Abstract
Background:
The aim of this study was to compare the effects of the second- and third-generation oral contraceptives on women's reproductive sexual function.
Materials and Methods:
This randomized, double-blind, placebo-controlled clinical trial was conducted on 82 married women of reproductive age in Tehran. Samples were randomized into the groups receiving second- and third-generation oral contraceptive pills. Female Sexual Function Index (FSFI) tool was used before the intervention and 2 and 4 months after the intervention. Data analysis was carried out using analysis of variance (ANOVA) within repeated measures and P < 0.05 were considered significant.
Results:
There was a statistically significant difference in the positive and negative moods between the experimental and control groups before the intervention in the second and fourth months. The second-generation pills caused a decrease in sexual function in the second month and an increase in sexual function in the fourth month, but the third-generation pills led to an increase in sexual function in the second and fourth months. The increase in sexual function that resulted from using the third-generation pills was significantly higher than that resulted on using the second-generation pills.
Conclusions:
According to the results of this study, sexual functioning decreased in the second month of using the second-generation pills and sexual performance was significantly more on using the third-generation pills compared to second-generation pills. The most common type of oral contraceptive used in Iran is the second-generation oral contraceptive LD™ (low-dose estrogen), which is freely distributed in health centers. Therefore, it is necessary for women who wish to use these contraceptive methods to be educated and consulted before they start using them. The third-generation contraceptive pills can be recommended to women who wish to use oral contraceptives.
Keywords: Second-generation combined oral contraceptives, sexual function, third-generation combine oral contraceptives
INTRODUCTION
Sexual desires are an important part of human life and are a fundamental part of people's quality of life (QoL) and emotional health.[1] In 2002, the World Health Organization (WHO) provided an empirical definition for sexual health, in which it is explained as a state of physical, emotional, mental, and social well-being related to sexual desires, and is not achieved only with lack of illness, dysfunction, or disability. Despite this guideline, there is still a big challenge to define natural and true sexual functioning (sexual health), especially of women.[2]
In a national survey conducted in Iran in 2005, 31.5% of women had sexual dysfunction.[3] Sexual dysfunction due to any reason has many negative outcomes. Researches indicated that sexual problems are associated with social problems such as crime, sexual abuse, mental illness, and divorce, while satisfactory sexual performance is a factor for strengthening family ties and a basic for obtaining and consolidating a culture.[4] Sexual dysfunction is listed as one of the most common reasons for withdrawal of oral contraceptives.[5,6,7,8]
Birth control pills are a class of drugs which have been widely studied since 1960, and are used by more than 70 million women daily.[9] In a national research conducted in the US on the contraceptive methods, it was concluded that the oral contraceptives had the highest rate of use, and using oral contraceptives was the first-grade selected method in 15-44-year-old women (18.9%).[10] In the present circumstances of Iran, oral contraceptives are one of the most practical and effective methods of preventing pregnancy, which is chosen by many couples.[11] The oral contraceptive pills are a combination of two components which are estrogen and progestin, and they are divided into three generations based on the type of progesterone they contain. The first-generation progestin includes norethindrone, lynestrenol, ethynodiol diacetate, and norethisterone. The second generation includes levonorgestrel and norgestrel. The third generation includes desogestrel, gestodene, and norgestodene. Due to their causality with breast cancer, first-generation progestins are not used and have more side effects than the second- and third-generation ones.[12] In general, the estrogen part of pill increases the production of sex hormone-binding globulin and also reduces the amount of androgens in the blood circulation. The progestin in oral contraceptives decreases the amount of free testosterone and limits the conversion of testosterone to its active metabolite by inhibiting 5α-reductase which is dihydrotestosterone.[13] The third-generation progestin has less androgenic properties than the second-generation.[9,10] Desogestrel has no intrinsic androgenic properties. Combined oral contraceptives that have desogestrel increase the sex hormone-binding globulin capacity to androgens and this leads to a significant decrease in free testosterone and free 5α-dihydrotestosterone.[9] Androgens play a significant role in sexual desire in both genders, and a reduction in testosterone level has been reported as the major cause of low sexual desire in women. There is also evidence of the role of testosterone in sexual desire.[14] Despite this, there is conflicting evidence about the effects of testosterone on sexual desire.[15] In a study on 1021 18-75-year-old women in the United States, there was no association reported between the sexual problems and decreased total and free testosterone and androstenedione.[16] In Graham et al.'s study on the effects of oral contraceptives on androgen levels and their effects on sexual desire, there was no association between the oral contraceptives and reduced total and free testosterone and dehydroepiandrosterone-sulfate (DHEA-S) levels and decreased sexual desire.[17] In contrast, testosterone therapy in women with sexual dysfunction resulted in increased sexual satisfaction.[18]
Effects of oral contraceptives on sexual desire have not been fully recognized. Also, conflicting reports exist on the effects of oral contraceptives on sexual desire, and some women reported improved sexual desire, some stated decrease, and most of them reported no change at all.[17,18,19] Caruso et al., in their study on women using third-generation contraceptives, reported decreased sexual desire within 3, 6, and 12 months, decreased sexual frequency during 9 months, decreased arousal during 3 months, and declined orgasm during 3-9 months.[20] In addition, the study of Battaglia et al. concluded that the third-generation contraceptive pills decrease libido.[21] In contrast, the study of Gricu et al. reported that the third-generation oral contraceptives increase sexual desire.[22] Malekian et al. studied the effects of second-generation contraceptives on sexual functioning and observed improved sexual functioning within 4 months of use.[23] Due to the importance of sexual functioning on the individual and family health, the WHO recommended comparison of various contraceptives methods based on progesterone type on sexual desire and satisfaction.[12] Second-generation pills (LD™; low-dose estrogen) are the most used oral contraceptives in Iran, and use of this method has increased from 18.4% in 2000 to 19.3% in 2005.[24] The present study aimed to investigate the effects of the second- and third-generation oral contraceptives on sexual functioning in women in reproductive ages.
