicinal plants is a step toward self-sufficiency and has attracted the attention of researchers.[10] One of these plants is lavender. Lavender is a plant belonging to the family of mints, and its scientific name is Lavandula.[11] It can be administered through oral use, inhalation, and massage. Overall, the essential oils that are generally extracted from a plant are hundred times more effective than the plant itself.[12] Lavender oil contains linalool, linalyl acetate, cineol, lavender, geraniol tannin, flavonoids and has antifungal, antimicrobial, antibiotic, and antidepressant effects.[11,13] The most common form of aromatherapy used by nurses is massage.[14,15] It is said that massage relieves pain by stimulating endorphins, and lavender oil, by reducing anxiety, causes more pain relief.[12,15] Lavender oil increases adrenocorticotropic hormone that stimulates menstrual blood flow and decreases toxicity and allergies. Aromatherapy massage is used extensively in complementary therapies in nursing.[16,17] This study examined the impact of aromatherapy massage with lavender oil on the severity of primary dysmenorrhea.
MATERIALS AND METHODS
Ethical considerations
The research and ethics committee of Azad University of Arsanjan branch, reviewed and approved this study in the aspect of methodology and ethics consideration.
This study was a clinical trial. The study population consisted of 200 nursing and midwifery students aged 18-24 years, who lived in Islamic Azad University of Arsanjan's dormity, Iran. The reason for choosing this population was the relative similarity of subjects regarding place of residency, diet, physical activity, knowledge of anatomy, physiology, pharmacology, greater sensitivity to health issues, and their cooperation in scientific papers. In this population, 100 were suffering from menstrual pain, and all of them were given questionnaires and consent forms to complete before the intervention. Of these subjects, 80 patients with primary dysmenorrhea and a visual analogue scale (VAS) score above 6 on the first day of menstruation participated in the study. Therefore, convenient sampling was performed. The questionnaire contained questions about demographic status, height, weight, menstrual history, age at menarche, medications, exercise, special diet, disease of the reproductive system, and the severity of pain. On the first day of the menstrual cycle, the severity of pain was measured using VAS with a 10-point ruler. No feeling of pain was given a score of 0, average feeling of pain was scored 6 and above, and maximum pain was given 10 points.
The essence of blooming branches of lavender plant of the officinalis type is extracted by a Clevenger apparatus in Shiraz Department of Agriculture, Iran. Its active ingredients, including linalyl acetate, linalool, cineol, tujin, and lavandulyl acetate, are analyzed by gas chromatography–mass spectrometry (GC–MS) and confirmed. Moreover, since pure essential oils are volatile and can cause irritation and inflammation of the skin, for topical use, they should be diluted with inert oil.[17,18,19] For this purpose, every two drops of lavender essential oil was mixed with 5 ml of sweet almond oil and a 2% concentration of the oil was prepared.[18,19] To avoid oxidation, the oils were stored in a dark container with lid.[12] Although the results of other researches did not report sensitivity to lavender essence, sensitivity testing of the samples was performed for more caution.[14] For this purpose, two drops of lavender oil were placed on the elbows and after 15 min, the sensitivity was controlled.
Since all the interventions could not be performed by one person, five nursing and midwifery students who did not participate in the research and lived in the dormitory were used as research assistants. In order to minimize the risk of errors and create coordination between the assistants, they were trained on the methods to complete questionnaires, measure pain intensity by VAS, and to massage. Then, the performance of the research assistants was observed, and its reliability was confirmed. Each subject underwent intervention during three periods of menstruation. During the first cycle, the severity of menstrual pain without the intervention was measured by the 10-point VAS. In the second cycle, patients were randomly divided into two groups, and for the first group, code 1 medication (lavender oil) and for group 2, code 2 medication (placebo) were used for massage. In the third cycle, in contrast to the first cycle, group 1 received code 2 medication and group 2 received code 1 medication. In this study, each group was used as its own control group for the next month. The subjects were divided into two groups in order to measure the influence of time. In the second and third cycles, before and after using placebo or lavender oil, the subjects’ severity of pain and intensity were measured using the VAS. Thus, five scores of VAS were obtained for each participant.
