Abstract
Introduction:
Spigelian hernias represent only 1% to 2% of all abdominal wall hernias. The treatment, however, remains controversial but depends on institutional expertise. This case series reports the first experience with single-incision laparoscopic totally extraperitoneal (SILTEP) repair of Spigelian hernias with telescopic extraperitoneal dissection in combination with inguinal hernia repair.
Methods:
From February 2013 to April 2014, all patients referred with inguinal or Spigelian hernias, without histories of extraperitoneal intervention, underwent SILTEP repair with telescopic extraperitoneal dissection. A single-port device, 5.5 mm/52 cm/30° angled laparoscope, and conventional straight dissecting instruments were used for all cases. Extraperitoneal dissection was performed under direct vision with preservation of preperitoneal fascia overlying retroperitoneal nerves. Inguinal herniorrhaphy was performed with lightweight mesh that covered low-lying Spigelian defects. High-lying Spigelian defects were repaired with additional mesh.
Results:
There were 131 patients with 186 (92 direct) inguinal hernias and 7 patients with 8 Spigelian hernias (6 incidental, including 1 bilateral and 2 preoperatively diagnosed), with a mean age of 51.3 years and a mean body mass index of 25.1 kg/m2. An additional piece of mesh was used for 3 hernias. All Spigelian hernias were associated with direct inguinal hernias, and 8 combined inguinal and Spigelian hernias were successfully repaired with SILTEP repair with telescopic extraperitoneal dissection as day cases. There were no clinical recurrences during a mean follow-up period of 6 months (range, 1–15 months).
Conclusions:
Combined Spigelian and inguinal hernias can be successfully treated with SILTEP herniorrhaphy with telescopic extraperitoneal dissection. The high incidence of Spigelian hernias associated with direct inguinal hernias suggests a high index of suspicion for Spigelian hernias during laparoscopic inguinal herniorrhaphy.
Keywords: Spigelian hernia, Inguinal, Single-incision laparoscopic surgery, Telescopic extraperitoneal dissection
INTRODUCTION
Adriaan van den Spiegel first described the semilunar line (Spigelian line) in 1645.1 In 1764, Josef Klinkosch described and defined the Spigelian hernia as a hernia, which protrudes through the transversus abdominis muscle.2 There is a propensity for hernia development in the so-called Spigelian hernia belt, which is a 6-cm-wide region inferior to the umbilicus and superior to the inferior epigastric vessels resulting in high-lying Spigelian hernias, although so-called low-lying Spigelian hernias have also been reported protruding through the Spigelian aponeurosis in the region of Hesselbach's triangle.3–5
Most Spigelian hernias are not detectable on clinical examination, because the herniation through the transversus abdominis is contained anteriorly by the intact external oblique muscle. Hence, symptoms tend to be vague initially, and a high index of suspicion together with the use of ultrasonography and computed tomography will increase the diagnostic yield preoperatively.6–8, It has been estimated that up to 17% of Spigelian hernias present with strangulation because of delays in diagnosis.9 With the increasing popularity of the laparoscopic approach for treating abdominal hernias, Spigelian hernias can now be treated in the same fashion as other abdominal hernias,10 namely, laparoscopic preperitoneal11–16 and intraperitoneal onlay mesh repair17,18 in addition to conventional anterior repair.9,19 The exact laparoscopic modality depends on many factors, including institutional expertise, incidental or preoperative diagnosis, and strangulation.
In an attempt to further reduce parietal trauma, single-incision laparoscopic (SIL) surgery has become increasingly used in the treatment of inguinal hernias.20–22 It therefore becomes a natural progression to treat Spigelian hernias in the same way. Our institution has been performing SIL total extraperitoneal (SILTEP) inguinal23 and ventral24 routinely since December 2009. Although SILTEP repair offers real potential advantages over conventional multiport total extraperitoneal repair in reducing postoperative pain and analgesic requirements and allowing earlier return to work and normal physical activities (A Prospective Study Comparing Single and Multiport Laparoscopic Inguinal Hernia Repair [SILSTEP]; ClinicalTrials.gov identifier NCT01660048), the former procedure until now has remained more expensive because of the relatively higher costs of single-port devices.21 With the increasing popularity of SIL surgery, the costs of these devices have decreased, and now, for the first time, SILTEP repair can be performed with telescopic extraperitoneal dissection, negating the use of balloon dissection, with potential cost savings.
