Abstract
Individuals with chronic pain often report using cigarettes to cope, and smoking and chronic pain appear prevalent among US veterans. Pain may be a barrier to cigarette cessation and abstinence in this population. Because of physiological effects, smoking cigarettes may also interfere with pain management. A better understanding of how cigarette use relates to pain may assist in veteran cigarette cessation and pain management efforts. To assist these efforts, we searched the literature using keywords, such as “pain,” “smoking,” and “veteran,” to identify 23 journal articles published from 1993 to 2013 that reported on studies examining pain and smoking variables among military or veteran populations. Studies found that veterans reported using cigarettes to cope with pain, there was greater occurrence of pain and disability among smokers in the military, and smoking increased the odds of veterans receiving an opioid prescription for pain and misusing opioids. Studies also found increased odds of pain and smoking among Veterans Health Administration patients with post-traumatic stress disorder when compared with those without post-traumatic stress disorder. Studies support an interaction between pain and smoking among veterans. However, the mechanisms underlying this relationship remain unclear. Future studies focused on this interaction would benefit veteran populations.
Keywords: cigarette smoking, pain, veterans
INTRODUCTION
Chronic pain (any pain lasting more than 12 weeks) and cigarette smoking are prevalent among US veterans (1–3), and individuals with chronic pain are frequently found to have higher odds of smoking than those without pain (4–6). Individuals with chronic pain report using cigarettes to cope, making pain a potential barrier to cigarette cessation and abstinence (6). A better understanding of how cigarette use relates to pain may assist in veteran cigarette cessation efforts. We reviewed studies that included cigarette use or cessation and chronic pain variables among veterans to determine the extent of associations between pain and smoking in this population and their possible links. We first provide context by exploring potential mechanisms linking smoking and pain. Although mechanisms beyond those discussed are possible (6), a full review of these is beyond the scope of this paper. Mechanisms discussed are those that appeared most salient to veteran literature. We also briefly discuss the biopsychosocial model in relation to pain and smoking, with references to more thorough discussions of this model in relation to pain research (7, 8). Finally, we examine the prevalence of cigarette smoking among veterans.
Smoking cigarettes to cope with pain
Individuals with chronic pain may use cigarettes to cope for different reasons. Cigarettes may distract from pain by providing a nonpain focal point (9), and individuals with chronic pain have reported using cigarettes this way (10). However, purposeful use of cigarettes to cope may contribute to increased smoking, as these smokers teach themselves to respond with a cigarette when they feel pain or pain-related stress (10).
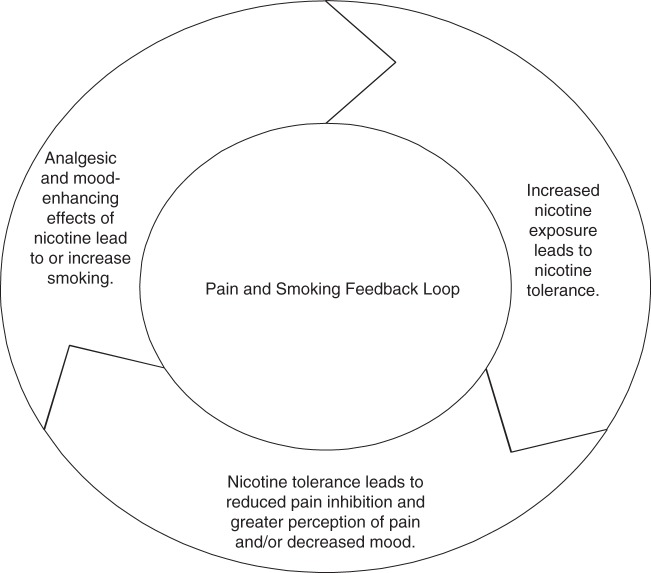
Nicotine may also provide an analgesic effect through release of neurotransmitters and activation of inhibitory pain pathways in the central nervous system (11, 12). Animal studies find reduced or delayed pain reactions in nicotine-exposed subjects (6). Human studies also find that pain increases smoking desire in some individuals (5, 13), and increased pain correlates with increased smoking (14). However, evidence also suggests that increased smoking increases pain. Studies find that smoking increases the odds of chronic pain onset and progression (15) and that, compared with nonsmokers, smokers have more severe pain (13, 16), worse treatment outcomes (17), increased opioid use (10), increased pain interference (16, 18), increased odds of suicidal ideation, or pain-related disability (17, 19). The discrepancy in findings that smoking may lead to decreased acute pain while simultaneously increasing long-term pain sensitivity led Ditre et al. (6) to propose a feedback loop, whereby recurrent nicotine exposure results in physiological dependence and tolerance or a need for increasing nicotine doses to stimulate similar effects, and nicotine tolerance then leads to reduced pain inhibition and greater pain perception (Figure 1). Over time, individuals must smoke more to achieve consistent levels of relief, and increased smoking contributes to or reinforces nicotine dependence and greater tolerance (6).
Figure 1.
Hypothesized associations between pain and smoking based on information provided by Ditre et al. (Psychol Bull. 2011;137(6):1065–1093) (6).
Finally, individuals with chronic pain have increased levels of poor mental health (20), and studies suggest that individuals with depression and anxiety might use cigarettes to cope with negative emotions (21). As with the pain feedback loop, continuing short-term cycles of withdrawal that occur throughout the day might increase mental health symptoms (6). A large body of research exists that explores cigarette use to regulate mood, and it appears that similar mechanisms are involved as those proposed for pain coping (21). The mental health literature suggests that the physiological effects of smoking on mood also vary on the basis of smoking duration (21). By a mechanism similar to the feedback loop of Ditre et al. (6), new smokers may feel the greatest relief from cigarettes, while long-term smokers may smoke more to maintain stasis (21).
Biopsychosocial model and pain
The biopsychosocial model offers a frame for understanding the complex interactions among biological, psychological, and social factors (7). It encompasses the physiological processes that occur when someone is exposed to stimulus, such as nerve activation or release of neurotransmitters (7, 8), the psychological effects of stimulus, such as pain perception or enjoying smoking, and social factors, such as the social views of people in pain or smoking (7, 8). If smoking relates to pain, their interaction is likely integrated into aspects described by this model. Interactions described by the biopsychosocial model may be unique for veterans because of their military experiences, the way civilians perceive them, and the culture of the Veterans Health Administration (its unique structure, mission, and service population) (22).
Cigarette smoking prevalence
A similar or greater proportion of veterans may smoke cigarettes compared with civilians (civilians, 18%–23%; male veterans, 23%–44%; and female veterans, 16.9%–34%) (3, 23–25). The reported proportions of cigarette-smoking veterans who use services from the Veterans Health Administration are also higher for female (25%–29%) but not male (approximately 19%–23%) veterans (26, 27). The smoking cessation needs of female Veterans Health Administration patients may be particularly relevant as female enrollment in the Veterans Health Administration has increased over 40% in the past decade (28). Additionally, Yoon et al. (29) compared Veterans Health Administration-sponsored inpatient, outpatient, and pharmacy utilization and cost data for female veterans from 2000 and 2008 and found a 139% increase in diagnosis of tobacco use disorder.
Potential mechanisms of pain–smoking interrelations with increased relevance to veteran populations
Veterans may experience greater impact of pain–smoking interrelations for multiple reasons. For example, military personnel who smoke may be more susceptible to injury as microtraumas that occur during athletic activity might heal more slowly than similar traumas among nonsmokers and compound over time (30). Although the effects of smoking on musculoskeletal pain and injury are not fully understood, smoking can contribute to bone demineralization, immune suppression, reduced cellular oxygenation, and delayed nutrient progression to injury sites, thus increasing injury risk as well as delaying healing (31). If smoking exacerbates musculoskeletal injury, the potential for a smoking–pain feedback loop is problematic, as smoking to deal with pain could worsen injury.
The effects of smoking on opioid processes are relevant to veterans, as a study found that 15.1% of 2,597 (6.9% female) recently returned combat soldiers reported past-month opioid use, with only 5.6% of them not reporting past-month pain (2). Prescription medications are used for pain management, and civilians with pain and an opioid prescription are more likely to smoke cigarettes than civilians with pain and no such prescription (32). Nicotine may provide an analgesic effect. However, the physiological process underlying this analgesia may impede opioid effectiveness among smokers who are experiencing pain, as demonstrated by hospitalized patients who smoke or once smoked and who, deprived of nicotine while in the hospital following surgery, appear to require increased doses of benzodiazepines than nonsmokers to obtain similar levels of pain relief (33). Veterans who smoke and experience pain may also require increased pain medication to experience relief.
Longitudinal data have shown increased nicotine dependence among young adults with a history of traumatic exposure (34). Veterans returning from Iraq and Afghanistan have a high prevalence of post-traumatic stress disorder (PTSD), particularly those who use services from the Veterans Health Administration (35). Veterans with poor mental health, such as PTSD, are also more likely than those with better mental health to report pain (36), and studies find that veterans with PTSD and depression are more likely to smoke cigarettes and have a greater number of health conditions than veterans without PTSD (37–40).
