Abstract
Objective
To conduct a systematic review of the effects of frequent family meals on psychosocial outcomes in children and adolescents, and to examine whether there are differences in outcomes between males and females.
Data sources
Studies were identified through a search of MEDLINE (1948 to fifth week of June 2011) and PsycINFO (1806 to first week of July 2011) using the Ovid interface. The MeSH terms and key words used both alone and in combination were family, meal, food intake, nutrition, diets, body weight, adolescent attitudes, eating behaviour, feeding behaviour, and eating disorders. Bibliographies of papers deemed relevant were also reviewed.
Study selection
The original search yielded 1783 articles. To be included in the analysis, studies had to meet the following criteria: have been published in a peer-reviewed journal in English; involve children or adolescents; discuss the role of family meals on the psychosocial outcomes (eg, substance use, disordered eating, depression) of children or adolescents; and have an adequate study design, including appropriate statistical methods for analyzing outcome data. Fourteen papers met inclusion criteria. Two independent reviewers studied and analyzed the papers.
Synthesis
Overall, results show that frequent family meals are inversely associated with disordered eating, alcohol and substance use, violent behaviour, and feelings of depression or thoughts of suicide in adolescents. There is a positive relationship between frequent family meals and increased self-esteem and school success. Studies show substantial differences in outcomes for male and female children and adolescents, with females having more positive results.
Conclusion
This systematic review provides further support that frequent family meals should be endorsed. All health care practitioners should educate families on the benefits of having regular meals together as a family.
Psychosocial dysfunction has become widely acknowledged as the most common chronic condition among children and adolescents.1,2 Given that adolescents’ psychosocial health problems have implications for adult morbidity, mortality,3 and development of other diseases,4,5 investigating methods that affect and alter the course of these issues merits attention. Adolescents’ healthy development is influenced by myriad family factors.6 Healthy family environments, including family connectedness (ie, feelings of love, warmth, and caring from parents) have been found to be protective against poor mental health or psychosocial outcomes, and the role of the family has long been studied as an important contribution to adolescent well-being.7–9 Interestingly, there is evidence that young males might respond differently than females do to family environments and dynamics.10–13
A simple, nonintrusive intervention that could easily be applied to increase healthy family environments is engaging in family meals. Family meals might serve as an arena for augmenting family cohesion,14–16 stability,17 and connectedness,8 or for enhancing adolescent developmental assets,18 such as problem-focused coping15 and social-emotional development.8 Moreover, family rituals and routines, like the family meal, might offer consistency and a venue for checking in with family members, and for learning and teaching healthy food behaviour and attitudes.19
Recent interest has been dedicated to investigating the importance of family meals and their positive effects on child and adolescent nutritional outcomes. Current research suggests that eating meals together as a family is beneficial to adolescents’ eating habits and that more frequent family meals have been found to lead to better dietary intake among children and adolescents.20–25 Several studies have also examined the relationship between family meals and children being overweight or obese with inconsistent results.26–29 One study reported that a higher frequency of family meals was associated with reduced odds of being overweight and of becoming overweight in the future,26 while other reports found that the frequency of family dinners was inversely associated with overweight status at baseline, but not with the likelihood of becoming overweight in the future.27,28
Researchers have also begun to study the role of family meals on markers of adolescent well-being, such as rates of substance use and disordered eating behaviour.19,30 These studies appear to vary in design and scope. A recent review by Skeer and Ballard looking at family meals and adolescent risk prevention showed a generally positive relationship between frequent family meals and decreased adolescent engagement in risk behaviour.31 The review also mentioned that adolescents’ sex had a substantial role in this relationship; sex seemed to influence the strength of family meals’ protective effects on risk behaviour, with female adolescents benefiting more than male adolescents did.
To our knowledge, no systematic review has been completed on the relationship between family meals and psychosocial outcomes in children and adolescents. As such, the purpose of this paper was to conduct a systematic review of the effects of family meals on psychosocial outcomes in children and adolescents, and to examine whether differences in outcomes between males and females have been studied. A study of this nature has the potential to increase knowledge of the importance of frequent family meals while providing evidence in support of an easy-to-implement prevention strategy or adjunctive treatment intervention.
DATA SOURCES
Studies were identified through a MEDLINE search (1948 to the fifth week of June 2011) and PsycINFO (1806 to first week of July 2011) using the Ovid interface. No date, language, age, or study design limits were imposed on the search. The bibliographies of papers deemed relevant were also reviewed for further relevant papers.
Study selection
To be included in the analysis, studies had to meet the following criteria: have been published in a peer-reviewed journal in English; involve children or adolescents; discuss the role of family meals on the psychosocial outcomes (eg, substance use, disordered eating, depression) of children or adolescents; and have an adequate study design that allowed for the relationship between family meals and psychosocial outcomes to be studied directly, including cross-sectional or longitudinal cohort studies and randomized control trials. Case studies, commentaries, and narrative reviews were excluded. Additionally, study design had to include appropriate statistical methods for analyzing outcome data. As the purpose of this review was to assess the effects of family meals on the psychosocial health outcomes of children and adolescents, studies were excluded if they only focused on the effect of family meals in the context of treatment, such as for eating disorders.
Two authors (M.H., H.W.) reviewed and compared the studies that met inclusion criteria for the following: study purpose, study sample and demographic characteristics, study design (longitudinal vs cross-sectional), and effect of family meals on outcomes measured (P ≤ .05 was used to determine significance). The studies were categorized according to the specified outcomes assessed, as well as differences between males and females.
