Abstract
Purpose
Differentiated thyroid cancer has a good prognosis and high incidence in young women. Since endoscopic techniques were first recorded in 1996, surgical indications of endoscopic thyroidectomy have broadened. Therefore, the aim of this study is to investigate the usefulness of endoscopic thyroidectomy in clinically lymph node negative (cN0) thyroid cancer patients, based on oncologic completeness and safety, considering cosmetic outcomes.
Methods
From July 2009 to June 2011, a total of 166 cases had undergone endoscopic thyroidectomy using the BABA (bilateral axillo-breast approach) method or conventional open thyroidectomy by one surgeon. Finally, excluding 72 patients, 94 patients with cN0 thyroid cancer were divided into two groups according to operative methods and analyzed to compare differences between the two methods retrospectively (endoscopic group, n = 49; conventional open group, n = 45).
Results
We practiced comparative analysis for clinicopathologic characteristics, surgical outcomes including postoperative complications, and recurred cases during follow-up periods of each group. The results showed there was a tendency for patients, young, women rather than men, and having small size of thyroid cancer, to prefer endoscopic surgery to open surgery. Meanwhile, in postoperative complications, there were no statistically significant differences. During short follow-up periods, no recurrence or mortality case was observed.
Conclusion
Endoscopic thyroidectomy is a feasible and safe method for the treatment of clinically lymph node negative (cN0) thyroid cancer.
Keywords: Endoscopic thyroidectomy, Lymph nodes, Thyroid neoplasms
INTRODUCTION
Thyroid cancer is the most common endocrine malignancy and has been considered a disease with excellent prognosis [1]. Papillary thyroid cancer (PTC) and follicular thyroid cancer (FTC) are differentiated thyroid cancers, which account for more than 90% of all thyroid malignances [2]. Especially, PTC is the most prevalent type as well as being relatively indolent and highly curable. The overall survival rate has remained at 90% to 95% in recent decades according to a SEER (surveillance, epidemiology, and end results) report [1,3].
In recent decades, the incidence of thyroid cancer has more than doubled in much of the developed world, including the United States and Canada. The incidence of PTC continues to increase in both men and women. Since the 1990s, thyroid cancer has become the fastest increasing cancer in women [4,5,6,7,8].
According to the 2002 Annual Report of the Korea Central Cancer Registry, the thyroid gland is the fourth most common cancer site among females and the incidence of thyroid cancer showed a continued increase in women. Classifying all cases under four groups by age, thyroid gland is the most common cancer among females and the fifth among male for the age group of 15-34, and the third among females for the age group of 35-64, and the ninth among females for the age group of 65 and over [9].
Thus, according to a desire for good cosmetic outcome among females with a continued increase of thyroid cancer with favorable prognosis, interest in oncoplastic surgery is increasing.
Recently, oncoplastic concept for treatment of thyroid cancer has been often mentioned where both complete surgical resection of the thyroid gland (including the tumor) and cosmetic outcome are pursued simultaneously [10]. By reason of cosmetic effect without postoperative neck scar, endoscopic or robotic surgery has been introduced in surgery of thyroid cancer [11,12,13,14,15], and has overcome a plethora of technical limitations, with the development of surgical instruments for endoscopic or robotic procedure. However, there is no consensus regarding the specific indications for this procedure of thyroid cancer. By many researchers, to date, this method has been applied to some select patients, including no clinical evidence of lateral lymph node (LN) metastasis and small size of thyroid cancer [13,14,15,16]. Most researches have shown that it is as safe as open surgery in terms of the completeness of the operation and postoperative complications but, according to surgical methods in clinically N0 thyroid cancer, there were few studies to compare surgical outcomes and recurrence rate.
Therefore, we have performed endoscopic thyroidectomy or conventional thyroidectomy according to patients' preference, in clinically LN negative thyroid cancer through preoperative examination and compared two groups through retrospective analysis for clinical features and surgical outcomes.
That is, our report compared one group undergoing endoscopic thyroidectomy with the other group undergoing open thyroidectomy in postoperative complications, pathologic results, serum thyroglobulin (Tg) levels before and after radioiodine (RI) therapy and recurrence by regulatory laboratory values, radiologic findings during follow-up periods. Based on analyzed results, we intend to propose the indication to apply endoscopic thyroidectomy.