Benefits of quitting cigarettes
Cigarette smokers can benefit from quitting. The negative impact that smoking has on health and the health benefits of quitting are established (41). Although the use of cigarettes to cope with chronic pain is a potential barrier to cigarette cessation and abstinence (6), smokers with chronic pain may especially benefit from cigarette cessation. Cigarette cessation may reduce pain (6). Additionally, cigarette use exacerbates the health conditions that cause pain and may decrease the effectiveness of pain relief medications (42, 43).
Research agenda
Although 3 recent reviews explored the literature on pain and smoking (6, 19, 44), none focused on veterans. Interactions between smoking and pain may be more salient in this population. For example, veterans may be at increased risk for psychopathologies that underlie pain–smoking relationships. Better knowledge of how pain and smoking relate in this population could assist in pain management and smoking cessation efforts for them. To assist these efforts, we identified and reviewed studies that included smoking and pain among veterans and military personnel.
METHODS
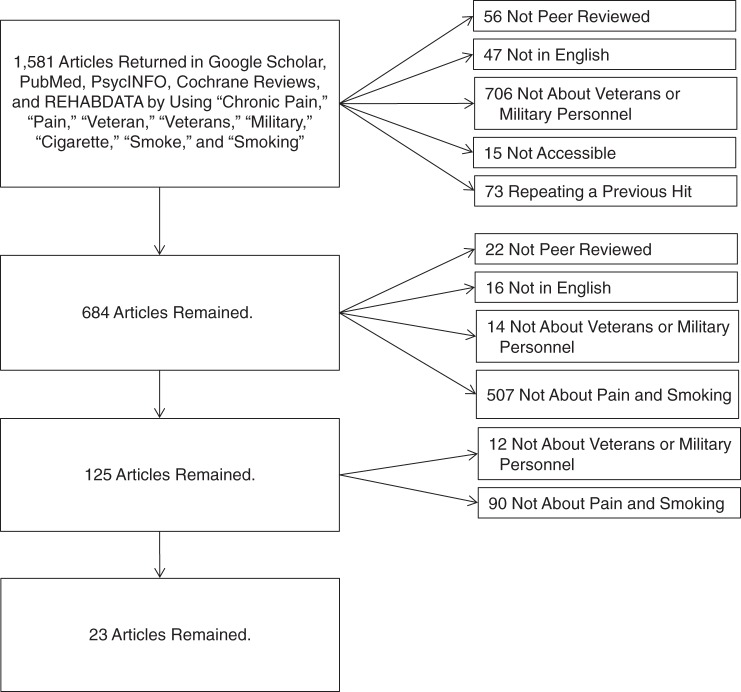
We searched for literature beginning in December 2013 through July 2014. Although we initially tried limiting searches in multiple ways, such as including only veterans, we found such a small number of results that we removed the limits to identify more articles. The final search had no article date or study population age limits but was limited to peer-reviewed articles published in English. During article title, abstract, and text review, articles were excluded that did not explore pain (defined as a physical feeling that results from disease, injury, or something that hurts the body), and articles were included that had a measure of pain (quality-of-life subscale measures, self-reported pain) or painful injury (musculoskeletal injury) and cigarette smoking among veterans or military personnel (defined as men and women who either had served or were serving in any branch of the US Armed Forces). We used different combinations and orderings of key words in each database, attempting to find the most articles possible. Key words included “chronic pain” and “pain” (to identify studies that included pain), “veteran” and “veterans” (to identify studies of veteran populations), “military” (to expand results to include studies of military personnel), and “cigarette,” “smoke,” and “smoking” (to identify articles that focused on cigarette smoking). Inclusion criteria and the elimination process are further described in Figure 2.
Figure 2.
Summary of literature search and inclusion.
We searched PubMed to explore the medical literature and identified 3 articles. We searched PsycINFO to explore psychological studies and identified 1 article. We searched Google Scholar to explore a broad range of literature and identified 19 articles. Comparing PubMed with Google Scholar, Bramer et al. (45) found that Google Scholar identified more articles than PubMed. In a similar comparison, Nourbakhsh et al. (46) also found that articles identified by Google Scholar came from higher ranked journals. Google Scholar is limited because it returns a large number of unrelated articles, its search tool lacks sophistication, and it does not list more than 1,000 hits, even when it indicates identifying more than 1,000. Additionally, Google Scholar changes its functionality and coverage, and the same search query returns different results at different times (45). Even with these limitations, we chose to search Google Scholar to identify as many articles on our subject as possible, considered acceptable as long as Google Scholar is not the only database used (45, 46). We also searched Cochrane Reviews (health and health policy literature) and REHABDATA (rehabilitation studies) but identified no new articles with them. Exclusion left 23 articles (Table 1).
Table 1.
Identified Studies That Included Pain and Cigarette Smoking Variables in Studies of Veteran or Military Populations
| First Author, Year (Reference No.) | Sample Size, No. | Population | % Female | Location | Data Collection Method | Study Type | Pain Type | Smoking Onset | Findings |
|---|---|---|---|---|---|---|---|---|---|
| Aversa, 2013 (66) | 943 | Cigarette-smoking veterans with PTSD | 6 | Archival data from VA hospital patients | Postlongitudinal (12 months) | Pain measures on health-related quality-of-life surveys | Not reported | Participants smoked just over 1 pack a day with a mean of 21.7 cigarettes (SD, 10.5); the pretreatment physical component score was 38.02 (SD, 10.6), physical functioning score was 52.02 (SD, 28.5), and bodily pain score was 42.70 (SD, 24.5); prolonged abstinence was associated with higher general health scores; improved numbing symptoms correlated with improved bodily pain scores. | |
| Rabadi, 2013 (58) | 170 (4% female) veterans | Veterans | 4 | Oklahoma City, OK | Survey | Cross-sectional | HRQoL | Not reported | 31% extreme pain or discomfort. While smoking habits are known to cumulatively impact the HRQoL, these variables were not associated with health state or HRQoL on the basis of the EQ-5D questionnaire in this sample of veterans. |
| Dodge, 2013 (12) | 153 | VA patients | 23 | Cincinnati VAMC, OH | Patient records | Prospective cohort | PDPH | Prior to injury | 5 (<1%) females and 45 (15.6%) males used cigarettes; cigarette smokers had a lower incidence of PDPH than did nonsmokers (13.7% vs. 34.1%, respectively; P = 0.009). Tobacco use was the only explanatory variable to survive a backward elimination stepwise process (other variables were diagnosis, race, sex, BMI, and age group). |
| Jeffery, 2013 (63) | 28,546 | Military personnel | 14.2 | Department of Defense Survey of Health-Related Behaviors | Cross-sectional | Prescription drug misuse | Current, former, never | The strongest predictor of reported pain reliever misuse was having received a pain reliever prescription previously (past-month AOR = 2.56, 95% CI: 2.23, 2.94; past-year AOR = 2.51, 95% CI: 2.25, 2.81). An interaction between former smoking and alcohol consumption negligibly decreased use of prescription drugs (statistics not reported). | |
| Dobscha, 2013 (60) | 5.961 | Veterans | 10 | Pacific Northwest | Clinical data | Longitudinal (12 months) | Opioid prescription | Nicotine dependence | 35% of the sample received an opioid prescription; 5% received COT. Veterans prescribed COT were younger and had greater pain intensity and high rates of psychiatric and substance use disorders compared with veterans in the other 2 groups; among patients receiving COT, 29% were prescribed long-acting opioids; adjustments for age, sex, baseline pain intensity, and major depression (OR = 1.24, 95% CI: 1.10, 1.39; OR = 1.48, 95% CI: 1.14, 1.93), and nicotine dependence (OR = 1.34, 95% CI: 1.17, 1.53; OR = 2.02, 95% CI: 1.53, 2.67) were associated with receiving any opioid prescription and with COT, respectively. |
| George, 2012 (49) | 1,230 | Military personnel | 30.4 | Participants had completed training at Fort Sam Houston in San Antonio, TX | In person questionnaire, Internet, and telephone | Longitudinal (2 years) | Lower back pain | Smoking prior to service | 42.1% reported lower back pain. Characteristics positively correlated with lower back pain included being female, active duty, Beck Depression Inventory, Fear and Pain Questionnaire, physical component score, mental component score, and profiled. Multivariate analysis results: being male (AOR = 0.644, 95% CI: 0.49, 0.846), active duty (AOR = 1.441, 95% CI: 1.094, 1.899), physical component score (AOR = 0.96, 95% CI: 0.935, 0.987), and mental component score (AOR = 0.964, 95% CI: 0.943, 0.985). |
| Aversa, 2012 (65) | 943 | Cigarette smoking veterans with PTSD | 6 | Archival data from VA hospital patients | Postlongitudinal (12 months) | Pain measures on health-related quality of life surveys | Not reported | Scores indicated diagnostic levels of PTSD within the sample with a mean of 59.2, (SD, 12.0), clinically severe symptoms with a mean of 75.2 (SD, 18.5), and an average level of moderate depression with a mean of 16.0 (SD, 6.9); SF-36 scores indicated a poor health-related quality of life, and those who reported fewer depressive symptoms reported better health-related quality of life when controlling for PTSD symptom severity and long-term cigarette abstinence. | |
| Patterson, 2012 (47) | 151 | VA patients | 7.9 | Urban VA clinic in the United States | Survey and clinical data | Cross-sectional | Smoking to cope with pain | Current smoking | 49.4% reported smoking to cope. Those who smoked to cope reported greater pain intensity, poorer pain-related function, and worse fear of pain than did nonsmokers and smokers not using cigarettes to cope. Veterans using cigarettes to cope had better relaxation and coping scores. |
| Childs, 2011 (51) | 4,325 | Military personnel | 29 | Fort Sam Houston, San Antonio, TX | In-person questionnaire, Internet, and telephone | Secondary analysis of clinical trial data | Lower back pain | In multivariate analysis (generalized linear mixed model), covariates associated with increased pain included age (AOR = 1.05, 95% CI: 1.02, 1.07) and smoked cigarettes prior to service (vs. not smoked) (AOR = 1.69, 95% CI: 1.41, 2.03). Covariates associated with decreased pain included black race (vs. white race) (AOR = 0.76, 95% CI: 0.57, 0.99), high school or less (vs. college graduate) (AOR = 0.54, 95% CI: 0.40, 0.71), some college (vs. graduated from college) (AOR = 0.70, 95% CI: 0.54, 0.91), active duty (vs. reserved) (AOR = 0.68, 95% CI: 0.56, 0.81), and no physical exam (vs. an exam) (AOR = 0.70, 95% CI: 0.54, 0.90). BMI was marginally significant (AOR = 0.97, 95% CI: 0.94, 1.00) (P = 0.027). | |