SYNTHESIS
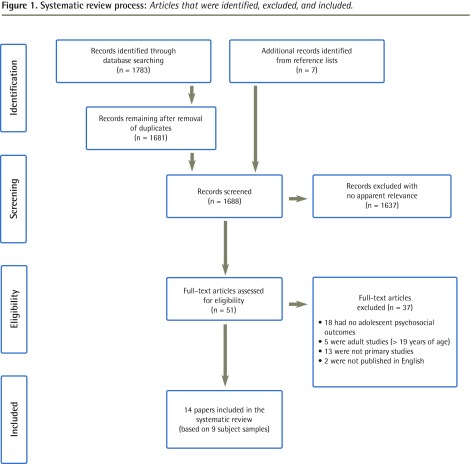
Figure 1 describes the articles that were identified, excluded, and included. Fourteen articles (7 longitudinal and 7 cross-sectional studies) met inclusion criteria (Table 1).15,16,18,19,30,32–40 These 14 articles were based on 9 different subject samples. Five of the papers (3 longitudinal, 2 cross-sectional) used data from Project EAT-I (Eating Among Teens) or EAT-II,19,36,38–40 and 2 longitudinal papers collected data from the Growing Up Today Study project.30,32 Other study data sources included the National Heart, Lung, and Blood Institute Growth and Health Study15 and the Controlling Overweight and Obesity for Life study.33 The remainder of the data were from individual studies. However, there is no duplication of data among these publications, as each article reviewed a different outcome or a specific group of the subject sample. Table 115,16,18,19,30,32–40 shows the data sources, data collection methodology, study response rates, and demographic information. Table 215,16,18,19,30,32–40 presents main findings of the studies reviewed.
Figure 1.
Systematic review process: Articles that were identified, excluded, and included.
Table 1.
Design and characteristics of studies reviewed
| STUDY | N VALUE | DATA SOURCE AND SETTING | PARTICIPANT CHARACTERISTICS | STUDY DESIGN | OUTCOMES MEASURED | DEFINITION OF FFM | PSYCHOSOCIAL MEASURES |
|---|---|---|---|---|---|---|---|
| Franko et al,15 2008 | 2379 | Girls from California, Cincinnati, and Maryland aged 9 or 10 y at study entry who participated in the NGHS | Girls only Mean age at the start of the study was 9.5 y Mean age at 10 y was 18.6 y |
Longitudinal data collected annually for 10 y as part of the NGHS Measures administered in alternating years Participant retention at 10 y was 89% Family meals data were obtained at 1 y and 3 y and the main outcome measures were obtained at 5 y, 6 y, and 10 y |
Disordered eating behaviour, body image concern, and substance use | “How often do you eat with your parent(s)?” FFM not defined |
EDI—the drive for thinness, body dissatisfaction, and bulimia subscales Perceived Stress Scale Family Adaptability and Cohesion Evaluation Scale III— the cohesion subscale Coping Strategies Inventory Various questions to assess FMF and demographic characteristics |
| White and Halliwell,16 2010 | 550 | Students (aged 11–16 y) in grades 7, 9, and 10 from comprehensive state schools based in an urban area of the UK | Ethnically and socioeconomically diverse Males (n = 274), females (n = 276) Mean (SD) age was 14.13 (1.09) y |
Cross-sectional data collected Sex, date of birth, height, weight, and parental employment were self-reported by participants Self-reported questionnaires were used to assess FMF, family connectedness, family mealtime environment, and alcohol and tobacco consumption |
Substance use | “During the past seven days, how many times did all, or most, of your family living in your house eat a meal together?” FFM defined as ≥ 5 times per wk |
Family Eating Attitudes and Behavior Scale Various questions to assess demographic characteristics, FMF, familial factors, and alcohol and tobacco consumption |
| Fulkerson et al,18 2006 | 99 462 | Students in grades 6–12 from public and alternative schools in the US (213 cities, 25 states) | Ethnically diverse Males (n = 49 138), females (n = 49 620) |
Cross-sectional data collected during the 1996–1997 school year Profiles of student life; Attitudes and Behaviors survey administered in classrooms by participating school districts |
Disordered eating behaviour, depressive symptoms or suicidality, self- esteem, academic achievement, substance use, and violent behaviour | 7 times per wk | Profiles of student life; Attitudes and Behaviors survey Various questions chosen to assess substance use, depressive symptoms, suicidality, violence, academic problems, FMF, and demographic variables |
| Neumark-Sztainer et al,19 2004 | 4746 | Adolescents from the urban and suburban school districts of Minneapolis who participated in Project EAT | Ethnically diverse Males and females Mean (SD) age was 14.9 (1.7) y |
Cross-sectional data collected during the 1998–1999 school year Project EAT survey administered by staff (RR 81.5%); height and weight assessed |
Disordered eating behaviour | “During the past 7 days, how many times did all, or most, of your family living in your house eat a meal together?” FFM defined as ≥ 5 meals per wk |
Specific questions developed for the Project EAT study were based on adolescent focus group findings, a review of existing instruments, expert revisions, a social-cognitive theoretical framework, and pilot tests |
| Fisher et al,30 2007 | 5511 | Cohort of children who participated in GUTS across the US GUTS participants are the children of women taking part in the Nurses’ Health Study II |
Males (n = 2228), females (n = 3283) Age range was 11–18 y |
Longitudinal data collected in 1996 and in 1998 and 1999, examining predictors of alcohol initiation and binge drinking Starting in 1996, GUTS follow-up self-report questionnaires were mailed to participants annually In 1998 and 1999, the alcohol use section of the questionnaire was expanded and administered to participants (RR 70%) |
Substance use | “How often do you sit down with other members of your family to eat dinner or supper?” FFM not defined |
Alcohol Expectancy Questionnaire— adolescent version Harter Self-Perception Profile for Children Various questions to assess demographic, family, and social context variables, and alcohol use behaviour |
| Haines et al,32 2010 | 13 448 | Cohort of children who participated in GUTS across the US Participants in GUTS are the children of women taking part in the Nurses’ Health Study II |
Males (n = 5913), females (n = 7535) Mean (SD) age (Time 1) was 11.9 (1.6) y |
Longitudinal data collected in 1996, (Time 1, baseline), 1997 (Time 2), 1998 (Time 3), and 1999 (Time 4) Self-administered questionnaires were mailed to participants annually |
Disordered eating behaviour | “How often do you sit down with other members of your family to eat dinner or supper?” FFM not defined |
Youth Risk Behaviour Surveillance Questionnaire McKnight Risk Factor Survey Various questions to assess variables such as FMF, parental weight teasing, and importance of thinness to parents |
| Fulkerson et al,33 2009 | 145 | At-risk adolescents from urban and suburban alternative high schools in Minneapolis who participated in the COOL pilot study | Ethnically diverse Males (52%), females (61%) Mean (SD) age was 17.2 (1.2) y |