METHODS
Patients
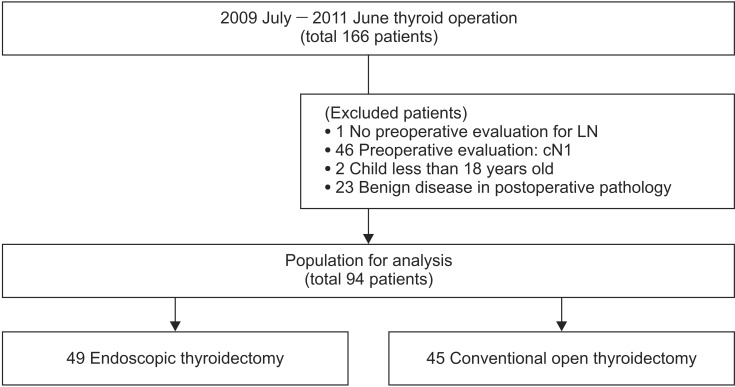
From July 2009 to June 2011, we performed analyses for a total of 166 patients undergoing thyroidectomy with or without central LN dissection whose thyroids were diagnosed as a malignancy by preoperative ultrasound (US)-guided fine needle aspiration and cytology (FNAC) or suspicious of malignancy by preoperative neck US, neck CT, PET-CT. Of those, 72 patients were excluded from this study; 46 patients were excluded with more than one clinically positive LN in preoperative evaluation, one with no preoperative evaluation for regional LNs, two less than 18 years old, and 23 diagnosed as benign neoplasm in postoperative pathology. Finally, 94 patients with thyroid cancer of clinically radiological node negative were adopted for analysis, classified under two groups. That is, we divided 94 patients into group A including 49 patients undergoing endoscopic surgery using BABA (bilateral axillo-breast approach) and group B including 45 patients undergoing conventional open thyroidectomy (Fig. 1) (endoscopic group, n = 49; open group, n = 45). In each group, all patients were analyzed for clinicopathologic characteristics, operative extents, operative time, postoperative complications, and the existence of recurrence during follow-up periods by various tests including off-T4 Tg levels. We applied 1 ng/mL as cutoff Tg level to suggest a postoperative recurrence.
Fig. 1.
Flow chart of accrued patients. LN, lymph node.
As postoperative complications, a criterion dividing a complication into transient injury or permanent injury was defined as six months, that is, transient complication was a case recovered from an injury within six months after operation and permanent complication was a case having a persisting injury over six months. For example, transient hypocalcemia was one case showing blood calcium levels below 8.0 mg/dL associated with clinical signs or symptoms from postoperative day 1 but recovering within 6 months after operation in clinical signs or symptoms and serum Ca levels. Permanent hypocalcemia was defined as persistent hypocalcemia for more than six months after operation, requiring calcium supplement, and recording low parathyroid hormone levels below the reference value (14 to 72 pg/mL).
All patients had undergone operation by one surgeon at one clinical center. One closed suction drain was placed into the operative bed via the edge of the open wound in conventional open surgery and the left axillary incision in endoscopic surgery during operation of all patients. When the volume drained became sufficiently low (below 30 mL/day), the inserted drain was removed and the patients were discharged.
All patients except 18 patients were regularly followed up by the treating surgeon or endocrinologists at one clinical center to date. Three patients among the excepted 18 patients were lost to follow-up after the first visit as a postoperative outpatient. Two patients among them were lost to follow-up between 6 months and 12 months postoperatively, 7 patients between postoperative months 12 and 24, and the other 6 patients between months 24 and 36. All excepted patients were followed up at other hospitals due to habitation problem or for RI therapy.
The mean follow-up period was 1,440.81 ± 31.84 days after endoscopic surgery and 1,447.73 ± 42.58 days after open surgery. All data were retrospectively analyzed.
Surgical methods
In this study, all patients for analysis experienced one of two surgical methods. That is, according to the approach method, patients were divided into group A receiving endoscopic thyroidectomy using BABA method without cervical incision and group B receiving conventional open thyroidectomy through a cervical incision.
