ABSTRACT
The emergence of novel influenza viruses that cause devastating human disease is an ongoing threat and serves as an impetus for the continued development of novel approaches to influenza vaccines. Influenza vaccine development has traditionally focused on producing humoral and/or cell-mediated immunity, often against the viral surface glycoproteins hemagglutinin (HA) and neuraminidase (NA). Here, we describe a new vaccine candidate that utilizes a replication-defective vesicular stomatitis virus (VSV) vector backbone that lacks the native G surface glycoprotein gene (VSVΔG). The expression of the H5 HA of an H5N1 highly pathogenic avian influenza virus (HPAIV), A/Vietnam/1203/04 (VN1203), and the NA of the mouse-adapted H1N1 influenza virus A/Puerto Rico/8/34 (PR8) in the VSVΔG vector restored the ability of the recombinant virus to replicate in cell culture, without the requirement for the addition of trypsin. We show here that this recombinant virus vaccine candidate was nonpathogenic in mice when given by either the intramuscular or intranasal route of immunization and that the in vivo replication of VSVΔG-H5N1 is profoundly attenuated. This recombinant virus also provided protection against lethal H5N1 infection after a single dose. This novel approach to vaccination against HPAIVs may be widely applicable to other emerging strains of influenza virus.
IMPORTANCE Preparation for a potentially catastrophic influenza pandemic requires novel influenza vaccines that are safe, can be produced and administered quickly, and are effective, both soon after administration and for a long duration. We have created a new influenza vaccine that utilizes an attenuated vesicular stomatitis virus (VSV) vector, to deliver and express influenza virus proteins against which vaccinated animals develop potent antibody responses. The influenza virus hemagglutinin and neuraminidase proteins, expressed on the surface of VSV particles, allowed this vaccine to grow in cell culture and induced a potent antibody response in mice that was effective against infection with a lethal influenza virus. The mice showed no adverse reactions to the vaccine, and they were protected against an otherwise lethal influenza infection after only 14 days postvaccination and after as many as 140 days postvaccination. The ability to rapidly produce this safe and effective vaccine in cell culture is additionally advantageous.
INTRODUCTION
With the ongoing public health threat of emerging strains of influenza virus and the precedent for potentially devastating worldwide pandemics, novel approaches to influenza vaccination remain a priority. The influenza virus surface glycoproteins hemagglutinin (HA) and neuraminidase (NA) are key mediators of the viral infectious cycle and obvious proteins of interest for novel vaccines. The majority of recent vaccine candidates focus predominantly on the immunogenic properties of the influenza virus HA, and sometimes NA, glycoprotein, seeking to utilize vector systems (1–3), adjuvants (4–6), alternative routes of immunization (7, 8), and novel antigen presentation and delivery systems (9–12) to increase humoral and/or cell-mediated immunity against these and other influenza virus antigens. Creating vaccines that also exploit the functional properties of the influenza virus glycoproteins represents a unique approach.
Influenza virus propagation in tissue culture typically requires the addition of exogenous trypsin to cleave the HA0 precursor, commonly at a basic amino acid between HA1 and HA2. This cleavage is essential for virus attachment and entry into host cells (13). Highly pathogenic avian influenza viruses (HPAIVs) have been shown to contain polybasic amino acid cleavage sites in HA that can be promiscuously activated by ubiquitous cellular proteases, leading to severe disease and also allowing for trypsin-independent growth in tissue culture (14–17). These influenza viruses have caused devastating outbreaks among poultry and wild birds and have sporadically caused cases of human disease (18–21). HPAIVs were originally found in areas of China and Southeast Asia, where they still circulate today, although their geographic distribution has spread widely (21, 22).
Our laboratory has developed vesicular stomatitis virus (VSV) as a vector for a wide variety of experimental vaccines (23–32). Due to its lack of pathogenicity in humans, potent induction of immune responses, wide range of cellular tropism, and exuberant growth properties, VSV is an ideal vaccine vector. Although the results of the first phase I trial utilizing an attenuated VSV vector as an HIV-1 vaccine candidate have not yet been published, preliminary safety and immunogenicity results suggest that this vaccine does not cause significant adverse events in humans (HVTN 090 study [http://clinicaltrials.gov/ct2/show/NCT01438606]).
VSV relies on the G surface glycoprotein for infectivity. Replication-deficient, pseudotyped VSVΔG vaccine vectors have been shown to be safe and effective in animal models (31, 33–35). While VSVΔG strains pseudotyped with VSV G or other viral glycoproteins are capable of only a single round of infection, our laboratory and others have shown that substituting other viral surface glycoprotein genes for VSV G in recombinant viruses can restore replication competence to VSVΔG (23, 36–39). We have termed these recombinants “surrogate viruses” to distinguish them from VSV pseudotypes that are made by complementation of VSVΔG with other viral glycoproteins (38). These recombinant, surrogate viruses can serve as potent vaccines while lacking pathogenicity. In previous studies, we generated VSVΔG recombinants expressing influenza virus HA and NA genes from a mouse-adapted influenza virus (WSN), but these viruses did not propagate without VSV G complementation, even though substantial quantities of HA and NA were present in the viral membrane (our unpublished data).
In the current study, we have created a novel vaccine against HPAIVs utilizing a hybrid VSVΔG vector expressing the HA of the H5N1 HPAIV A/Vietnam/1203/04 (VN1203) and the NA of a mouse-adapted H1N1 influenza virus, A/Puerto Rico/8/34 (PR8). This virus propagates in BHK-21 cells without any requirement for the addition of exogenous trypsin. This surrogate virus is nonpathogenic in mice yet protects mice against lethal challenge with an H5N1 influenza challenge virus (HALo, a 6:2 reassortant influenza virus containing the HA and NA segments of VN1203 and internal gene segments from PR8, with the removal of the polybasic cleavage site in HA [40]).
MATERIALS AND METHODS
Plasmid constructions.
To generate pVSVΔG-H5N1, the VSV G gene was first removed from full-length plasmid pVSV-H5-HA(VN1203) (27) by MluI-XhoI digestion. The PR8 NA gene was amplified by PCR from pCAGGS-NA(PR8) using the forward primer GTACGTACacgcgtactATGAATCCAAATCAGAAAAT and the reverse primer GATCGATCctcgagCGTGATATCTGTTAGTTTTTTTCATACTACTTGTCAATGCTGAATGG (lowercase letters represent restriction sites), containing a VSV transcription stop-start sequence. This PCR product was purified, digested with MluI-XhoI, and cloned into the VSVΔG vector described above. Plasmid pCAGGS-HA(VN1203) was made by digesting pVSV-H5-HA(VN1203) with XhoI-NheI to release the H5 HA gene, which was then ligated into pCAGGS digested with XhoI-NheI.
Metabolic labeling of cells infected with recombinant viruses and SDS-PAGE of cell lysates.
BHK-21 cells were infected with recombinant viruses at a multiplicity of infection (MOI) of 10. At 6 h postinfection (p.i.), cells were washed with methionine-free Dulbecco's modified Eagle's medium (DMEM), followed by labeling with 100 μCi of [35S]methionine in 0.5 ml of methionine-free DMEM for 1 h at 37°C. Cells were washed with phosphate-buffered saline (PBS) and lysed with detergent lysis buffer (1% Nonidet P-40, 0.4% deoxycholate, 50 mM Tris-HCl [pH 8.0], 62.5 mM EDTA) on ice for 5 min. Lysates were subjected to SDS-PAGE on a 4 to 12% Bis-Tris NuPAGE gel (Invitrogen, CA). Protein bands on the dried gel were scanned by using a Fujifilm BAS 1800 imaging system.
Antisera and antibodies.
The anti-VSV G monoclonal antibodies I1 and I14 (41) were used to detect VSV G expression. Sheep antiserum to recombinant HA (rHA) [subtype H5 influenza A/HK/156(483)/97 (H5N1) virus] was obtained from BEI Resources. Polyclonal anti-VSV serum was used to detect VSV proteins in Western blots. Antisera to PR8 NA was obtained from BALB/c mice that had recovered from an infection with PR8.
Indirect immunofluorescence microscopy.