| Macey, 2011 (61) | 762 | OEF/OIF veterans | 15 | Pacific Northwest | Clinical data (Veterans Integrated Service Network-20) | Longitudinal (12 months) | Opioid prescription | Nicotine dependence | Veterans with PTSD (OR = 1.42, 95% CI: 1.04, 1.96) and nicotine use disorder (OR = 2.14, 95% CI: 1.41, 3.27) were more likely to receive opioid prescriptions than those without these disorders. |
| Morasco, 2010 (62) | 1,478 | VA patients | 9.3 | Pacific Northwest | Clinical data (Veterans Integrated Service Network-20) | Longitudinal (12 months) | Opioid prescription | Nicotine dependence | Those with nicotine dependence were marginally more likely to have a high-dose opioid prescription (AOR = 1.36, 95% CI: 1.00, 1.86) as were those with neuropathy (AOR = 1.95, 95% CI: 1.28, 2.97) and lower back pain (AOR = 1.88, 95% CI: 1.32, 2.70). |
| Woodruff, 2010 (53) | 5,503 followed from March 1996 to March 1997 to June 2005 | Navy recruits | 100 | Smoking survey and career history archival medical and personnel system | Longitudinal cohort | Musculoskeletal injury | Smoking status assessed prior to receipt of medical services but not reassessed for changes | Over the course of the study, pregnancy, mental disorders, genitourinary system conditions, digestive system conditions, and poisoning/injuries were the most common reasons for hospitalization. Daily smokers had a rate of 116.7 per 1,000 person-years for any-cause hospitalization compared with ∼101 and 105 per 1,000 person-years for other and never smokers. Daily smokers’ hospitalization rate for musculoskeletal conditions was 5.0 per 1,000 person-years. The average number of days hospitalized was longer for daily smokers than for never and other smokers by about half a day. | |
| Becker, 2009 (64) | 6,377 | Veterans referred from primary care | 9.3 | Referred from Philadelphia, PA, and VA or satellite clinics | Telephone survey | Cross-sectional | Prescription drug misuse | Current smoking | 36.7% of participants reported current smoking. Positive bivariate correlates of prescription drug misuse included younger age, possible depression (OR = 1.9, 95% CI: 1.3, 2.8), probable depression (OR = 2.4, 95% CI: 1.6, 3.4), smoking (OR= 1.4, 95% CI: 1.1, 1.8), illicit drug use (OR = 2.8, 95% CI: 2.2, 3.7), and chronic pain (OR = 1.9, 95% CI: 1.4, 2.5). Multivariate correlates of frequent drug misuse included younger age, strained financial situation (OR = 1.5, 95% CI: 1.01, 2.1), smoking (OR = 1.8, 95% CI: 1.3, 2.7), illicit drug use (OR = 3.4, 95% CI: 2.3, 5.0), and chronic pain (OR = 1.6, 95% CI: 1.1, 2.4). |
| Silberbogen, 2007 (55) | 38 seen from December 2005 through April 2006 | VA patients | 16 | VA clinics in Hines, IL, and Boston, MA | Survey | Cross-sectional | Hepatitis C | Current smoking | 82.7% of hepatitis C-diagnosed participants also reported pain symptoms; 30% reported pain duration of 5 years or more, 35% reported 1–5 years, and 35% reported 1 year or less; 45.8% had consumed alcohol in the past year; 28% of participants with HCV and pain reported that they did not have anyone to help them with daily tasks, and 25% did not feel they had anyone they could rely on for emotional support. |
| Yoo, 2008 (56) | 112 | VA patients | 2.7 | West Haven VAMC, CT | Patient records | Retrospective cohort | Diverticulitis | Smoked prior to condition | Significant smoking history: >30 pack-years was present in 70.5% of patients; a larger number of smokers (n = 41) required colectomy compared with nonsmokers (n = 35) (marginally significant at P = 0.06). Patients were more likely to undergo colectomy if they had comorbid chronic obstructive pulmonary disorder. |
| Ouimette, 2004 (68) | 134 | VA patients | 16.1 | General medical and women's health clinics at the VAMC in Palo Alto and Menlo Park, CA | Survey | Cross-sectional | Pain measures on health-related quality-of-life surveys | Not reported | Thirty-three participants (25%) met criteria for PTSD; compared with men, women had poorer physical health-related quality of life on 2 subscales (role limitations due to physical health and general health), and women more often had poorer general health. Compared with women, men more often had a circulatory diagnosis; PTSD patients were younger; the interaction between energy/fatigue and PTSD symptom severity was significant, and it was stronger among men (β = −0.62, P < 0.001, R2 change = 0.27) than women (β = −0.25, P < 0.05, R2 change = 0.04). |
| Dobi, 2004 (69) | 1,935 | VA patients | 100 | Puget Sound, WA | Mailed survey | Cross-sectional | Health history including multiple kinds of pain (e.g., back pain, stomach pain) | Not reported | 21% screened positive for PTSD. Those who screened positive for current PTSD (21%) were more likely than those who did not to report fibromyalgia (19.2% vs. 8.0%, respectively), irritable bowel syndrome (37% vs. 17.9%), and chronic pelvic pain (33.5% vs. 14.4%). The odds of smoking cigarettes were higher among those with PTSD symptoms than those without (OR = 2.04, 95% CI: 1.52, 2.75). They were also significantly more likely to endorse other physical health problems including obesity, polycystic ovary disease, asthma, cervical cancer, and stroke. Women who screened positive for PTSD also endorsed higher levels of somatic distress and were more likely to screen positive for depression, eating disorders, and panic disorder. |
| Lincoln, 2003 (31) | 15,120 | Army personnel | 15 | Across the United States | Total Army Injury and Health Outcomes Database | Retrospective cohort | Musculoskeletal disorders | Not reported | Excess fraction due to smoking among subjects with meniscal injuries who currently smoke was 38%. Disability was significantly associated with heavy smoking among all subjects (relative hazard = 1.21). Both heavy smokers (relative hazard = 1.49) and light-to-moderate smokers (relative hazard = 1.44) were at greater risk for disability following meniscal injuries. For all musculoskeletal diagnoses combined, heavy smokers had the highest cumulative risk of disability (17.6%), followed by light-to-moderate smokers (15.8%), nonsmokers (12.2%), and then former smokers (10.3%), suggesting a dose-response relationship (P < 0.001). |
| Voelker, 2002 (57) | 3,695 | Gulf War veterans | 0.09 | Across the United States | Iowa Gulf War Study | Combined cross-sectional/cohort design | Health-related quality of life | Current, former, never | High prevalence of current smoking (45% Gulf War deployed and 48% not Gulf War deployed). Nondeployed participants reported excellent health more often than did deployed participants (31% vs. 21%, P < 0.01). Smoking was an independent risk factor for poorer health after deployment (compared with never smokers, decrease in mean score of 2.5 (SD, 0.4)). |
| Barrett, 2002 (39) | 3,682 | Gulf War veterans and control subjects | 9 | Across the United States | Population survey | Cross-sectional | Health status | Current, former, never | Current smokers were almost 4 times more likely to screen positive for PTSD than never smokers (AOR = 3.83, 95% CI: 1.40, 10.46). Those who screened positive for PTSD had a greater number of health conditions than did those who did not screen positive (PTSD mean medical conditions = 10.18 vs. no PTSD mean medical conditions = 1.73 medical conditions). |
| The number of physical symptoms positively correlated with PTSD severity (r = 0.60, P < 0.001). Similarly, a positive relationship was found between the number of medical conditions reported and PTSD severity (r = 0.50, P < 0.0001). | |||||||||
| Altarac, 2000 (30) | 2,002 | Basic training recruits | 46 | Fort Jackson, SC | Survey and physical analysis | Longitudinal (8-week period) | Injury | Smoking prior to enlistment | Smoking was common in this population, with 42% of men and 40% of women reporting smoking at least 1 cigarette in the prior year. Recruits who reported smoking at least 1 cigarette in the month prior to beginning basic training (conducted in a smoke-free environment) had significantly higher injury rates during training than those who did not report smoking (40% vs. 29% for men, and 56% vs. 46% for women). |
| Schnurr, 1999 (67) | 921 | VA patients | 0 | Boston VA, MA | Normative Aging Study | Cross-sectional | Physical component summary score | Not reported in relation to onset of pain | Combat exposure was related to pain (P < 0.05). Smoking was related to pain, vitality, mental health (P < 0.05), and vitality (P < 0.001). PTSD related to all scales (physical functioning, role-physical, pain, general health perceptions, vitality. Combat exposure was positively related to current smoking and PTSD symptoms. Current smoking and PTSD symptoms correlated with decreased health. |
| O'Connor, 1993 (52) | 160 | Military personnel | 0 | Basic training recruits | Survey questionnaire | Longitudinal (8-week period) | Lower back pain (new onset) | Smoking prior to enlistment | Cigarette smokers were more likely to experience lower back pain. Cigarette smoking was the only variable significantly associated with back pain. |
Abbreviations: AOR, adjusted odds ratio; BMI, body mass index; CI, confidence interval; COT, chronic opioid therapy; EQ-5D, 5-dimensional measure of health status from the EuroQol Group (Rotterdam, the Netherlands); HCV, hepatitis C virus; HRQol, health-related quality of life; OEF, Operation Enduring Freedom; OIF, Operation Iraqi Freedom; OR, odds ratio; PDPH, post-dural puncture headache; PTSD, post-traumatic stress disorder; SD, standard deviation; SF-36, 36-item Short Form Health Survey; VA, Veterans Health Administration; VAMC, Veterans Affairs Medical Center.