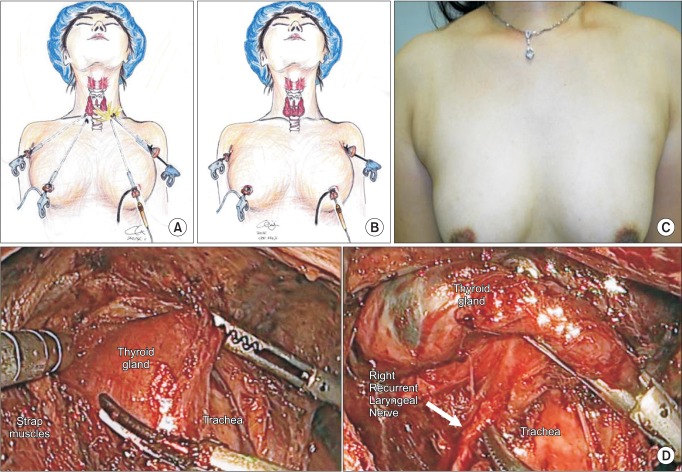
Conventional open surgery is the method of approaching the thyroid gland through a 5- to 6-cm incision line made along a transverse skin crease at 2-3 cm above the sternal notch. Thus, a postoperative neck scar is left, whereas endoscopic surgery is the method of approaching the lesion by using endoscopic instruments inserted through incision lines of about 10-, 20-mm length along right and left anterior axillary crease and about 10-mm length along upper areola line of bilateral breast (Fig. 2). Thus endoscopic surgery using BABA method has no neck scar and also no obviously observed scars. In the course of surgical excision, all subjects in each group were managed with the same method.
Fig. 2.
Endoscopic thyroidectomy using the BABA (bilateral axillo-breast approach) method; (A) intraoperative scope insertion, (B) actual surgical approach, (C) outcome at 2nd week postoperatively, and (D) intraoperative picture (anatomy).
Statistical analysis
Statistical analysis was performed with SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). Statistical differences between two groups were determined with the Student t-test and chi-square test or Fisher exact test for trend with a P-value <0.05 considered statistically significant.
RESULTS
Comparative analysis of clinicopathologic characteristics
This study performed comparative analyses between group A undergoing endoscopic surgery and group B undergoing conventional surgery in the patients with clinically N0 thyroid cancer.
First, in the clinical characteristics, group A was younger than group B in mean age (39.39 ± 8.9 years vs. 49.44 ± 12.3 years, P < 0.001). As for sex, men were predominantly chose the conventional method, whereas women somewhat preferred endoscopic surgery more than conventional surgery; the number of males undergoing conventional surgery was 9 out of a total of 11 (81.8%), the number of females undergoing endoscopic surgery was 47 out of a total of 83 (56.6%) (P = 0.023). These results showed statistically significant differences.
But, from the view-point of mean height and weight, there were no statistically significant differences between the two groups (160.9 ± 5.9 cm vs. 159.0 ± 7.8 cm, P = 0.062; 59.3 ± 9.5 kg vs. 61.9 ± 12.3 kg, P = 0.506). In operation time, group A was a little longer than group B but there was no statistically significant difference (183.4 ± 41.2 minutes vs. 156.2 ± 56.6 minutes, P = 0.798). In the length of hospitalization, group A was shorter than group B but there was no statistically significant difference (3.5 ± 1.6 days vs. 4.1 ± 2.1 days, P = 0.780).
In operative extent, all in the two groups had total thyroidectomy performed more than thyroid lobectomy (T: group A [33/49, 67.3%] vs. group B [40/45, 88.9%] and L: group A [16/49, 32.7%] vs. group B [5/45, 11.1%]) but, in cases of thyroid lobectomy a tendency to somewhat prefer endoscopic surgical method showed, whereas in cases of total thyroidectomy to there was a tendency to select further conventional surgical method (lobectomy in group A [16/21, 76.2%] vs. total thyroidectomy in group B [40/73, 54.8%], P = 0.012).
The mean tumor size was 0.80 ± 0.64 cm and 1.33 ± 1.26 cm in groups A and B, respectively, which showed statically significant difference (P = 0.013).
Cases of extrathyroidal extension were 11 cases in group A (22.45%) and 17 cases in group B (37.78%) but, those didn't show significant difference (P = 0.105). All cases presenting extrathyroidal extension were extensions limited to the perithyroidal soft tissues on pathology.