BHK-21 cells on coverslips were infected with recombinant wild-type (wt) VSV, VSV-H5, or VSVΔG-H5N1 for 6 h. Cells were then washed twice with PBS and fixed with 3% paraformaldehyde for 30 min. Cells were again washed with PBS-glycine (10 mM) and incubated with a 1:200 dilution of VSV G monoclonal antibodies (I1/I14), a 1:200 dilution of sheep anti-H5N1, or a 1:100 dilution of mouse anti-PR8 NA. The cells were then washed in PBS-glycine and incubated with a 1:500 dilution of goat anti-mouse Alexa Fluor 488 IgG or donkey anti-sheep Alexa Fluor 488 IgG (Molecular Probes, Eugene, OR). Cells were washed twice in PBS-glycine, mounted onto slides by using Prolong Gold antifade reagent with 4′,6-diamidino-2-phenylindole (DAPI) (Molecular Probes, Eugene, OR), and imaged with a Nikon Eclipse 80i fluorescence microscope using a 40× objective.
Recombinant virus recovery.
Recombinant VSV (rVSV) was recovered from pVSVΔG-H5N1 as described previously (42, 43). In brief, BHK-21 cells were infected with vTF-7.3 (44) at an MOI of 10. The cells were transfected with pVSVΔG-H5N1 together with support plasmids pBS-N, pBS-P, pBS-L, and pBS-G, encoding VSV proteins. The cell supernatants were collected at 48 h and passaged onto BHK-21 cells that were transfected with pCAGGS-G (45) 1 day earlier. This supernatant containing the virus was collected after 48 h. The virus was plaque purified without VSV G complementation on BHK-21 cells and further passaged on BHK-21 cells to generate a non-G-complemented VSVΔG-H5N1 stock. The stock was serially diluted and plaqued on BHK-21 cells. Plaques were stained with crystal violet after 48 h.
Virus neutralization assays.
To measure neutralizing antibodies (NAbs) to H5N1 in mice, serum samples were serially diluted with PBS in a 96-well plate and mixed with ∼100 infectious particles of wt VSV or VSVΔG-H5N1 to a final volume of 100 μl. The mixture was incubated at 37°C for 1 h, and 100 μl of BHK-21 cells (5 × 103 cells) was added to each well. The cells were incubated at 37°C for 48 to 72 h. The neutralization titer was defined as the reciprocal of the highest serum dilution at which duplicate wells showed complete neutralization of the virus.
Neutralizing antibody titers were additionally determined by a microneutralization assay, as described previously (46). Briefly, serial 2-fold dilutions of heat-inactivated serum were prepared, beginning with a 1:10 dilution. Equal volumes of serum and virus were combined, incubated at room temperature for 1 h, and added to MDCK cells. The residual infectivity of each dilution of the virus-serum mixture was determined in quadruplicate. The neutralizing titer was defined as the reciprocal of the highest dilution of serum that completely neutralized the infectivity of 100 50% tissue culture infective doses (TCID50) of the appropriate wt H5N1 virus for MDCK cells. Infectivity was identified by the presence of a cytopathic effect (CPE) on day 4.
Endpoint ELISA titers.
Flat-Bottom Immuno Nonsterile 4 HBX 96-well plates (Thermo Scientific) were coated with 50 μl of recombinant protein diluted in enzyme-linked immunosorbent assay (ELISA) coating buffer (pH 9.4) at a concentration of 2 μg/ml per well and refrigerated at 4°C overnight. Coating buffer was discarded, and wells were blocked with 100 μl of blocking solution (PBS containing 0.1% Tween 20 [T-PBS], 3% goat serum [Gibco], and 0.5% milk powder) for 1 h at room temperature. Another 50 μl of blocking solution was added to the first column of the wells, as was 1.5 μl of mouse serum (starting concentration of 1:100). The samples were 3-fold serially diluted and incubated at room temperature for 2 h. The plates were washed 6 times with T-PBS, and 50 μl of blocking solution containing anti-mouse IgG (Fab specific)-peroxidase antibody (Sigma) at a concentration of 1:3,000 was added. After 1 h of incubation at room temperature, the plates were washed 6 times with T-PBS and developed with 100 μl of SigmaFast OPD (Sigma) per well. The developing process was stopped after 10 min with 3 M hydrochloric acid (HCl), and the absorbance at 490 nm was read with a Synergy H1 hybrid multimode microplate reader (BioTek).
The average absorbance plus 3 times the standard deviations of all blanks below an absorbance of 0.065 was calculated and used as the cutoff for endpoint titer analysis.
Hemagglutination inhibition assays.
To remove unspecific serum reactivity, mouse sera were trypsin-heat-periodate treated. A one-half volume of l-1-tosylamido-2-phenylethyl chloromethyl ketone (TPCK)-trypsin at a concentration of 8 mg/ml was added to 1 volume of serum, and the mixture was incubated at 56°C for 30 min and then cooled to room temperature. Three volumes of 0.011 M metapotassium periodate (KlO4) were added, and sera were incubated at room temperature for 15 min. Three volumes of 1% glycerol saline were added, and sera were incubated for another 15 min at room temperature. Two and a half volumes of 85% PBS were added for a final serum dilution of 1:10.
Influenza viruses were prepared at a concentration of 8 hemagglutination units (HAUs) per 50 μl, and chicken red blood cells (RBCs) were diluted in PBS to a concentration of 0.5%.
Fifty microliters of trypsin-heat-periodate-treated serum was added to the first well of a 96-well V-bottom plate and 2-fold serially diluted in PBS to a final volume of 25 μl per well. Twenty-five microliters of diluted virus was added to each well, and the contents were mixed and incubated at room temperature for 30 min. Fifty microliters of RBCs was added to each well, and the contents were mixed. After incubation at 4°C for 45 min, the hemagglutination inhibition (HAI) titers were determined. Back titrations of the viruses were performed to confirm a concentration of 8 HAUs/50 μl.
Western blots.
Whole-cell extracts were prepared from BHK-21 cells infected with VSV G, VSV-H5, and VSVΔG-H5N1. Samples were analyzed by SDS-PAGE on a 4 to 12% Bis-Tris NuPAGE gel (Invitrogen), and Western blot analysis was performed by using antibodies specific for H5 HA or VSV (Indiana serotype). The anti-H5 blot was stripped and reprobed with anti-VSV antibody.
Animal experiments.
Six- to eight-week-old female BALB/c mice were obtained from Charles River Laboratories (Wilmington, MA) and housed for 1 week prior to immunization. Animals were housed under biosafety level 2 (BSL-2) conditions in microisolator cages. Viruses were diluted in serum-free DMEM for immunizations. Intranasal (i.n.) inoculations were performed with either VSVΔG-H5N1 or a control virus (VSV-EGFP [47]) administered in a volume of 25 μl to animals that were lightly anesthetized with 20% (vol/vol) isoflurane (Baxter) diluted in propylene glycol. For intramuscular (i.m.) immunizations, the VSVΔG-H5N1 virus, or a control virus [VSVΔG-G(NiV) (VSVΔG expressing the G glycoprotein of Nipah virus) (37)], was injected in a volume of 50 μl into the left hind leg muscle. Blood was collected from the retro-orbital sinus for neutralization assays.
Influenza virus challenges were performed with the low-pathogenicity H5N1 HALo influenza virus (6:2 reassortant influenza virus containing internal gene segments from A/Puerto Rico/8/34 and HA and NA from A/Vietnam/1203/04 with the removal of the polybasic cleavage site in HA [40]). Mice were anesthetized with 20% isoflurane (Baxter) as described above, and the challenge virus was administered in a volume of 50 μl. The Yale University and Icahn School of Medicine at Mount Sinai Institutional Animal Care and Use Committees approved all immunization and challenge experiments (Yale University protocol permit number 2012-07680), and experiments were done in a biosafety level 2 animal facility in accordance with the regulations of Yale University.
In vivo recovery of VSVΔG-H5N1.
Groups of BALB/c mice were immunized with either VSVΔG-H5N1 or a control virus (VSV-cH5/1 [1]) by both the i.m. and i.n. routes. Vaccination with VSVΔG-H5N1 was done with a 100-fold-higher dose than that used for vaccination with VSV-cH5/1 (2 × 107 PFU of VSVΔG-H5N1 versus 2 × 105 PFU of VSV-cH5/1). Mice were euthanized either 24 h or 96 h after vaccination, and tissues (lung, spleen, draining lymph nodes, and leg muscle) were isolated and frozen. Homogenates were prepared in 2.5% DMEM, as previously described (48), and frozen at −80°C prior to inoculation of cell monolayers. BHK-21 cells that were plated onto 24-well plates the day prior were then exposed to 20 μl of the supernatant and observed for viral CPE for 72 h. Any well demonstrating CPE within this time period was subjected to a plaque assay to determine the titer of recovered virus.
RESULTS
Preliminary complementation studies.
