Abstract
Background
Uptake of HPV vaccine remains low among adolescents in the United States. We sought to assess barriers to HPV vaccine provision in school health centers to inform subsequent interventions.
Methods
We conducted structured interviews in Fall 2010 with staff from all 33 school health centers in North Carolina that stocked HPV vaccine.
Results
Centers had heterogeneous policies and procedures. Out-of-pocket costs for children to receive privately-purchased HPV vaccine were a key barrier to providing HPV vaccine within school health centers. Other barriers included students not returning consent forms, costs to clinics of ordering and stocking privately-purchased HPV vaccine, and difficulty using the statewide immunization registry. Most (82%) school health centers were interested in hosting interventions to increase HPV vaccine uptake, especially those that the centers could implement themselves, but many had limited staff to support such efforts. Activities rated as more likely to raise HPV vaccine uptake were student incentives, parent reminders, and obtaining consent from parents while they are at school (all p < .05).
Conclusions
While school health centers reported facing several key barriers to providing HPV vaccine, many were interested in partnering with outside organizations on low-cost interventions to increase HPV vaccine uptake among adolescent students.
Keywords: School health, adolescent health, HPV vaccine
Human papillomavirus (HPV) causes almost all cervical cancers and a significant portion of vulvar, vaginal, penile, anal, and oropharyngeal cancers.1 Two vaccines protecting against HPV infection could prevent the majority of these HPV-associated cancers.2,3 Current guidelines from the Advisory Committee on Immunization Practices recommend routine administration of HPV vaccine to adolescents ages 11 or 12, with catch-up vaccination appropriate through age 21 for young men and age 26 for young women.4 However, coverage remains low, with only 53.0% of girls and 8.3% of boys ages 13 through 17 receiving at least one dose of the three-dose HPV vaccine series, and series completion is even lower at 34.8% and 1.3%, respectively.5
A potentially feasible and effective way to increase HPV vaccine coverage is through in-school vaccination programs. School-located programs offering voluntary HPV vaccination free of charge in countries such as the United Kingdom and Australia have achieved completion rates that exceed 80%.6–11 Indeed, HPV vaccine series completion is highest when provided in school settings.12 One option is mass vaccination programs that bring temporary vaccination clinics to schools, but these have been only moderately successful in the U.S. in improving vaccine uptake for the seasonal flu shot,13–15 tetanus, diphtheria, and pertussis booster,16 varicella vaccine,17 or HPV vaccine.18 For example, the median increase in HPV vaccine coverage from mass vaccination programs is 10%.19
An alternative is to use health centers that are linked to or located within schools. School health centers are associated with increased rates of adolescent vaccination,20,21 especially for adolescents who are under- or uninsured20,22 or those who interact less frequently with more traditional healthcare venues.23 Both parents24 and physicians25 have favorable attitudes towards vaccination at school sites, and most school health centers (84%) already have the refrigeration equipment, staff, and billing systems to provide adolescent vaccines.22,26 However, school health centers often focus on basic health services rather than more resource-intensive preventive health services, such as vaccines,27 and expanding school health centers’ services requires local commitment in terms of budget and health priorities.28 Improving interventions aimed at delivering vaccines through existing school health centers in the United States could boost support for school health centers as well as increase rates of HPV vaccine initiation and completion.
Our study aimed to better understand HPV vaccination services in school health centers and to identify barriers to their providing the vaccine. We also sought to assess the viability of potential interventions to increase HPV vaccine provision in these centers. These results can guide future interventions to increase HPV vaccination rates at school health centers.
METHODS
Participants
We interviewed representatives from school health centers in North Carolina that stocked HPV vaccine. The North Carolina School Community Health Alliance, a statewide organization that supports the work of school health centers, provided us with contact information for all 53 school health centers in NC and emailed our study recruitment letter to representatives at each center. School health centers were eligible for the study if they (1) were school-based (located on a school campus) or school-linked (located off-campus but serving students from designated schools) and (2) offered HPV vaccine. We excluded school health centers that did not stock HPV vaccine because our study aimed to focus specifically on barriers to maintaining, rather than establishing, an HPV vaccination program.
Twenty school health centers in NC were ineligible to participate in this study. Nine of these centers did not offer any vaccine services, and eight offered other vaccines but not HPV vaccine. The remaining three school health centers were ineligible because they did not serve students in the targeted age range for HPV vaccine.