RESULTS
Smoking cigarettes to cope with pain
Only 1 identified study queried participants about their use of cigarettes to cope with pain. Patterson et al. (47) examined smoking among 151 (7.9% female) chronic pain patients seen at an urban Veterans Health Administration clinic during an undisclosed period and found that 49.4% reported smoking to cope. Those who smoked to cope reported greater pain intensity, poorer pain-related function, and worse fear of pain than did nonsmokers and smokers not using cigarettes to cope. However, veterans using cigarettes to cope had better relaxation and coping scores. Because nicotine dependence, depression and anxiety, and opioid-use measures were similar among groups, Patterson et al. (47) eliminated underlying nicotine dependence, depression, and attenuation of opioid analgesia as reasons for worse pain outcomes in the smoking-to-cope group. Instead, Patterson et al. (47) suggested that using cigarettes to cope might result in delayed mood or symptom severity change, thus providing a pain-stabilizing effect (48). Patterson et al. (47) further suggested that, as an active and purposeful coping mechanism, smoking might enhance mood by decreasing pain-related anxiety. If veterans use cigarettes to stabilize pain or enhance mood, increasing levels of nicotine may be necessary to maintain the same effect over time (6, 21). Alternatively, veterans who smoke to cope may simply be more aware of pain (47), which could result in their training themselves to smoke each time they reach their pain threshold. Either way, veterans who smoke to cope may have greater cigarette dependence. Studies of large data sets that include additional variables, such as when individuals began smoking and experiencing pain, are needed to explore potential mechanisms.
Musculoskeletal and lower back pain
We have identified 4 studies that examined cigarette use in relation to musculoskeletal pain or injury among military personnel. One study explored cigarette smoking in relation to short- and long-term lower back pain. Among 1,230 (30.4% female) soldiers followed from induction to basic training through 2 years after, George et al. (49) found that a multivariate model including gender, smoking status, and previous injury predicted higher disability scores (R2 = 6.2%, P value not reported). Although the authors did not report odds ratios for each variable, they reported that soldiers who smoked prior to service scored an average of 2.7 points higher when compared with those who did not smoke. The Oswestry Disability Questionnaire is an established, effective measure of disability in individuals with back pain that is made up of 10 questions scored 0–5, with 0 reflecting mild intermittent pain and 5 reflecting constant severe pain (50). A patient's score is summed, divided by 50, and reported as a percentage.
Two studies examined the occurrence of lower back pain among recruits. Childs et al. (51) analyzed data collected from 4,325 (29% female) US Army recruits during their first 16 weeks of training and found that increased age (adjusted odds ratio (AOR) = 1.05, 95% confidence interval (CI): 1.02, 1.07) and cigarette smoking prior to service (vs. not smoking) (AOR = 1.69, 95% CI: 1.41, 2.03) increased the likelihood of pain. In a similar study, O'Connor and Marlowe (52) examined the onset of lower back pain among 160 male US Army recruits before and after basic training; the only variable significantly associated with pain was cigarette smoking before enlistment (63.0% vs. 38.3%) (P = 0.02). In a study looking at injury and not pain, Altarac et al. (30) explored data from 2,002 (46% female) US Army recruits and found that those who smoked before basic training had increased odds of musculoskeletal injury (traumatic and overuse) when compared with those who did not smoke (any injury: male AOR = 1.48, 95% CI: 1.11, 1.98; female AOR = 1.61, 95% CI: 1.19, 2.17). Together, findings suggest the potential for increased pain and injury among recruits who smoked cigarettes prior to service.
We have identified 1 study that examined disability. Lincoln et al. (31) analyzed data for 15,120 (15% female) US Army personnel diagnosed with a musculoskeletal injury from 1989 to 1996 and followed through 1997 in the Total Army Injury and Health Outcomes Database and found that 9.5% received a disability status (1.1% permanent, 7.4% lump sum severance, 1.0% temporary). Smoking status was based on initial survey responses. Heavy smokers (13%) had the highest 5-year cumulative risk for disability (risk hazard = 1.21, 95% CI: 1.04, 1.42), followed by light-to-moderate smokers (18%), former smokers (17%), and nonsmokers. The finding of increased disability with increased smoking was greatest for individuals with meniscal injuries (risk hazard = 1.49, 95% CI: 1.06, 2.11; light-to-moderate smoking risk hazard = 1.44, 95% CI: 1.07, 1.94). When meniscal injuries were removed from analysis, the trend of increasing disability with increased smoking lost significance. Findings suggest that smoking increases the potential for long-term dysfunction, and they suggest that injured smokers could benefit from learning the ways smoking impedes healing.
Only one study identified by this review explored a potential relationship between cigarettes and musculoskeletal injury specifically among females. Woodruff et al. (53) examined Career History Archival Medical and Personnel System data (records to June 2005) from 5,503 female US Navy personnel initially asked their cigarette smoking status at recruitment (March 1996–March 1997) and found that never (45%) and nondaily (28% smoked sometimes but not daily) smokers had a lower relative risk of any cause (relative risk = 0.90, 95% CI: 0.81, 0.99 and relative risk = 0.87, 95% CI: 0.78, 0.96, respectively) and musculoskeletal (relative risk = 0.35, 95% CI: 0.19, 0.63 and relative risk = 0.34, 95% CI: 0.18, 0.66, respectively) hospitalizations than did daily smokers (27%). The hospitalization rate for musculoskeletal conditions was also higher for daily smokers (5.0 per 1,000 person-years) than for never or nondaily smokers (1.7 per 1,000 person-years). Smokers and nonsmokers may have the same incidence of injury in this study, with smoking increasing hospitalization (53). Case-control studies could address this possibility.
In summary, studies examining musculoskeletal and lower back pain among military personnel found greater occurrence of pain and increased disability among smokers. These data support the suggestion that the physical effects of smoking increase pain and injury potential. Injured smokers may benefit from additional cessation support including education on the potential effects of smoking on healing.