The aim of this prospective study was to assess the safety, efficacy, and potential benefits of SILTEP repair, with telescopic extraperitoneal dissection, for Spigelian hernias, which were diagnosed either preoperatively or as incidental hernias during SILTEP inguinal herniorrhaphy.
MATERIALS AND METHODS
Prior to commencement of enrollment into this study, all patients signed consent forms that had been approved by the Independent Review Board of Holroyd and St Luke's Hospitals for the purpose of data collection and patient follow-up. All patients referred between February 18, 2013, and April 8, 2014, with inguinal or Spigelian hernias, without prior laparoscopic inguinal hernia repair, underwent SIL surgery with telescopic extraperitoneal dissection. After induction of general anesthesia, 1 g of cefazolin was given intravenously. All patients were catheterized for the duration of the surgical procedure.
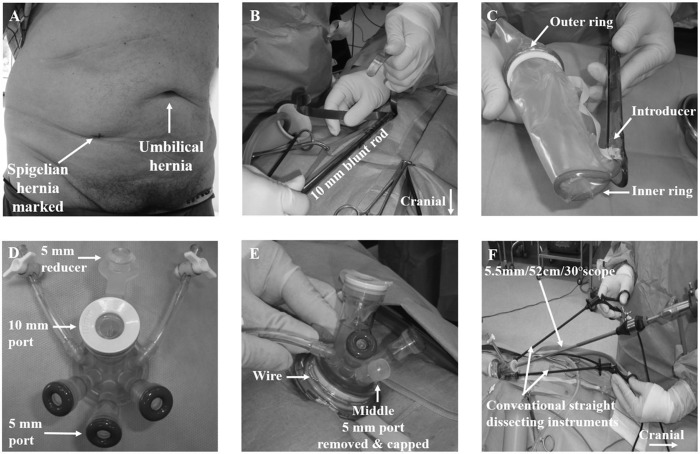
Placement of the Single-Port Device
After infiltration with 20 mL of bupivacaine 0.5% with 1:200,000 ephedrine, a 1.5-cm crescentic infraumbilical incision was made, and the anterior rectus sheath was incised transversely and the rectus muscle retracted laterally. The patient was then placed in a Trendelenburg position at 15° head down. A blunt rod was inserted into the extraperitoneal space parallel and posterior to the rectus muscle toward the pubic symphysis (Figure 1). This created a small tunnel (similar to placing the distension balloon trocar) to help with the extraperitoneal dissection. The inner ring of the single-port device (Triport+; Olympus Winter & Ibe GmbH, Hamburg, Germany) was then deployed into the extraperitoneal space, and the former was pulled back firmly against the rectus muscle. The excess sheath was then removed before the top platform was placed onto the outer ring. To prevent slippage of the plastic sleeve through the outer ring and the top platform, a wire was tightened around the outer ring (Figure 1). After insufflation with carbon dioxide, a 5.5-mm/30°/52-cm laparoscope (Karl Storz, Tuttlingen, Germany) was placed into the 10-mm port with a 5-mm reducer, and 2 conventional straight dissecting instruments were placed into the 5-mm ports directly into the extraperitoneal space (Figure 1).
Figure 1.
SIL Spigelian and inguinal hernia repair with telescopic extraperitoneal dissection. (A) A patient with a Spigelian hernia diagnosed and marked by ultrasonography and right inguinal and umbilical hernia diagnosed clinically. (B) Insertion of a blunt rod into the extraperitoneal space. (C) Plastic sheath and introducer of Triport system. (D) The top platform of Triport system. (E) Deployed Triport+. (F) Intraoperative setup for single incision laparoscopic surgery with a 5.5-mm/52-cm/30° angled laparoscope and conventional straight dissecting instruments.