Cross-sectional data collected in 2006 as baseline data for the Team COOL pilot study Trained research staff administered a psychosocial survey to students during class; height and weight measurements were also recorded |
Disordered eating behaviour, depressive symptoms, and substance use | “During the past week, how many days did all, or most, of the people you live with eat dinner together?” FFM defined as 5–7 meals per wk |
Specific questions came from previously published surveys |
| Sen,34 2010 | 8984 | Youth (aged 12–16 y) who participated in the National Longitudinal Survey of Youth | Nationally representative sample of the US population Youth aged ≤ 14 y as of December 31, 1996, who were living with at least 1 parent Sex numbers not specified |
Longitudinal data collected from 1997 to 2000 | Substance use and violent behaviour | Youth were asked to report the number of days in a typical week their family ate dinner together FFM not defined |
Audio Computer-Assisted Self-Interview |
| Woodruff and Hanning,35 2009 | 3223* | Students in grades 6–8 from 86 schools across northern and southern Ontario and Nova Scotia | Males (n = 1454), females (n = 1548) | Cross-sectional data collected during the 2005–2006 school year Web-based Food Behaviour Questionnaire was administered (RR varied by region or city and ranged from 34%–98%) |
Disordered eating behaviour, body image concern, and self-efficacy | “Typically, how many days per week do you eat dinner or supper with at least one parent?” FFM defined as ≥ 6 d per wk |
Food Behaviour Questionnaire Various questions to assess FMF, body image concern, and self-efficacy |
| Eisenberg et al,36 2004 | 4746 | Adolescents from the urban and suburban school districts of Minneapolis who participated in Project EAT | Ethnically diverse Males and females Mean (SD) age was 14.9 (1.7) y |
Cross-sectional data collected during the 1998–1999 school year Project EAT survey administered by staff during class (RR 81.5%); height and weight assessed |
Self-esteem, academic achievement, depressive symptoms or suicidality, and substance use | “During the past 7 days, how many times did all, or most, of your family living in your house eat a meal together?” FFM defined as ≥ 5 meals per wk |
Rosenberg Self-Esteem Scale Various questions to assess FMF, family factors, academic performance, depression, suicidality, and sociodemographic factors |
| Sierra-Baigrie et al,37 2009 | 259 | Secondary school students aged 12 to 21 y from Avilés, a town in northern Spain | Males (58.3%), females (41.7%) Mean age was 14.72 y |
Cross-sectional data were collected in the form of various self-reported questionnaires assessing topics including bulimic symptomatology, psychosocial competencies, emotional and behavioural problems, and family meal patterns Researchers administered the questionnaires within classrooms to students in groups of 25–30 |
Disordered eating behaviour | “With what frequency do you eat the midday meal at the table with the family members who are at home?” “With what frequency do you eat the evening meal at the table with the family members who are at home?” FFM not defined |
Bulimic Investigatory Test, Edinburgh Youth self-report Various questions to assess FMF and binge-eating episodes |
| Neumark-Sztainer et al,38 2008 | 2516 | Adolescents from urban and suburban school districts in Minneapolis who participated in Project EAT-I and Project EAT-II | Ethnically and socioeconomically diverse Males (n = 1130), females (n = 1386) Mean (SD) age of middle school participants: Time 1 was 12.8 (0.8) y; Time 2 was 17.2 (0.6) y Mean (SD) age of high school participants: Time 1 was 15.8 (0.8) y; and Time 2 was 20.4 (0.8) y |
Longitudinal data collected during the 1998–1999 school year (Time 1) and again in 2003–2004 (Time 2) Time 1: Project EAT-I survey administered by staff (RR 81.5%) Time 2: Project EAT-II survey distributed via mail and self-administered (RR 68.4%) |
Disordered eating behaviour | “During the past 7 days, how many times did all or most of your family living in your house eat a meal together?” FFM defined as ≥ 5 meals wk |
Specific questions developed for the Project EAT study were based on adolescent focus group findings, a review of existing instruments, expert revisions, a social-cognitive theoretical framework, and pilot tests |
| Neumark- Sztainer et al,39 2007 | 2516† | Adolescents from urban and suburban school districts in Minneapolis who participated in Project EAT-I and Project EAT-II | Ethnically and socioeconomically diverse Males (n = 1130), females (n = 1386) Mean (SD) age of middle school participants: Time 1 was 12.8 (0.8) y; Time 2 was 17.2 (0.6) y Mean (SD) age of high school participants: Time 1 was 15.8 (0.8) y; Time 2 was 20.4 (0.8) y |
Longitudinal data collected during the 1998–1999 school year (Time 1) and again in 2003–2004 (Time 2) Time 1: Project EAT-I survey administered by staff (RR 81.5%) Time 2: Project EAT-II survey distributed via mail and self-administered (RR 68.4%) |
Disordered eating behaviour | “During the past 7 days, how many times did all, or most, of your family living in your house eat a meal together?” FFM defined as ≥ 5 meals per wk |
Specific questions developed for the Project EAT study were based on adolescent focus group findings, a review of existing instruments, expert revisions, a social-cognitive theoretical framework, and pilot tests |
| Eisenberg et al,40 2008 | 806 | Adolescents from middle schools (grades 7–8) in Minnesota who participated in Project EAT-I and then in Project EAT-II | Ethnically and socioeconomically diverse Males (n = 366), females (n = 440) Mean (SD) age at Time 1 was 12.8 (0.8) y; at Time 2 was 17.2 (0.6) y |
Longitudinal data collected during the 1998–1999 school year (Time 1) and again in 2003–2004 (Time 2) Time 1: Project EAT-I survey administered by staff Time 2: Project EAT-II survey distributed via mail and self-administered (RR 69.5%) |
Substance use | “During the past 7 days, how many times did all, or most, of your family living in your house eat a meal together?” FFM defined as ≥ 5 meals wk |
Specific questions developed for the Project EAT study were based on adolescent focus group findings, a review of existing instruments, expert revisions, a social-cognitive theoretical framework, and pilot tests |
COOL—Controlling Overweight and Obesity for Life, EDI—Eating Disorders Inventory, FFM—frequent family meals, FMF—family meal frequency, GUTS—Growing Up Today Study, NGHS—National Heart, Lung, and Blood Institute Growth and Health Study, Project EAT—Project Eating Among Teens, RR—response rate, UK—United Kingdom, US—United States.