To determine if the influenza virus HA and NA glycoproteins could substitute for the VSV G protein to generate infectious, pseudotyped particles, we initially tried to complement VSVΔG-EGFP (30) with the HA and NA proteins of influenza virus strain A/Puerto Rico/8/34 expressed from the pCAGGS vector (49). We were able to detect only low and variable levels (102 to 103 infectious units [IU]/ml) of pseudotyped particles after complementation. Furthermore, this low level of infectivity was detectable only after trypsin treatment of the pseudotypes, indicating poor cleavage of the expressed HA protein by cellular enzymes.
Because the HA proteins of HPAIV strains are cleaved efficiently at a polybasic sequence by cellular furin-like proteases (14–17), we next tested the complementation of VSVΔG-EGFP by an HPAIV H5 HA protein (A/Vietnam/1203/04) in combination with the PR8 (H1) NA protein. Complementation with both proteins yielded pseudotyped virus with titers of >5 × 105 IU/ml in the absence of trypsin treatment. These pseudotype titers were only 5- to 10-fold lower than those obtained by complementation with the VSV G protein. Complementation with H5 HA or H1 NA alone did not yield infectious pseudotypes. Although HA alone could in theory confer infectivity, the NA protein is presumably required for the release of pseudotyped particles from cells through cleavage of the sialic acid receptor (50).
Construction and recovery of VSVΔG-H5N1.
Because of the positive complementation results with the H5 and N1 proteins, we next determined if a VSVΔG recombinant expressing both the H5 HA (A/Vietnam/1203/04) and N1 (A/Puerto Rico/8/1934) proteins could be constructed and might be infectious in the absence of VSV G. We included the NA and HA genes as two separate genes with their own transcription start-stop and poly(A) signals. These genes replaced the VSV G gene, as diagrammed in Fig. 1A.
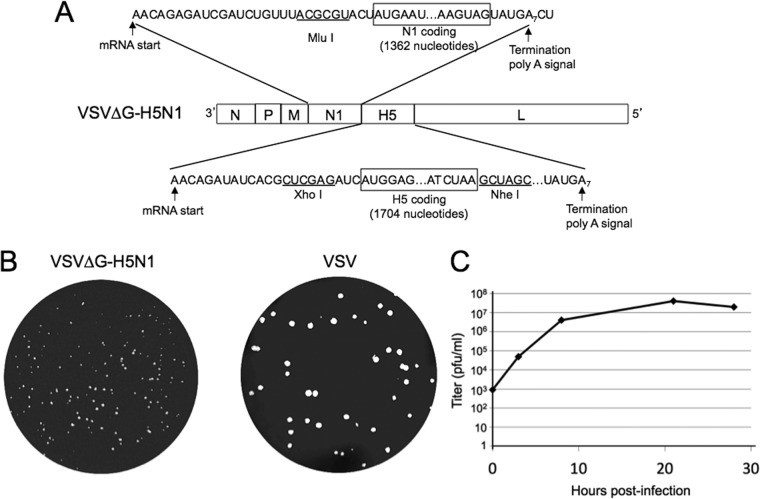
FIG 1.
The VSVΔG recombinant encoding the influenza virus HA and NA genes and representative plaque morphology. (A) Diagram of the VSV recombinant with the insertion of the influenza virus N1 NA and H5 HA genes between the VSV M and L genes in a VSVΔG vector. (B) Plaque morphology of VSVΔG-H5N1 and VSV 2 days after infection of BHK-21 cells. (C) One-step growth curve of VSVΔG-H5N1. BHK-21 cells were infected at time zero with VSVΔG-H5N1 at an MOI of 5, the inoculum was removed after 30 min, cells were washed twice with PBS, and samples of the medium were taken immediately (time zero) and at the indicated times thereafter for subsequent plaque titration.
The VSVΔG-H5N1 recombinant was recovered initially by complementation with the VSV G protein, but we found subsequently that it propagated on BHK-21 cells in the absence of the VSV G protein. The titers of VSVΔG-H5N1 particles obtained on BHK-21 cells were typically ∼2 × 107 PFU per ml, or 25-fold lower than those of VSV. Consistent with the lower titers, we found that the recombinant made much smaller plaques than did VSV (Fig. 1B). A one-step growth curve of VSVΔG-H5N1 is shown in Fig. 1C, where a maximal titer was reached by 21 h postinfection.
The VSVΔG-H5N1 recombinant expresses both HA and NA on the cell surface.
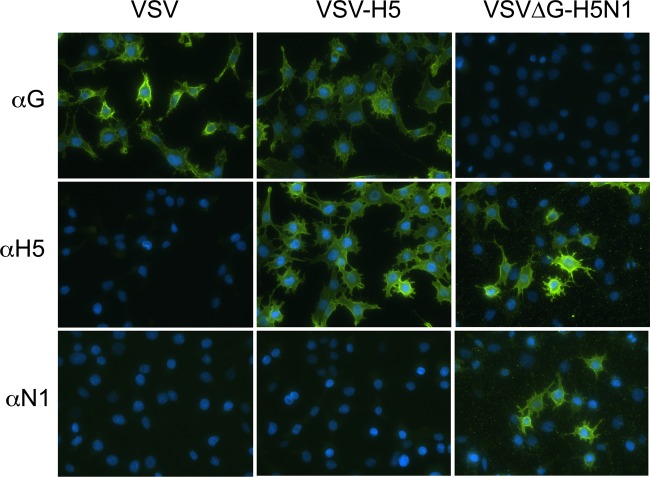
We next used indirect immunofluorescence microscopy to determine if the HA and NA proteins expressed by VSVΔG-H5N1 were present on the cell surface. BHK-21 cells infected with VSV, VSV-H5 (a previously described VSV recombinant expressing HA from A/Hong Kong/156/97), or VSVΔG-H5N1 were fixed and incubated separately with antibodies binding to VSV G, influenza virus H5 HA, or influenza virus H1 NA and then with a secondary fluorescent antibody.
The results (Fig. 2) showed that cells infected with VSVΔG-H5N1 did not express VSV G but did express H5 HA and NA on the cell surface. Control cells infected with VSV were positive for VSV G on the cell surface but negative for HA or NA. Additional control cells infected with VSV-H5 showed expression of HA and VSV G, but not NA, on the cell surface.
FIG 2.
Indirect immunofluorescence microscopy of VSVΔG-H5N1- and VSV-H5-infected cells. BHK-21 cells were infected with the indicated viruses for 6 h and then fixed in 3% paraformaldehyde. Cells were then incubated with either anti-VSV G mouse monoclonal antibodies, anti-H5 polyclonal sheep serum, or anti-PR8 NA polyclonal mouse serum, followed by anti-mouse or anti-sheep Alexa Fluor 488-conjugated secondary antibody staining. Nuclei are stained with DAPI. Images were taken with a Nikon Eclipse 80i fluorescence microscope.
VSVΔG-H5N1 expresses similar levels of HA and NA.
We next examined the expression levels of both HA and NA from the recombinant by metabolic labeling of infected cells with [35S]methionine (Fig. 3A). BHK-21 cells were infected with VSV, VSV-H5, or VSVΔG-H5N1 and labeled for 30 min; the labeled cell lysates were then fractionated by SDS-PAGE, and the proteins were detected on a phosphorimager. The cells infected with VSV showed the major bands of all five VSV proteins (L, G, N, P, and M), while cells infected with VSVΔG-H5N1 lacked the G band and showed new protein bands with the expected mobilities of the uncleaved HA0 precursor and NA proteins. The band intensities of HA0 and NA appeared equivalent, but when corrected for methionine content (13 in HA0 and 9 in NA), the NA expression level was slightly higher, consistent with its expression from the more upstream position in the VSV genome (51). Cells infected with VSV-H5 (52) showed the HA0 precursor as well as VSV G. Note that this VSV-H5 expresses the HK156 HA protein, which migrates slightly faster than the VN1203 HA protein expressed by VSVΔG-H5N1 (52).
FIG 3.