Although the number of mean retrieved central LN during surgery was less in group A than in group B (6.1 ± 5.8 vs. 16.7 ± 16.6, P < 0.001), the number of median metastatic LNs confirmed pathologically didn't show statistically significant difference (3 vs. 1.5, P = 0.866).
In the multiplicity of thyroid cancer and thyroiditis accompanied with thyroid cancer, there were no statistically significant differences between the two groups (Table 1).
Table 1.
Comparison of clinicopathologic characteristics between two groups
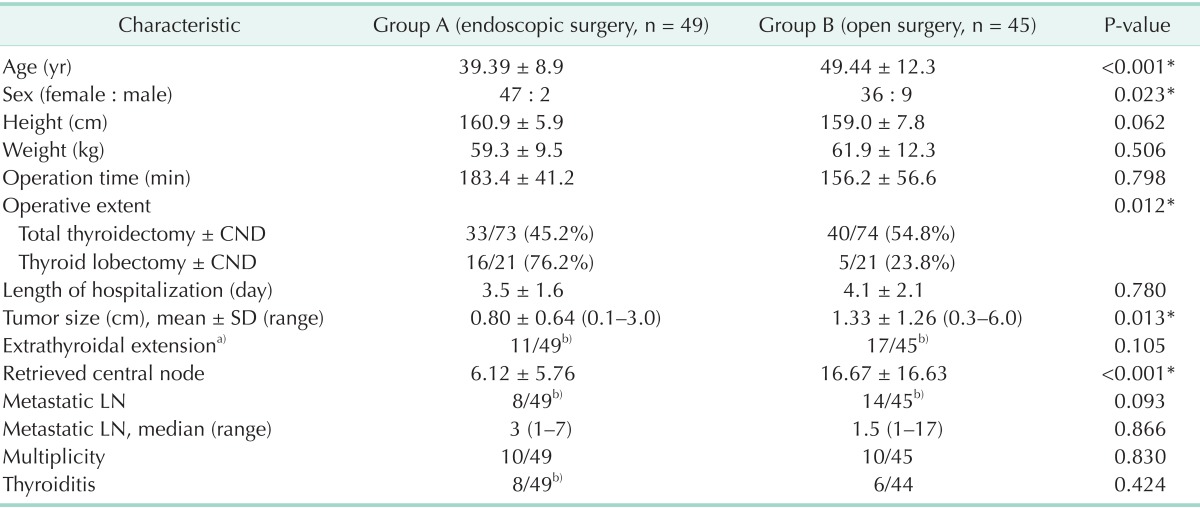
Values are presented as mean ± standard deviation (SD) unless otherwise indicated.
LN, lymph node; CND, central neck lymph node dissection.
a)Minimal extrathyroidal extension (limited to the perithyroidal soft tissues). b)The number of detected patient/the number of total patients.
*P < 0.05, statistically significance.
Postoperative complications
Transient hypocalcemia, permanent hypocalcemia, hoarse voice, bleeding, chyle leakage and infection were reported in some patients as postoperative complications. Meanwhile, esophageal or tracheal injury, and seroma hadn't been reported (Table 2).
Table 2.
Comparison of surgical outcomes between two groups
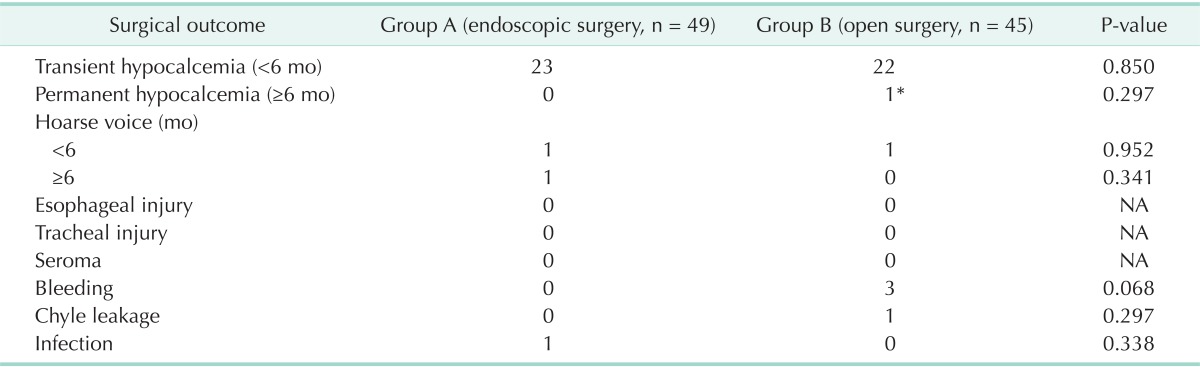
NA, not available.