The intervention was performed in the following manner. In the second and third cycles, at the onset of pain coinciding with the onset of menstruation, the subjects were invited after a phone call to a room at 23-25°C temperature, with low light intensity, and with beds and chairs prepared in the dormitory. First, severity of pain was measured and then subjects lay on their backs. A small pillow was placed under their knees. Then, the researcher would wash, dry, and warm the hands, spill 2 ml of lavender oil or placebo on them, and would massage with rotation movements using both hands without creating pressure on the abdomen for 15 min.[19] The upper part of the pubic bone and the part around the navel were massaged. The hands were opened and used to cover the abdomen. Then, the researcher cleaned the area with a tissue and after 30 min, the pain was measured and recorded. Data were analyzed using descriptive statistics and paired t-test by SPSS for Windows (version 16; SPSS Inc., Chicago, IL, USA). In this study, an alpha level of 0.05 or less indicated the significance of the results.
RESULTS
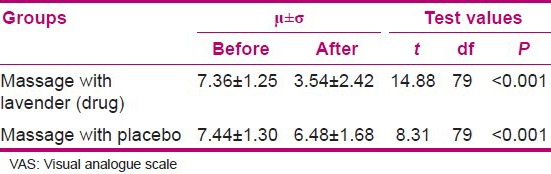
A total of 80 nursing and midwifery students of 18–24 years of age with primary dysmenorrhea participated in this study. The mean age of participants was 20.4 ± 1.33 years, the average age of menarche was 13.5 ± 1.07 years, and the mean pre-intervention pain intensity was 7.44 ± 1.35. No sensitivity was observed among the participants. The severity of pain on the first day of menstruation before the intervention showed no statistically significant difference during the three consecutive months. Nonetheless, the pain before and after lavender oil massage (t = 14.88, P < 0.001) and placebo massage (t = 8.31, P < 0.001) had statistically significant differences [Table 1].
Table 1.
Comparison of dysmenorrhea before and after massage with lavender oil and placebo based on the VAS
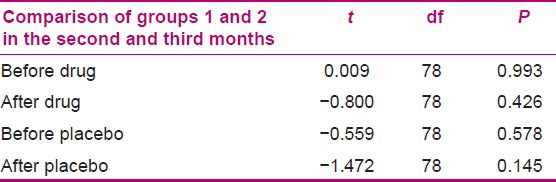
Minimum and maximum severity of pain after massage with lavender oil and placebo, respectively, were 0-9 and 2–10. There was a significant difference between lavender oil and placebo in terms of pain reduction (t = 11.31, P < 0.001) [Table 2]. The difference in the mean pain intensity before and after taking the drug and placebo, determined using paired t-test, was significantly different (P < 0.001). This proved the higher effectiveness of the drug compared to the placebo [Table 3]. In addition to the results obtained by comparing pain scores in groups 1 and 2 in the second and third cycles, it was found that in all conditions, there was no significant difference between groups 1 and 2 [Table 4]. Therefore, it was showed that time did not affect drug or placebo.
Table 2.
Comparison of dysmenorrhea after intervention based on VAS
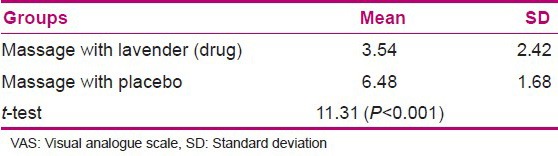
Table 3.
The mean difference in pain intensity before and after using drug and placebo
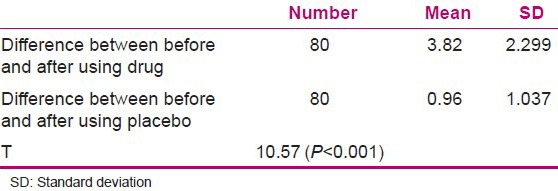
Table 4.