Telescopic Extraperitoneal Dissection
The extraperitoneal dissection was performed under direct vision using a combination of blunt dissection and electrocautery that allowed small blood vessels to be cauterized or clipped, or both (Figures 2 and 3). The dissection followed a precise sequence, namely, the dissection of the suprapubic space and then, staying high and lateral to the inferior epigastric vessels, the lateral space before turning attention to reducing any direct, indirect inguinal, and/or femoral hernia and any associated lipoma of the cord. The peritoneum was dissected proximally by at least 5 cm, preserving the vas deferens and testicular vessels in men and the round ligament in women and, more important, the preperitoneal fascia overlying the retroperitoneal nerves akin to the dissection during a transabdominal preperitoneal repair. During conventional multiport laparoscopic total extraperitoneal inguinal hernia repair, the extraperitoneal space is partially created by the distension balloon, and the dissection takes place via the 5-mm ports, which are placed inferior to the structural balloon inflation bulb (Tyco Healthcare; Norwalk, Connecticut) at the umbilicus, and the dissection starts at the pubic symphysis and then laterally. The bulkiness of the structural balloon bulb tends to limit proximal dissection. However, during telescopic dissection with the Triport system, the dissection of the extraperitoneal space starts at the umbilicus and follows the rectus muscle down to the pubic symphysis. The low profile of the inner ring of the Triport system allows the dissection to proceed more laterally from the umbilicus diagonally toward the anterior superior iliac spine, across the Spigelian hernia belt. This allows dissection of both preoperatively diagnosed and incidental Spigelian hernias (Figure 2). Any Spigelian hernia sac and contained contents, usually extraperitoneal fat, were reduced. Perforating blood vessels in and around the Spigelian hernia were doubly clipped and divided and the dissection then continued some 5 cm proximal to the Spigelian hernia for adequate mesh coverage (Figure 3).
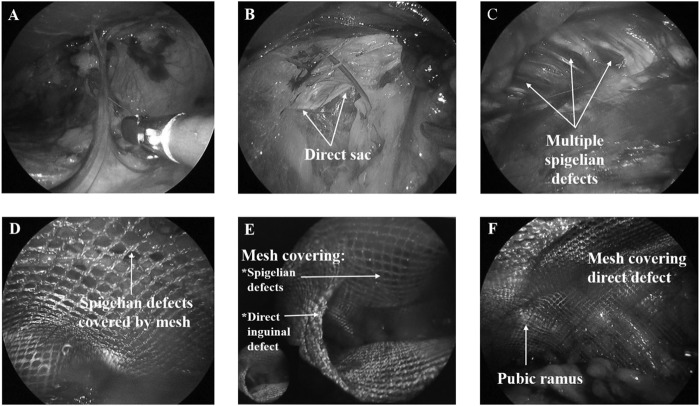
Figure 2.
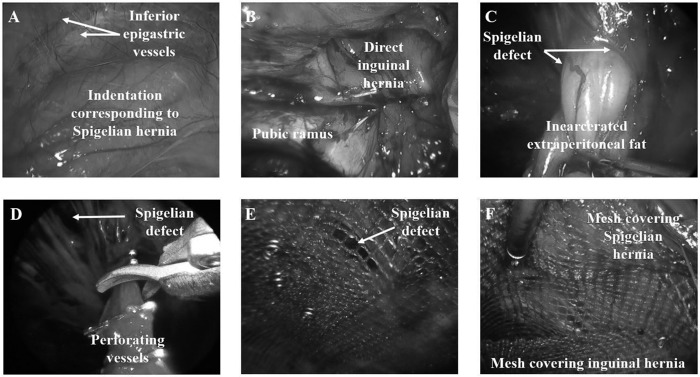
Intraoperative views of a patient (from Figure 1) presenting with right Spigelian and direct inguinal hernia undergoing SIL Spigelian and inguinal hernia repair with mesh. (A) Intraperitoneal view of site of Spigelian hernia. (B) Direct inguinal hernia. (C) Incarcerated extraperitoneal fat via sharp small defect in the transversus abdominis. (D) Perforating blood vessels being clipped and divided to achieve adequate proximal clearance for mesh placement. (E) Mesh covering Spigelian defect. (F) Mesh covering the inguinal hernia to cover the inferior aspect of mesh covering Spigelian defect.