*Serum PTH was 13.62 pg/mL, serum Ca was 7.1 mg/dL on the follow-up test at 9 months after operation and this patient was still taking Ca supplement then.
Twenty-three patients of group A and 22 patients of group B who underwent transient hypocalcemia recovered within six months and only one patient of group B showed permanent hypocalcemia but, there were no statistically significant differences (P = 0.850, P = 0.297, respectively).
One patient in group A and one patient in group B who experienced hoarse voice recovered within six months and one patient in group A experienced hoarse voice which persisted over six months but, there were no statistically significant differences (P = 0.952, P = 0.341, respectively). On the other hand, bleeding, chyle leakage and infection also were observed in the two groups but, there were no statistically significant differences.
Postoperative follow-up
During postoperative follow-up periods, recurrence was not found by regulatory laboratory values, radiologic imaging and nuclear medicine imaging or FNAC in suspicious cases. Before the first 131I therapy and after, a median value of serum levels of Tg measured had less than 1.0 ng/mL in both groups, which showed no statistically significant difference (Table 3). Increasing serum Tg levels were not observed during regular follow-up periods in both groups. In postoperative RI doses, there was no statistically significant difference between both groups (Table 3). And abnormal uptake on thyroidal RI uptake test also did not arise in both groups. Meanwhile, in 3 patients suspected by radiologic findings during postoperative follow-up periods, the results of FNAC were benign diseases such as reactive hyperplasia.
Table 3.
Comparison of postoperative oncologic completeness between two groups
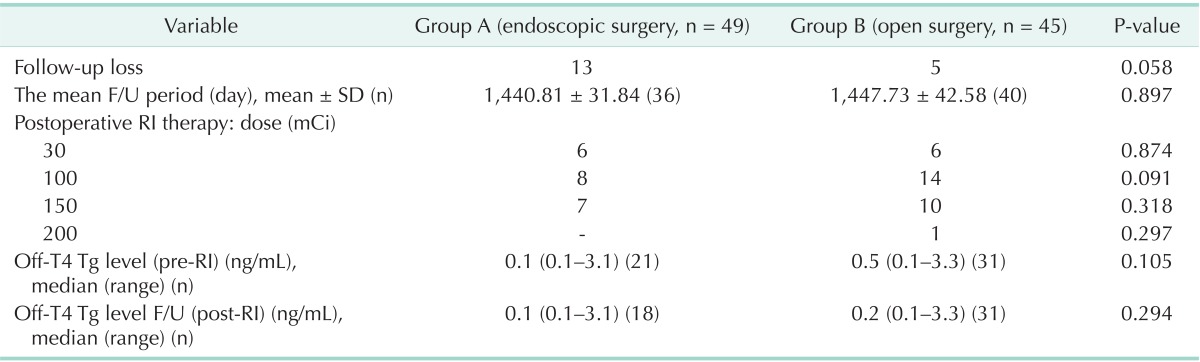
F/U, follow-up; SD, standard deviation; Tg, thyroglobulin; RI, radioiodine.
DISCUSSION
Thyroid cancer is the most common endocrine malignancy, and its incidence has increased considerably over the past few decades. Age-standardized incidence of thyroid cancer is estimated to be 9.1 per 100,000 females and 2.9 per 100,000 males in developed countries [2,17].
In histological types of thyroid cancer, PTC and FTC are differentiated thyroid cancers, which account for more than 90% of all thyroid malignances [2]. Fortunately, PTC is the most prevalent type and also relatively indolent and highly curable. The overall survival rate of patients is reported as >90%, particularly for patients younger than 45 years [18,19].
Although the incidence of thyroid surgery is increasing, the prognosis of thyroid cancer is favorable; accordingly, concern about postoperative neck scars in young women has increased [10]. In addition to oncologic completeness and surgical safety, surgical methods have developed to consider cosmetic effect without neck scar. Endoscopic or robotic surgery as approach methods have been a concern from many patients [13,14,15]. Many researchers have reported that these methods have been performed in PTC with small-size tumors (≤2 cm or solitary nodule under 30 mm its largest diameter or under 35 mm), intracapsular lesions, nonposterior locations, and no clinical evidence of lateral LN metastasis, no thyroiditis, and no previous neck irradiation or surgery as main indications [13,14,15,16,20,21,22].