Comparison of the mean pain score in groups 1 and 2 in the second and third cycles
DISCUSSION
In the present study, the effects of aromatherapy massage in nursing and midwifery students suffering from dysmenorrhea and living in the dormitory of Islamic Azad University of Arsanjan were studied. According to the findings, mean severity of dysmenorrhea among the subjects before the intervention was 7.44 ± 1.35. Han et al. in their study, found the severity of dysmenorrhea to be 7.8 ± 1.37, and Iravani estimated this mean as 7.8 ± 1.6 with 10-point VAS.[6,17] These results are almost consistent with the present study. However, several variations in the severity of dysmenorrhea have been observed in different studies. Serap et al. estimated the mean severity as 82.38 ± 10.86 with a 100-point VAS and Ozerdogan et al. estimated it as 6.56 ± 1.81 using a 10-point VAS.[16,20] One reason for this variation in results is the difference in understanding and tolerance of pain due to cultural, social, and lifestyle factors.[20,21] The study by Valiani et al. on the effect of massage therapy on dysmenorrhea due to endometriosis found that before the intervention, 3.52% of the subjects reported severe pain using VAS.[22] Furthermore, according to the findings, after massage with placebo, a decrease in the severity of dysmenorrhea was observed. Valiani et al. achieved a reduction in the severity of dysmenorrhea due to endometriosis immediately and after 6 weeks of massage.[22] Serap et al. also achieved a reduction in the severity of dysmenorrhea after massage with placebo.[16] These results are consistent with the results of this study and can be attributed to the nature of the massage. Bahrainy et al. believe that massage therapy results in pain relief by stimulating endorphins.[12] Massage relaxes and reduces tension in the muscles.[16] Novak and Berek wrote in this regard that primary dysmenorrhea has a colic nature and heals via abdominal massage.[1] Also, slow massage without pressure on the perineal area can increase the elasticity of the perineum and increase the blood flow.[23]
From other findings of this study it can be concluded that although placebo massage can reduce the severity of dysmenorrhea, the amount of reduction of the severity of dysmenorrhea achieved by massaging with combined essential oils is significantly greater than that achieved with placebo massage alone. In this regard, Atashzadeh Shurideh et al. in a study on 80 patients with multiple sclerosis (MS), concluded that although sweet almond oil massage is effective, the effect of massage with pepper essence is greater than that of massage alone.[24] During topical application of lavender oil, the muscles relax and blood supply to the tissue and the elasticity increase.[23] Han et al. also observed a reduction of severe menstrual cramps and pain after massage with lavender essential oil.[17] In relation to using aromatherapy with massage, Yip and Tse reported the mean intensity of pain in neck in the group receiving eight sessions of acupressure combined with lavender essential oil to be 4.91 ± 1.87 and in the group with acupressure without aromatherapy to be 5.12 ± 2.18.[25] However, Vakilian et al. in their study, did not find a significant difference between the severity of pain 5 days after episiotomy in the group using essential oils and the group using Betadine.[26] This difference can be explained in terms of the method of using essential oils; in the study by Vakilian et al. the essence was used as sitting bathing.
There is evidence that the oils, after topical or inhalation use, are absorbed into the bloodstream. In addition, the concentration of their active ingredients will remain on the skin approximately 90 min after rubbing.
However, the amount of oil entering the bloodstream is low.[19] In this relation, Jager et al. believed that linalool and linalyl acetate in the essential oils are absorbed through the skin. Approximately 19 min after application, they reach their peak in plasma and by directly affecting the central nervous system provide relaxation.[27] In the present study, the lasting effect of lavender essential oil was also less than 1 month. Bahrainy believes that the effect of essential oils is short-lasting and the disposal is quick, and it seems unlikely that they accumulate in body tissues.[12]
However, there are differences in the field of massage sustainability. Beckman and Garret studied the effects of perinea massage from 34 weeks gestation until the onset of labor on reducing the incidence of perinea laceration in Australia. They concluded that the reduction of perinea pain persisted even up to 3 months after delivery.[28] In this regard, Valiani et al. applied massage techniques and pressure on 24 parts of the abdomen and 10 parts of sacral region, each for 2 min. They concluded that reduction of pain 6 weeks after massage was less than its effect immediately after its application.[22] In the present study, a month after giving massage with placebo, there was no change in pain intensity. Moreover, it can be stated that the effect of massage did not last up to 1 month in this study. Differences in the lasting effects of massage in this study compared with the research of Valiani et al. can be due to the differences in the massage techniques applied. They used the technique of acupressure and deep pressure to certain points on the abdomen and back, while in the present study surface and gentle massage was performed without pressure.[22]
Massage with lavender oil was used in this study. Choi did not observe any significant differences between massage and inhalation of lavender essential oil in the reduction of dysmenorrhea in his study.[29] However, aroma therapists prefer massage to inhalation.[21] On the other hand, Wong et al. performed an extensive study on 1092 female high school students in Malaysia, and during the survey, 60% of patients with dysmenorrhea stated that they preferred the kind of drugs which were used for massage.[30] A study supported the importance of lavender essential oil and its effectiveness without massage. In this respect, Jahdi et al. used sitting bathing method after delivery in their study and found a significant difference between the control group who used Betadine and the experimental group.[14] Mojab believed that the combined use of essential oils increases efficiency.[19] However, in a research by Han et al. a combination of lavender, sage, and rose essences was used a week prior to menstruation until the first day; they obtained results similar to that of the present study.[17]
CONCLUSION
It can be concluded that lavender oil, compared to other essential oils used in the study by Han et al. has a more important role in reduction of pain severity. The results of this study in nursing and midwifery students can be used for people who suffer from dysmenorrhea.