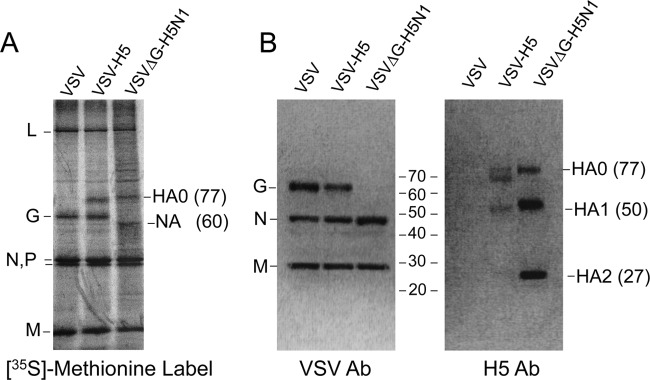
Metabolic labeling and Western blotting. (A) Metabolic labeling of proteins expressed from recombinant VSV vectors. BHK-21 cells were infected with the indicated viruses and then metabolically labeled with [35S]methionine. Cell lysates were subjected to SDS-PAGE on a 4-to-12% gradient gel, and the protein bands on the dried gel were imaged. Positions of VSV proteins are indicated on the left side of the gel image, and influenza virus proteins are indicated on the right side. (B) Western blot analysis of BHK-21 whole-cell extracts infected with the indicated viruses. Sample lysates were analyzed by SDS-PAGE on a 4-to-12% gradient gel, and Western blotting was performed by using a polyclonal VSV (Indiana serotype) antiserum and the polyclonal H5 HA-specific antibody (Ab) NR-665. The positions of full-length (HA0) and cleaved (HA1 and HA2) H5 HA isoforms are indicated on the right side of the anti-H5 blot.
The majority of HA incorporated into VSVΔG-H5N1 particles is cleaved to HA1 and HA2.
We also used Western blotting to examine the incorporation and extent of cleavage of H5 HA present in VSV particles (Fig. 3B). Purified virus particles prepared from cells infected with VSV, VSV-H5, or VSVΔG-H5N1 were fractionated by SDS-PAGE and then blotted with anti-HA antibody or antibody to VSV. Blotting with anti-VSV antibody showed the expected major VSV proteins (G, N, and M) in VSV particles as well as the absence of VSV G in the VSVΔG-H5N1 particles. Blotting of VSVΔG-H5N1 with anti-H5 HA revealed major bands of proteins with the mobilities expected for HA1 (50 kDa) and HA2 (27 kDa) and a minor band of HA0 (77 kDa). This result indicates that the majority of HA present in the particles is cleaved. The VSV-H5 blot also showed a clear band of HA1 and a faint band of HA2, but the extent of cleavage of this HK156 H5 protein appears to be lower than that of the VN1203 protein in VSVΔG-H5N1 particles.
VSVΔG-H5N1 is nonpathogenic in mice.
VSV and prototype VSV recombinants expressing VSV G and foreign antigens can cause significant pathogenesis in mice when given by the i.n. route. This pathogenesis is most easily quantified by monitoring weight loss after inoculation. To determine if VSVΔG-H5N1 was pathogenic, we inoculated BALB/c mice (5 mice per group) with 1.25 × 107 PFU of VSVΔG-H5N1 i.n. and monitored their weights for 13 days (Fig. 4). Control animals were inoculated i.n. with 106 PFU of a VSV recombinant expressing enhanced green fluorescent protein (VSV-EGFP) (30). The animals inoculated with VSV-EGFP showed the typical 10 to 15% weight loss at days 2, 3, and 4, followed by a gradual recovery. In contrast, the animals inoculated with VSVΔG-H5N1 showed no weight loss. In subsequent vaccination studies, no weight loss or any other signs of pathogenesis were observed for mice inoculated with VSVΔG-H5N1 for several months.
FIG 4.
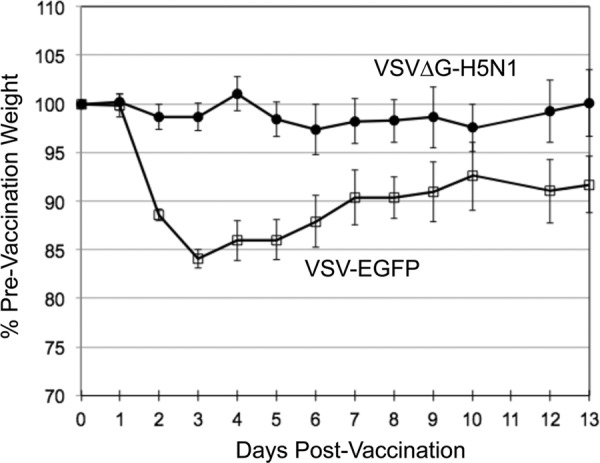
VSVΔG-H5N1 is nonpathogenic in mice. Groups of five 6- to 8-week-old female BALB/c mice were lightly anesthetized prior to i.n. vaccination with either 1.25 × 107 PFU of VSVΔG-H5N1 or 106 PFU of a VSV recombinant expressing EGFP. Weights were recorded daily for 13 days postinoculation and are graphically displayed as the average percentage of the prevaccination weight. Error bars represent 1 standard deviation above and below the average weight.
To determine if we could detect any replication of VSVΔG-H5N1 in vivo, we inoculated mice either i.n. or i.m. with 2 × 107 PFU of VSVΔG-H5N1 or 2 × 105 PFU of a control rVSV expressing VSV G and a hybrid influenza virus hemagglutinin (VSV-cH5/1). Tissues (leg muscle, lung, spleen, and draining lymph nodes) were isolated and homogenized at either 24 h or 96 h, as described previously, and assayed for infectious virus on BHK-21 cells (48). We detected no infectious VSVΔG-H5N1 in any tissue at either time point. Control experiments indicated a detection level of <200 PFU/tissue. In contrast, rVSV was recovered from all tissues of i.n. vaccinated mice at 24 h and from lung only at 96 h. In mice vaccinated i.m. with rVSV, virus was recovered only from muscle and draining lymph nodes. This finding is consistent with results from previous studies using rVSVs (48). These experiments indicate that VSVΔG-H5N1 does not replicate extensively in vivo.
VSVΔG-H5N1 induces neutralizing antibodies to HPAIV after a single dose.
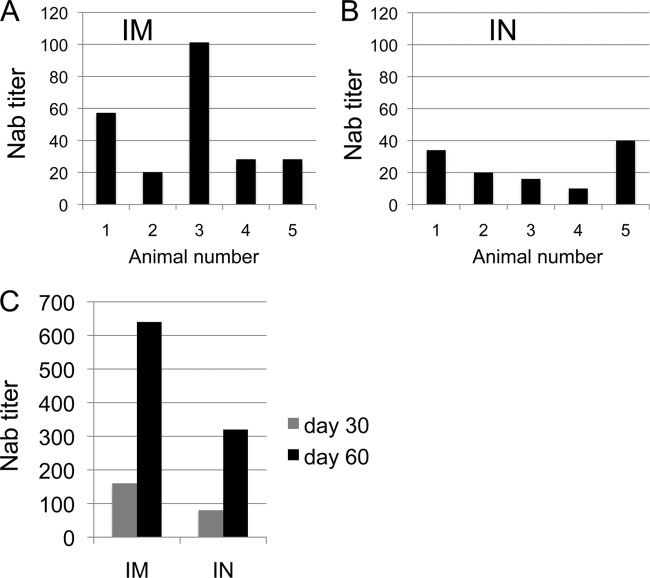
To determine if VSVΔG-H5N1 could induce NAbs to HPAIV, we inoculated BALB/c mice (5 per group) with 106 PFU VSVΔG-H5N1 by either the i.n. or i.m. route and assayed antibody titers after 60 days using a microneutralization assay (46) for influenza virus A/Vietnam/1203/2004 carrying the homologous H5 HA. In the i.m. inoculated group, the geometric mean titer (GMT) was 39, and the titers for the individual animals varied from 28 to 101 (Fig. 5A). In the i.n. inoculated group, the GMT was 21.3, and the range was 10 to 34 (Fig. 5B). To determine if the animals developed cross-clade NAbs to influenza virus A/Indonesia/05/2005, we used pooled serum from each group because of limited material. Pooled serum from the i.m. inoculated group had a clear cross-clade NAb titer of 25, while the i.n. inoculated group had a lower titer of 10.
FIG 5.
VSVΔG-H5N1 immunization induces NAbs in mice. Groups of five 6- to 8-week-old female BALB/c mice were vaccinated with 106 PFU of VSVΔG-H5N1 by either the i.m. (IM) or i.n. (IN) route, and serum was collected after 30 and 60 days to assay neutralizing antibody titers. (A) NAb titers from serum of individual mice vaccinated by the i.m. route. A microneutralization assay was performed by utilizing influenza virus A/Vietnam/1203/2004 with homologous H5 HA. (B) NAb titers from serum of individual mice vaccinated by the i.n. route as determined by a microneutralization assay. (C) Titers of NAbs in pooled 30- and 60-day-postvaccination serum from groups of 5 mice vaccinated with VSVΔG-H5N1 by either the i.m. or i.n. route. Titers are the reciprocal dilutions of pooled serum required to provide 100% neutralization of VSVΔG-H5N1 prior to incubation with BHK-21 cells.