But, distinct indications for endoscopic thyroidectomy have not been prescribed yet. Thus, the aim of this study is to propose cN0 as the only indication in various indications of endoscopic thyroidectomy for thyroid cancer patients, based on oncologic completeness and safety, considering cosmetic effects. Firstly, a total of 94 patients of PTC or FTC with clinically negative node were selected for analysis. Ninety-one in those were PTC and 3 were FTC. They had endoscopic surgery or conventional open surgery performed. According to the operative method, they were divided into two groups for comparative analysis. Clinicopathologic characteristics, postoperative complications and recurrence rates during follow-up periods were compared between the two groups. According to the results of the study, there were no statistically significant differences in operation time, length of hospitalization, extrathyroidal extension, median number of metastatic LN, multiplicity, or thyroiditis.
But, for sex, male patients known to have poor prognosis had predominantly conventional open surgery, whereas female patients preferred endoscopic surgery considering cosmetic effect to open surgery.
In size, endoscopic surgery had been applied to smaller size tumors more than open surgery (0.8 cm [range, 0.1-3.0 cm], 1.3 cm [0.3-6.0], respectively, P = 0.013), which showed significant difference. Here, in patients undergoing endoscopic operation, cases with more than 2-cm tumor size were three; 2 patients were confirmed as 2.8-, 3-cm PTC and the other was confirmed as 2.5-cm FTC on postoperative pathology. However, the maximum size observed in preoperative radiologic imaging was 3.5 cm on CT, 3.7 cm on US, and 3.5 cm on US, in respective cases of three patients mentioned above. As mentioned above, many researchers presented less than 2 cm or 3 cm, or 3.5 cm as its largest diameter as an indication for small size tumor to perform endoscopic operation. Although, in some of our cases, endoscopic surgery was performed for tumor sizes of 3 cm and under confirmed on pathology; its size was more than 3 cm on preoperative evaluation. As a surgical method is determined by a preoperative assessment, we think it yet hard to present a definite criterion on 'small size'. Therefore, we think to propose a limit on small tumor size for endoscopic surgery after comparing surgical outcomes of more patients with various tumor sizes in several centers, undergoing endoscopic or conventional open surgery.
Several patients presenting an extrathyroidal extension on postoperative pathology have been reported but there were no significant difference (22.45%, 37.78%, respectively, P = 0.105). All cases showing extrathyroid extension were cases limited to the perithyroidal soft tissues. Hence, it suggests that the existence of minimal extrathyroidal extension is no contraindication of endoscopic approach.
In the number of mean retrieved central LN, there was statistically significant difference (6.12 vs. 16.67, respectively, P < 0.001). However, in the median number of metastatic LN confirmed on pathologic reports, there was no significant difference (3 [range, 1-7] vs. 1.5 [range, 1-17], P = 0.866). Additionally, according to a study analyzing patients undergoing total thyroidectomy without the elective central compartment neck dissection in the cN0 central neck, the 10-year diseasespecific survival was 100% after a median follow-up of 70 months [23]. As well in our study, there was no recurrent case to the last follow up after a median follow up of 1,441 days in group A and 1,448 days in group B. Accordingly, it does not seem that the number of central LNs dissected prophylactically is important in an assessment of recurrence.
In mean operation time, a significant difference between the two groups was recorded but it seems to take a longer time to be operated on using endoscopic surgery or conventional open surgery at our center than other centers [13,14]. It may be, we think, that it is due to an operation practiced by one surgeon and short experience since first operation introduced at our center in 2009. Recently, the operative time of our center has been shortened about 30-60 minutes than recorded in this study, although not mentioned here.
Meanwhile, for postoperative complications, there were no statistically significant differences.
During the follow-up period, cases of recurrence or mortality in all patients of the two groups did not occur. That is, before and after 131I therapy, there was no significant difference in serum Tg level of the two groups. In doses of postoperative RI therapy, there was also no significant difference. Abnormal RI uptake didn't arise in both groups and the results of FNAC about suspected lesions were benign diseases.