Headache pain
One identified study examined cigarette smoking and post-dural puncture headache (PDPH) pain among veterans. PDPH occurs when one of the meninges surrounding the brain and spinal cord is punctured during a medical procedure, such as during administration of spinal anesthesia. It presents within hours to days and is characterized by complaints of headache and nausea (54). Dodge et al. (12) compared the occurrence of PDPH between 153 (23% female) cigarette smoking and nonsmoking veterans who presented at an Ohio Veterans Health Administration clinic for cerebral spinal fluid sampling during an undisclosed period and found that nonsmokers had greater odds of developing PDPH (AOR = 3.1, 95% CI: 1.3, 8.1) than did smokers. Overall, PDPH is thought to occur when fluid leaks from the puncture site. Dodge et al. (12) suggested that smoking might reduce PDPH because of denser clotting in smokers. Alternatively, nicotine-related analgesia could reduce perceived pain. The conversion of nicotine-stimulated dopamine to norepinephrine, a vasoconstrictor, could also reduce leakage (12). Although PDPH is often acute, some patients experience long-term pain, and longitudinal data are needed to understand how smoking may relate to pain duration.
Hepatitis C
Pain and cigarette smoking may also relate to one another among veterans with hepatitis C virus (HCV) infection. Silberbogen et al. (55) examined self-reported pain and health behaviors among 38 (16% female) veterans aged 41–60 years who self-reported HCV and were seen at Veterans Health Administration clinics in Illinois and Massachusetts from March 2005 to April 2006 and found that 82.7% of participants with an HCV diagnosis (76.3%) reported pain. The shoulder/arm/hand (70.8%), hip/leg/foot (58.3%), and lower back (54.2%) were the most common pain sites; participants with an HCV diagnosis and pain more often endorsed HCV symptoms, such as muscle and joint aches, trouble sleeping, and depressive symptoms, than those with an HCV diagnosis and no pain. Overall, participants endorsed significant depressive symptoms, with 58% reporting a past depression and 30.8% a past anxiety diagnosis. Of those reporting pain, 62% were current cigarette smokers. Silberbogen et al. (55) did not explore smoking in relation to pain. However, they identified a high prevalence of smoking as problematic, as smoking aggravates liver function, increases risk of liver fibrosis, and decreases the efficacy of treatment. They also highlight a high prevalence of depressive symptoms and suggest that depression may interfere with the participant's ability to cope with pain. Alternatively, cigarette withdrawal may increase depressive symptoms among smokers or, as discussed above, HCV-positive patients may use smoking to cope with depression (6).
Diverticulitis
Cigarette smoking may exacerbate medical conditions beyond hepatitis C. Yoo et al. (56) examined medical records for 112 (2.7% female) patients with diverticulitis, a condition where small, bulging pouches along the inner lining of the intestine become inflamed or infected, at a Connecticut veterans' medical center and found that 70.5% of participants had smoked cigarettes for >30 years. More (n = 41) patients who smoked required colectomy, a surgical procedure to remove all or part of the colon, compared with those who did not smoke (n = 35), which was marginally significant (P = 0.06). Patients were also more likely to undergo colectomy if they had comorbid chronic obstructive pulmonary disorder compared with those who did not (30.7% vs. 15.1%) (P = 0.06). Chronic obstructive pulmonary disorder is not known to complicate diverticulitis. However smoking may be an underlying factor that increases chronic obstructive pulmonary disorder and diverticulitis complications (56).
Health-related quality of life
Examining cigarette smoking in relation to health-related quality of life, Voelker et al. (57) explored physical and mental health summary scores from the 36-item Short Form Health Survey (SF-36) among 3,695 (0.09% female) Gulf War deployed and nondeployed veterans and found that war-deployed veterans had poorer adjusted health scores (approximately 2 points lower) than did nondeployed veterans. Smoking independently related to poorer health following deployment, with a decrease in mean score compared with never smokers of 2.5 (standard deviation, 0.4).
Exploring musculoskeletal injury, health-related quality of life, and smoking among 170 veterans (4% female) attending an outpatient wheelchair clinic in Oklahoma City, Rabadi and Vincent (58) found that smoking did not impact health-related quality of life, including pain measures. However, a greater number of health conditions correlated with decreased quality of life. Smoking cigarettes is known to increase chronic health conditions (59), so smoking may still relate to decreased quality of life.
Cigarette smoking and pain medication
We identified 3 studies exploring cigarette smoking and pain in relation to prescription opioid use among veterans. Dobscha et al. (60) examined Veterans Health Administration data to identify 5,961 veterans with elevated pain scores who were not prescribed opioids in the past year and, following them for another year, compared those prescribed opioids with those not prescribed opioids. Dobscha et al. (60) found that major depression (AOR = 1.24, 95% CI: 1.10, 1.39; AOR = 1.48, 95% CI: 1.14, 1.93) and nicotine dependence (AOR = 1.34, 95% CI: 1.17, 1.53; AOR = 2.02, 95% CI: 1.53, 2.67) increased the likelihood of veterans receiving an opioid prescription and chronic opioid therapy. Nicotine dependence may have increased odds of a prescription because of a psychiatric disorder or alteration in pain processes related to the physical effects of nicotine (60). In a similar study, Macey et al. (61) analyzed data from the Veterans Integrated Service Network-20 for 762 veterans (15% female) seen at a Pacific Northwest Veterans Health Administration facility to explore patterns and correlates of prescription opioid use among those with chronic noncancer pain and found that veterans with PTSD (AOR = 1.42, 95% CI: 1.04, 1.96) or nicotine use disorder (AOR = 2.14, 95% CI: 1.41, 3.27) were more likely to receive opioid prescriptions than those without these disorders. Among all analyzed variables, nicotine use disorder had the strongest relationship with opioid receipt (61). Morasco et al. (62) also examined data from the Veterans Integrated Service Network-20 for 1,478 veterans with chronic pain and found that those with nicotine dependence were marginally more likely to have a high-dose opioid prescription (AOR = 1.36, 95% CI: 1.00, 1.86) as were those with neuropathy (AOR = 1.95, 95% CI: 1.28, 2.97) and lower back pain (AOR = 1.88, 95% CI: 1.32, 2.70). Examining opioid prescriptions sheds light on smokers’ need for additional pain medication. Future studies should explore pain levels in conjuncture with opioid prescriptions.
We also identified 2 studies that explored prescription drug misuse and cigarette smoking. Jeffery et al. (63) examined correlates of prescription drug misuse among 28,546 (14.2%) military personnel and found that the strongest correlate of misuse was having received a previous prescription for a pain reliever (past-month AOR = 2.56, 95% CI: 2.23, 2.94; past-year AOR = 2.51, 95% CI: 2.25, 2.81). Data were self-reported, and prescription drug misuse was defined in the survey instrument as nonmedical use of a prescription drug (without a physician's prescription, in greater amounts or more often than a doctor prescribed, or for reasons such as to get “high” or for “thrill” or “kicks” and including the examples of sedatives, barbiturates, pain relievers, stimulants other than methamphetamine, and tranquilizers or muscle relaxers). Examples of specific brand names were also included. An interaction between former smoking and alcohol consumption negligibly decreased prescription drug misuse (63). However, statistics were not reported. Becker et al. (64) examined prescription drug misuse among 6,377 (9.3% female) veterans and found that chronic pain (odds ratio = 1.9, 95% CI: 1.4, 2.5) and smoking (odds ratio = 1.4, 95% CI: 1.1, 1.8) correlated with misuse, as did younger age, possible depression, and probable depression. Also, based on self-reported data, prescription drug misuse was considered to occur when respondents answered yes to the question, “In the last 6 months have you intentionally misused prescription medications (misused means taking more medication than you're supposed to or taking prescription medication not prescribed to you)?” Adjusted analysis found that younger age, strained financial situation (AOR = 1.5, 95% CI: 1.01, 2.1), smoking (AOR = 1.8, 95% CI: 1.3, 2.7), illicit drug use (AOR = 3.4, 95% CI: 2.3, 5.0), and chronic pain (AOR = 1.6, 95% CI: 1.1, 2.4) correlated with frequent misuse. Adjusted models were not explored for misuse alone (64). It is possible that participants with pain used prescription drugs and cigarettes in an attempt to self-manage symptoms and may benefit from additional pain management support (63).
In summary, cigarette smoking increased the likelihood of veterans receiving opioid prescriptions and misusing opioids. Research did not elucidate whether increased opioid use among smokers related to the physiological effects of smoking-related pain relief or to poor mental health. Studies that found an association between opioid use and smoking also found that depression or PTSD correlated with receiving a prescription or misuse. If individuals use smoking to cope with negative emotions (21), it is possible that those with chronic pain and depressive symptoms use cigarettes to cope with both.