Results based on a sample size of N = 3025 owing to participant exclusions.
Results are based on a subset of patients who were overweight or who participated in binge eating or extreme weight-control behaviour, which consisted of 577 females and 312 males (total N = 889).
Table 2.
Main findings of studies reviewed: A) Studies in which results differed between sexes; B) Studies in which sex was not specified.
|
A) STUDY IN WHICH RESULTS DIFFERED BETWEEN SEXES |
OUTCOMES MEASURED |
MAIN FINDINGS
|
|
|---|---|---|---|
| FEMALES | MALES | ||
| Franko et al,15 2008 | Disordered eating behaviour, body image concern, and substance use | There was a statistically significant inverse association between FMF and bulimia symptoms, body dissatisfaction, drive for thinness, and cigarette smoking FMF was not significantly associated with extreme weight-control behaviour nor with alcohol consumption |
NA |
| Neumark-Sztainer et al,19 2004 | Disordered eating behaviour | There was a statistically significant inverse association between FMF and extreme and less extreme weight-control behaviour and chronic dieting FMF was not significantly associated with binge eating |
There was a statistically significant inverse association between FMF and extreme and less extreme weight-control behaviour (this relationship with less extreme weight-control behaviour was only present after adjusting for BMI and sociodemographic factors) FMF was not significantly associated with binge eating nor with chronic dieting |
| Fisher et al,30 2007 | Substance use | There was a statistically significant inverse association between FMF and alcohol initiation (ie, girls who ate a family meal every day were 50% less likely to initiate alcohol use than those who ate a family meal some days or never) | FMF was not significantly associated with alcohol initiation |
| Haines et al,32 2010 | Disordered eating behaviour | There was a statistically significant inverse association between FMF and purging, binge eating, and chronic dieting | There was a statistically significant inverse association between FMF and binge eating and FMF and chronic dieting FMF was not significantly associated with purging |
| Sen,34 2010 | Substance use and violent behaviour | There was a statistically significant inverse association between FMF and smoking, marijuana use, alcohol use, and physical violence | There was a statistically significant inverse association between FMF and smoking, marijuana use, alcohol use, and physical violence |
| Neumark-Sztainer et al,38 2008 | Disordered eating behaviour | There was a statistically significant inverse association between FMF and extreme and less extreme weight-control behaviour, binge eating, and chronic dieting | FMF was not significantly associated with extreme weight-control behaviour, binge eating, or chronic dieting FMF was statistically significantly associated with an increased likelihood of less extreme weight-control behaviour (ie, skipping meals and eating very little food) |
| Eisenberg et al,36 2004 | Self-esteem, academic achievement, depressive symptoms or suicidality, and substance use | There was a statistically significant inverse association between FMF and low self-esteem, a low grade point average, high depressive symptoms, suicidal thoughts, suicide attempts, cigarette use, marijuana use, and alcohol use | There was a statistically significant inverse association between FMF and a low grade point average, high depressive symptoms, suicidal thoughts, cigarette use, marijuana use, and alcohol use FMF was not significantly associated with low self-esteem |
| Neumark-Sztainer et al,39 2007 | Disordered eating behaviour | FMF was statistically significantly associated with extreme weight-control behaviour and binge eating | FMF was not significantly associated with extreme weight- control behaviour nor with binge eating |
| Eisenberg et al,40 2008 | Substance use | There was a statistically significant inverse association between FMF and cigarette, marijuana, and alcohol use | FMF was not significantly associated with cigarette, marijuana, and alcohol use |
|
B) STUDY IN WHICH SEX WAS NOT SPECIFIED |
OUTCOMES MEASURED | MAIN FINDINGS | |
|---|---|---|---|
|
| |||
| White and Halliwell,16 2010 | Substance use | There was a statistically significant inverse association between FMF and tobacco smoking and alcohol use | |
| Fulkerson et al,18 2006 | Disordered eating behaviour, depressive symptoms or suicidality, self-esteem, academic achievement, substance use, and violent behaviour | There was a statistically significant inverse association between FMF and purging, binge eating, depression or suicide risk, alcohol use, drug use, tobacco use, and violent behaviour FMF was statistically significantly positively associated with increased self-esteem and increased commitment to learning |
|
| Woodruff and Hanning,35 2009 | Disordered eating behaviour, body image concern, and self-efficacy | No association was found between FMF and dieting There was a statistically significant inverse association between FMF and skipping meals (specifically breakfast) and with concern about high body weight FMF was statistically significantly positively associated with increased self-efficacy for healthy eating both at home with family and at social events with friends |
|
| Fulkerson et al,33 2009 | Disordered eating behaviour, depressive symptoms, and substance use | There was a statistically significant inverse association between FMF and skipping a meal (specifically breakfast) and depressive symptoms FMF was not significantly associated with extreme and less extreme weight-control behaviour, nor with cigarette, marijuana, alcohol, or illicit drug use |
|
| Sierra-Baigrie et al,37 2008 | Disordered eating behaviour | FMF was not significantly associated with binge eating | |
BMI—body mass index, FMF—family meal frequency, NA—not applicable.