Considering results mentioned above, we propose to perform endoscopic thyroidectomy in cases of clinical N0 thyroid cancer as the main indication. That is, in main indications presenting in several previous studies, we think that small size-under 30 mm or 35 mm, intracapsular lesion, thyroiditis, multiplicity need not to be considered.
Some studies have reported that the advantages of endoscopic over open surgery for thyroid diseases include reduced rates of hyperesthesia and paresthesia of the neck and highly improved cosmetic outcomes. However, endoscopic thyroidectomy with neck dissection has technical limitations due to the two-dimensional view and reduced dexterity of movement, particularly when operating on thyroid tumors and adjacent LNs. For these reasons, some have proposed a robotic approach to overcome these limitations and facilitate manipulations [11,12,16]. However, robotic surgery has been introduced and used in only some centers to date because of its expensive costs, whereas endoscopic surgery is a surgical method easier to approach in cost-effectiveness.
The present study does have a limitation. That is, this is a retrospective study performed by one surgeon at a single institute after a short term of follow-up period, and there were relatively few patients in the subject of the study. Thus, reassessment can be necessary for the efficacy of endoscopic thyroidectomy after continuous follow-up and analysis of more participants at more clinical centers.
In conclusion, endoscopic thyroidectomy using BABA method in cN0 thyroid cancer is as efficient as conventional open surgery in terms of the oncologic completeness, safety including postoperative complications, recurrence, and as a method showing excellent cosmetic outcomes. Therefore, we suggest cN0 as the only indication applying endoscopic thyroidectomy to thyroid cancer patients.
ACKNOWLEDGEMENTS
This study was supported by Konkuk University School of Medicine in 2014.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Yang L, Shen W, Sakamoto N. Population-based study evaluating and predicting the probability of death resulting from thyroid cancer and other causes among patients with thyroid cancer. J Clin Oncol. 2013;31:468–474. doi: 10.1200/JCO.2012.42.4457. [DOI] [PubMed] [Google Scholar]
- 2.Liu M, Ruan M, Chen L. Update on the molecular diagnosis and targeted therapy of thyroid cancer. Med Oncol. 2014;31:973. doi: 10.1007/s12032-014-0973-9. [DOI] [PubMed] [Google Scholar]
- 3.Barney BM, Hitchcock YJ, Sharma P, Shrieve DC, Tward JD. Overall and cause-specific survival for patients undergoing lobectomy, near-total, or total thyroidectomy for differentiated thyroid cancer. Head Neck. 2011;33:645–649. doi: 10.1002/hed.21504. [DOI] [PubMed] [Google Scholar]
- 4.Cramer JD, Fu P, Harth KC, Margevicius S, Wilhelm SM. Analysis of the rising incidence of thyroid cancer using the Surveillance, Epidemiology and End Results national cancer data registry. Surgery. 2010;148:1147–1152. doi: 10.1016/j.surg.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 5.Moon EK, Park HJ, Oh CM, Jung KW, Shin HY, Park BK, et al. Cancer incidence and survival among adolescents and young adults in Korea. PLoS One. 2014;9:e96088. doi: 10.1371/journal.pone.0096088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Horn-Ross PL, Lichtensztajn DY, Clarke CA, Dosiou C, Oakley-Girvan I, Reynolds P, et al. Continued rapid increase in thyroid cancer incidence in california: trends by patient, tumor, and neighborhood characteristics. Cancer Epidemiol Biomarkers Prev. 2014;23:1067–1079. doi: 10.1158/1055-9965.EPI-13-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vergamini LB, Frazier AL, Abrantes FL, Ribeiro KB, Rodriguez-Galindo C. Increase in the incidence of differentiated thyroid carcinoma in children, adolescents, and young adults: a population-based study. J Pediatr. 2014;164:1481–1485. doi: 10.1016/j.jpeds.2014.01.059. [DOI] [PubMed] [Google Scholar]