We also tested the neutralization of VSVΔG-H5N1 by the pooled sera obtained from the same animals at 30 and 60 days postinoculation. Serial dilutions of the sera were incubated with 100 PFU of VSVΔG-H5N1 prior to infection of BHK-21 cells. The serum dilution that gave 100% inhibition of cytopathic effect in duplicate samples was determined. As shown in Fig. 5C, the 100% neutralization titers from the i.m. inoculated group were 1:160 and 1:640 at days 30 and 60, respectively. The titers from the i.n. inoculated group were 1:80 and 1:320 at days 30 and 60, respectively. The lower titers in the i.n. inoculated group were consistent with the results from the direct HPAIV NAb assays.
To better characterize the humoral response to VSVΔG-H5N1, serum collected from mice at 30 days post-i.m. vaccination with VSVΔG-H5N1 was subjected to ELISA with substrates including an H5 HA (A/Vietnam/1203/04), a chimeric HA containing an H6 HA head and an H1 HA stalk (cH6/1 HA), and N1 NA (Table 1). Endpoint titers against H5 HA and N1 NA were 1:24,300 and 1:8,100, respectively, but there was no detectable response against cH6/1 HA, indicating that the antibodies generated in response to this vaccine are largely specific for the HA head and the NA glycoprotein. The lack of reactivity with the cH6/1 HA substrate indicates a lack of heterosubtypic HA-specific and anti-stalk antibodies. Serum from mice vaccinated with VSVΔG-G(NiV) was used as a control and showed only low-level reactivity against all substrates.
TABLE 1.
Serum from mice vaccinated with VSVΔG-H5N1 recognizes H5 HA and N1 NA but not cH6/1 HA
| Mouse group | Reciprocal endpoint titer determined by ELISA |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| H5 VN04 |
cH6/1 (PR8 stalk) |
N1 PR8 |
|||||||
| Expt 1 | Expt 2 | Avg | Expt 1 | Expt 2 | Avg | Expt 1 | Expt 2 | Avg | |
| i.m. VSVΔG-H5N1 | 24,300 | 24,300 | 24,300 | 100 | 100 | 100 | 8,100 | 8,100 | 8,100 |
| i.m. VSVΔG-G(NiV) | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
Hemagglutination inhibition (HAI) experiments were performed, and mice vaccinated with a single i.m. VSVΔG-H5N1 dose did not produce detectable HAI titers 30 days after vaccination. This is not unexpected, as protective/neutralizing humoral responses against H5 HA in the absence of detectable HAI, even in human subjects, have been documented (53).
A single dose of VSVΔG-H5N1 protects mice from lethal avian influenza virus challenge.
To determine if VSVΔG-H5N1 could confer protection from lethal avian influenza virus challenge, we used the same mice for which we had measured the NAb titers and challenged them i.n. with 4 50% lethal doses (LD50) of the low-pathogenicity H5N1 HALo virus at 140 days after vaccination. As shown in Fig. 6A, three unvaccinated age-matched control animals showed rapid weight loss, and two of the three animals died on days 6 and 8 postchallenge. One animal made a gradual recovery to normal weight by day 22. In contrast, the five vaccinated animals in each group were all protected. On average, animals in the i.m. inoculated group lost no more than 5% of their weight, and animals in the i.n. inoculated group lost no more than 8% of their weight. Neither group showed signs of disease.
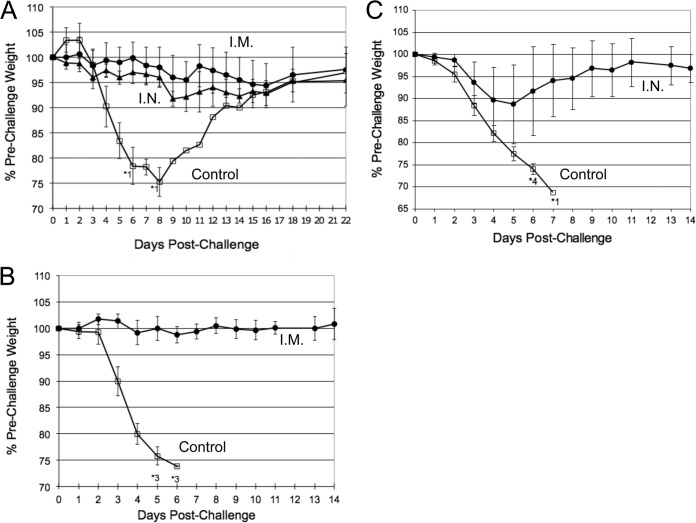
FIG 6.
VSVΔG-H5N1 provides protection against H5N1 challenge. Mice vaccinated with VSVΔG-H5N1 are protected against lethal challenge with the low-pathogenicity HALo influenza challenge virus, a 6:2 gene segment reassortant virus containing HA and NA of VN1203, with the removal of the polybasic cleavage site in HA, and the internal gene segments of PR8. (A) Duration of protective immunity against HALo challenge. Groups of 5 mice vaccinated with 106 PFU of VSVΔG-H5N1 by either the i.m. or i.n. route were challenged with 4 LD50 of HALo influenza virus at 140 days postvaccination. Control mice were a group of 3 unvaccinated age-matched mice. (B) Challenge experiments utilizing higher-dose (1.25 × 107 PFU) i.m. vaccination with VSVΔG-H5N1 and a shorter interval to challenge. Groups of 6 mice were vaccinated i.m. with 1.25 × 107 PFU of either VSVΔG-H5N1 or VSVΔG-G(NiV) (VSVΔG expressing the G glycoprotein of Nipah virus) (control group). Mice were challenged with 10 LD50 of HALo influenza virus at 34 days postvaccination. (C) Short-interval challenge to establish if rapid protection against lethal challenge can be achieved. Groups of 5 mice were vaccinated i.n. with either 1.25 × 107 PFU of VSVΔG-H5N1 or 106 PFU of VSV-EGFP (control group). Mice were challenged with 10 LD50 of HALo influenza virus at 14 days postvaccination. Error bars represent 1 standard deviation above and below the average weight. Asterisks indicate the number of animals that died at the given time points.
We next repeated this challenge study using a single high-dose i.m. vaccination of six mice with 1.25 × 107 PFU VSVΔG-H5N1 and a control group of six animals. The animals were challenged at 34 days postvaccination with 10 LD50 of HALo. All control animals died by day 6, while all vaccinated animals were completely protected and showed no weight loss. In a separate study designed to determine how rapidly protection could be achieved, mice were vaccinated i.n. with high-dose VSVΔG-H5N1 (1.25 × 107 PFU) and challenged at 14 days postvaccination with 10 LD50 of HALo. All vaccinated mice were protected from challenge (Fig. 6C), although there was a modest amount of weight loss recorded, with an average maximal weight loss of ∼11% on postchallenge day 5. In contrast, control mice rapidly lost weight, and all control mice died by day 7 postchallenge.
DISCUSSION
Although there are multiple reports of pseudotyped viruses that are capable of a single round of infection after complementation with influenza virus HA (54–58), the pseudotypes are not capable of multiple cycles of replication. The recombinant VSVΔG expressing an H5 HA and an N1 NA that we describe here is replication competent in tissue culture and generates single-dose protective immunity to a lethal H5N1 challenge in mice. The use of a replication-competent vector expressing the influenza virus HA and NA proteins in place of VSV G has the major advantage of not inducing vector-specific NAbs and could facilitate the use of the same vector for multiple influenza vaccines. Other VSV vector-based vaccination schemes require exchanging the G glycoprotein for that of a distinct serotype in order to avoid neutralization of boosting constructs by preexisting NAbs directed at VSV G (59). VSVΔG vaccines are not subject to this limitation.
Another group recently described the construction of replication-competent VSVΔG recombinants expressing HA and NA (termed pseudotypes), but these were not tested in animals (60). As in our studies, the HA used in these hybrid VSVs was derived from a HPAIV strain containing a polybasic cleavage site. This site presumably facilitates the growth of the recombinant virus because there is efficient HA cleavage by cellular proteases.