Frequency of family meals
The reported family meal frequency rates in the reviewed studies varied from 32.9%16 to 60.6%.34 Reports of infrequent family meals (0 to 2 family meals per week) also varied, ranging from 11%35 to 33.1%.36 The varying results are likely influenced by many different factors (eg, age).24 Three longitudinal studies found that the frequency of family meals decreased as the adolescent progressed toward adulthood.32,34,35 Similarly, other factors such as geographic location and cultural issues have also been shown to affect results. For example, frequent family meals appear to be more common in Spain than in the United States or Britain, with 78% of youth in Spain reporting a high frequency of family meals37 versus only 45% of American youth18,38 and 32.9% of British youth.16 The only Canadian study reports a 70% prevalence of high family meal frequency35; however, it should be noted that the sample in this study is young (grades 6 to 8), which might be a contributing factor to this higher rate.
Disordered eating behaviour
Table 215,16,18,19,30,32–40 presents the main findings of the following discussion. Nine of the 14 studies reviewed explored the relationship between family meal frequency and disordered eating behaviour, including extreme weight-control behaviour (defined as ingestion of diet pills, self-induced vomiting, use of laxatives, or use of diuretics to control weight),15,18,19,32,33,38,39 less extreme weight-control behaviour (defined as fasting, eating very little food, using food substitutes, skipping meals, or smoking cigarettes to control weight),19,33,35,38 binge eating,15,18,19,32,37–39 and chronic dieting.19,32,35,38
In general, some studies report an inverse association between family meal frequency and extreme weight-control behaviour,15,19,32,38,39 less extreme weight-control behaviour,19,38 binge eating,15,32,38,39 and chronic dieting,19,32,38 with most studies maintaining statistically significant findings for females even after adjusting for factors such as family connectedness, sociodemographic characteristics, and personal and behavioural qualities.15,19,32,38,39
Conversely for males, most studies reported no significant association between frequent family meals and extreme weight-control behaviour,19,38,39 binge eating,19,38,39 or chronic dieting.19,38 Additionally, 1 longitudinal study indicated that frequent family meals were statistically significantly associated with a greater likelihood of less extreme weight-control behaviour, both before and after adjusting for a variety of variables.38
Studies that did not specify results by sex showed inconsistent results.18,33,35,37
Externalizing behaviour
Research has explored associations between family meal frequency and externalizing behaviour such as substance use and violence.
Substance use.
The substances examined in these studies included tobacco (cigarette smoking), marijuana, alcohol, and illicit drugs. For females, an inverse association between family meal frequency and use of cigarettes,15,34,36,40 alcohol,30,34,36,40 and marijuana34,36,40 was found, even after adjusting for demographic, familial, and parental characteristics, socioeconomic status, and earlier substance use variables.34,36,40
Study results were less consistent for males. Family meal frequency was negatively associated with cigarette, marijuana, and alcohol use in some studies34,36 but not in others.30,40 Table 215,16,18,19,30,32–40 shows results from studies that did not differentiate between sexes.16,18,33
Violence.
Inverse associations were found in 2 studies between family meal frequency and violence, such as frequency of fighting, hitting, injuring a person, carrying or using a weapon, and threatening physical harm.18,34
Internalizing behaviour
Associations between family meal frequency and internalizing behaviour including body image, self-esteem, academic achievement, and depressive symptoms and suicidal thoughts are discussed here.
Body image concern.
Family meal frequency was inversely associated with both body dissatisfaction and drive for thinness15 and concern about high body weight.35 There were no studies that examined these variables in males.
Self-esteem or self-efficacy.
One study found a negative association between family meal frequency and low self-esteem in females but not in males.36 Another study (not sex specific) reported a positive association between frequent family meals and increased self-esteem, even after controlling for various familial factors,18 while a second study that was also not sex specific reported a positive association between frequent family meals and increased self-efficacy for healthy eating in various social environments.35
Academic achievement.
Frequent family meals were positively associated with a higher grade point average in both females and males in one study, and statistical significance was maintained in the female sample even after controlling for various demographic and familial factors. 36 Another study found a similar association between family meal frequency and commitment to learning, which also remained statistically significant after adjusting for family support and family communication.18
Depressive symptoms or thoughts of suicide.
One study reported a statistically significant negative association between family meal frequency and high depressive symptoms, as well as between family meal frequency and suicidal thoughts, in both females and males.36 This statistical significance was maintained even after adjusting for various demographic and familial factors. The only noted difference between the sexes was the existence of a statistically significant negative association between family meal frequency and suicide attempts in females that was not present in males. Two other non–sex-specific studies found a statistically significant inverse association between family meal frequency and depressive symptoms,18,33 with one study extending this association to include suicidal risk.18 Findings also remained statistically significant after controlling for similar factors.
DISCUSSION
The findings of this systematic review indicate that eating frequent family meals is associated with better psychosocial outcomes for children and adolescents. In general, frequent family meals were inversely associated with disordered eating, alcohol and substance use, violent behaviour, and feelings of depression or thoughts of suicide. There was a positive relationship between frequent family meals and increased self-esteem and commitment to learning or a higher grade point average. However, the findings also highlight the differences in outcomes for males and females, with females seemingly gaining more protective effects from frequent family meals than males do.
What do we know about the barriers that exist to having frequent family meals? Both parents’ and adolescents’ busy schedules41–45 are often cited as common reasons for less frequent family meals. In addition, there is a disparity of family meal frequency across socioeconomic levels. Neumark-Sztainer and colleagues found that lower socioeconomic status was associated with lower frequency of family meals,21 and Widome and colleagues found that food-insecure youth ate fewer family meals than food-secure youth.46 From 1999 to 2010, there was a decline in family meal frequency among adolescents from low socioeconomic status and an increase in frequency among adolescents from high-middle socioeconomic families.47
Despite our advances in some areas of understanding, it remains unclear exactly how family meals improve adolescent outcomes, especially for females. The relationship between family meals and psychosocial outcomes might in fact be bidirectional (ie, increased family meals lead to decreased odds of poor psychosocial outcomes but also that psychosocially healthier youth and families might simply engage in more family meals).