Limitations of the study
Since this study was conducted on nursing and midwifery students living in dormitories of Islamic Azad University of Arsanjan, the results cannot be generalized to the wider community. Further research on other groups of women is necessary.
ACKNOWLEDGMENT
The authors would like to express their thanks to the research vice-chancellor of the Islamic Azad University, Arsanjan Branch, for the financial support, the Department of Agriculture staff, staff of pharmacy college library.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Berek JS, Novak E. Trans Davaritanha F. 15th ed. Tehran: Artinteb; 2012. Berek and Novak's Gynecology; pp. 530–4. [Google Scholar]
- 2.Spiroff L, Fritz MA. Trans valadan M. 8th ed. Tehran, Iran: Ketabarjmand; 2011. Clinical Gynecologic Endocrinology and Infertility; pp. 631–4. [Google Scholar]
- 3.Brunner LS, Sudarth DS, O’conell Smeltzer SC. Trans Sami P. 10th ed. Philadelphia: Lippincott Wilkins; 2004. Brunner and Sudarth's textbook of medical surgical of nursing; pp. 50–1. [Google Scholar]
- 4.Jun EM, Change S, Kang DH, Kim S. effects of acupressure on dysmenorrhoeal and skin temperature change in college students: Randomized controlled trial. Int J Nurs Stud. 2007;44:973–81. doi: 10.1016/j.ijnurstu.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 5.Black G, Hux J. Medical surgical of nursing. In: Tran Atashzadeh F, Blurchi F., editors. 1st ed. Tehran, Iran: Jamenegar; 2005. pp. 684–5. [Google Scholar]
- 6.Iravani M. Effects of Thymus vulgaris estract on primary dysmenorrhea. J Med Plants. 2008;8:54–5. [Google Scholar]
- 7.Andrea J, Rapkin RC, Gambone JC. Essential of Obstetrics and Gynecology. 4th ed. Edinburgh: Chirchil; 2004. Dysmenorrhea and chronic pelvic pain; p. 287. [Google Scholar]
- 8.Heshmati P, Asadinughabi A. 3rd ed. Tehran, Iran: Raphi Co; 2006. Generic Medicines; p. 296. [Google Scholar]
- 9.Rasuli M, Teimuri F. 2nd ed. Tehran: Andishe Raphi Co; 2010. Iran Generic Drugs With Nursing Care; p. 884. [Google Scholar]
- 10.Mohammad S. 15th ed. Tehran, Iran: Ataei Co; 2005. Tebolmophid; p. 6. [Google Scholar]
- 11.Jaefarnia S, Khosrowshahi S, Ghasemi M. 6th ed. Tehran: Iran: Sokhan Gostar; 2011. Medicinal plants. [Google Scholar]
- 12.Bahrainy S, Nagi A, Manani R. Aromatherapy and it s application. J Urmia Nurs Midwifery Fac. 2011;9:1–8. [Google Scholar]
- 13.Rajinder SH, Tarun G. 1st ed. Nepal: Campus Books International; 2009. Encyclopedia of medicinal plants; pp. 1210–3. [Google Scholar]
- 14.Jahdi F, Sheikhan F, Merghati E, Haghani H. Effect of lavender essential on preneal pain after episiotomy. J Sabzevar Univ Med Sci. 2009;16:127–30. [Google Scholar]
- 15.Maddocks-Jenings W, Wilkinson JM. Aromatherapy practice in nursing Literature review. J Adv Nurs. 2004;48:93–103. doi: 10.1111/j.1365-2648.2004.03172.x. [DOI] [PubMed] [Google Scholar]
