Abstract
Background
Back pain due to Lumbar Disc Disease is a major clinical problem. The treatment options range from physiotherapy to fusion surgery. A number of minimally invasive procedures have also been developed in the recent past for its management. Disc-FX is a new minimally invasive technique that combines percutaneous discectomy, nuclear ablation and annular modification. Literature on its role in the management of lumbar disc pathology is scarce.
Methods
We included 24 consecutive patients who underwent the Disc-FX for back pain due to lumbar disc pathology non-responsive to non-operative treatment for a period of at least 6 months. Based on Magnetic Resonance Imaging (MRI) these patients fell into 2 groups – those with degenerative disc disease (DDD) (n = 12) and those with a contained lumbar disc herniation (CLDH)(n = 12). They were evaluated using the Visual analogue scale (VAS), Oswestry Disability Index (ODI) and Short Form-36 (SF-36) scores preoperatively and postoperatively.
Results
The mean age was 37.9 years (21-53 years). There were 17 males and 7 females. One patient in each subgroup was excluded from the final evaluation. Significant improvement was seen in all outcome measures. The overall rate of reintervention for persistent symptoms was 18.18% (4/22); in the CLDH subgroup, it was 36.36% (4/11).
Conclusions and level of evidence
Early results after the Disc-FX procedure suggest that it s a reasonable treatment option for patients with back pain due to lumbar disc disease, especially for those with DDD who fail conservative treatment. It could be an alternative to procedures like fusion or disc replacement.
This study presents Level IV evidence.
Clinical relevance
We feel that our study establishes Disc-FX as a modality of treating symptomatic lumbar disc disease due to DDD. However, longer term prospective studies are needed to prove this and to evaluate its role in the treatment of patients with CLDH.
Keywords: Annulo-nucleoplasty, Disc-FX, lumbar disc disease, lumbar disc prolapse, degenerative disc disease
Introduction
Low back pain (LBP) from lumbar disc disease may be due to degenerative disc disease (DDD) or due to a disc prolapse. The spectrum of management of LBP due to DDD ranges from conservative treatment such as physiotherapy to surgical procedures such as disc replacement or spinal fusion. Major procedures like the latter are associated with a higher rate of surgical morbidity and complications.1–3 The role of discectomy in relieving leg pain due to a disc prolapse is well established. However, its utility in the management of back pain due to a small, contained lumbar disc herniation (CLDH) is less clear.4, 5 Hence, it is not surprising that several minimally invasive techniques have been introduced in recent years to manage back pain due to DDD and CLDH. Most of these techniques aim at reducing the intra-discal pressure and decompressing the disc, which in turn relieves the pressure on the neural tissue.6 There is considerable information on techniques such as nucleoplasty in the management of back pain and/or leg pain due to disc pathology 4, 7. There are some visualized endoscopic discectomy and annuloplasty procedures in the literature which may be more invasive, but have the advantage of visualizing the dorsal annulus following discectomy and visualized thermal annuloplasty.8 However, information on annulo-nucleoplasty using the Disc-FX (Elliquence, LLC, Baldwin, NY) system in the management of lumbar disc pathology is scarce. This system combines percutaneous manual discectomy, nucleus ablation and annular modification procedures at one sitting in a sequential manner. We did not find any study on Disc-FX during a comprehensive search of the English literature in MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials and Web of Science database. Using Google Scholar search, we were able to locate two English9, 10 and one Chinese11 article that described results with the use of the Disc-FX system.
The aim of our study was to evaluate the early results of the Disc-FX procedure in the management of back pain due to lumbar disc disease in patients who have failed conservative treatment. We also wanted to study the patient sub-groups in which the Disc-FX system would be most effective in treating back pain.
Material and methods
Our study included patients with symptomatic lumbar disc disease who failed non-operative treatment of at least 6 months. A total of 24 consecutive patients between September 2010 and December 2011, who fulfilled the criteria listed in Table 1 and who agreed to treatment with the Disc-FX system were recruited for the study. Lumbar disc disease may be in the form of degenerative disc disease (DDD) or disc prolapse. Degenerative disc disease is characterized by the presence of disc dehydration, as evidenced by a low signal on T2 weighted MRI images and loss of disc height. On the other hand, encroachment of epidural or foraminal space by an annular bulge or a disc fragment would be classified as a disc prolapse. Sequestered discs are not considered suitable for the Disc-FX procedure and have not been offered this procedure leaving only contained lumbar disc herniations (CLDH). CLDH may be in the form of a focal disc prolapse with thinning of the annulus fibrosus and protrusion of the nucleus pulposus or in the form of a diffuse annular bulge with no thinning of the annulus and no nuclear material protrusion. A cohort of patients who underwent discectomy done by the senior author (NK) during the same period were included as a control group. The indication for discectomy (rather than a DiscFX) was a clinical presentation of only leg pain or of leg pain overwhelmingly more than back pain.