It is unclear why there are differences between the effects of family meals for males and females. Research has shown that males and females respond differently to family dynamics. For example, Crosnoe found that family instability magnified the socioemotional risks of obesity for girls but not for boys.11 Other researchers have also found that high-risk youths’ perception of their family connectedness being strong is associated with reduced odds of being sexually experienced and having initiated sex before the age of 13 for females but not for males.13 In addition, females respond differently to family economic problems than males do, and females are more sensitive to family disruptions (ie, parents’ negative moods) than males are.10 Griffin and colleagues found that some protective effects of parenting practices were limited to females and not males12; for example, frequent parent checking of homework was associated with less aggression in females but not males. If the mechanism of the positive effects of family meals is related to family connectedness and other similar family factors, it is therefore possible that males do not gain the same protective effect from frequent family meals because of their different response to family dynamics.31
Future studies should examine the specific mechanisms by which frequent family meals might lead to improved psychosocial outcomes in youth. Furthermore, research should continue to explore the barriers that exist to having frequent family meals, including socioeconomic implications.
Limitations
Limitations exist with all the individual studies reviewed. Regarding the results of the cross-sectional studies, we can infer associations but not causality. For example, those with concern about high body weight or those with already-established disordered eating or substance use or abuse, etc, might avoid family meals, and children and youth who are already doing well could be more likely to eat with their families. Many studies also relied on self-report survey data that have the potential of recall bias and social desirability bias. There might also be an unmeasured protective factor in families who dine together regularly that was not captured; there is the potential that other unmeasured confounders (eg, family structure) could explain the positive results. In addition, the overall generalizability of some of the samples is variable depending on the demographic variability of the samples. However, even with these limitations, together these studies produce patterns based on very large, often diverse, samples. The studies reviewed had sample sizes between 145 and 99 462, including different ethnicities, and many attempted to control results for potential confounders such as family connectedness. In addition, the longitudinal nature of some of the reviewed studies adds more powerful associations.
Conclusion
This review provides further support that frequent family meals are associated with better psychosocial outcomes for children and adolescents. Although more research is needed to prove causality, there are few risks to recommending that families strive to have frequent family meals. All health care practitioners should educate families on the potential effects of having regular meals together as a family. In addition, practitioners should explore any obstacles that might exist to having family meals and discuss potential strategies for their implementation.
EDITOR’S KEY POINTS
This systematic review found that eating frequent family meals was associated with better psychosocial outcomes for children and adolescents. Frequent family meals were inversely associated with disordered eating, alcohol and substance use, violent behaviour, and feelings of depression or thoughts of suicide. There was a positive relationship between frequent family meals and increased self-esteem and commitment to learning or a higher grade point average.
Findings also highlighted that females seemingly gained more protective effects from frequent family meals than males did.
Given that psychosocial dysfunction is one of the most common chronic conditions among children and adolescents, health care practitioners should educate families on the benefits of having regular meals together. In addition, practitioners should explore any obstacles that might exist to having family meals and discuss potential strategies for their implementation.
Footnotes
This article has been peer reviewed
This article is eligible for Mainpro-M1 credits. To earn credits, go to www.cfp.ca and click on the Mainpro link.
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro de février 2015 à la page e107.
Contributors
Dr Harrison contributed to study design and acquisition of data, reviewed all articles included in the systematic review, interpreted data, and drafted the manuscript. Dr Norris contributed to study conception and design, and revised the manuscript. Dr Obeid participated in data analysis and interpretation, and contributed to drafting and revising the manuscript. Ms Fu contributed to data analysis, as well as drafting and revising the manuscript. Dr Weinstangel participated in data acquisition, reviewed articles included in the systematic review, contributed to data analysis, and helped with manuscript drafting. Dr Sampson participated in the study design and data acquisition, as well as drafting and revising the manuscript. All authors read and approved the final manuscript.
Competing interests
None declared
References
- 1.Kelleher KJ, Wolraich ML. Diagnosing psychosocial problems. Pediatrics. 1996;97(6 Pt 1):899–901. [PubMed] [Google Scholar]