Figure 3.
SIL repair of an incidental Spigelian hernia during repair of direct inguinal hernia with telescopic extraperitoneal dissection. (A–F) Extraperitoneal views. (A) Dissection of the extraperitoneal space under direct vision allowing electrocautery of blood vessels. (B) Direct inguinal hernia sac being dissected. (C) Incidental multiple Spigelian defects and associated thin fibers of the transversus abdominis predisposing to further herniation. (D) Mesh covering the Spigelian defects. (E) Superior view of 2 separate meshes that covered Spigelian and direct inguinal hernia defects. (F) Direct inguinal defect well covered with mesh extending inferior to pubic ramus as well as medially.
Mesh Placement and Fixation
The 5-mm laparoscope was placed into a 5-mm port and introduced into the extraperitoneal space to lie just within the inner ring. The rolled-up mesh was introduced via the 10-mm port directly into the extraperitoneal space (Figure 1). A low-lying Spigelian hernia may be covered by the same mesh as for the inguinal hernia, although the mesh (VyproII; Johnson & Johnson International, St Stevens-Woluwe, Belgium) would be 14 to 15 cm as opposed to 12 to 15 cm normally used, with the shorter diameter in the craniocaudal direction. High-lying or more laterally placed Spigelian hernias were repaired with an additional 10 to 15 cm mesh, with the longer diameter in the craniocaudal direction. The superior edge of the mesh was tacked (Protack; Covidien, Norwalk, Connecticut) with spiral tacks 5 cm proximal and 2 cm distal to the Spigelian hernia while its inferior edge was left “floating,” though fully unrolled, but this was then lifted up against the anterior abdominal wall by the mesh used to repair the inguinal hernia (Figure 3). The latter mesh was tacked medially in the midline above the pubic symphysis twice and laterally, at least 1 cm medial and superior to the anterior superior iliac spine, once. For direct inguinal hernias, a further tack was placed into the pubic ramus to minimize the risk for the mesh protruding into a large direct sac, if present. During deflation of the extraperitoneal space, the patient was placed into a reverse Trendelenburg position, and this process was carefully observed to prevent the inferior edge of the mesh from lifting up. The anterior rectus sheath was then closed with 0 PDS continuous sutures, and the skin wound was closed with dissolvable suture subcuticularly.
RESULTS
Between February 18, 2013, and April 8, 2014, 131 patients were referred with 186 (92 direct) inguinal hernias. The mean age of these patients was 50.7 year (range, 21–78 years), and there were 6 women. From this cohort, 7 patients had 8 Spigelian hernias; 6 were on the right side, all in men with a mean age of 51.3 years (range, 22–73 years). The mean body mass index was 25.3 kg/m2 (range, 22.1–27.5 kg/m2). Two patients were referred with Spigelian hernias whose hernias were not palpable, and both were diagnosed by ultrasonography and computed tomography. These 2 patients were found to have clinically obvious ipsilateral inguinal hernias that were subsequently confirmed at operation. There were 6 incidental Spigelian hernias in 5 patients. All patients underwent SIL extraperitoneal repair with telescopic extraperitoneal dissection without the use of additional ports or conversion to open surgery (Table 1). There were no intraoperative complications. One patient, preoperatively, who was on a high prophylactic dose of short-acting subcutaneous anticoagulant for clotting tendencies, developed an extraperitoneal hematoma 3 days after anticoagulant was restarted after surgery. This was initially treated conservatively by stopping anticoagulation. On 6-week follow-up, the hematoma persisted and was causing persistent discomfort. It was successfully drained with a small incision in the right iliac fossa, and there were no further complications. All patients undergoing SIL inguinal and Spigelian hernia repair with telescopic extraperitoneal dissection were discharged home on the same day. There were no clinical recurrences of either inguinal or Spigelian hernias with a mean follow-up of 9 months (range, 3–18 months).
Table 1.