Table 1.
Inclusion and Exclusion criteria
Inclusion Criteria
|
Exclusion Criteria
|
The Institutional Review Board's approval was obtained prior to the study and informed consent was taken from every patient. There were 12 in the DDD subgroup and 12 in the CLDH subgroup based on the preoperative MRI scan. These were patients who had failed at least 6 months of non-operative treatment. All patients had back and/or leg pain. A total of 24 procedures in 24 patients were performed. Visual analogue scale (VAS) and Oswestry Disability Index (ODI) scores were recorded for every patient pre–operatively, immediately post–operatively and at six months and one year after the procedure. Short form-36 (SF-36) scores were also obtained. At one-year follow-up, all patients were also asked if they would recommend the procedure to their family or friends. These patients continue to be followed up for long-term results.
Technique
All the cases were performed as a daycare procedure under conscious sedation (managed anaesthesia care) and local anesthesia. The patient was placed in prone position on a flat Jackson table with all bony prominences well padded. The target disc level was identified using an image intensifier (II). The side of the pathology was the preferred side of approach. The II image projections of the disc and lateral border of the pedicle on an AP image were marked on the skin. Similarly, on the lateral view, the projections of the disc space and the posterior vertebral body were marked. The entry point for a 45° trajectory from the vertical would be about a palms breadth away from the midline along the AP projection of the disc space. Similarly, a horizontal trajectory would start in line with the posterior border of the relevant disc in the lateral projection. If the distance between the latter point and the midline is divided into thirds it would mark the entry points for a 30° and a 60° trajectory. The gap between the 30° trajectory and teh zero degree trajectory is again divided into 3 parts to get the 10° and 20° trajectory. The trajectory of the needle depends upon the location of the pathology on the preoperative MRI scan. A 20°-30° trajectory from the horizontal plane is commonly used if feasible (The trajectory is modified at L5-S1 level when such trajectory is not possible due to a high iliac crest). The point of entry into the disc is the postero-lateral corner as guided by the AP and lateral II projections. Using the above entry point and target point, a 16G/18G spinal needle was guided lateral to the superior articular pillar (SAP), yet medial to the exiting nerve root. For the purpose of description, the procedure performed is discussed under the following steps:
Discogram
Manual Discectomy
Nucleus Ablation
Annulus Modulation
After the needle was positioned appropriately, a discogram was performed using a 2 ml mixture of the solution (10ml solution = 5ml of Omnipaque dye, 3ml of saline & 2ml of indigo carmine). Documentation included concordance and severity of the pain and a grading of the disc morphology.12 A guidewire was then placed through the needle into the nucleus pulposus, right up to the middle of the disc on AP and lateral. A small skin incision of 3mm was made to accommodate the introduction of the access cannula and the soft tissue dilator into the annulus. Manual discectomy of the intra-annular or subligamentary disc material is done using a small disc forceps or disc rongeurs. The steerable Trigger-Flex (Elliquence) probe was inserted through the cannula and nucleus ablation was performed with the Surgi-Max (Elliquence) generator set at Bipolar-Turbo mode. Six strokes of ablation were carried out for the nucleus in six different directions. Then extraction of any nuclear material is done using disc irrigation. Modulation of dorsal annulus was then carried out by placing the Trigger-Flex probe under the pathological annulus and using the Bipolar-Hemo mode of the Surgi-Max generator. Four strokes of modulation were performed in different directions on the annulus covering the width of the annulus.
Post-procedure, the patient was observed for any neurological deficit or other procedure related problems. The patient is usually discharged the same or on the following day.
Statistical analysis
The demographic and clinical data of the patients were analyzed descriptively. Clinical outcome scores like VAS, ODI and SF-36 score were compared with the respective preoperative scores using the paired t-test. Comparison of respective scores between the two subgroups was done using the student ‘t’ test. Rate of re-intervention and complications are summarized descriptively.