Recombinant wild-type VSV and VSV recombinants are nonpathogenic when given by the i.m. route but can be pathogenic in mice when given by the i.n. route because they spread systemically and can cause encephalitis (33, 61, 62). Highly attenuated VSV vectors that lack detectable neurovirulence and are nonpathogenic have been developed (63–65). Initial clinical trials utilizing the attenuated VSV vector as an HIV-1 vaccine candidate in humans have shown no significant adverse events, even at very high doses (HVTN 090 study [http://clinicaltrials.gov/ct2/show/NCT01438606]). Furthermore, multiple VSVΔG vaccines have been shown to be nonpathogenic, even those that have in vitro growth capabilities restored by the addition of other viral surface glycoproteins from highly pathogenic viruses such as Ebola, Marburg, and chikungunya viruses (23, 39, 66). Given the high virulence of many HPAIV strains that have been isolated, there is concern that hybrid viruses containing components of HPAIV, especially replication-competent viruses such as VSVΔG-H5N1, may have increased virulence; however, it is clear that the expression of HA alone from HPAIVs did not confer pathogenicity to VSV in animal models, even when utilizing complete VSV-HPAIV HA strains (27, 28, 52). Our experiments additionally confirm that VSVΔG-H5N1 strains were nonpathogenic when administered i.n. to mice. We were not able to recover any VSVΔG-H5N1 from animals given this recombinant i.n. or i.m, indicating that it does not replicate to detectable levels in vivo. Thus, this construct appears to have a novel ability to replicate efficiently in vitro while being nonpathogenic in an animal model.
Given the rapid spread and length of circulation of newly emergent influenza viruses, vaccine-induced protection should ideally be achieved rapidly and be of a relatively long duration. The VSVΔG-H5N1 vaccine that we describe appears to possess both of these properties: i.n. vaccination protected mice against lethal challenge after 14 and 140 days postvaccination. Additionally, the i.m. route of vaccination, which has been shown to be even more effective than i.n. vaccinations at generating both immune responses and protection in other VSVΔG models (37, 67), completely protected mice against lethal influenza virus challenge at an intermediate time point. While we anticipate that H5 HA-specific antibodies mediate protection against the challenge virus, it is possible that there is an additional contribution from NA-specific antibodies, which were also quite robust in our experiments. Overall, these results suggest that this novel vaccine candidate is safe and effective after a single i.n. or i.m. dose. Because VSVΔG-H5N1 can be grown rapidly in tissue culture without the need for complementation, it could be produced rapidly in large quantities in response to an influenza pandemic.
Beyond its use as a vaccine candidate, the unique growth properties and apparent lack of pathogenicity of VSVΔG-H5N1 open the door to other potentially useful applications, including finding utility as a clinical and laboratory reagent for assays that would normally be precluded by biosafety level requirements. New applications for this construct as well as additional vaccination strategies are currently being explored.
ACKNOWLEDGMENTS
We thank Peter Palese for contributing influenza virus reagents and advice regarding experimental design. Microneutralization assays were performed in the laboratory of Kanta Subbarao.
This study was supported by NIH grant R01-AI080781 and by the Division of Intramural Research of the National Institute of Allergy and Infectious Diseases (NIAID), NIH. Alex B. Ryder was supported by Yale University School of Medicine NRSA training grant 5T32HL007974-13. Florian Krammer was supported by an Erwin Schrödinger fellowship (J3232) from the Austrian Science Fund (FWF).
REFERENCES
- 1.Krammer F, Hai R, Yondola M, Tan GS, Leyva-Grado VH, Ryder AB, Miller MS, Rose JK, Palese P, Garcia-Sastre A, Albrecht RA. 2014. Assessment of influenza virus hemagglutinin stalk-based immunity in ferrets. J Virol 88:3432–3442. doi: 10.1128/JVI.03004-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balazs AB, Bloom JD, Hong CM, Rao DS, Baltimore D. 2013. Broad protection against influenza infection by vectored immunoprophylaxis in mice. Nat Biotechnol 31:647–652. doi: 10.1038/nbt.2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hessel A, Savidis-Dacho H, Coulibaly S, Portsmouth D, Kreil TR, Crowe BA, Schwendinger MG, Pilz A, Barrett PN, Falkner FG, Schafer B. 2014. MVA vectors expressing conserved influenza proteins protect mice against lethal challenge with H5N1, H9N2 and H7N1 viruses. PLoS One 9:e88340. doi: 10.1371/journal.pone.0088340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frey SE, Reyes MR, Reynales H, Bermal NN, Nicolay U, Narasimhan V, Forleo-Neto E, Arora AK. 2014. Comparison of the safety and immunogenicity of an MF59-adjuvanted with a non-adjuvanted seasonal influenza vaccine in elderly subjects. Vaccine 32:5027–5034. doi: 10.1016/j.vaccine.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 5.Perez-Giron JV, Belicha-Villanueva A, Hassan E, Gomez-Medina S, Cruz JL, Ludtke A, Ruibal P, Albrecht RA, Garcia-Sastre A, Munoz-Fontela C. 2014. Mucosal polyinosinic-polycytidylic acid improves protection elicited by replicating influenza vaccines via enhanced dendritic cell function and T cell immunity. J Immunol 193:1324–1332. doi: 10.4049/jimmunol.1400222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McElhaney JE, Beran J, Devaster JM, Esen M, Launay O, Leroux-Roels G, Ruiz-Palacios GM, van Essen GA, Caplanusi A, Claeys C, Durand C, Duval X, El Idrissi M, Falsey AR, Feldman G, Frey SE, Galtier F, Hwang SJ, Innis BL, Kovac M, Kremsner P, McNeil S, Nowakowski A, Richardus JH, Trofa A, Oostvogels L. 2013. AS03-adjuvanted versus non-adjuvanted inactivated trivalent influenza vaccine against seasonal influenza in elderly people: a phase 3 randomised trial. Lancet Infect Dis 13:485–496. doi: 10.1016/S1473-3099(13)70046-X. [DOI] [PubMed] [Google Scholar]
- 7.Wang J, Shah D, Chen X, Anderson RR, Wu MX. 2014. A micro-sterile inflammation array as an adjuvant for influenza vaccines. Nat Commun 5:4447. doi: 10.1038/ncomms5447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koutsonanos DG, Vassilieva EV, Stavropoulou A, Zarnitsyn VG, Esser ES, Taherbhai MT, Prausnitz MR, Compans RW, Skountzou I. 2012. Delivery of subunit influenza vaccine to skin with microneedles improves immunogenicity and long-lived protection. Sci Rep 2:357. doi: 10.1038/srep00357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pushko P, Pearce MB, Ahmad A, Tretyakova I, Smith G, Belser JA, Tumpey TM. 2011. Influenza virus-like particle can accommodate multiple subtypes of hemagglutinin and protect from multiple influenza types and subtypes. Vaccine 29:5911–5918. doi: 10.1016/j.vaccine.2011.06.068. [DOI] [PubMed] [Google Scholar]
- 10.Kanekiyo M, Wei CJ, Yassine HM, McTamney PM, Boyington JC, Whittle JR, Rao SS, Kong WP, Wang L, Nabel GJ. 2013. Self-assembling influenza nanoparticle vaccines elicit broadly neutralizing H1N1 antibodies. Nature 499:102–106. doi: 10.1038/nature12202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mallajosyula VV, Citron M, Ferrara F, Lu X, Callahan C, Heidecker GJ, Sarma SP, Flynn JA, Temperton NJ, Liang X, Varadarajan R. 2014. Influenza hemagglutinin stem-fragment immunogen elicits broadly neutralizing antibodies and confers heterologous protection. Proc Natl Acad Sci U S A 111:E2514–E2523. doi: 10.1073/pnas.1402766111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen H, Angel M, Li W, Finch C, Gonzalez AS, Sutton T, Santos J, Perez DR. 2014. All-in-one bacmids: an efficient reverse genetics strategy for influenza A virus vaccines. J Virol 88:10013–10025. doi: 10.1128/JVI.01468-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klenk HD, Rott R, Orlich M, Blodorn J. 1975. Activation of influenza A viruses by trypsin treatment. Virology 68:426–439. doi: 10.1016/0042-6822(75)90284-6. [DOI] [PubMed] [Google Scholar]