Sixteen organizations coordinated the 33 eligible school health centers, and representatives from all of these organizations completed interviews in fall 2010, yielding a response rate of 100%. Respondents were school health center administrators (N = 13) or another person designated by the administrator as more knowledgeable about the topics on the survey (N = 2 nurse practitioners and 1 physician). Seven participants represented only one school health center, while the remaining nine participants represented organizations that coordinated more than one school health center; for these latter participants, we completed separate interviews in reference to each eligible school health center that the participant coordinated. We entered each of the 33 participating school health centers into a drawing for one of two unrestricted $500 donations.
Procedure
Interviewers used a structured telephone questionnaire that focused on school health center vaccination services and procedures, barriers to providing HPV vaccine, and potential interventions for increasing vaccine uptake (questionnaire available at www.unc.edu/~ntbrewer/hpv.htm). Interviewers made case notes that we verified using audio recordings of the interviews. The institutional review board of the University of North Carolina approved the study protocol.
Measures
The questionnaire assessed existing procedures and services, including standard operations of the center (eg, hours, whether the center accepts private insurance); if centers stocked publicly- or privately-funded HPV vaccine; successes and challenges to providing HPV vaccine; use of the North Carolina Immunization Registry (NCIR), a centralized electronic health record database containing information on children’s and adolescents’ immunization history; tracking and reminders (eg, postcards or automated phone calls) to students who initiate HPV vaccination; costs and reimbursements for HPV vaccine; and procedures for obtaining parent and/or student consent for HPV vaccination. Questions about barriers to providing HPV vaccine to students measured respondents’ concerns about obtaining medical records, costs to school health centers, costs to parents, and interference from school administration. Respondents could report on all of their perceived barriers, and we also asked them to identify area(s) of greatest concern.
Finally, we asked participants to rate several activities to increase uptake of HPV vaccine in terms of effectiveness, 1 (“would not increase uptake a lot”) to 3 (“would increase uptake a lot”); feasibility, 1 (“not very doable”) to 3 (“very doable); and helpfulness, 1 (“not very helpful”) to 3 (“very helpful”). Activities included those led by school health centers (eg, sending parents letters endorsing adolescent vaccines; student-led promotional campaigns; and student incentives for vaccination) and those led by outside parties (eg, adding school health centers to networks of approved providers for private insurance plans; developing new consent forms that appeal to parents; and addressing HPV vaccine in health education classes). We also asked respondents more general questions about HPV vaccination activities, such as staff availability to implement interventions and their interest in partnering with outside organizations to conduct the new activities.
Data Analysis
We report descriptive quantitative data around several topics from the surveys, including the number and percentage of respondents reporting a given outcome. For quantitative data, the denominator for percentages is 33, unless stated otherwise. We compared intervention ratings using either t-tests or analysis of variance, with post-hoc t-tests, as appropriate. We used SPSS version 18 (SPSS Inc., Chicago, IL) to perform two-tailed statistical analyses with a critical alpha of .05. These comparisons allowed us to evaluate which potential interventions were particularly attractive to school health center administrators, in terms of their perceived effectiveness, feasibility, and helpfulness.
We examined qualitative data from open-ended questions for common themes. Two coders independently evaluated the open-ended responses and discussed discrepancies as they arose to reach a final consensus.
RESULTS
Characteristics of School Health Centers
The 33 school health centers served schools with approximately 28,000 students in grades 6 or higher (mean = 863/school, standard deviation [SD] = 757, range = 24–3600) (Table 1). Centers’ average proportion of Spanish-speaking students served was 11% (SD = 14%, range = 0%–50%). Most (91%) of the centers were located on school premises, and 42% were in rural areas.
Table 1.
Characteristics of School Health Centers, North Carolina (N = 33).
| % | |
|---|---|
| Students enrolled in associated school, mean (SD) (N = 26) | 863 (757) |
| Percentage of Spanish-speaking students, mean (SD) | 11% (.14) |
| Type of school health center | |
| School-based | 91% |
| School-linked | 9% |
| Urbanicity | |
| Urban | 49% |
| Suburban | 9% |
| Rural | 42% |
| Hours of operation | |
| Most school days | 97% |
| Limited hours | 3% |
| Accept all types of private insurance | |
| Yes | 67% |
| No | 33% |
| Stock Vaccines for Children (VFC) vaccines | |
| Yes | 100% |
| No | 0% |
| Stock privately-purchased vaccines | |
| Yes | 55% |
| No | 46% |
| Use North Carolina Immunization Registry (NCIR) to update students’ electronic health records | |
| Yes | 100% |
| No | 0% |
| Use reminder/recall function of NCIR to track students who initiate vaccination | |
| Yes | 33% |
| No | 67% |
| Use other methods to track students who initiate vaccination | |
| Yes | 91% |
| No | 9% |
| Partner with outside organizations to provide HPV vaccine | |
| Yes | 46% |
| No | 55% |
| Use electronic records of HPV vaccination | |
| Yes | 70% |
| No | 30% |
| HPV vaccine product stocked | |
| Quadrivalent | 100% |
| Bivalent | 0% |
| HPV vaccine doses administered in 2009–2010 school year, mean (SD | 57 (93) |
| Number of students receiving all 3 doses of HPV vaccine in 2009–2010 school year, mean (SD) | 6 (9) |
Note. School-located clinics were located on premises while school-linked were located offsite.