Results
The mean age of the study population was 37.9 years (21-53 years) with 17 males and 7 females. The duration of follow up was a minimum of 12 months for all patients. There were 12 patients in the DDD group and 12 in the CLDH group. The level of the procedure was L4-5 in 12 patients and L5-S1 in the other twelve. The duration of follow-up was calculated only for those who did not require re-intervention after Disc-FX (18 patients). The VAS, ODI and SF-36 scores at different time intervals are shown in Table 2 and Table 3.
Table 2.
Visual analogue scale (VAS), Oswestry Disability Index (ODI) and Short form-36 (SF-36) scores at different time intervals for the entire study population.
| Preoperative | Post-operative | 6 months | 1 year | |
|---|---|---|---|---|
| VAS | 6.5 | 3.08(0.00) | 3.77(0.00) | 3.99(0.015) |
| ODI | 43.16 | 23.25(.00) | 28.32(0.005) | 27.14(0.024) |
| SF-36 | 37.91 | - | 41.46(0.066) | 42.89(0.086) |
Figure in parentheses indicates p value when compared to the respective preoperative score. SF-36 scores were recorded only at 6 months and 1 year postoperatively.
Table 3.
Visual analogue scale (VAS), Oswestry Disability Index (ODI) and Short form-36 (SF-36) scores at different time intervals for the two subgroups-degenerative disc disease (DDD) and contained lumbar disc herniation (CLDH).
| Preoperative | Postoperative | 6 months | 1 year | |
|---|---|---|---|---|
| Visual analogue scale (VAS) scores | ||||
| DDD | 6.4 | 3.08 (0.002) | 3.41 (0.009) | 3.7 (0.173) |
| CLDH | 6.6 | 3.08 (0.002) | 4.2 (0.01) | 4.28 (0.041) |
| Oswestry Disability Index (ODI) scores | ||||
| DDD | 40.66 | 24.33 (0.003) | 27.16(0.028) | 26.28(0.091) |
| CLDH | 45.66 | 22.16(0.002) | 29.7(0.047) | 28(0.128) |
| Short form-36 (SF-36) scores | ||||
| DDD | 42.91 | - | 39.4(0.357) | 42.6(0.461) |
| CLDH | 32.9 | - | 43.17(0.136) | 43.25(0.102) |
Figure in parentheses indicates p value when compared to the respective preoperative score. SF-36 scores were recorded only at 6 months and 1 year postoperatively.
Visual analogue scale (VAS) scores
The mean VAS score for the entire population improved from 6.5 preoperatively to 3.77 at 6 months post-operatively and this improvement was statistically significant (p = 0.000). The mean VAS at one year post-operation deteriorated to 3.99 but the difference was not statistically significant (p = 0.015), although all patients had improvement in symptoms. The trend was similar in the two subgroups (DDD and CLDH) when analysed separately; with significant improvement sustained till six months post-operatively, which continued up-to one year although the difference was not significant.
Oswestry Disability Index (ODI) score
Significant improvement in the ODI was seen from a mean preoperative score of 43.16 to 28.32 at six months (p = 0.005). This improvement was sustained in patients followed up till one year but not statistically significant (p = 0.024). When the two subgroups were analaysed separately, significant improvement was sustained only till six months post-operatively in each of the groups.
Short Form-36 (SF-36) score
The changes in the SF-36 scores at six months and one year were not significant either for the entire population or the subgroups.
The changes in the outcome scores after the procedure when compared to the respective preoperative ones were not significantly different between the two subgroups (Table 3).
Reintervention
Four patients in the CLDH subgroup required micro-discectomy within one year of the primary procedure in view of recurrent symptoms. One of these underwent a repeat Disc-FX procedure followed by a micro-discectomy all within one year of the primary procedure. In one patient with persistent back pain after the primary procedure for CLDH, the source of pain was identified as L5 lysis. He underwent L5 lysis repair at three months after the first procedure and showed significant relief of symptoms. One patient in the DDD subgroup developed new onset leg pain two months after the Disc-FX procedure. This was managed with a trans-foraminal block at a different level to the index procedure vitiating further follow-up. If the lysis-repair patient and the one undergoing trans-foraminal block were excluded, 4/11 (36.36%) patients required a re-intervention in the CLDH subgroup against none in the DDD group. The overall rate of re-intervention was 4/22 (18.18%).