- 16.Serap E, Sevban A, Reva B, Ayda C. Effect of aromatherapy massage on dysmenorrheal In Turkish students. Pain Manag Nurs. 2010;13:236–40. doi: 10.1016/j.pmn.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Han SH, Hur MH, Buckle J, Choi J, Lee MS. Effect of aromatherapy on symptoms of dysmenorrhea in college students. J Altern Complem Med. 2006;12:535–41. doi: 10.1089/acm.2006.12.535. [DOI] [PubMed] [Google Scholar]
- 18.Salehisurmaghy M. 2nd ed. Tehran, Iran: Nutrition World Co; 2008. Phytotherapy and medicinal Plants; p. 62. 31,39,46. [Google Scholar]
- 19.Mojab F. Razi J Med Sci. Vol. 4. Shahid beheshti medicine university; 2002. Aromaterapy; pp. 277–84. [Google Scholar]
- 20.Ozerdogan N, Sayiner D, Ayranci U, Unsal A, Giray S. Prevalence and predictors of dysmenorrhea among students at a university in Turkey. Int J Gynecol Obstet. 2009;107:39–43. doi: 10.1016/j.ijgo.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 21.Khodakrami N, Moatar F, Ghahiri A. The effect of an Iranian herbal drug on primary dysmenorrhea: A clinical controlled trial. J Midwifery Womens Health. 2009;54:401–4. doi: 10.1016/j.jmwh.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 22.Valiani M, Ghasemi N, Bahadoran P, Heshmat R. The effect of massage therapy on dysmenorrhea caused by endometriosis. Iran J Nurs Midwifery Res. 2010;15:167–71. [PMC free article] [PubMed] [Google Scholar]
- 23.Atarha M, Vakilian K, Ruzbehani N, Bekhradi R. Effect of preneal massage with lavender essential on episiotomy and preneal rapture. J Arak Univ Med Sci. 2009;11:26–8. [Google Scholar]
- 24.Atashzadeh Shurideh F, Mohammadi S, Abedsaeidi ZH, Alavi Majd H, Salehi H. A comparison of aromatherapy and massage on pain severity in women with multiple sclerosis. J Nurs Midwifery Shahid Beheshti Univ Med Sci. 2008;16:28–32. [Google Scholar]
- 25.Yip YB, Tse SH. An experimental study on the effectiveness of acupressure with aromatic lavender essential oil for sub-acute, non-spesific neck pain in Hong Kong. Complement Ther Clin Pract. 2006;12:18–26. doi: 10.1016/j.ctcp.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 26.Vakilian K, Atarha M, Bekhradi R, Fabel F, Hemati Z, Seraj A. Effect of lavende essential on episiotomy wound care post partum. J. SKUMS. 2008:63–9. [Google Scholar]
- 27.Jager W, Buchbauer G, Jirovertz L, Fritzer M. Percutaneous absorption of lavender oil from a massage oil. J Soc Cosmet Chem. 1992;43:49–54. [Google Scholar]
- 28.Beckman MM, Garret AJ. Antenatal massages for reducing perineal trauma. Cochrane Database Syst Rev. 2006;25:CDoo5123. doi: 10.1002/14651858.CD005123.pub2. [DOI] [PubMed] [Google Scholar]
- 29.Choi EH. Comparison of effect lavender abdominal massage and inhalation on dysmenorrhea, pain, anexiety and depression. J Korean Acad Fundam Nurs. 2009;16:300–6. [Google Scholar]
- 30.Wong l, Ming Khoo E. Dysmenorrhea in a multiethnic population of adolescent Asian girls. Int J Gynaecol Obstet. 2010;108:139–42. doi: 10.1016/j.ijgo.2009.09.018. [DOI] [PubMed] [Google Scholar]