- 8.Shaw A, Semenciw R, Mery L. Cancer in Canada fact sheet series #1 - thyroid cancer in Canada. Chronic Dis Inj Can. 2014;34:64–68. [PubMed] [Google Scholar]
- 9.Shin HR, Jung KW, Won YJ, Park JG. 2002 annual report of the Korea Central Cancer Registry: based on registered data from 139 hospitals. Cancer Res Treat. 2004;36:103–114. doi: 10.4143/crt.2004.36.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee KE, Choi JY, Youn YK. Bilateral axillo-breast approach robotic thyroidectomy. Surg Laparosc Endosc Percutan Tech. 2011;21:230–236. doi: 10.1097/SLE.0b013e31822d0455. [DOI] [PubMed] [Google Scholar]
- 11.Aidan P, Pickburn H, Monpeyssen H, Boccara G. Indications for the gasless transaxillary robotic approach to thyroid surgery: experience of forty-seven procedures at the american hospital of paris. Eur Thyroid J. 2013;2:102–109. doi: 10.1159/000350854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee J, Chung WY. Robotic surgery for thyroid disease. Eur Thyroid J. 2013;2:93–101. doi: 10.1159/000350209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choi JY, Lee KE, Chung KW, Kim SW, Choe JH, Koo do H, et al. Endoscopic thyroidectomy via bilateral axillo-breast approach (BABA): review of 512 cases in a single institute. Surg Endosc. 2012;26:948–955. doi: 10.1007/s00464-011-1973-x. [DOI] [PubMed] [Google Scholar]
- 14.Chung YS, Choe JH, Kang KH, Kim SW, Chung KW, Park KS, et al. Endoscopic thyroidectomy for thyroid malignancies: comparison with conventional open thyroidectomy. World J Surg. 2007;31:2302–2306. doi: 10.1007/s00268-007-9117-0. [DOI] [PubMed] [Google Scholar]
- 15.Im HJ, Koo DH, Paeng JC, Lee KE, Chung YS, Lim I, et al. Evaluation of surgical completeness in endoscopic thyroidectomy compared with open thyroidectomy with regard to remnant ablation. Clin Nucl Med. 2012;37:148–151. doi: 10.1097/RLU.0b013e3182335fdc. [DOI] [PubMed] [Google Scholar]
- 16.Bae DS, Koo DH, Choi JY, Kim E, Lee KE, Youn YK. Current status of robotic thyroid surgery in South Korea: a web-based survey. World J Surg. 2014;38:2632–2639. doi: 10.1007/s00268-014-2606-z. [DOI] [PubMed] [Google Scholar]
- 17.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 18.Daliri M, Abbaszadegan MR, Bahar MM, Arabi A, Yadollahi M, Ghafari A, et al. The role of BRAF V600E mutation as a potential marker for prognostic stratification of papillary thyroid carcinoma: a long-term follow-up study. Endocr Res. 2014;39:189–193. doi: 10.3109/07435800.2013.879169. [DOI] [PubMed] [Google Scholar]
- 19.Hughes DT, Haymart MR, Miller BS, Gauger PG, Doherty GM. The most commonly occurring papillary thyroid cancer in the United States is now a microcarcinoma in a patient older than 45 years. Thyroid. 2011;21:231–236. doi: 10.1089/thy.2010.0137. [DOI] [PubMed] [Google Scholar]
- 20.Muenscher A, Dalchow C, Kutta H, Knecht R. The endoscopic approach to the neck: a review of the literature, and overview of the various techniques. Surg Endosc. 2011;25:1358–1363. doi: 10.1007/s00464-010-1452-9. [DOI] [PubMed] [Google Scholar]
- 21.Gal I, Solymosi T, Szabo Z, Balint A, Bolgar G. Minimally invasive video-assisted thyroidectomy and conventional thyroidectomy: a prospective randomized study. Surg Endosc. 2008;22:2445–2449. doi: 10.1007/s00464-008-9806-2. [DOI] [PubMed] [Google Scholar]
- 22.Piniek A, Schuhmann R, Coerper S. Minimally invasive video-assisted thyroidectomy: establishment in a thyroid center. Chirurg. 2014;85:246–252. doi: 10.1007/s00104-013-2624-7. [DOI] [PubMed] [Google Scholar]
- 23.Nixon IJ, Ganly I, Patel SG, Morris LG, Palmer FL, Thomas D, et al. Observation of clinically negative central compartment lymph nodes in papillary thyroid carcinoma. Surgery. 2013;154:1166–1172. doi: 10.1016/j.surg.2013.04.035. [DOI] [PubMed] [Google Scholar]