MATERIALS AND METHODS
This was an interventional, randomized clinical trial conducted on 82 married women of reproductive age (15-45 years old) who referred to the Health Treatment Center in the eastern region of Tehran, Iran in 2011 to choose the oral contraceptive method and met the inclusive criteria. In this center, health services such as family planning, maternal and child health, and vaccination are provided. The reason for selecting this health treatment center in the eastern region of Tehran was the high rate of oral contraceptive methods used here. Inclusive criteria included the absence of absolute and relative contraindications for combined contraceptive pills, no history of taking medications having negative effects on sexual functioning, such as blood pressure medications or antidepressants, no history of taking sexual stimulant medications such as danazol and laduca, having a stable and satisfactory sexual relationship, no sexual dysfunction in spouse according to their self-report, lack of illness effective on sexual functioning according to the patient and the clinic physicist, lack of exposure to any critical incident during the last 3 months, and not using hormonal methods for the past year. Sample size was calculated to be 34 in each group according to the available data from Samira Maleki's dissertation[23]; and given 10% sample loss, 41 patients were allocated for each group. After obtaining permission from the Ethics Committee (code: 9087), the subjects were assigned to the groups based on block randomization with an allocation ratio of 1:1 in the two groups, wherein one received second-generation contraceptive pills (LD; low-dose estrogen) and the other received third-generation pills (Desoceptive®). Block sizes were selected as fours and sixes in order to have secretion. After listing almost all the possible states of the blocks and giving a number to each of them using a computerized table of random numbers, sequence allocation was identified. LD pills of the second-generation contraceptive method contain 0.15 mg levonorgestrel and 0.03 mg ethinyl estradiol and are produced by Aboureihan Company in Tehran, Iran, and Desoceptive pills of the third-generation contraceptive method contain 0.15 mg desogestrel and 0.03 ethinyl estradiol and are made by Iran Hormone in Tehran, Iran. The latter pills having the same features and colors as the LD pills were used. To hide the allocation, sealed envelopes of the same form and size were used, which were numbered in order from 1 to 82 and contained two types of second- and third-generation contraceptive pills. The envelopes were given to the participants. The researcher and the subjects were not aware of the allocation sequence.
To collect data, a questionnaire on the demographic and social information and reproductive history, and female sexual function index (FSFI) was used.[25] The FSFI included six major parts, i.e. sexual desire (2 items), sexual stimulation (4 items), vaginal lubrication (4 items), orgasmic experience (3 items), sexual satisfaction (3 items), and pain during sex (3 items), which made a total of 19 questions. Based on the responses of the participants to the standard questionnaire of FSFI, their sexual functioning during the last 4 weeks was reviewed. Calculation of the scores in the sexual function section according to the Iranian standard questionnaire was as follows. Each question in the sexual function section had five options: questions 1 and 2 (minimum and maximum score of 1 and 5, respectively, with a coefficient of 0.6); questions 3-10 (minimum and maximum score of 0 and 5, respectively, with a coefficient of 0.3); questions 11-13 (minimum and maximum score of 0 and 5, respectively, with a coefficient of 0.4); questions 14-16 (minimum and maximum score of 0 and 5, respectively, with a coefficient of 0.4); and questions 17-19 (minimum and maximum score of 0 and 5, respectively, with a coefficient of 0.4). Therefore, the maximum and the minimum scores were 36 and 1.2, respectively. The reliability and validity of this questionnaire was validated by Mohammadi, Heidari, and Faghihzadeh in Tehran in 2008 on 53 women, i.e. tool sensitivity 82% and specificity of 83%. Reliability coefficient had been determined to be r ≥ 0.70 for this questionnaire.