- 2.Reijneveld SA, Vogels AG, Brugman E, van Ede J, Verhulst FC, Verloove-Vanhorick SP. Early detection of psychosocial problems in adolescents: how useful is the Dutch short indicative questionnaire (KIVPA)? Eur J Public Health. 2003;13(2):152–9. doi: 10.1093/eurpub/13.2.152. [DOI] [PubMed] [Google Scholar]
- 3.Piko BF. Self-perceived health among adolescents: the role of gender and psychosocial factors. Eur J Pediatr. 2007;166(7):701–8. doi: 10.1007/s00431-006-0311-0. Epub 2006 Nov 21. [DOI] [PubMed] [Google Scholar]
- 4.Bunker SJ, Colquhoun DM, Esler MD, Hickie IB, Hunt D, Jelinek VM, et al. “Stress” and coronary heart disease: psychosocial risk factors. Med J Aust. 2003;178(6):272–6. doi: 10.5694/j.1326-5377.2003.tb05193.x. [DOI] [PubMed] [Google Scholar]
- 5.Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull. 1992;112(1):64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- 6.Fulkerson JA, Strauss J, Neumark-Sztainer D, Story M, Boutelle K. Correlates of psychosocial well-being among overweight adolescents: the role of the family. J Consult Clin Psychol. 2007;75(1):181–6. doi: 10.1037/0022-006X.75.1.181. [DOI] [PubMed] [Google Scholar]
- 7.Kingon YS, O’Sullivan AL. The family as a protective asset in adolescent development. J Holist Nurs. 2001;19(2):102–21. doi: 10.1177/089801010101900202. [DOI] [PubMed] [Google Scholar]
- 8.Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, et al. Protecting adolescents from harm. Findings from the National Longitudinal Study on Adolescent Health. JAMA. 1997;278(10):823–32. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- 9.Resnick MD, Harris LJ, Blum RW. The impact of caring and connectedness on adolescent health and well-being. J Paediatr Child Health. 1993;29(Suppl 1):S3–9. doi: 10.1111/j.1440-1754.1993.tb02257.x. [DOI] [PubMed] [Google Scholar]
- 10.Conger RD, Conger KJ, Elder GH, Lorenz FO, Simon RL, Whitbeck LB. Family economic stress and adjustment of early adolescent girls. Dev Psychol. 1993;29:206–19. [Google Scholar]
- 11.Crosnoe R. Obesity, family instability, and socioemotional health in adolescence. Econ Hum Biol. 2012;10(4):375–84. doi: 10.1016/j.ehb.2012.04.005. Epub 2012 May 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Griffin KW, Botvin GJ, Scheier LM, Diaz T, Miller NL. Parenting practices as predictors of substance use, delinquency, and aggression among urban minority youth: moderating effects of family structure and gender. Psychol Addict Behav. 2000;14(2):174–84. doi: 10.1037//0893-164x.14.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Markham CM, Tortolero SR, Escobar-Chaves SL, Parcel GS, Harrist R, Addy RC. Family connectedness and sexual risk-taking among urban youth attending alternative high schools. Perspect Sex Reprod Health. 2003;35(4):174–9. doi: 10.1363/psrh.35.174.03. [DOI] [PubMed] [Google Scholar]
- 14.Larson RW, Branscomb KR, Wiley AR. Forms and functions of family mealtimes: multidisciplinary perspectives. New Dir Child Adolesc Dev. 2006;111:1–15. doi: 10.1002/cd.152. [DOI] [PubMed] [Google Scholar]
- 15.Franko DL, Thompson D, Affenito SG, Barton BA, Striegel-Moore RH. What mediates the relationship between family meals and adolescent health issues? Health Psychol. 2008;27(Suppl 2):S109–17. doi: 10.1037/0278-6133.27.2(Suppl.).S109. [DOI] [PubMed] [Google Scholar]
- 16.White J, Halliwell E. Alcohol and tobacco use during adolescence: the importance of the family mealtime environment. J Health Psychol. 2010;15(4):526–32. doi: 10.1177/1359105309355337. [DOI] [PubMed] [Google Scholar]
- 17.McDaniel SA, Tepperman L. Close relations: an introduction to the sociology of families. Toronto, ON: Prentice Hall Allyn and Bacon Canada; 2000. [Google Scholar]
- 18.Fulkerson JA, Story M, Mellin A, Leffert N, Neumark-Sztainer D, French SA. Family dinner meal frequency and adolescent development: relationships with developmental assets and high-risk behaviors. J Adolesc Health. 2006;39(3):337–45. doi: 10.1016/j.jadohealth.2005.12.026. Epub 2006 Jul 10. [DOI] [PubMed] [Google Scholar]
- 19.Neumark-Sztainer D, Wall M, Story M, Fulkerson JA. Are family meal patterns associated with disordered eating behaviors among adolescents? J Adolesc Health. 2004;35(5):350–9. doi: 10.1016/j.jadohealth.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 20.Videon TM, Manning CK. Influences on adolescent eating patterns: the importance of family meals. J Adolesc Health. 2003;32(5):365–73. doi: 10.1016/s1054-139x(02)00711-5. [DOI] [PubMed] [Google Scholar]
- 21.Neumark-Sztainer D, Hannan PJ, Story M, Croll J, Perry C. Family meal patterns: associations with sociodemographic characteristics and improved dietary intake among adolescents. J Am Diet Assoc. 2003;103(3):317–22. doi: 10.1053/jada.2003.50048. [DOI] [PubMed] [Google Scholar]
- 22.Larson NI, Neumark-Sztainer D, Hannan PJ, Story M. Family meals during adolescence are associated with higher diet quality and healthful meal patterns during young adulthood. J Am Diet Assoc. 2007;107(9):1502–10. doi: 10.1016/j.jada.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 23.Larson NI, Nelson MC, Neumark-Sztainer D, Story M, Hannan PJ. Making time for meals: meal structure and associations with dietary intake in young adults. J Am Diet Assoc. 2009;109(1):72–9. doi: 10.1016/j.jada.2008.10.017. [DOI] [PubMed] [Google Scholar]
- 24.Woodruff SJ, Hanning RM. A review of family meal influence on adolescents’ dietary intake. Can J Diet Pract Res. 2008;69(1):14–22. doi: 10.3148/69.1.2008.14. [DOI] [PubMed] [Google Scholar]
- 25.Pearson N, Biddle SJ, Gorely T. Family correlates of breakfast consumption among children and adolescents. A systematic review. Appetite. 2009;52(1):1–7. doi: 10.1016/j.appet.2008.08.006. Epub 2008 Aug 22. [DOI] [PubMed] [Google Scholar]
- 26.Sen B. Frequency of family dinner and adolescent body weight status: evidence from the National Longitudinal Survey of Youth, 1997. Obesity. 2006 Silver Spring;14(12):2266–76. doi: 10.1038/oby.2006.266. [DOI] [PubMed] [Google Scholar]