We compared this patient group to a group of 24 consecutive patients who underwent a discectomy procedure during the same period. The indication for discectomy (rather than a DiscFX) was a clinical presentation of only leg pain or of leg pain overwhelmingly more than back pain. None of the patients in the discectomy group needed a revision procedure during the follow-up period.
Recommend the procedure to family or friends
Only 3/11 (27.27%, patient with lysis repair excluded) patients in the CLDH subgroup were willing to recommend the procedure to their family or friends, as against 6/11 (54.55%, patient with new onset leg pain excluded) patients in the DDD subgroup.
Complications
No procedure related complications were noted in any of the patients. However, we encountered difficulty in accessing the L5-S1 disc level in three patients and a modified trajectory was used to perform the procedure.
Discussion
We would like to trace the historical evolution of the minimally invasive annuloplasty / annulo-nucleoplasty procedures. Percutaneous discectomy through a cannula has been around since the invention of the operative microscope in 1967; however, the microdiscectomy requires muscle stripping as well as bone resection and retraction of the nerve. Kambin and Hijikata described the endoscopic trans-foraminal discectomy technique in 1973.8, 13, 14 The original technique required the insertion of an endoscope intermittently to inspect the disc and the annulus. The use of a bi-portal approach allowed the performance of the discectomy under direct vision in real time. An endoscope with an added working channel then allowed for direct visualization via a uni-portal approach15. Yeung's modifications of the working channel rod-lens spine endoscope added multi-channel irrigation, specialized cannulas and discectomy tools.16
The role of nucleoplasty and intradiscal electrothermy (IDET) for DDD and CLDH has been well established in literature.4, 6, 7, 17–19 Radiofrequency and thermal treatment modalities rely mainly on indirect decompression due to thermal effect on the disc. Disc-FX system uses manual debulking of the disc, nucleus ablation and annular modification, whilst keeping the procedure minimally invasive.9, 10 Apart from the percutaneous manual discectomy, Disc-FX involves application of radiofrequency energy for nucleus ablation and annular modification. This technique utilizes higher frequency of 1.7 MHz through the Elliquence Surgi-Max generator with two different modulations -Bipolar Turbo and Bipolar Hemo modes. The Turbo mode allows nuclear ablation, while the Hemo mode allows annular modification with shrinkage.9, 10. The use of higher frequency offers the advantage of reduced heat and minimal tissue alteration9, 10 The radiofrequency energy is applied using a steerable probe (Trigger-Flex, Elliquence).
Post-mortem studies have shown that an average of 0.8g of disc material is removed with nuclear ablation with a corresponding reduction in intradiscal pressure9. Modulation of the dorsal annulus results in cauterization of inflamed structures, shrinkage of the annulus by 30% and expansion of the epidural space of up to 9%.9 Moreover, annular modulation may also cause reduction in pain generated by the annular nerve fibres in DDD by ablating the C-fibres. Steerable delivery system using Trigger-Flex probe permits targeted application in the region of the pathology. Disc-FX can, therefore, be an effective minimally invasive technique in the management of lumbar disc pathology. Endoscopic visualization in between the steps can help documentation of decompression but it is not an essential part of the procedure.
The learning curve to achieve a 90% excellent result using the foraminal endoscopic discectomy technique has been studied before.20 The authors surmise that an experience of 72 surgeries enables the surgeon to achieve this target level.
Mirzai et al,19 in their study on 52 patients with disc herniation causing leg pain treated with nucleoplasty showed a reduction in mean leg pain by >50%. Patient satisfaction was >80% with good improvements in disability and analgesia requirement. Only 2/52 (3.85%) patients in their series had to be operated after nucleoplasty at a mean follow-up of 12.1 ± 1.6 months. Gerszten17 in his study involving 67 patients with primarily radicular leg pain due to disc herniation concluded that nucleoplasty was a safe and viable minimally invasive technique, which improves leg pain and the quality of life of patients with contained disc herniation. In our study, patients with CLDH had statistically significant improvement in their VAS and ODI scores only upto six months after the procedure, although the results were sustained at one year after the procedure. Moreover, the one year scores in the CLDH subgroup is reflective of only eight patients since the other four had already undergone a second procedure before the end of one year. Only three out of the remaining eight were willing to recommend the procedure at one year.