Demographic and social information and reproductive history of the participants were completed by the researcher and his/her assistant before the intervention. Subjects were asked to complete the FSFI before the intervention. After the group allocations, the researcher and the study subjects were unaware of the type of pills given to them. After giving the envelopes containing 21 pills to the participants, they were instructed on how to use the pills, which was once a day for 21 days with a 7-day interval to start the next cycle of pills. At the end of the second and fourth month of using the pills, the subjects were asked to complete the FSFI questionnaire by phone calls. The duration of the intervention was 4 months, and data collection was done in three stages (pre-intervention, and 2 and 4 months after the intervention). Data for qualitative variables were reported as frequency (percentage) and for quantitative variables as mean difference and standard deviation (SD). For reviewing normalized quantitative variables in each group, Kolmogorov–Smirnov test (KS) was used and their normality was confirmed. To compare the qualitative variables in the two groups, χ2 (Chi-square) was used with precise P value. With regard to the sexual functioning variable in the groups, independent t-test and analysis of covariance (ANCOVA) were used to compare baseline values and the values in the post-intervention phase, respectively. In this analysis, the baseline measurement of sexual functioning and confounding variables (age) were adjusted. In addition, for checking the time measurement changes in each of the two groups for the sex variable, analysis of variance (ANOVA) with repeated measures and Holm-Šidák were used. Data analysis was done through SPSS for Windows 17.0 (SPSS Inc., Chicago, IL, USA) and P < 0.05 was set as the significant level.
RESULTS
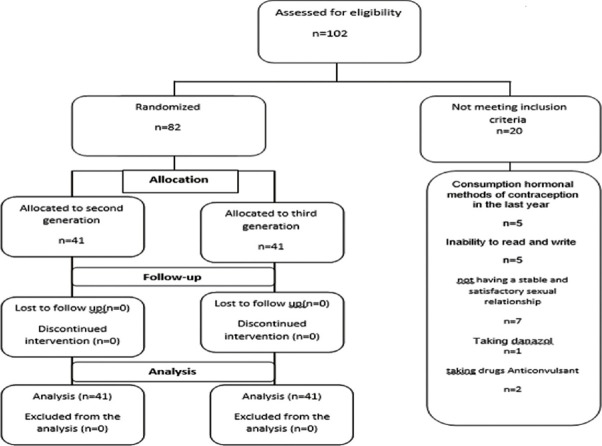
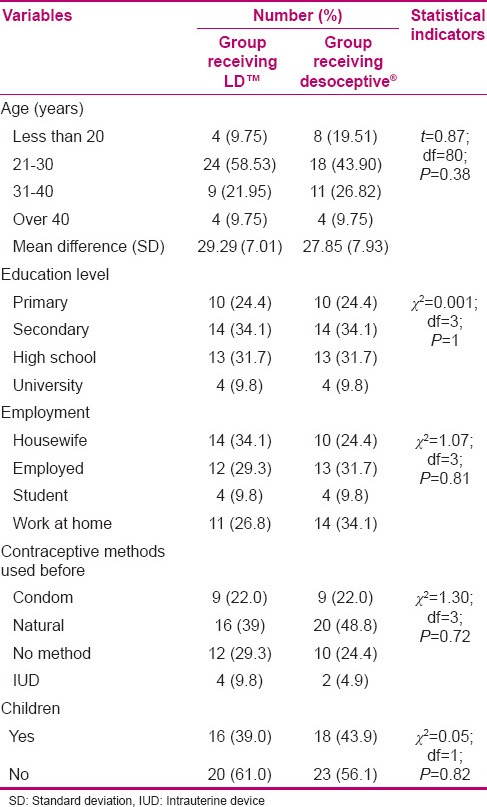
In this study, 102 women in their reproductive age who wished to participate in the study were selected. Twenty women were excluded from the study as they did not meet the inclusion criteria. Therefore, the study was conducted on 82 women in their reproductive age, in two groups of 41 each, with one group receiving second-generation oral contraceptives (LD) and the other group receiving third-generation oral contraceptives (Desoceptive). Data collection lasted for 6 months. There was no sample loss during the study and all the participants remained in the study until the end [Figure 1]. The two groups were similar in age and demographic characteristics. Mean age of the patients receiving LD was 29 years and of those receiving Desoceptive was 28 years. Majority (34.1%) of the patients in both groups were secondary school graduates. Majority of the patients in the group receiving second-generation pills were housewives (34.1%) and in the group receiving third-generation pills worked at home (34.1%). Other personal and social characteristics are shown in Table 1.