PTSD, pain, and cigarette smoking
We identified 5 studies that examined PTSD, physical health or chronic pain, and cigarette smoking. Analyzing archival data from 943 (6% female) cigarette-smoking Veterans Health Administration patients randomized to either integrated PTSD and smoking cessation treatment or treatment as usual (separate PTSD and smoking cessation treatment), Aversa et al. (65, 66) found that, before treatment, participants endorsed severe PTSD symptomology and poor health-related quality of life. Although only a small proportion (6.6%) achieved bio-verified abstinence at 6- or 18-month follow-up (8.9% in integrated care and 4.5% in usual treatment), participants’ PTSD symptoms improved over the course of the study. Improved intrusive, hyperarousal, and emotional numbing symptoms correlated with improved general health, while improved emotional numbing and hyperarousal symptoms correlated with less bodily pain, suggesting that heightened pain sensitivity is important among individuals with PTSD (65). Improved emotional numbing symptoms also correlated with improved vitality. Participants with fewer PTSD symptoms had better perceptions and future expectations of health than those with greater symptomology. Individuals with fewer PTSD or depressive symptoms also reported less bodily pain and fatigue and better social functioning than those with more symptoms. Finally, individuals with fewer depressive symptoms reported better health-related quality of life when controlling for PTSD symptom severity and long-term cigarette abstinence. Findings suggest that PTSD and depression independently relate to perceptions of greater pain among veterans and that, among those with PTSD, increased pain perception relates to increased sensitivity (65). If this is the case, veterans with PTSD who experience pain are potentially susceptible to the pain–smoking and mental health–smoking feedback loops (6, 21).
Barrett et al. (39) explored health and PTSD among 3,682 veterans, 1.4% with PTSD (13.2% female), and found that current smokers were more likely to screen positive for PTSD than were never smokers (AOR = 3.83, 95% CI: 1.40, 10.46) and that those who screened positive for PTSD had a greater mean number of health conditions than those who did not screen positive (with PTSD (n = 10.18) vs. without PTSD (n = 1.73)). The number of physical symptoms also positively correlated with PTSD severity (r = 0.60, P < 0.001). Similarly, a positive relation was found between the number of medical conditions reported and PTSD severity (r = 0.50, P < 0.0001). Barrett et al. (39) suggested that the relationship between PTSD and increased smoking might be important in understanding the relation between PTSD and health. Smoking may explain some of the poor health symptoms associated with PTSD.
In a similar study, Schnurr and Spiro (67) explored a potential relationship between physical health and PTSD among 921 male veterans enrolled in the Boston Veterans Health Administration Normative Aging Study and found that combat exposure and smoking weakly related to pain (bivariate correlations, −0.7 and −0.08, respectively; P < 0.05). PTSD strongly related to pain (bivariate correlation, −0.27; P < 0.001). In path analysis, combat exposure positively related to current smoking and to PTSD symptoms, PTSD symptoms positively related to current smoking, and current smoking and PTSD symptoms positively related to overall decreased health (67). Although the pathways are not clear, pain, PTSD, and smoking appear to be interrelated.
Examining health behaviors and health-related quality of life among predominantly female (61%) veterans visiting a Veterans Health Administration clinic (n = 134), Ouimette et al. (68) found that individuals with PTSD (25%) more often identified as current smokers (52%) than did those without (19%). PTSD diagnosis and, to a lesser degree, PTSD symptoms increased the participant's odds of having a circulatory (AOR = 3.69, 95% CI: 1.25, 10.18; AOR = 1.23, 95% CI: 1.07, 1.41, respectively) or musculoskeletal (AOR = 2.96, 95% CI: 1.13, 7.76; AOR = 1.13, 95% CI: 1.01, 1.26, respectively) condition. In addition, more severe PTSD symptoms positively correlated with poorer physical health-related quality of life, including pain (P < 0.01). More often than men, women endorsed never (13% vs. 48%) or current (15% vs. 21%) smoking and had worse scores in terms of role limitations due to physical and general health (68). The study was cross-sectional; thus, temporal sequences were not established. In addition, the authors did not report findings for analyses that explored smoking in relation to pain. However, the findings that increased PTSD severity correlated with increased levels of pain and that individuals with PTSD diagnoses had a high prevalence of smoking again suggest that individuals with PTSD may be susceptible to the pain–smoking feedback loop and highlight a need for studies of PTSD, cigarette smoking, and chronic pain.
In a similar study exploring self-reported health problems and functional impairment among only female veterans visiting a Veterans Health Administration clinic (n = 1,935), Dobie et al. (69) also found that veterans screening positive for PTSD (21%) were more likely than those who did not to endorse current cigarette smoking (AOR = 2.04, 95% CI: 1.52, 2.75). Veterans who screened positive for PTSD also endorsed poor mental health, including depressive symptoms and an eating or panic disorder, somatic distress, and poor physical health more than those without a positive PTSD screen. In addition, veterans with a positive screen were also more likely than those without to have a pain-related condition, including fibromyalgia (AOR = 3.00, 95% CI: 1.98, 4.45), irritable bowel syndrome (AOR = 2.82, 95% CI: 2.06, 3.85), and chronic pelvic pain (AOR = 2.75, 95% CI: 2.00, 3.81) (69). Smoking initiation, PTSD symptom onset, and pain onset were not reported. However, these observational findings suggest that female veterans with PTSD symptoms are more likely than those without to smoke and to have a pain-related and mental health condition. PTSD is strongly related to and often co-occurs with depression and anxiety, and smoking may serve similar functions of mood regulation for individuals with PTSD that it serves for individuals with depression and anxiety (21). Future research could explore if this is the case.
In summary, none of the identified studies reported findings regarding pain, smoking, or PTSD onset and, thus, exploring how variables related through time was impossible. Studies found increased odds of smoking among Veterans Health Administration patients with PTSD when compared with those without. Studies also found increased odds of pain among patients with PTSD. One study attempted to examine pain and PTSD in regard to smoking cessation. However, the small proportion of veterans who quit smoking during the study made detecting relationships difficult (65). Upon examination of pain and PTSD in relation to one another, the study found that both PTSD and depression might independently relate to perceptions of greater pain. In addition, among those with PTSD, increased pain perception may relate to increased sensitivity. Alternatively, studies found a relationship among combat exposure, smoking, PTSD, and pain, suggesting that exposure to combat or trauma may be the underlying variable connecting pain and smoking.
DISCUSSION
Veterans appear to have a similar or higher prevalence of smoking when compared with the general population (3, 25–27), and multiple mechanisms may increase their level of pain (22, 23, 37–40). Men and women in the military have identified coping with stress as a reason for starting smoking (70). Veterans may also smoke to cope with pain. Female veterans in particular may use cigarettes to cope, as female military personnel have reported smoking cigarettes to cope with the stress of being a woman in the military (71). Only 1 study identified by this review asked veterans with chronic pain if they used cigarettes to cope (47). However, veterans with chronic pain appear to be susceptible to the pain–smoking feedback loop proposed by Ditre et al. (6). In particular, smoking may worsen musculoskeletal and lower back injuries by causing deterioration of injury sites. Veterans with chronic pain may also use cigarettes to regulate mood, often in relation to pain.
Veteran studies that examined smoking in relation to pain did not examine the underlying mechanisms that might lead to or reinforce cigarette use as a way to address pain. Studies also did not explore smoking and pain in relation to the biopsychosocial model. Future studies should address these mechanisms and aspects of the biopsychosocial model that could further confound associations. Longitudinal studies must establish a timeline that includes smoking initiation in relation to pain onset and levels of cigarette consumption in relation to pain duration and magnitude to clarify whether veterans are caught in a pain–smoking feedback loop. Depression, anxiety, and PTSD are important covariates in future cigarette–pain studies. Links between poor mental health and pain and poor mental health and smoking are well established (6, 21). Because purposeful smoking to cope may also increase cigarette consumption, studies should explore self-identified reasons for smoking and if these reasons correlate with better or worse pain and cigarette cessation outcomes. Additionally, studies should identify better pain-coping strategies for male and female veterans.
There are multiple limitations to this study. Search engine algorithms may miss relevant articles. The algorithm used by Google Scholar is unknown (46), making it difficult to understand why particular results are returned. In addition, Google Scholar is known to have poor replicability so that a search query will return different results at different times (45). Identified papers primarily included cross-sectional findings, and future studies must include longitudinal data to establish when participants initiate smoking in relation to when their pain begins. Most studies also relied on self-reported data. Because individuals are sometimes embarrassed to report smoking and pain, self-reported results may not accurately represent the proportions of smokers or individuals who experience pain. Reported health measures that were not self-reported often came from International Classification of Diseases, Ninth Revision, diagnosis codes, which are known to have inaccuracies (72). Additionally, studies did not always differentiate whether pain was chronic. Future studies should address these limitations.
In conclusion, studies show an interaction between pain and smoking among veterans. However, mechanisms underlying this relationship remain unclear. Important mechanisms may include increased risk of musculoskeletal injury, decreased pain medication effectiveness, mood regulation, and PTSD. Future studies focused on this interaction, particularly among individuals who experience these mechanisms, could benefit veteran populations.
ACKNOWLEDGMENTS
Author affiliations: Kansas Health Institute, Topeka, Kansas (Shawna L. Carroll Chapman); and Department of Psychiatry and Behavioral Sciences, Duke University Medical Center, Durham, North Carolina (Li-Tzy Wu).
This work was made possible by research support from the US National Institutes of Health (R01MD007658, R33DA027503, R01DA019623, and R01DA019901 to L. W.) and the Department of Psychiatry and Behavioral Sciences (Psychiatry 4416016), Duke University School of Medicine.