All of the school health centers accepted both public and private health insurance, although some centers (33%) did not accept all types of private insurance (Table 1). All of the school health centers stocked publicly-purchased vaccines (ie, purchased by the Vaccines for Children [VFC] program), and 55% stocked privately-purchased vaccines.
To track adolescent vaccines delivered to students, school health centers used the NCIR (33%) and other methods (91%) (Table 1). To document HPV vaccination, 70% used electronic health records besides NCIR. All of the school health centers stocked quadrivalent HPV vaccine, but none stocked bivalent HPV vaccine. In the 2009–2010 school year, centers delivered an average of 57 doses of HPV vaccine (SD = 93, range = 0–436) (N = 27 centers reporting), and an average of 6 students received all three doses of HPV vaccine at each clinic (SD = 9, range = 0–26) (N = 13 centers reporting).
School Health Center Policies for Adolescent Vaccination
School health centers employed a wide variety of policies to manage adolescent vaccination. Below, we summarize the policies related to consent and cost.
Consent procedures
All of the school health centers sought written parental consent to provide health services to students, but a few (18%) also accepted verbal parental consent (Table 2). Most centers (76%) required additional consent forms from parents before administration of adolescent vaccines. Most often, this separate consent form was a vaccine checklist that included HPV vaccine and other adolescent vaccines, although two centers required a separate consent form for each adolescent vaccine. Most (55%) of the centers required parental consent for HPV vaccine for students of all ages.
Table 2.
School Health Center Vaccination Policies (N = 33).
| % | |
|---|---|
| Mode of consent for vaccination | |
| In writing | 100 |
| Verbally | 18 |
| Separate consent form required for adolescent vaccination | |
| Yes | 76 |
| No | 24 |
| Characteristics of separate consent form for adolescent vaccination (N = 25) | |
| Checklist of all adolescent vaccines | 76 |
| Separate consent form for each adolescent vaccine | 8 |
| Separate consent form only for HPV vaccine | 8 |
| Verbal consent for adolescent vaccines | 8 |
| Parent consent required to give HPV vaccine if younger than… (N = 31) | |
| 16 years | 3 |
| 18 years | 29 |
| 21 years | 13 |
| all ages | 55 |
| Cost of VFC-supported HPV vaccine administration, mean (SD) | $10 (7) |
Cost
For students receiving adolescent vaccines through VFC, the average fee charged to the family for administering one dose of HPV vaccine was $10 (SD = $7, range = $0-$18) (Table 2). Because costs for HPV vaccine for students with private insurance vary, we did not collect data on out-of-pocket costs for privately-purchased vaccines.
Barriers to HPV Vaccination
Students
More than three-quarters (79%) of school health centers cited out-of-pocket costs for students to receive privately-purchased HPV vaccine as a barrier to vaccination, and 51% cited this issue as the most important barrier (Table 3). Many (33%) school health centers also reported that out-of-pocket costs for students to receive VFC-purchased HPV vaccine were a barrier to vaccination. Few respondents indicated that parental attitudes towards HPV vaccine (18%) or parental knowledge about HPV (3%) were barriers to students’ receiving permission to receive HPV vaccine.
Table 3.
Barriers to HPV Vaccination for Students and for School Health Centers (N = 33).
| Barrier | Reported concern (%) | Greatest concern (%) |
|---|---|---|
| Barriers for students | ||
| Out-of-pocket costs for students to receive privately-purchased HPV vaccine | 79 | 51 |
| Out-of-pocket costs for students to receive VFC-purchased HPV vaccine | 33 | 21 |
| Parental attitudes towards HPV vaccine | 18 | -- |
| Parental knowledge about HPV | 3 | -- |
| Barriers for school health centers | ||
| Students not returning consent forms | 76 | 21 |
| Problems using North Carolina Immunization Registry | 76 | -- |
| Upfront costs of stocking privately-purchased HPV vaccine | 67 | 30 |
| Inadequate reimbursement from insurance companies for administering privately-purchased HPV vaccine | 42 | 18 |
| Obtaining students’ immunization history was a barrier to vaccination | 61 | 6 |
| School administrators’ concern about student time away from classes | 21 | 0 |
School health centers
The most commonly-cited barrier to HPV vaccination for school health centers was students not returning consent forms (76%) (Table 3). Many respondents also identified barriers such as upfront costs of stocking privately-purchased HPV vaccine (67%) and inadequate reimbursement from insurance companies for administering privately-purchased HPV vaccine (42%).