Figure 1.
Diagram of the conducted research
Table 1.
Comparison of the demographic characteristics of the two groups receiving second-and third-generation oral contraceptives
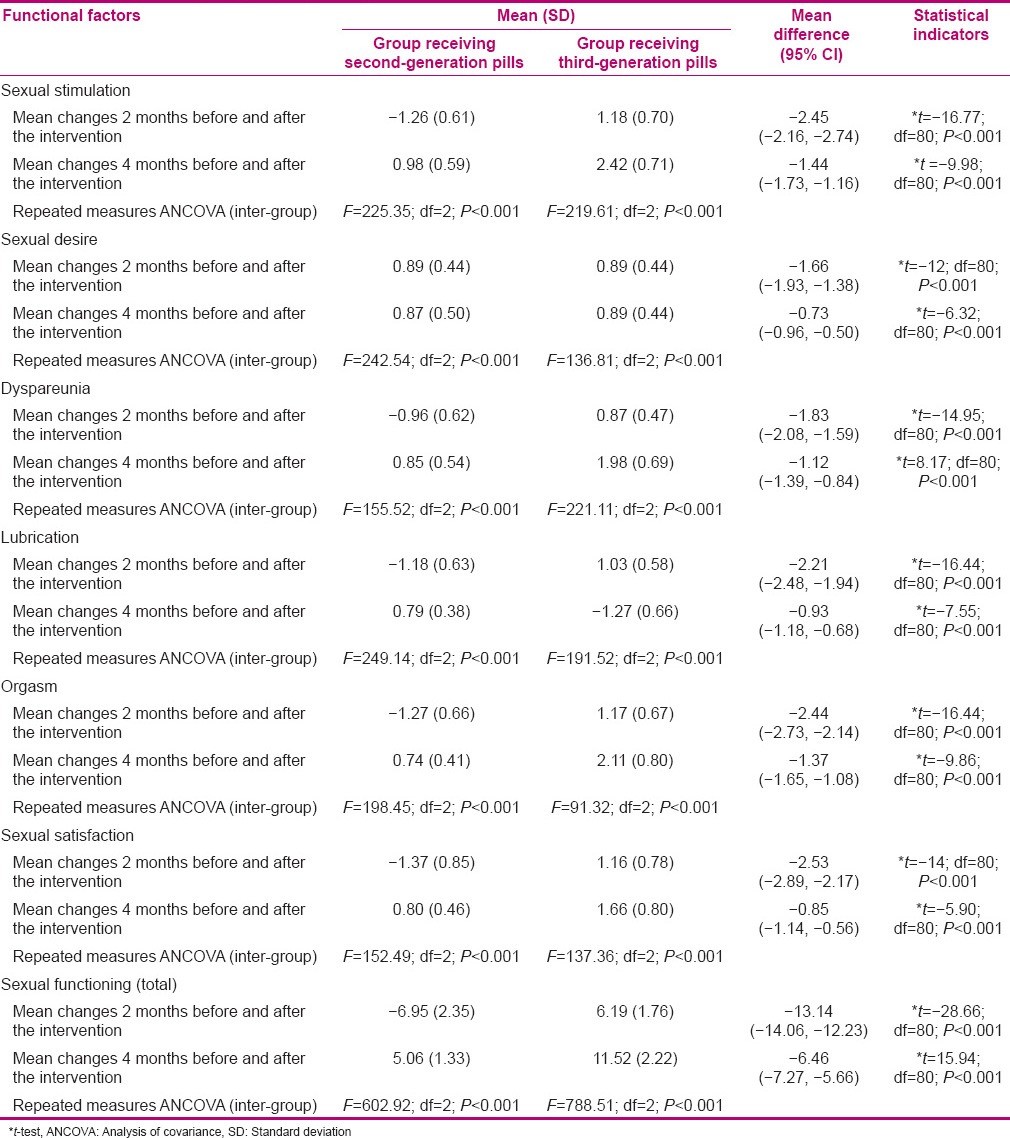
The results of the ANCOVA with adjustment for baseline values showed that in months 2 and 4, the mean score of sexual functioning and its subgroups (sexual desire, sexual stimulation, vaginal lubrication, sexual pain, orgasm, and sexual satisfaction) had a statistically significant difference between the two groups. Mean sexual functioning in the group using third-generation pills was higher compared to the group using second-generation pills in the second month, and in the fourth month, there was a significant increase in the sexual function in the group using third-generation pills compared to the group using second-generation pills [Table 2].
Table 2.