Patient age, BMI, hernia type, preoperative diagnosis, additional mesh used for Spigelian hernia, and operation time
| Patient | Age, y | BMI, kg/m2 | Inguinal/Type | Spigelian | Umbilical | Additional Mesh Used | Operation Time, min |
|---|---|---|---|---|---|---|---|
| 1 | 39 | 24.9 | B/direct | R, incidental | No | No | 88 |
| 2 | 58 | 25.9 | B/direct | R, incidental | No | No | 62 |
| 3 | 73 | 24.2 | R/direct | R, preoperative | Yes | Yes | 78 |
| 4 | 58 | 26.9 | B/direct | R, incidental | Yes | Yes | 98 |
| 5 | 63 | 25.8 | B/direct | B, incidental | No | No | 125 |
| 6 | 22 | 22.1 | B/direct | L, preoperative | No | No | 72 |
| 7 | 46 | 27.5 | R/direct | R, incidental | Yes | Yes | 115 |
All patients were men. All patients underwent SILTEP repair with telescopic extraperitoneal dissection. B, bilateral; BMI = body mass index, L, left; R, right.
DISCUSSION
Although Spigelian hernias are relatively rare, their risk for strangulation is much higher than for other types of hernias. Laparoscopic hernia repair has become increasingly more popular since the 1990s, and Spigelian hernias are increasingly repaired laparoscopically by total extraperitoneal, transabdominal preperitoneal, or intraperitoneal onlay mesh repair.11–18 Because of the relative rarity of Spigelian hernias, most reports consist of single cases or small series. Moreno-Egea et al25 prospectively randomized 22 patients to either anterior (11 patients) or laparoscopic (11 patients) repair. The latter group consisted of 8 totally extraperitoneal approaches and 3 intra-abdominal approaches. The laparoscopic group had significantly less morbidity and shorter hospital stays compared with the anterior approach, although there were no recurrences in either group. Yet others perform the repair with laparoscopic intraperitoneal onlay mesh, citing the importance of laparoscopy in the diagnosis and/or necessity for reduction and inspection of viability of incarcerated contents of Spigelian hernias.
Our unit has been performing SIL repair for virtually all inguinal and ventral (including parastomal) hernias since December 2009. We have shown in a prospective randomized setting (A Prospective Study Comparing Single and Multiport Laparoscopic Inguinal Hernia Repair [SILSTEP]; ClinicalTrials.gov identifier NCT01660048) that SIL inguinal hernia repair had significant benefits over conventional multiport repair in reducing postoperative pain and analgesic requirements and allowing earlier return to work or normal physical activities.20 We have further shown, in a prospective comparative study (A Prospective Study Comparing Telescopic vs. Balloon Dissection in Single Incision Laparoscopic Inguinal Herniorraphy [SILTELESCOPIC]; ClinicalTrials.gov identifier NCT01883115) comparing SILTEP with balloon dissection versus telescopic dissection that the latter was safe, efficient, and cost effective (unpublished results). In this study we have demonstrated the safety and efficacy of SILTEP repair with telescopic extraperitoneal dissection for Spigelian hernias that were either preoperatively diagnosed or incidental hernias. Telescopic extraperitoneal dissection saved us US$380 per case (which represents the cost of the balloon dissector) and allowed for and exposed 6 incidental Spigelian hernias (in 5 patients) from our cohort of 186 inguinal hernias in 131 patients. One interesting observation was that all Spigelian hernias were associated with direct (not indirect) inguinal hernia defects in this series. This probably makes anatomic sense, as the weakness in the Spigelian hernia belt would also extend more inferiorly along the lateral edge of the rectus as it inserts into the pubic tubercle, causing weakness and resultant direct inguinal hernia. Indeed, of the 8 Spigelian hernias treated with SILTEP repair, 5 were low-lying hernias, which were repaired with the same (albeit larger) mesh used for inguinal hernia repair. A review of our patient charts showed that there were 92 direct hernias from the entire cohort of 186 hernias. Therefore, the 8 Spigelian hernias (including 5 incidental) encountered in this series represent about 9% of all direct inguinal hernias, suggesting a high index of suspicion for the presence of incidental Spigelian hernias when a direct inguinal hernia is present. Furthermore, the 5 incidental Spigelian hernias were diagnosed only because the extraperitoneal space was dissected under direct vision during SILTEP repair. The low profile of the internal ring of the Triport system coupled with the fact that the dissection was initiated from the umbilical area posterior to the rectus muscle down as well as laterally. The latter dissection, in and around the Spigelian hernia belt, allowed exposure of Spigelian hernias, which would otherwise have been missed.