Hellinger9undertook a prospective study of 72 patients with radicular and local lumbar pain syndromes and mild neurological deficits secondary to contained disc extrusions and protrusions who underwent a Disc-FX procedure. He reported that back and leg pain showed a significant improvement, from an average VAS of 8.5 to 2 (post-operatively), 3.5 (after six weeks) and 3.3 (after six months). The original Mcnab Index showed 90% patients with excellent and good post-operative results. After six weeks and six months, the results were sustained in >70% patients. All patients would undergo a similar procedure again if necessary and were willing to recommend such a procedure to others. The good outcomes in this study could, perhaps, be attributed to the use of an endoscope for visualisation of the discectomy.
The improvement seen in the DDD subgroup in our study was not significantly different from the CLDH subgroup. However, none of the patients required re-intervention in the DDD subgroup. Three patients were advised spinal fusion or artificial disc replacement at 1 year as they had persistent back pain. However they opted for observation and physiotherapy as their pain had substantially improved after the Disc-FX procedure.
Clinical history and MRI appearance were used to decide on suitability of the patients for this procedure. Discogram is not useful in diagnosing a sequestrated disc. Preoperative discograms were not used to evaluate the morphology of the disc. While we accept that a CT discogram would best define the disc morphology, the benefits do not outweigh radiation, logistical and cost considerations. MRI examination alone has been deemed satisfactory as a selection tool for spinal fusion surgery.21 Discogram was used intra-operatively to show the pattern of dye leak and to guide the placement of the probe. It was not used for diagnostic purposes. Data is currently being collected on correlation between discogram findings and outcome but numbers are too small at present.
Chemical radiculitis was considered as a potential source of pain. Pain due to this pathology is more likely to respond to an epidural steroid injection.22 Not all of our patients underwent a selective nerve root block, however, they had all had symptoms for longer than 6 months and had failed other non-operative measures.
Irrigation used during the procedure helps to control the heat levels at the tip of the probe and to limit the area that is subjected to thermal coagulation. The indigo carmine dye has been shown to selective colour the degenerate part of intervertebral discs blue.23 Using the dye as part of the discogram injectate helps to define the boundaries of the degenerate disc. This is particularly useful at the time of discectomy as a marker for removal of the degenerate extruded disc and minimize the risk of removing normal disc material which could happen when it is not assisted by an endoscope.
Young patients with mild to moderate chronic low back pain secondary to DDD, who have failed conservative treatment, are a challenge to treat as the only options available currently are spinal fusion or disc replacement. Though these procedures have shown good results in the treatment of DDD, they have their own drawbacks. A successful Disc-FX procedure in these patients could help delay or obviate the need for a definitive fusion or disc replacement surgery. This procedure has minimal complications in comparison to fusion or replacement. There were no procedure related complications in our series after Disc-FX.
Six out of the twelve patients in the CLDH group had a re-intervention within one year of the primary procedure. On analysing the preoperative MRI scans of these patients, the morphology of the disc prolapse could be categorised into either a focal disc prolapse with thinning of the annulus fibrosus or a generalised disc bulge with no annular thinning. We noted that all four patients who did poorly after their Disc-FX procedure and required a formal micro-discectomy had a focal disc prolapse on their preoperative MRI scans. The one patient who responded to a lysis block after inadequate relief from the Disc-FX had a generalised disc bulge. There appears to be a trend suggesting that this procedure may be less effective in patients with a focal disc prolapse than in those with a generalised disc bulge. It is possible that these patients already have thinning of their annulus fibrosus and creation of a further 2.7mm annulotomy close to this site of weakness predisposes them to a recurrent prolapse(Figure 1).
Fig. 1.
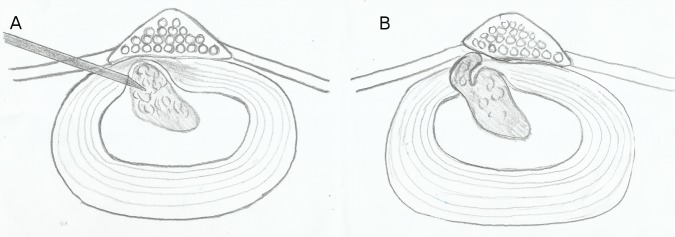
1A shows the position of the Disc-FX cannula relative to the focal disc relapse. 1B shows the possibility of a recurrent disc prolapse through the annulotomy rent.