Mean sexual function and its subgroups based on follow-up of the two groups receiving second- and third-generation contraceptive pills, respectively
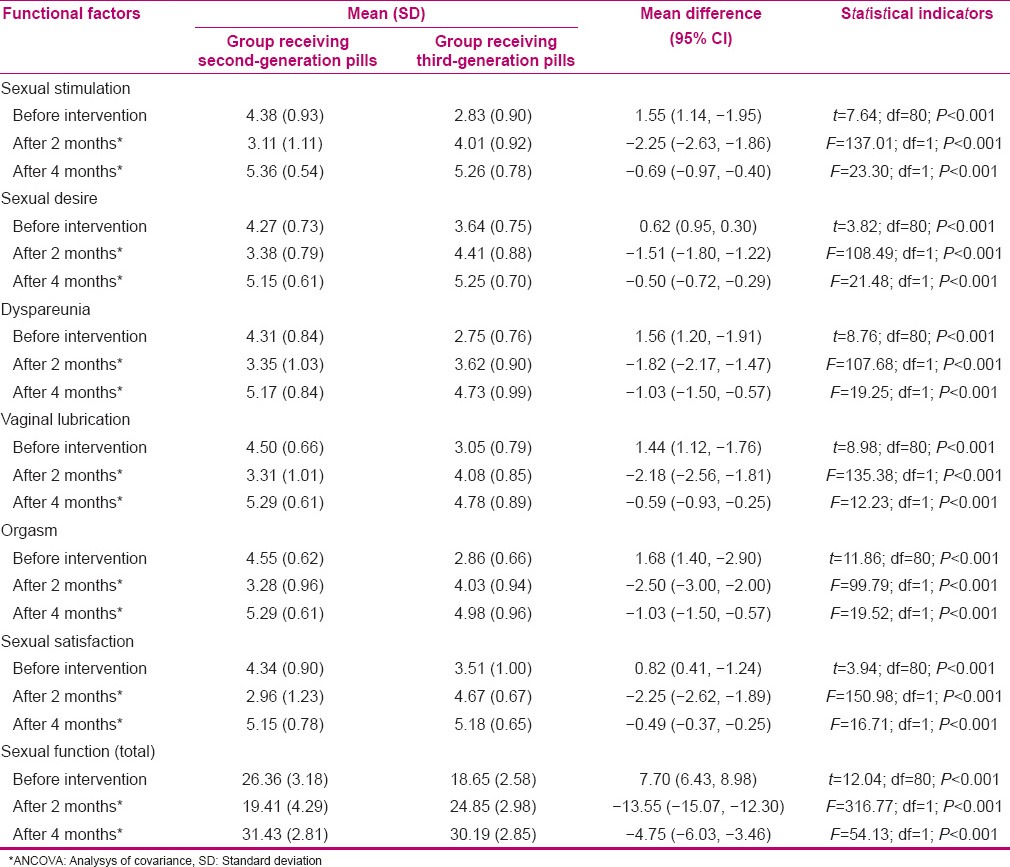
Inter-group comparison using ANOVA with repeated measures revealed that in both groups, using the second- and third-generation pills, respectively, changes in the mean values of the sexual function scores and their subgroups 2 and 4 months after the intervention were statistically significant compared to the values in pre-intervention phase (P < 0.001). The sexual functioning scores in the group using second-generation pills decreased in the second month and increased in the fourth month, and the sexual function scores in the group using third-generation pills had increased in both second and fourth months [Figure 2, Table 3].[26,27,28]
Figure 2.
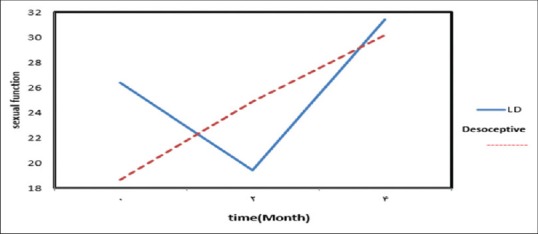
Mean sexual function in the two groups receiving second- and third-generation contraceptive pills, respectively
Table 3.
Mean changes in sexual functioning and its subgroups according to the follow-up of the two groups receiving second- and third-generation contraceptive pills, respectively
DISCUSSION
Various factors, including environmental factors, psychological, social, and contraceptive methods, may affect sexual desire.[29] For the first time in Iran, a double-blind randomized clinical trial has been performed to compare the effects of second-generation contraceptive LD and third-generation Desoceptive. The results indicated that sexual function scores and their subgroups had decreased in the second month after the intervention in the group taking second-generation contraceptive pills and had increased in the group using third-generation pills. In the fourth month after the intervention, the sexual function had increased in both groups. Mean score of sexual functioning in the second month after the intervention in the second-generation contraceptive group showed a decrease by about 26.36% compared to the pre-intervention phase. Also, in the third-generation group, it increased by about 33.24% compared to the pre-intervention phase. Sexual functioning in the fourth month after the intervention had increased by about 19.23% compared to the pre-intervention phase in the second-generation group and by about 87% compared to the pre-intervention phase in the third-generation group. This increase in sexual functioning in Month 4 was significant in the third-generation group compared to the second-generation group.