There are currently <1000 reported cases of Spigelian hernias, and most are small case series and case reports. Therefore, our experience with 8 cases over a 14-month period represents a significant contribution to the understanding of and treatment options for these relatively rare hernias. Furthermore, all 7 patients with Spigelian hernias also had concomitant inguinal hernias. This means that patients presenting with Spigelian hernias should be carefully checked for the presence of inguinal hernias. Indeed, 2 of the 7 patients who presented with Spigelian hernias alone were found to have clinical ipsilateral inguinal hernias that were subsequently confirmed and repaired at operation. This suggests that the same anatomic and pathologic processes may be involved in the formation of inguinal and Spigelian hernias. Of course, the laparoscopic extraperitoneal repair of Spigelian hernia would allow exploration of the inguinal region for unsuspecting inguinal hernias, which would not be possible with the conventional anterior repair.
Although high-volume hernia centers with dedicated hernia surgeons have confirmed the safety and efficacy of SILTEP repair,21,22 the paucity of available randomized controlled trials comparing single-port versus multiport totally extraperitoneal inguinal herniorrhaphy means that adoption of the former technique should, for now, remain at specialized centers, where the technique can undergo further scientific evaluation. However, its adoption and refinements, including telescopic extraperitoneal dissection, thus far, have resulted in some unexpected benefits, including cost savings.
CONCLUSIONS
SIL repair of inguinal hernias with telescopic extraperitoneal dissection allows the diagnosis of a significant number of incidental Spigelian hernias and results in the safe and efficient repair of both hernias. Dissection of the extraperitoneal space under direct vision resulted in significant cost savings compared with balloon dissection.
Contributor Information
Hanh Tran, Discipline of Surgery, Sydney Medical School, University of Sydney at Westmead Hospital, Westmead, Australia; Sydney Hernia Specialists Clinic, Sydney, Australia.
Kim Tran, Sydney Hernia Specialists Clinic, Sydney, Australia.
Marta Zajkowska, Sydney Hernia Specialists Clinic, Sydney, Australia.
Vincent Lam, Discipline of Surgery, Sydney Medical School, University of Sydney at Westmead Hospital, Westmead, Australia.
Wayne J. Hawthorne, Discipline of Surgery, Sydney Medical School, University of Sydney at Westmead Hospital, Westmead, Australia.
References:
- 1. Spangen L. Spigelian hernia. World J Surg. 1989;13(5):573–580. [DOI] [PubMed] [Google Scholar]
- 2. Klinkosch JT. Divisionem herniarum novamgue hernia ventralis proponit. Dissertationum Medicorum. 1764:184. [Google Scholar]
- 3. Read RC. Observations on the etiology of Spigelian hernia. Ann Surg. 1960;152:1004–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P. Spigelian hernia: surgical anatomy, embryology, and technique of repair. Am Surg. 2006;72(1):42–48. [PubMed] [Google Scholar]
- 5. Mathews FS. Hernia through the conjoined tendon. Ann Surg. 1923;78:300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nelson RL, Renigers SA, Nyhus LM, Sigel B, Spigos DG. Ultrasonography of the abdominal wall in the diagnosis of Spigelian hernia. Am Surg. 1980;46:373–376. [PubMed] [Google Scholar]
- 7. Balthazar EJ, Subramanyam BR, Megibow A. Spigelian hernia: CT and ultrasonography diagnosis. Gastrointest Radiol. 1984;9:81–84. [DOI] [PubMed] [Google Scholar]