The poor results in the focal disc prolapse subgroup may also be attributed to the fact that the percutaneous manual discectomy is carried out under II. The use of an endoscope allows decompression under direct vision and may improve the accuracy of cannula placement. This might have reduced the rate of recurrent leg pain. Our current numbers are not large enough to show a statistical significance in this observed difference between patients with a focal disc prolapse and a generalised disc bulge. We recommend that the Disc-FX Procedure be used with caution in patients with a focal disc prolapse. Other authors have also noted a higher rate of re-intervention after foraminal discectomy procedures in patients with disc extrusion.24 They recommend that in patients where the height of the extrusion is more than the base, an alternative procedure such as a standard discectomy be used.
Three patients with CLDH underwent a repeat MRI before undergoing microdiscectomy. It was incidentally noted that all three patients showed an increased signal intensity on sagittal T2 images when compared to pre-procedure MRI, suggesting rehydration of the disc after the Disc-FX procedure consistent with other reports in the literature.25
Conclusion
Our results for the Disc-FX procedure suggest that it could be a reasonable treatment option for patients with DDD who fail conservative treatment instead of fusion or disc replacement.
In our opinion, the ideal patient selection criteria for a DiscFx procedure would be a a patient with a combination of back and leg pain who has failed a period of non-operative treatment, with MRI evidence of mild to moderate DDD with or without a diffuse disc bulge. Patients with a sequestrated disc prolapse and with a known allergy to any of the components of the discogram injectate should not be offered this procedure. In addition, patients with little or no back pain or with a focal disc prolapse do not appear to be candidates for the Disc-Fx procedure at present. This could, however, change if the routine use of an endoscope to perform the discectomy under direct vision improves the outcome in this group of patients. Larger studies with a longer follow-up are suggested to collect more evidence on the efficacy of the Disc-FX procedure.
Disclosures
The authors declare no financial disclosures.
References
- 1.Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am. 2004 Jul;86-A(7):1497–1503. doi: 10.2106/00004623-200407000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Freeman BJ, Davenport J. Total disc replacement in the lumbar spine: a systematic review of the literature. Eur Spine J. 2006 Aug;15(Suppl 3):S439–447. doi: 10.1007/s00586-006-0186-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van den Eerenbeemt KD, Ostelo RW, van Royen BJ, Peul WC, van Tulder MW. Total disc replacement surgery for symptomatic degenerative lumbar disc disease: a systematic review of the literature. Eur Spine J. 2010 Aug;19(8):1262–1280. doi: 10.1007/s00586-010-1445-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gerges FJ, Lipsitz SR, Nedeljkovic SS. A systematic review on the effectiveness of the Nucleoplasty procedure for discogenic pain. Pain Physician. 2010 Mar-Apr;13(2):117–132. [PubMed] [Google Scholar]
- 5.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT) Spine (Phila Pa 1976). 2008 Dec 1;33(25):2789–2800. doi: 10.1097/BRS.0b013e31818ed8f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh V, Manchikanti L, Benyamin RM, Helm S, Hirsch JA. Percutaneous lumbar laser disc decompression: a systematic review of current evidence. Pain Physician. 2009 May-Jun;12(3):573–588. [PubMed] [Google Scholar]