The study of Strufaldi et al. on the effects of two types of contraceptive pills of the second generation in different dosages on sexual function and the amount of testosterone on forty-nine 28-year-old women showed that their sexual function increased 6 months after using the second-generation pills;[30] this was in accordance with the present study. The study of Malekian et al. with the aim of investigating the effects of second-generation pills (LD) with condom on sexual functioning concluded that the sexual functioning increased 4 months after using the second-generation pills. This result was in accordance with the present study, since the sexual function decreased in the second month but increased in the fourth month. It seems that the continued use of second-generation oral contraceptives was effective in improving sexual functioning.[23]
Caruso et al.'s study, which aimed to investigate the effects of third-generation contraceptive pills (containing 20 μg ethinyl estradiol and 3 mg drospirenone) on sexual function in 140 women aged 18-37 years, concluded that the sexual functioning had increased 3 and 6 months after using the third-generation pills.[31] Besides, in a double-blind clinical trial by Taneepanichskul and Oranratanaphan aiming to review the effects of pills containing progestin drospirenone and gestodene (third generation) on sexual function of women aged 18–35 years, it was found that the sexual desire in women using these pills had increased.[29] Caruso studied the effects of pills containing 15 μg atynl estradiol and 60 μg gestodene on 48 women aged 18-35 years. They concluded that the sexual function in these women increased 3, 6, and 9 months after using the third-generation contraceptive pills.[20] These results are consistent with the results of the present study.
Cagiano and Sabatini conducted a study for a year on 280 women aged 30 years on the effects of two types of oral contraceptives with vaginal rings on menstrual cycle, sexual desire, and their side effects. The results showed that sexual satisfaction and desire had decreased in women using the second- and third-generation pills.[32] While in the present study, sexual satisfaction and desire had increased 4 months after the intervention in the second- and third-generation groups. Thus, there is a discrepancy with the results of the present study.
The differences in the results of the mentioned study with the present study might be due to the different dosages of estrogen and progesterone in the pills that were given to the participants. In the present study, the second-generation pills contained 15 μg levonorgestrel and 30 μg ethinyl estradiol and the third-generation pills contained 15 μg desogestrel and 30 μg ethinyl estradiol, while in that study, the second-generation pills contained 100 μg levonorgestrel and 20 μg ethinyl estradiol and the third-generation pills contained 15 μg ethinyl estradiol and 120 μg etonogestrel. In addition, in the present study, sexual function and all its subgroups (sexual stimulation, sexual desire, sexual satisfaction, orgasm, dyspareunia, and vaginal lubrication) were compared to the pre-intervention phase, while in the other study, satisfaction and sexual desire were studied prospectively, without comparing them to the pre-intervention phase. And given that sexual behavior is influenced by interpersonal relations, life situations, and culture,[33] another reason for discrepancies observed in the present study and the mentioned study could be the differences in the demographic characteristics of the studied population, their attitude and cultural differences.
Battaglia et al. studied the effects of the third-generation contraceptive pills (30 μg ethinyl estradiol and 3 μg dexasporin) on sexual functioning of 22 women aged 18-35 years during 3 months. They found that sexual desire had decreased after 3 months of using these pills compared to the pre-intervention phase.[21] The results of the above-mentioned study were inconsistent with those of the present study. This difference might be due to the difference in the progesterone dosage of the pills used in both studies. In the present study, 0.15 mg desogestrel was used, whereas in the above-mentioned study, 3 mg dexasporin were used. Other differences might include the difference in the sample size (in the mentioned study, 22 was the sample size, and in the present study, the sample size was 82), differences in the tools used [in that study, McCoy Female Sexuality Questionnaire (MFSQ) was used, while in the present study, FSFI was used], difference in the duration of the study (in that study, 3 months was the duration to evaluate the effectiveness of the pills, while in the present study, this duration was 4 months), and also differences in the demographic characteristics, attitude, and culture. No study was found that compared the contraceptive pills of two generations in association with sexual performance.