- 27.Taveras EM, Rifas-Shiman SL, Berkey CS, Rockett HR, Field AE, Frazier AL, et al. Family dinner and adolescent overweight. Obes Res. 2005;13(5):900–6. doi: 10.1038/oby.2005.104. [DOI] [PubMed] [Google Scholar]
- 28.Fulkerson JA, Neumark-Sztainer D, Hannan PJ, Story M. Family meal frequency and weight status among adolescents: cross-sectional and 5-year longitudinal associations. Obesity. 2008 Silver Spring;16(11):2529–34. doi: 10.1038/oby.2008.388. Epub 2008 Aug 14. [DOI] [PubMed] [Google Scholar]
- 29.Valdés J, Rodríguez-Artalejo F, Aguilar L, Jaén-Casquero MB, Royo-Bordonada MÁ. Frequency of family meals and childhood overweight: a systematic review. Pediatr Obes. 2013;8(1):e1–13. doi: 10.1111/j.2047-6310.2012.00104.x. Epub 2012 Dec 13. [DOI] [PubMed] [Google Scholar]
- 30.Fisher LB, Miles IW, Austin SB, Camargo CA, Jr, Colditz GA. Predictors of initiation of alcohol use among US adolescents: findings from a prospective cohort study. Arch Pediatr Adolesc Med. 2007;161(10):959–66. doi: 10.1001/archpedi.161.10.959. [DOI] [PubMed] [Google Scholar]
- 31.Skeer MR, Ballard EL. Are family meals as good for youth as we think they are? A review of the literature on family meals as they pertain to adolescent risk prevention. J Youth Adolesc. 2013;42(7):943–63. doi: 10.1007/s10964-013-9963-z. Epub 2013 May 28. [DOI] [PubMed] [Google Scholar]
- 32.Haines J, Gillman MW, Rifas-Shiman S, Field AE, Austin SB. Family dinner and disordered eating behaviors in a large cohort of adolescents. Eat Disord. 2010;18(1):10–24. doi: 10.1080/10640260903439516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fulkerson JA, Kubik MY, Story M, Lytle L, Arcan C. Are there nutritional and other benefits associated with family meals among at-risk youth? J Adolesc Health. 2009;45(4):389–95. doi: 10.1016/j.jadohealth.2009.02.011. Epub 2009 May 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sen B. The relationship between frequency of family dinner and adolescent problem behaviors after adjusting for other family characteristics. J Adolesc. 2010;33(1):187–96. doi: 10.1016/j.adolescence.2009.03.011. Epub 2009 May 23. [DOI] [PubMed] [Google Scholar]
- 35.Woodruff SJ, Hanning RM. Associations between family dinner frequency and specific food behaviors among grade six, seven, and eight students from Ontario and Nova Scotia. J Adolesc Health. 2009;44(5):431–6. doi: 10.1016/j.jadohealth.2008.10.141. Epub 2009 Jan 9. [DOI] [PubMed] [Google Scholar]
- 36.Eisenberg ME, Olson RE, Neumark-Sztainer D, Story M, Bearinger LH. Correlations between family meals and psychosocial well-being among adolescents. Arch Pediatr Adolesc Med. 2004;158(8):792–6. doi: 10.1001/archpedi.158.8.792. [DOI] [PubMed] [Google Scholar]
- 37.Sierra-Baigrie S, Lemos-Giráldez S, Fonseca-Pedrero E. Binge eating in adolescents: its relation to behavioural problems and family-meal patterns. Eat Behav. 2009;10(1):22–8. doi: 10.1016/j.eatbeh.2008.10.011. Epub 2008 Oct 31. [DOI] [PubMed] [Google Scholar]
- 38.Neumark-Sztainer D, Eisenberg ME, Fulkerson JA, Story M, Larson NI. Family meals and disordered eating in adolescents: longitudinal findings from project EAT. Arch Pediatr Adolesc Med. 2008;162(1):17–22. doi: 10.1001/archpediatrics.2007.9. [DOI] [PubMed] [Google Scholar]
- 39.Neumark-Sztainer DR, Wall MM, Haines JI, Story MT, Sherwood NE, van den Berg PA. Shared risk and protective factors for overweight and disordered eating in adolescents. Am J Prev Med. 2007;33(5):359–69. doi: 10.1016/j.amepre.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 40.Eisenberg ME, Neumark-Sztainer D, Fulkerson JA, Story M. Family meals and substance use: is there a long-term protective association? J Adolesc Health. 2008;43(2):151–6. doi: 10.1016/j.jadohealth.2008.01.019. Epub 2008 Apr 11. [DOI] [PubMed] [Google Scholar]
- 41.National Center on Addiction and Substance Abuse at Columbia University . The importance of family dinners VI. New York, NY: The National Center on Addiction and Substance Abuse at Columbia University; 2010; Available from: www.casacolumbia.org/upload/2010/20100922familydinners6.pdf. Accessed 2015 Jan 14. [Google Scholar]
- 42.Hill JP, Holmbeck GN. Attachment and autonomy during adolescence. In: Whitehurst G, editor. Annals of child development. Greenwich, CT: JAI Press; 1986. [Google Scholar]
- 43.Rovner AJ, Mehta SN, Haynie DL, Robinson EM, Pound HJ, Butler DA, et al. Perceived benefits, barriers, and strategies of family meals among children with type 1 diabetes mellitus and their parents: focus-group findings. J Am Diet Assoc. 2010;110(9):1302–6. doi: 10.1016/j.jada.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Neumark-Sztainer D, Story M, Ackard D, Moe J, Perry C. The “family meal”: views of adolescents. J Nutr Educ. 2000;32(6):329–34. [Google Scholar]
- 45.Ritchie LD, Welk G, Styne D, Gerstein DE, Crawford PB. Family environment and pediatric overweight: what is a parent to do? J Am Diet Assoc. 2005;105(5 Suppl 1):S70–9. doi: 10.1016/j.jada.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 46.Widome R, Neumark-Sztainer D, Hannan PJ, Haines J, Story M. Eating when there is not enough to eat: eating behaviors and perceptions of food among food-insecure youths. Am J Public Health. 2009;99(5):822–8. doi: 10.2105/AJPH.2008.139758. Epub 2009 Mar 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Neumark-Sztainer D, Wall M, Fulkerson JA, Larson N. Changes in the frequency of family meals from 1999 to 2010 in the homes of adolescents: trends by sociodemographic characteristics. J Adolesc Health. 2013;52(2):201–6. doi: 10.1016/j.jadohealth.2012.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]