- 8. Papierniak K, Wittenstein B, Bartizal JF, Wielgolewski JW, Love L. Diagnosis of Spigelian hernia by computed tomography. Arch Surg. 1983;118:109–110. [DOI] [PubMed] [Google Scholar]
- 9. Larson DW, Farley DR. Spigelian hernias: repair and outcome for 81 patients. World J Surg. 2002;26(10):1277–1281. [DOI] [PubMed] [Google Scholar]
- 10. Kavic MS. Abdominal wall hernia: the procedure. In: Kavic MS, ed. Laparoscopic Hernia Repair. Amsterdam, the Netherlands: Harwood Academic Publishers; 1997:83–94. [Google Scholar]
- 11. Tarnoff M, Rosen M, Brody F. Planned totally extraperitoneal laparoscopic Spigelian hernia repair. Surg Endosc. 2002;16(2):259. [DOI] [PubMed] [Google Scholar]
- 12. Peterko AC, Kirac I, Cugura JF, Bekavac-Beslin M. Single incision laparoscopic Spigelian hernia repair—an approach with standard instrumentarium. Acta Clin Croat. 2013;52(3):383–386. [PubMed] [Google Scholar]
- 13. Rath A, Bhatia P, Kalhan S, et al. Laparoscopic management of Spigelian hernias. Asian J Endosc Surg. 2013;6(3):253–256. [DOI] [PubMed] [Google Scholar]
- 14. Palanivelu C, Vijaykumar M, Kalpesh V, et al. Laparoscopic transabdominal preperitoneal repair of Spigelian hernia. JSLS. 2006;10(2):193–198. [PMC free article] [PubMed] [Google Scholar]
- 15. Chan JW, Chiu PW, Ng EK. Simultaneous laparoscopic totally extraperitoneal repair for concurrent ipsilateral Spigelian and indirect inguinal hernia. Surg Laparosc Endosc Percutan Tech. 2008;18(4):414–416. [DOI] [PubMed] [Google Scholar]
- 16. Koksal N, Altinli E, Celik A, Oner I. Extraperitoneal laparoscopic approach to Spigelian hernia combined with groin hernias. Surg Laparosc Endosc Percutan Tech. 2004;14(4):204–206. [DOI] [PubMed] [Google Scholar]
- 17. Appeltans BM, Zeebregts CJ, Cate Hoedemaker HO. Laparoscopic repair of a Spigelian hernia using an expanded polytetrafluoroethylene (ePTFE) mesh. Surg Endosc. 2000;14(12):1189. [DOI] [PubMed] [Google Scholar]
- 18. Barie PS, Thompson WA, Mack CA. Planned laparoscopic repair of a spigelian hernia using a composite prosthesis. J Laparoendosc Surg. 1994;4(5):359–363. [DOI] [PubMed] [Google Scholar]
- 19. Campanelli G, Pettinari D, Nicolosi FM, Avesani EC. Spigelian hernia. Hernia. 2005;9(1):3–5. [DOI] [PubMed] [Google Scholar]
- 20. Tsai YC, Ho CH, Tai HC, Chung SD, Chueh SC. Laparoendoscopic single-site versus conventional laparoscopic total extraperitoneal hernia repair: a prospective randomized clinical trial. Surg Endosc. 2013;27(12):4684–4692. [DOI] [PubMed] [Google Scholar]
- 21. Tran H, Turingan I, Tran K, Zajkowska M, Lam V, Hawthorne W. Potential benefits of single-port compared to multiport laparoscopic inguinal herniorraphy: a prospective randomized controlled study. Hernia. In press. [DOI] [PubMed] [Google Scholar]
- 22. Wijerathne S, Agarwal N, Ramzy A, Lomanto D. A prospective randomized controlled trial to compare single-port endo-laparoscopic surgery versus conventional TEP inguinal hernia repair. Surg Endosc. In press. [DOI] [PubMed] [Google Scholar]
- 23. Tran HM. Safety and efficacy of single incision laparoscopic surgery for total extraperitoneal inguinal hernia repair. JSLS. 2011;15(1):47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tran HM. Safety and efficacy of laparoendoscopic single-site surgery for abdominal wall hernias. JSLS. 2012;16(2):242–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Moreno-Egea A, Carrasco L, Girela E, Martín JG, Aguayo JL, Canteras M. Open vs laparoscopic repair of Spigelian hernia: a prospective randomized trial. Arch Surg. 2002;137(11):1266–1268. [DOI] [PubMed] [Google Scholar]