The sponsoring agencies had no further role in the writing of this paper or the decision to submit the paper for publication. The opinions expressed in this paper are solely those of the authors.
Conflict of interest: none declared.
REFERENCES
- 1.Spelman JF, Hunt SC, Seal KH, et al. Post deployment care for returning combat veterans. J Gen Intern Med. 2012;27(9):1200–1209. doi: 10.1007/s11606-012-2061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Toblin RL, Quartana PJ, Riviere LA, et al. Chronic pain and opioid use in US soldiers after combat deployment. JAMA Intern Med. 2014;174(8):1400–1401. doi: 10.1001/jamainternmed.2014.2726. [DOI] [PubMed] [Google Scholar]
- 3.Brown DW. Smoking prevalence among US veterans. J Gen Intern Med. 2010;25(2):147–149. doi: 10.1007/s11606-009-1160-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Michna E, Ross EL, Hynes WL, et al. Predicting aberrant drug behavior in patients treated for chronic pain: importance of abuse history. J Pain Symptom Manage. 2004;28(3):250–258. doi: 10.1016/j.jpainsymman.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 5.Ditre JW, Heckman BW, Butts EA, et al. Effects of expectancies and coping on pain-induced motivation to smoke. J Abnorm Psychol. 2010;119(3):524–533. doi: 10.1037/a0019568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ditre JW, Brandon TH, Zale EL, et al. Pain, nicotine, and smoking: research findings and mechanistic considerations. Psychol Bull. 2011;137(6):1065–1093. doi: 10.1037/a0025544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gatchel RJ, Peng YB, Peters ML, et al. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133(4):581–624. doi: 10.1037/0033-2909.133.4.581. [DOI] [PubMed] [Google Scholar]
- 8.Plante T. Contemporary Clinical Psychology. 2nd ed. Hoboken, NJ: Wiley & Sons, Inc.; 2005. [Google Scholar]
- 9.Ditre JW, Brandon TH. Pain as a motivator of smoking: effects of pain induction on smoking urge and behavior. J Abnorm Psychol. 2008;117(2):467–472. doi: 10.1037/0021-843X.117.2.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hooten WM, Shi Y, Gazelka HM, et al. The effects of depression and smoking on pain severity and opioid use in patients with chronic pain. Pain. 2011;152(1):223–229. doi: 10.1016/j.pain.2010.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Benowitz NL. Nicotine and postoperative management of pain. Anesth Analg. 2008;107(3):739–741. doi: 10.1213/ane.0b013e3181813508. [DOI] [PubMed] [Google Scholar]
- 12.Dodge HS, Ekhator NN, Jefferson-Wilson L, et al. Cigarette smokers have reduced risk for post-dural puncture headache. Pain Physician. 2013;16(1):E25–E30. [PubMed] [Google Scholar]
- 13.Zale EL, Ditre JW. Associations between chronic pain status, attempts to quit smoking, and use of pharmacotherapy for smoking cessation. Psychol Addict Behav. 2014;28(1):294–299. doi: 10.1037/a0032515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hahn EJ, Rayens MK, Kirsh KL, et al. Brief report: pain and readiness to quit smoking cigarettes. Nicotine Tob Res. 2006;8(3):473–480. doi: 10.1080/14622200600670355. [DOI] [PubMed] [Google Scholar]
- 15.Agahi N, Shaw BA. Smoking trajectories from midlife to old age and the development of non-life-threatening health problems: a 34-year prospective cohort study. Prev Med. 2013;57(2):107–112. doi: 10.1016/j.ypmed.2013.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weingarten TN, Moeschler SM, Ptaszynski AE, et al. An assessment of the association between smoking status, pain intensity, and functional interference in patients with chronic pain. Pain Physician. 2008;11(5):643–653. [PubMed] [Google Scholar]
- 17.Fishbain DA, Lewis JE, Gao J, et al. Are chronic low back pain patients who smoke at greater risk for suicide ideation? Pain Med. 2009;10(2):340–346. doi: 10.1111/j.1526-4637.2009.00570.x. [DOI] [PubMed] [Google Scholar]
- 18.Yunus MB, Arslan S, Aldag JC. Relationship between fibromyalgia features and smoking. Scand J Rheumatol. 2002;31(5):301–305. doi: 10.1080/030097402760375214. [DOI] [PubMed] [Google Scholar]
- 19.Shi Y, Weingarten TN, Mantilla CB, et al. Smoking and pain: pathophysiology and clinical implications. Anesthesiology. 2010;113(4):977–992. doi: 10.1097/ALN.0b013e3181ebdaf9. [DOI] [PubMed] [Google Scholar]
- 20.Dominick CH, Blyth FM, Nicholas MK. Unpacking the burden: understanding the relationships between chronic pain and comorbidity in the general population. Pain. 2012;153(2):293–304. doi: 10.1016/j.pain.2011.09.018. [DOI] [PubMed] [Google Scholar]
- 21.Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect: correlation, causation, and context across stages of smoking. Psychol Bull. 2003;129(2):270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- 22.Horowitz S. Treating veterans’ chronic pain and mental health disorders: an integrative, patient-centered approach. Altern Complement Ther. 2013;19(3):133–138. [Google Scholar]
- 23.Barrett DH, Boehmer TK, Boothe VL, et al. Health-related quality of life of U.S. military personnel: a population-based study. Mil Med. 2003;168(11):941–947. [PubMed] [Google Scholar]
- 24.Blosnich J, Foynes MM, Shipherd JC. Health disparities among sexual minority women veterans. J Womens Health. 2013;22(7):631–636. doi: 10.1089/jwh.2012.4214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dichter ME, Cerulli C, Bossarte RM. Intimate partner violence victimization among women veterans and associated heart health risks. Womens Health Issues. 2011;21(4 Suppl):S190–S194. doi: 10.1016/j.whi.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 26.Duffy SA, Kilbourne AM, Austin KL, et al. Risk of smoking and receipt of cessation services among veterans with mental disorders. Psychiatr Serv. 2012;63(4):325–332. doi: 10.1176/appi.ps.201100097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Farmer MM, Rose DE, Riopelle D, et al. Gender differences in smoking and smoking cessation treatment: an examination of the organizational features related to care. Womens Health Issues. 2011;21(4):S182–S189. doi: 10.1016/j.whi.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 28.Batuman F, Bean-Mayberry B, Goldzweig CL, et al. Health Effects of Military Service on Women Veterans. Washington, DC: Department of Veterans Affairs; 2011. (VA-ESP Project # 05-226) [PubMed] [Google Scholar]
- 29.Yoon J, Scott JY, Phibbs CS, et al. Trends in rates and attributable costs of conditions among female VA patients, 2000 and 2008. Womens Health Issues. 2012;22(3):e337–e344. doi: 10.1016/j.whi.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 30.Altarac M, Gardner JW, Popovich RM, et al. Cigarette smoking and exercise-related injuries among young men and women. Am J Prev Med. 2000;18(3 Suppl):96–102. doi: 10.1016/s0749-3797(99)00166-x. [DOI] [PubMed] [Google Scholar]
- 31.Lincoln AE, Smith GS, Amoroso PJ, et al. The effect of cigarette smoking on musculoskeletal-related disability. Am J Ind Med. 2003;43(4):337–349. doi: 10.1002/ajim.10195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ekholm O, Grønbæk M, Peuckmann V, et al. Alcohol and smoking behavior in chronic pain patients: the role of opioids. Eur J Pain. 2009;13(6):606–612. doi: 10.1016/j.ejpain.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 33.Creekmore FM, Lugo RA, Weiland KJ. Postoperative opiate analgesia requirements of smokers and nonsmokers. Ann Pharmacother. 2004;38(6):949–953. doi: 10.1345/aph.1D580. [DOI] [PubMed] [Google Scholar]
- 34.Roberts ME, Fuemmeler BF, McClernon FJ, et al. Association between trauma exposure and smoking in a population-based sample of young adults. J Adolesc Health. 2008;42(3):266–274. doi: 10.1016/j.jadohealth.2007.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vaughan CA, Schell TL, Tanielian T, et al. Prevalence of mental health problems among Iraq and Afghanistan veterans who have and have not received VA services. Psychiatr Serv. 2014;65(6):833–835. doi: 10.1176/appi.ps.201300111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frayne SM, Chiu VY, Iqbal S, et al. Medical care needs of returning veterans with PTSD: their other burden. J Gen Intern Med. 2011;26(1):33–39. doi: 10.1007/s11606-010-1497-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beckham JC, Kirby AC, Feldman ME, et al. Prevalence and correlates of heavy smoking in Vietnam veterans with chronic posttraumatic stress disorder. Addict Behav. 1997;22(5):637–647. doi: 10.1016/s0306-4603(96)00071-8. [DOI] [PubMed] [Google Scholar]
- 38.Beckham JC, Roodman AA, Shipley RH, et al. Smoking in Vietnam combat veterans with post-traumatic stress disorder. J Trauma Stress. 1995;8(3):461–472. doi: 10.1007/BF02102970. [DOI] [PubMed] [Google Scholar]
- 39.Barrett DH, Doebbeling CC, Schwartz DA, et al. Posttraumatic stress disorder and self-reported physical health status among U.S. military personnel serving during the Gulf War period: a population-based study. Psychosomatics. 2002;43(3):195–205. doi: 10.1176/appi.psy.43.3.195. [DOI] [PubMed] [Google Scholar]
- 40.Chwastiak LA, Rosenheck RA, Kazis LE. Association of psychiatric illness and obesity, physical inactivity, and smoking among a national sample of veterans. Psychosomatics. 2011;52(3):230–236. doi: 10.1016/j.psym.2010.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Centers for Disease Control and Prevention, Office on Smoking and Health. Smoking and Tobacco Use. http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/ Updated February 6, 2014. Accessed March 3, 2014.