- 7.Kumar NS, Shah SM, Tan BW, Juned S, Yao K. Discogenic axial back pain: is there a role for nucleoplasty? Asian spine journal. 2013 Dec;7(4):314–321. doi: 10.4184/asj.2013.7.4.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tsou PM, Alan Yeung C, Yeung AT. Posterolateral transforaminal selective endoscopic discectomy and thermal annuloplasty for chronic lumbar discogenic pain: a minimal access visualized intradiscal surgical procedure. Spine J. 2004 Sep-Oct;4(5):564–573. doi: 10.1016/j.spinee.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 9.Hellinger S. Disc-FX – A Treatment for Discal Pain Syndromes Combining a Manual and Radiofrequency-assisted Posterolateral Microtubular Decompressive Nucleotomy. European Musculoskeletal Review. 2011;6(2):100–104. [Google Scholar]
- 10.Hellinger S. Radiofrequency -assisted Lumbar Semi-endoscopic Manual Discectomy using the Disc-FX System-Perliminary Results of Various Ongoing Clinical Outcome Studies Worldwide. European Musculoskeletal Review. 2011;6(4):265–271. 21 october 2011. [Google Scholar]
- 11.Zhang WWH, Jiao JX, Wang YX, Yang DL, Ding WY. Primary results of the 3 in 1 technique of Disc-FX system for the discogenic low back pain. Chin J Orthop. 2011;31(10):1049–1055. [Google Scholar]
- 12.Kumar NSS, Tan PK. Discography. Techniques in Orthopaedics. 2013;28(1):73–77. 2013. [Google Scholar]
- 13.Hijikata SY, Hijikata N, Nakayama T. Percutaneous discectomy: a new treatment method for lumbar disc herniation. J Toden Hosp. 1975;5:5–13. [Google Scholar]
- 14.Kambin P. Arthroscopic microdiskectomy. The Mount Sinai journal of medicine, New York. 1991 Mar;58(2):159–164. [PubMed] [Google Scholar]
- 15.Yeung AT. Minimally Invasive Disc Surgery with the Yeung Endoscopic Spine System (YESS) Surgical technology international. 1999;8:267–277. [PubMed] [Google Scholar]
- 16.Yeung AT. The evolution of percutaneous spinal endoscopy and discectomy: state of the art. The Mount Sinai journal of medicine, New York. 2000 Sep;67(4):327–332. [PubMed] [Google Scholar]
- 17.Gerszten PC, Welch WC, King JT., Jr Quality of life assessment in patients undergoing nucleoplasty-based percutaneous discectomy. J Neurosurg Spine. 2006 Jan;4(1):36–42. doi: 10.3171/spi.2006.4.1.36. [DOI] [PubMed] [Google Scholar]
- 18.Helm Ii S, Deer TR, Manchikanti L, et al. Effectiveness of thermal annular procedures in treating discogenic low back pain. Pain Physician. 2012 May-Jun;15(3):E279–304. [PubMed] [Google Scholar]
- 19.Mirzai H, Tekin I, Yaman O, Bursali A. The results of nucleoplasty in patients with lumbar herniated disc: a prospective clinical study of 52 consecutive patients. Spine J. 2007 Jan-Feb;7(1):88–92. doi: 10.1016/j.spinee.2006.02.033. discussion 92-83. [DOI] [PubMed] [Google Scholar]
- 20.Morgenstern RM, Morgenstern C, Yeung A.T. The Learning Curve in Foraminal Endoscopic Discectomy: Experience Needed to Achieve a 90% Success Rate. SASJ. 2007;1(3):100–108. doi: 10.1016/SASJ-2007-0005-RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gill K, Blumenthal SL. Functional results after anterior lumbar fusion at L5-S1 in patients with normal and abnormal MRI scans. Spine (Phila Pa 1976). 1992 Aug;17(8):940–942. doi: 10.1097/00007632-199208000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Manchikanti L, Buenaventura RM, Manchikanti KN, et al. Effectiveness of therapeutic lumbar transforaminal epidural steroid injections in managing lumbar spinal pain. Pain Physician. 2012 May-Jun;15(3):E199–245. [PubMed] [Google Scholar]
- 23.Kim IS, Kim KH, Shin SW, Kim TK, Kim JI. Indigo carmine for the selective endoscopic intervertebral nuclectomy. Journal of Korean medical science. 2005 Aug;20(4):702–703. doi: 10.3346/jkms.2005.20.4.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yeung AT. The Evolution and Advancement of Endoscopic Foraminal Surgery: One Surgeon's Experience Incorporating Adjunctive Techologies. SASJ. 2007;1(3):108–117. doi: 10.1016/SASJ-2006-0014-RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arslan E, Demirci I, Kilincaslan MO, Hacifazlioglu C, Demir T, Demirkale I. Identification of intervertebral disc regeneration with magnetic resonance imaging after a long-term follow-up in patients treated with percutaneous diode laser nucleoplasty: a retrospective clinical and radiological analysis of 14 patients. Eur Spine J. 2014 May;23(5):1044–1051. doi: 10.1007/s00586-014-3194-1. [DOI] [PubMed] [Google Scholar]