Among the strengths of this study were the type of the study, choice of sample selection, and being a double-blind study. The limitations of this study included the time limitation in evaluating the effects of second- and third-generation contraceptive pills on sexual function and not measuring the serum levels of DHEA-S, free testosterone, and total testosterone due to budget limitations. Therefore, it is recommended to conduct this study for duration longer than 4 months, with measurement of androgen in serum, and also to study other possible side effects such as nausea and menstrual bleeding. It is also recommended that health care staff provide accurate information about the possible changes in sexual functioning for people using oral contraceptive methods, and according to each individual's condition, recommend the best oral contraceptive which is suitable for them.
CONCLUSIONS
Sexual functioning in women is important and has an impact on the strength of family and social relationships, and sexual dysfunction for any reason is the cause of many negative consequences. Sexual problems are associated with social problems such as crime, sexual abuse, mental illness, and divorce. Satisfactory sexual performance is a factor for strengthening families and is the basis for obtaining and consolidating a culture. According to the results of this study, sexual functioning decreased in the second month of using the second-generation pills and sexual performance was significantly more in the group using third-generation pills compared to the group using second-generation pills. The most common type of oral contraceptive used in Iran is the second-generation oral contraceptive LD, which is freely distributed in health centers. Therefore, it is necessary for women who wish to use these contraceptive methods to be educated and consulted before they start using them. The third-generation contraceptive pills can be recommended to women who wish to use oral contraceptives.
Footnotes
Source of Support: Tabriz University of Medical Sciences
Conflict of Interest: Nil.
REFERENCES
- 1.Walsh KE, Berman JR. Sexual dysfunction in the older woman: An overview of the current understanding and management. Drugs Aging. 2004;21:655–75. doi: 10.2165/00002512-200421100-00004. [DOI] [PubMed] [Google Scholar]
- 2.Geneva: World Health Organization; 2006; 2002. Jan 28-31, World Health Organization. Defining sexual health: Report of a technical consultation on sexual health. [Google Scholar]
- 3.Safarinejad M. Female sexual dysfunction in a population-based study in Iran: Prevalence and associated risk factors. Int J Impot Res. 2006;18:382–95. doi: 10.1038/sj.ijir.3901440. [DOI] [PubMed] [Google Scholar]
- 4.Jahanfar S, Mowlanejad M. 3rd ed. Tehran: Byzhh, Publication Salemi; 2007. Textbook sexual dysfunction. [Google Scholar]
- 5.Kay C. The Royal College of General Practitioners’ Oral Contraception Study: Some recent observations. Clin Obstet Gynaecol. 1984;11:759–86. [PubMed] [Google Scholar]
- 6.Rosenberg MJ, Waugh MS. Oral contraceptive discontinuation: A prospective evaluation of frequency and reasons. Am J Obstet Gynecol. 1998;179:577–82. doi: 10.1016/s0002-9378(98)70047-x. [DOI] [PubMed] [Google Scholar]
- 7.Ott MA, Shew ML, Ofner S, Tu W, Fortenberry JD. The influence of hormonal contraception on mood and sexual interest among adolescents. Arch Sex Behav. 2008;37:605–13. doi: 10.1007/s10508-007-9302-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sanders SA, Graham CA, Bass JL, Bancroft J. A prospective study of the effects of oral contraceptives on sexuality and well-being and their relationship to discontinuation. Contraception. 2001;64:51–8. doi: 10.1016/s0010-7824(01)00218-9. [DOI] [PubMed] [Google Scholar]
- 9.Ryan KJ. Unites States: Mosby Incorporated; 1999. Kistner's gynecology and women's health. [Google Scholar]
- 10.Berek JS, Adashi EY, Hillard PA. Maryland: West Camden Street; 2012. Novak's gynecology: Williams and Wilkins Baltimore; p. 159. [Google Scholar]
- 11.Niroomanesh S, Lmyyan M. Tehran: Arjmandi; 2008. effective oral contraception in preventing pregnancy. 1st. [Google Scholar]
- 12.Festin M. Philippines: The WHO Reproductive Health Library (RHL); 2006. Progestogensin combined oral contraceptives for contraception. [Google Scholar]
- 13.Garycunningham F, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY. 23rd ed. New York: McGraw Hill Medical; 2010. Williams's obstetrics. [Google Scholar]