Several barriers to HPV vaccination revolved around difficulties with tracking students’ immunizations and maintaining accurate health records. Many (61%) school health centers stated that obtaining students’ immunization history was a barrier to vaccination (Table 3). Although all of the school health centers used NCIR, many centers (76%) reported in open-ended responses that they had difficulty using this system, including slow operating systems, effort involved in double-entry of data into both the Registry and internal records, and need for additional training to use the Registry.
Finally, few school health centers (21%) rated school administrators’ concern about students’ time away from classes as a barrier to providing HPV vaccine (Table 3). One center reported that a school administrator expressed concern that the vaccination clinics might draw the school into the public discussion over HPV vaccine.
Activities to Increase HPV Vaccination
Most (82%) school health centers were somewhat or very interested in taking part in activities to increase HPV vaccine uptake. However, 67% reported that limited staff affected their ability to implement new activities, and few respondents thought that teaching staff would be willing to assist with HPV vaccine interventions (21%). Therefore, centers were most interested in activities that did not require a lot of effort from center staff.
Current activities
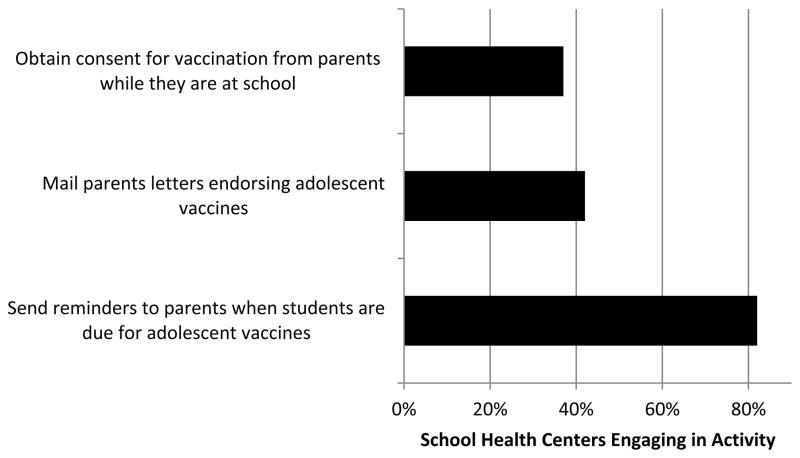
Many centers already engaged in interventions to increase HPV vaccination among students. Notably, 82% of centers sent reminders to parents when students were due for adolescent vaccines (Figure 1). Fewer centers mailed parents letters endorsing adolescent vaccines (42%) or obtained consent for vaccination from parents while they were physically at the school (eg, at parent-teacher conferences) (37%).
Figure 1.
Current Activities to Increase HPV Vaccine Provision among School Health Centers in North Carolina (N = 33).
New activities
Most (79%) school health centers reported that they were interested in taking part in new activities to promote HPV vaccination. Respondents’ open-ended responses reflected enthusiasm for receiving HPV vaccine brochures or posters specifically-tailored for adolescents, although they would prefer promotional materials about multiple adolescent vaccines over materials that only focused on HPV vaccine. Other activities suggested by respondents in open-ended responses included media campaigns for parents of boys, parent education campaigns, literature with photos of genital warts and cervical cancer, subsidization of out-of-pocket vaccine costs, health fairs, expert forums, mass immunization events, and dissemination of information on evidence-based practices that have been successful in other school health centers.
Among new activities that school health centers would lead, respondents rated student incentives for vaccination and sending parents letters endorsing adolescent vaccines as more feasible than the remaining activities (post-hoc t-test comparing these 2 interventions to remaining 3 school-led activities, p < .005) (Table 4). When asked to rate whether activities would increase HPV vaccine uptake, respondents gave higher marks to student incentives for vaccination, sending parents reminders when students are due for adolescent vaccines, and obtaining consent from parents while they are at the school than they did to the remaining activities (post-hoc t-test comparing these 3 interventions to remaining 3 school-led activities, p < .05).
Table 4.