- 14.Bogs J, Veits J, Gohrbandt S, Hundt J, Stech O, Breithaupt A, Teifke JP, Mettenleiter TC, Stech J. 2010. Highly pathogenic H5N1 influenza viruses carry virulence determinants beyond the polybasic hemagglutinin cleavage site. PLoS One 5:e11826. doi: 10.1371/journal.pone.0011826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Munster VJ, Schrauwen EJ, de Wit E, van den Brand JM, Bestebroer TM, Herfst S, Rimmelzwaan GF, Osterhaus AD, Fouchier RA. 2010. Insertion of a multibasic cleavage motif into the hemagglutinin of a low-pathogenic avian influenza H6N1 virus induces a highly pathogenic phenotype. J Virol 84:7953–7960. doi: 10.1128/JVI.00449-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suguitan AL Jr, Matsuoka Y, Lau YF, Santos CP, Vogel L, Cheng LI, Orandle M, Subbarao K. 2012. The multibasic cleavage site of the hemagglutinin of highly pathogenic A/Vietnam/1203/2004 (H5N1) avian influenza virus acts as a virulence factor in a host-specific manner in mammals. J Virol 86:2706–2714. doi: 10.1128/JVI.05546-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Veits J, Weber S, Stech O, Breithaupt A, Graber M, Gohrbandt S, Bogs J, Hundt J, Teifke JP, Mettenleiter TC, Stech J. 2012. Avian influenza virus hemagglutinins H2, H4, H8, and H14 support a highly pathogenic phenotype. Proc Natl Acad Sci U S A 109:2579–2584. doi: 10.1073/pnas.1109397109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martin V, Pfeiffer DU, Zhou X, Xiao X, Prosser DJ, Guo F, Gilbert M. 2011. Spatial distribution and risk factors of highly pathogenic avian influenza (HPAI) H5N1 in China. PLoS Pathog 7:e1001308. doi: 10.1371/journal.ppat.1001308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gilbert M, Newman SH, Takekawa JY, Loth L, Biradar C, Prosser DJ, Balachandran S, Subba Rao MV, Mundkur T, Yan B, Xing Z, Hou Y, Batbayar N, Natsagdorj T, Hogerwerf L, Slingenbergh J, Xiao X. 2010. Flying over an infected landscape: distribution of highly pathogenic avian influenza H5N1 risk in South Asia and satellite tracking of wild waterfowl. Ecohealth 7:448–458. doi: 10.1007/s10393-010-0672-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang X, Fang S, Lu X, Xu C, Cowling BJ, Tang X, Peng B, Wu W, He J, Tang Y, Xie X, Mei S, Kong D, Zhang R, Ma H, Cheng J. 2014. Seroprevalence to avian influenza A(H7N9) virus among poultry workers and the general population in southern China: a longitudinal study. Clin Infect Dis 59:e76–e83. doi: 10.1093/cid/ciu399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel RB, Mathur MB, Gould M, Uyeki TM, Bhattacharya J, Xiao Y, Khazeni N. 2014. Demographic and clinical predictors of mortality from highly pathogenic avian influenza A (H5N1) virus infection: CART analysis of international cases. PLoS One 9:e91630. doi: 10.1371/journal.pone.0091630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liang L, Xu B, Chen Y, Liu Y, Cao W, Fang L, Feng L, Goodchild MF, Gong P. 2010. Combining spatial-temporal and phylogenetic analysis approaches for improved understanding on global H5N1 transmission. PLoS One 5:e13575. doi: 10.1371/journal.pone.0013575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chattopadhyay A, Wang E, Seymour R, Weaver SC, Rose JK. 2013. A chimeric vesiculo/alphavirus is an effective alphavirus vaccine. J Virol 87:395–402. doi: 10.1128/JVI.01860-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schell JB, Rose NF, Bahl K, Diller K, Buonocore L, Hunter M, Marx PA, Gambhira R, Tang H, Montefiori DC, Johnson WE, Rose JK. 2011. Significant protection against high-dose simian immunodeficiency virus challenge conferred by a new prime-boost vaccine regimen. J Virol 85:5764–5772. doi: 10.1128/JVI.00342-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cobleigh MA, Buonocore L, Uprichard SL, Rose JK, Robek MD. 2010. A vesicular stomatitis virus-based hepatitis B virus vaccine vector provides protection against challenge in a single dose. J Virol 84:7513–7522. doi: 10.1128/JVI.00200-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brandsma JL, Shlyankevich M, Su Y, Zelterman D, Rose JK, Buonocore L. 2010. Reversal of papilloma growth in rabbits therapeutically vaccinated against E6 with naked DNA and/or vesicular stomatitis virus vectors. Vaccine 28:8345–8351. doi: 10.1016/j.vaccine.2009.04.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schwartz JA, Buonocore L, Suguitan A Jr, Hunter M, Marx PA, Subbarao K, Rose JK. 2011. Vesicular stomatitis virus-based H5N1 avian influenza vaccines induce potent cross-clade neutralizing antibodies in rhesus macaques. J Virol 85:4602–4605. doi: 10.1128/JVI.02491-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwartz JA, Buonocore L, Suguitan AL Jr, Silaghi A, Kobasa D, Kobinger G, Feldmann H, Subbarao K, Rose JK. 2010. Potent vesicular stomatitis virus-based avian influenza vaccines provide long-term sterilizing immunity against heterologous challenge. J Virol 84:4611–4618. doi: 10.1128/JVI.02637-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chattopadhyay A, Park S, Delmas G, Suresh R, Senina S, Perlin DS, Rose JK. 2008. Single-dose, virus-vectored vaccine protection against Yersinia pestis challenge: CD4+ cells are required at the time of challenge for optimal protection. Vaccine 26:6329–6337. doi: 10.1016/j.vaccine.2008.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kapadia SU, Simon ID, Rose JK. 2008. SARS vaccine based on a replication-defective recombinant vesicular stomatitis virus is more potent than one based on a replication-competent vector. Virology 376:165–172. doi: 10.1016/j.virol.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kahn JS, Roberts A, Weibel C, Buonocore L, Rose JK. 2001. Replication-competent or attenuated, nonpropagating vesicular stomatitis viruses expressing respiratory syncytial virus (RSV) antigens protect mice against RSV challenge. J Virol 75:11079–11087. doi: 10.1128/JVI.75.22.11079-11087.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rose NF, Marx PA, Luckay A, Nixon DF, Moretto WJ, Donahoe SM, Montefiori D, Roberts A, Buonocore L, Rose JK. 2001. An effective AIDS vaccine based on live attenuated vesicular stomatitis virus recombinants. Cell 106:539–549. doi: 10.1016/S0092-8674(01)00482-2. [DOI] [PubMed] [Google Scholar]
- 33.Roberts A, Buonocore L, Price R, Forman J, Rose JK. 1999. Attenuated vesicular stomatitis viruses as vaccine vectors. J Virol 73:3723–3732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Publicover J, Ramsburg E, Rose JK. 2005. A single-cycle vaccine vector based on vesicular stomatitis virus can induce immune responses comparable to those generated by a replication-competent vector. J Virol 79:13231–13238. doi: 10.1128/JVI.79.21.13231-13238.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lo MK, Bird BH, Chattopadhyay A, Drew CP, Martin BE, Coleman JD, Rose JK, Nichol ST, Spiropoulou CF. 2014. Single-dose replication-defective VSV-based Nipah virus vaccines provide protection from lethal challenge in Syrian hamsters. Antiviral Res 101:26–29. doi: 10.1016/j.antiviral.2013.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gunther S, Feldmann H, Geisbert TW, Hensley LE, Rollin PE, Nichol ST, Stroher U, Artsob H, Peters CJ, Ksiazek TG, Becker S, ter Meulen J, Olschlager S, Schmidt-Chanasit J, Sudeck H, Burchard GD, Schmiedel S. 2011. Management of accidental exposure to Ebola virus in the biosafety level 4 laboratory, Hamburg, Germany. J Infect Dis 204(Suppl 3):S785–S790. doi: 10.1093/infdis/jir298. [DOI] [PubMed] [Google Scholar]
- 37.Chattopadhyay A, Rose JK. 2011. Complementing defective viruses that express separate paramyxovirus glycoproteins provide a new vaccine vector approach. J Virol 85:2004–2011. doi: 10.1128/JVI.01852-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boritz E, Gerlach J, Johnson JE, Rose JK. 1999. Replication-competent rhabdoviruses with human immunodeficiency virus type 1 coats and green fluorescent protein: entry by a pH-independent pathway. J Virol 73:6937–6945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Geisbert TW, Daddario-Dicaprio KM, Geisbert JB, Reed DS, Feldmann F, Grolla A, Stroher U, Fritz EA, Hensley LE, Jones SM, Feldmann H. 2008. Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with Ebola and Marburg viruses. Vaccine 26:6894–6900. doi: 10.1016/j.vaccine.2008.09.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Steel J, Lowen AC, Pena L, Angel M, Solorzano A, Albrecht R, Perez DR, Garcia-Sastre A, Palese P. 2009. Live attenuated influenza viruses containing NS1 truncations as vaccine candidates against H5N1 highly pathogenic avian influenza. J Virol 83:1742–1753. doi: 10.1128/JVI.01920-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lefrancois L, Lyles DS. 1982. The interaction of antibody with the major surface glycoprotein of vesicular stomatitis virus. II. Monoclonal antibodies of nonneutralizing and cross-reactive epitopes of Indiana and New Jersey serotypes. Virology 121:168–174. [DOI] [PubMed] [Google Scholar]