- 14.Guay A, Jacobson J, Munarriz R, Traish A, Talakoub L, Quirk F, et al. Serum androgen levels in healthy premenopausal women with and without sexual dysfunction: Part B: Reduced serum androgen levels in healthy premenopausal women with complaints of sexual dysfunction. Int J Impot Res. 2004;16:121–9. doi: 10.1038/sj.ijir.3901176. [DOI] [PubMed] [Google Scholar]
- 15.Bancroft J, Loftus J, Long JS. Distress about sex: A national survey of women in heterosexual relationships. Arch Sex Behav. 2003;32:193–208. doi: 10.1023/a:1023420431760. [DOI] [PubMed] [Google Scholar]
- 16.Davis AR, Castaño PM. Oral contraceptives and libido in women. Annu Rev Sex Res. 2004;15:297–320. [PubMed] [Google Scholar]
- 17.Graham CA, Bancroft J, Doll HA, Greco T, Tanner A. Does oral contraceptive-induced reduction in free testosterone adversely affect the sexuality or mood of women? Psychoneuroendocrinology. 2007;32:246–55. doi: 10.1016/j.psyneuen.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 18.Kingsberg S. Testosterone treatment for hypoactive sexual desire disorder in postmenopausal women. J Sex Med. 2007;4:227–34. doi: 10.1111/j.1743-6109.2007.00449.x. [DOI] [PubMed] [Google Scholar]
- 19.Davis SR, Burger HG. The role of androgen therapy. Best Pract Res Clin Endocrinol Metab. 2003;17:165–75. doi: 10.1016/s1521-690x(02)00078-7. [DOI] [PubMed] [Google Scholar]
- 20.Caruso S, Agnello C, Intelisano G, Farina M, Di Mari L, Cianci A. Sexual behavior of women taking low-dose oral contraceptive containing 15 μg ethinylestradiol/60 μg gestodene. Contraception. 2004;69:237–40. doi: 10.1016/j.contraception.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 21.Battaglia C, Battaglia B, Mancini F, Busacchi P, Paganotto M, Morotti E, et al. Sexual behavior and oral contraception: A pilot study. J Sex Med. 2012;9:550–7. doi: 10.1111/j.1743-6109.2011.02597.x. [DOI] [PubMed] [Google Scholar]
- 22.McCoy NL, Matyas JR. Oral contraceptives and sexuality in university women. Arch Sex Behav. 2007;25:73–90. doi: 10.1007/BF02437907. [DOI] [PubMed] [Google Scholar]
- 23.Malekian S. Tehran: Tehran University of Medical Sciences; 2009. The effect of oral contraceptives (L.D) and condoms on sexual function Females 49-19. [Google Scholar]
- 24.Khosravi A. 1st ed. Kermanshah: Health Research Center, Kermanshah University of Medical Sciences and Health Services; 2010. Health indicators in the Islamic Republic of Iran Broadcasting. [Google Scholar]
- 25.Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI) A Multidimensional Self-Report Instrument for the Assessment of Female Sexual Function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 26.Jafarabadi MA, Mohammadi S. Statistical Series: Summarizing and Displaying Data. J Diabetes Lipid Disord. 2013;12:83–100. [Google Scholar]
- 27.Jafarabadi MA, Mohammadi S. Statistical Series: Introduction to Statistical Inference (Point Estimation, Confidence Interval and Hypothesis Testing) J Diabetes Lipid Disord. 2013;12:173–92. [Google Scholar]
- 28.Asghari Jafarabadi M, Soltani A, Mohammadi SM. Statistical Series: Tests for Comparing of Means. Journal of Diabetes, 2013;12:265–291. [Google Scholar]
- 29.Oranratanaphan S, Taneepanichsku S. A double blind randomized control trial, comparing effect of drospirenone and gestodene to sexual desire and libido. J Med Assos Thai. 2006;89:17–22. [PubMed] [Google Scholar]
- 30.Strufaldi R, Pompei LM, Steiner ML, Cunha EP, Ferreira JA, Peixoto S, et al. Effects of two combined hormonal contraceptives with the same composition and different doses on female sexual function and plasma androgen levels. Contraception. 2010;82:147–54. doi: 10.1016/j.contraception.2010.02.016. [DOI] [PubMed] [Google Scholar]
- 31.Caruso S, Agnello C, Romano M, Cianci S, Lo Presti L, Malandrino C, et al. Preliminary study on the effect of Four-phasic Estradiol Valerate and Dienogest (E2V/DNG) Oral contraceptive on the quality of Sexual life. J Sex Med. 2011;8:2841–50. doi: 10.1111/j.1743-6109.2011.02409.x. [DOI] [PubMed] [Google Scholar]
- 32.Sabatini R, Cagiano R. Comparison profiles of cycle control, side effects and sexual satisfaction of three hormonal contraceptives. Contraception. 2006;74:220–3. doi: 10.1016/j.contraception.2006.03.022. [DOI] [PubMed] [Google Scholar]
- 33.DUNCAN, Laurie E, et al. Does hypertension and its pharmacotherapy affect the quality of sexual function in women? and ast. American journal of hypertension. 2000;13(6):640–647. doi: 10.1016/s0895-7061(99)00288-5. [DOI] [PubMed] [Google Scholar]