- 42.Fogelholm RR, Alho AV. Smoking and intervertebral disc degeneration. Med Hypotheses. 2001;56(4):537–539. doi: 10.1054/mehy.2000.1253. [DOI] [PubMed] [Google Scholar]
- 43.Ackerman WE, 3rd, Ahmad M. Effect of cigarette smoking on serum hydrocodone levels in chronic pain patients. J Ark Med Soc. 2007;104(1):19–21. [PubMed] [Google Scholar]
- 44.Parkerson HA, Zvolensky MJ, Asmundson GJ. Understanding the relationship between smoking and pain. Expert Rev Neurother. 2013;13(12):1407–1414. doi: 10.1586/14737175.2013.859524. [DOI] [PubMed] [Google Scholar]
- 45.Bramer WM, Giustini D, Kramer BMR, et al. The comparative recall of Google Scholar versus PubMed in identical searches for biomedical systematic reviews: a review of searches used in systematic reviews. Syst Rev. 2013;2:115. doi: 10.1186/2046-4053-2-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nourbakhsh E, Nugent R, Wang H, et al. Medical literature searches: a comparison of PubMed and Google Scholar. Health Info Libr J. 2012;29(3):214–222. doi: 10.1111/j.1471-1842.2012.00992.x. [DOI] [PubMed] [Google Scholar]
- 47.Patterson AL, Gritzner S, Resnick MP, et al. Smoking cigarettes as a coping strategy for chronic pain is associated with greater pain intensity and poorer pain-related function. J Pain. 2012;13(3):285–292. doi: 10.1016/j.jpain.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chaiton M, Cohen J, O'Loughlin J, et al. Use of cigarettes to improve affect and depressive symptoms in a longitudinal study of adolescents. Addict Behav. 2010;35(12):1054–1060. doi: 10.1016/j.addbeh.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 49.George SZ, Childs JD, Teyhen DS, et al. Predictors of occurrence and severity of first time low back pain episodes: findings from a military inception cohort. PLoS One. 2012;7(2):e30597. doi: 10.1371/journal.pone.0030597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976) 2000;25(24):3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 51.Childs JD, Teyhen DS, Van Wyngaarden JJ, et al. Predictors of web-based follow-up response in the Prevention of Low Back Pain in the Military Trial (POLM) BMC Musculoskelet Disord. 2011;12:132. doi: 10.1186/1471-2474-12-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.O'Connor FG, Marlowe SS. Low back pain in military basic trainees: a pilot study. Spine (Phila Pa 1976) 1993;18(10):1351–1354. doi: 10.1097/00007632-199308000-00015. [DOI] [PubMed] [Google Scholar]
- 53.Woodruff SI, Conway TL, Shillington AM, et al. Cigarette smoking and subsequent hospitalization in a cohort of young U.S. Navy female recruits. Nicotine Tob Res. 2010;12(4):365–373. doi: 10.1093/ntr/ntq007. [DOI] [PubMed] [Google Scholar]
- 54.Turnbull DK, Shepherd DB. Post-dural puncture headache: pathogenesis, prevention and treatment. Br J Anaesth. 2003;91(5):718–729. doi: 10.1093/bja/aeg231. [DOI] [PubMed] [Google Scholar]
- 55.Silberbogen AK, Janke EA, Hebenstreit C. A closer look at pain and hepatitis C: preliminary data from a veteran population. J Rehabil Res Dev. 2007;44(2):231–244. doi: 10.1682/jrrd.2006.05.0053. [DOI] [PubMed] [Google Scholar]
- 56.Yoo PS, Garg R, Salamone LF, et al. Medical comorbidities predict the need for colectomy for complicated and recurrent diverticulitis. Am J Surg. 2008;196(5):710–714. doi: 10.1016/j.amjsurg.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 57.Voelker MD, Saag KG, Schwartz DA, et al. Health-related quality of life in gulf war era military personnel. Am J Epidemiol. 2002;155(10):899–907. doi: 10.1093/aje/155.10.899. [DOI] [PubMed] [Google Scholar]
- 58.Rabadi MH, Vincent AS. Health status profile and health-related quality of life of veterans attending an out-patient clinic. Med Sci Monit. 2013;19:386–392. doi: 10.12659/MSM.889097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sturm R. The effects of obesity, smoking, and drinking on medical problems and costs. Health Aff. 2002;21(2):245–253. doi: 10.1377/hlthaff.21.2.245. [DOI] [PubMed] [Google Scholar]
- 60.Dobscha SK, Morasco BJ, Duckart JP, et al. Correlates of prescription opioid initiation and long-term opioid use in veterans with persistent pain. Clin J Pain. 2013;29(2):102–108. doi: 10.1097/AJP.0b013e3182490bdb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Macey TA, Morasco BJ, Duckart JP, et al. Patterns and correlates of prescription opioid use in OEF/OIF veterans with chronic noncancer pain. Pain Med. 2011;12(10):1502–1509. doi: 10.1111/j.1526-4637.2011.01226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Morasco BJ, Duckart JP, Carr TP, et al. Clinical characteristics of veterans prescribed high doses of opioid medications for chronic non-cancer pain. Pain. 2010;151(3):625–632. doi: 10.1016/j.pain.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jeffery DD, Babeu LA, Nelson LE, et al. Prescription drug misuse among U.S. active duty military personnel: a secondary analysis of the 2008 DoD survey of health related behaviors. Mil Med. 2013;178(2):180–195. doi: 10.7205/milmed-d-12-00192. [DOI] [PubMed] [Google Scholar]
- 64.Becker WC, Fiellin DA, Gallagher RM, et al. The association between chronic pain and prescription drug abuse in veterans. Pain Med. 2009;10(3):531–536. doi: 10.1111/j.1526-4637.2009.00584.x. [DOI] [PubMed] [Google Scholar]
- 65.Aversa LH, Stoddard JA, Doran NM, et al. PTSD and depression as predictors of physical health-related quality of life in tobacco-dependent veterans. J Psychosom Res. 2012;73(3):185–190. doi: 10.1016/j.jpsychores.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 66.Aversa LH, Stoddard JA, Doran NM, et al. Longitudinal analysis of the relationship between PTSD symptom clusters, cigarette use, and physical health-related quality of life. Qual Life Res. 2013;22(6):1381–1389. doi: 10.1007/s11136-012-0280-x. [DOI] [PubMed] [Google Scholar]
- 67.Schnurr PP, Spiro A., 3rd Combat exposure, posttraumatic stress disorder symptoms, and health behaviors as predictors of self-reported physical health in older veterans. J Nerv Ment Dis. 1999;187(6):353–359. doi: 10.1097/00005053-199906000-00004. [DOI] [PubMed] [Google Scholar]
- 68.Ouimette P, Cronkite R, Henson BR, et al. Posttraumatic stress disorder and health status among female and male medical patients. J Trauma Stress. 2004;17(1):1–9. doi: 10.1023/B:JOTS.0000014670.68240.38. [DOI] [PubMed] [Google Scholar]
- 69.Dobie DJ, Kivlahan DR, Maynard C, et al. Posttraumatic stress disorder in female veterans: association with self-reported health problems and functional impairment. Arch Intern Med. 2004;164(4):394–400. doi: 10.1001/archinte.164.4.394. [DOI] [PubMed] [Google Scholar]
- 70.Bray RM, Hourani LL, Olmsted KLR, et al. 2005 Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel, A Component of the Defense Lifestyle Assessment Program (DLAP) Research Triangle Park, NC: Research Triangle Institute; 2006. [Google Scholar]
- 71.Bray RM, Fairbank JA, Marsden ME. Stress and substance use among military women and men. Am J Drug Alcohol Abuse. 1999;25(2):239–256. doi: 10.1081/ada-100101858. [DOI] [PubMed] [Google Scholar]
- 72.Birman-Deych E, Waterman AD, Yan Y, et al. Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care. 2005;43(5):480–485. doi: 10.1097/01.mlr.0000160417.39497.a9. [DOI] [PubMed] [Google Scholar]