- 42.Lawson ND, Stillman EA, Whitt MA, Rose JK. 1995. Recombinant vesicular stomatitis viruses from DNA. Proc Natl Acad Sci U S A 92:4477–4481. doi: 10.1073/pnas.92.10.4477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schnell MJ, Johnson JE, Buonocore L, Rose JK. 1997. Construction of a novel virus that targets HIV-1-infected cells and controls HIV-1 infection. Cell 90:849–857. doi: 10.1016/S0092-8674(00)80350-5. [DOI] [PubMed] [Google Scholar]
- 44.Fuerst TR, Niles EG, Studier FW, Moss B. 1986. Eukaryotic transient-expression system based on recombinant vaccinia virus that synthesizes bacteriophage T7 RNA polymerase. Proc Natl Acad Sci U S A 83:8122–8126. doi: 10.1073/pnas.83.21.8122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Okuma K, Matsuura Y, Tatsuo H, Inagaki Y, Nakamura M, Yamamoto N, Yanagi Y. 2001. Analysis of the molecules involved in human T-cell leukaemia virus type 1 entry by a vesicular stomatitis virus pseudotype bearing its envelope glycoproteins. J Gen Virol 82:821–830. [DOI] [PubMed] [Google Scholar]
- 46.Suguitan AL Jr, McAuliffe J, Mills KL, Jin H, Duke G, Lu B, Luke CJ, Murphy B, Swayne DE, Kemble G, Subbarao K. 2006. Live, attenuated influenza A H5N1 candidate vaccines provide broad cross-protection in mice and ferrets. PLoS Med 3:e360. doi: 10.1371/journal.pmed.0030360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ramsburg E, Publicover J, Buonocore L, Poholek A, Robek M, Palin A, Rose JK. 2005. A vesicular stomatitis virus recombinant expressing granulocyte-macrophage colony-stimulating factor induces enhanced T-cell responses and is highly attenuated for replication in animals. J Virol 79:15043–15053. doi: 10.1128/JVI.79.24.15043-15053.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Simon ID, van Rooijen N, Rose JK. 2010. Vesicular stomatitis virus genomic RNA persists in vivo in the absence of viral replication. J Virol 84:3280–3286. doi: 10.1128/JVI.02052-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Niwa H, Yamamura K, Miyazaki J. 1991. Efficient selection for high-expression transfectants with a novel eukaryotic vector. Gene 108:193–199. doi: 10.1016/0378-1119(91)90434-D. [DOI] [PubMed] [Google Scholar]
- 50.Palese P, Tobita K, Ueda M, Compans RW. 1974. Characterization of temperature sensitive influenza virus mutants defective in neuraminidase. Virology 61:397–410. doi: 10.1016/0042-6822(74)90276-1. [DOI] [PubMed] [Google Scholar]
- 51.Iverson LE, Rose JK. 1981. Localized attenuation and discontinuous synthesis during vesicular stomatitis virus transcription. Cell 23:477–484. doi: 10.1016/0092-8674(81)90143-4. [DOI] [PubMed] [Google Scholar]
- 52.Schwartz JA, Buonocore L, Roberts A, Suguitan A Jr, Kobasa D, Kobinger G, Feldmann H, Subbarao K, Rose JK. 2007. Vesicular stomatitis virus vectors expressing avian influenza H5 HA induce cross-neutralizing antibodies and long-term protection. Virology 366:166–173. doi: 10.1016/j.virol.2007.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Leroux-Roels I, Van der Wielen M, Kafeja F, Vandermeulen C, Lazarus R, Snape MD, John T, Carre C, Nougarede N, Pepin S, Leroux-Roels G, Hoppenbrouwers K, Pollard AJ, Van Damme P. 2009. Humoral and cellular immune responses to split-virion H5N1 influenza vaccine in young and elderly adults. Vaccine 27:6918–6925. doi: 10.1016/j.vaccine.2009.08.110. [DOI] [PubMed] [Google Scholar]
- 54.Cheresiz SV, Kononova AA, Razumova YV, Dubich TS, Chepurnov AA, Kushch AA, Davey R, Pokrovsky AG. 2014. A vesicular stomatitis pseudovirus expressing the surface glycoproteins of influenza A virus. Arch Virol 159:2651–2658. doi: 10.1007/s00705-014-2127-y. [DOI] [PubMed] [Google Scholar]
- 55.Kalhoro NH, Veits J, Rautenschlein S, Zimmer G. 2009. A recombinant vesicular stomatitis virus replicon vaccine protects chickens from highly pathogenic avian influenza virus (H7N1). Vaccine 27:1174–1183. doi: 10.1016/j.vaccine.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 56.Halbherr SJ, Brostoff T, Tippenhauer M, Locher S, Berger Rentsch M, Zimmer G. 2013. Vaccination with recombinant RNA replicon particles protects chickens from H5N1 highly pathogenic avian influenza virus. PLoS One 8:e66059. doi: 10.1371/journal.pone.0066059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Haynes JR, Dokken L, Wiley JA, Cawthon AG, Bigger J, Harmsen AG, Richardson C. 2009. Influenza-pseudotyped Gag virus-like particle vaccines provide broad protection against highly pathogenic avian influenza challenge. Vaccine 27:530–541. doi: 10.1016/j.vaccine.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 58.Nefkens I, Garcia JM, Ling CS, Lagarde N, Nicholls J, Tang DJ, Peiris M, Buchy P, Altmeyer R. 2007. Hemagglutinin pseudotyped lentiviral particles: characterization of a new method for avian H5N1 influenza sero-diagnosis. J Clin Virol 39:27–33. doi: 10.1016/j.jcv.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 59.Rose NF, Roberts A, Buonocore L, Rose JK. 2000. Glycoprotein exchange vectors based on vesicular stomatitis virus allow effective boosting and generation of neutralizing antibodies to a primary isolate of human immunodeficiency virus type 1. J Virol 74:10903–10910. doi: 10.1128/JVI.74.23.10903-10910.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zimmer G, Locher S, Berger Rentsch M, Halbherr SJ. 2014. Pseudotyping of vesicular stomatitis virus with the envelope glycoproteins of highly pathogenic avian influenza viruses. J Gen Virol 95:1634–1639. doi: 10.1099/vir.0.065201-0. [DOI] [PubMed] [Google Scholar]
- 61.Publicover J, Ramsburg E, Rose JK. 2004. Characterization of nonpathogenic, live, viral vaccine vectors inducing potent cellular immune responses. J Virol 78:9317–9324. doi: 10.1128/JVI.78.17.9317-9324.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Roberts A, Rose JK. 1998. Recovery of negative-strand RNA viruses from plasmid DNAs: a positive approach revitalizes a negative field. Virology 247:1–6. doi: 10.1006/viro.1998.9250. [DOI] [PubMed] [Google Scholar]
- 63.Cooper D, Wright KJ, Calderon PC, Guo M, Nasar F, Johnson JE, Coleman JW, Lee M, Kotash C, Yurgelonis I, Natuk RJ, Hendry RM, Udem SA, Clarke DK. 2008. Attenuation of recombinant vesicular stomatitis virus-human immunodeficiency virus type 1 vaccine vectors by gene translocations and G gene truncation reduces neurovirulence and enhances immunogenicity in mice. J Virol 82:207–219. doi: 10.1128/JVI.01515-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Johnson JE, Nasar F, Coleman JW, Price RE, Javadian A, Draper K, Lee M, Reilly PA, Clarke DK, Hendry RM, Udem SA. 2007. Neurovirulence properties of recombinant vesicular stomatitis virus vectors in non-human primates. Virology 360:36–49. doi: 10.1016/j.virol.2006.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Clarke DK, Nasar F, Lee M, Johnson JE, Wright K, Calderon P, Guo M, Natuk R, Cooper D, Hendry RM, Udem SA. 2007. Synergistic attenuation of vesicular stomatitis virus by combination of specific G gene truncations and N gene translocations. J Virol 81:2056–2064. doi: 10.1128/JVI.01911-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Geisbert TW, Feldmann H. 2011. Recombinant vesicular stomatitis virus-based vaccines against Ebola and Marburg virus infections. J Infect Dis 204(Suppl 3):S1075–S1081. doi: 10.1093/infdis/jir349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Simon ID, Publicover J, Rose JK. 2007. Replication and propagation of attenuated vesicular stomatitis virus vectors in vivo: vector spread correlates with induction of immune responses and persistence of genomic RNA. J Virol 81:2078–2082. doi: 10.1128/JVI.02525-06. [DOI] [PMC free article] [PubMed] [Google Scholar]