Activities to Increase HPV Vaccination at School Health Centers, North Carolina (N = 33).
| Activities led by school health centers | Feasible (mean) | Would increase uptake (mean) |
|---|---|---|
|
|
||
| Obtain consent for vaccination from parents while they are at school† | 1.7 | 2.3 b |
| Mail parents letters endorsing adolescent vaccines† | 2.4 a | 2.0 |
| Send reminders to parents when students are due for adolescent vaccines† | -- | 2.4 b |
| Have student-led promotional campaigns | 2.1 | 2.0 |
| Host school-based HPV vaccine awareness raising events | 2.0 | 2.2 |
| Give student incentives for receiving adolescent vaccines | 2.8 a | 2.5 b |
| Activities led by outside parties | Helpful (mean) | Would increase uptake (mean) |
|
|
||
| Provide additional training to use NCIR | 2.1 | 1.9 |
| Pay for privately-purchased doses of HPV vaccine after administration | 2.0 | 2.0 |
| Add school health centers to private insurance plans’ approved providers | 2.2 | 2.1 |
| Develop new consent forms that appeal to parents | 2.1 | 2.0 |
| Give additional HPV vaccine brochures or posters | 2.1 | 2.1 |
| Address HPV vaccine in health education classes | 2.1 | 2.0 |
Note. Response scales had 3 options (ie, “not at all doable” to “very doable”; “would increase uptake not at all” to “would increase uptake a lot”; or “would help not at all” to “would help a lot”).
Does not include clinics already engaging in these activities.
These two activities had higher ratings for “Feasibility” that the remaining 3 school-led activities, based on post-hoc t-tests.
These three activities had higher ratings for “Would increase uptake” than the remaining 3 school-led activities, based on post-hoc t-tests.
Respondents rated the new activities that outside organizations would lead as similarly helpful (ANOVA comparing 6 activities, p = .82) and similarly likely to increase HPV vaccine uptake (ANOVA comparing 6 activities, p = .50) (Table 4). Respondents rated school health center-led activities as more likely to increase vaccine uptake than activities led by outside parties (t-test comparing the two types of activities, p = .008).
DISCUSSION
Although school health centers have a wide variety of policies regarding student vaccination, parental consent, and private insurance, almost all school health centers said that cost to parents and centers of stocking and administering HPV vaccine hinders immunization efforts. School health centers were interested in interventions that would address these and other barriers to HPV vaccination, especially interventions that are low-cost, easy to implement, and implemented by the centers. Below, we highlight several themes from the interviews with administrators of school health centers in North Carolina and discuss their implications for interventions efforts aimed at increasing HPV vaccination.
Consistent with other research,29–31 we found that costs associated with HPV vaccine, both for the school health centers and for the families of students, were a significant barrier to provision. The costs of privately-purchased HPV vaccine were particularly problematic in terms of both the upfront costs for school health centers to stock the vaccine and the out-of-pocket costs for students to receive the vaccine. Even theoretically nominal out-of-pocket administration fees for VFC-purchased vaccines were a barrier, suggesting that federal laws requiring providers to waive administration fees for VFC-eligible individuals who could not afford them are not enough to entirely address this problem. Interviews with physicians have identified similar cost-related barriers to providing HPV vaccine.31,32 Cost barriers offer multiple points of intervention, though they may require more resources than school health centers are able to provide. It remains to be seen how policy changes, such as the Affordable Care Act, will affect the provision of vaccines in school health centers; however, we know that policy interventions are likely to have the biggest impact on public health.33
Another major challenge facing school health centers is parental consent for HPV vaccine. Future interventions could focus on encouraging parents to consent to HPV vaccination delivered at school health centers. Better consent tracking systems or revised consent forms offer an opportunity for a sustainable change in practice that may increase uptake of HPV and other adolescent vaccines. Another option is opt-out consent, which has increased participation in a variety of health services in other contexts in the U.S.34–36 Alternatively, two school health centers reported that they did not require parental consent for HPV vaccine due to the North Carolina confidential services law that allows provision of certain health services without parental consent.37 Eliminating the requirement for parental consent, or establishing a younger age at which parental consent is no longer necessary, would reduce some barriers to HPV vaccine provision.
Characteristics of school health centers also represent challenges for future interventions. The school health centers in our study were heterogeneous in terms of size, location, organizational structure, and populations served. The impact of future interventions could vary greatly between centers; therefore, interventions should be easily adaptable for varied settings. In addition, school health centers varied widely in terms of stocking and providing HPV vaccine. The most successful school health center delivered more than 400 HPV doses in the 2009–2010 school year, yet fully one-third of school health centers in North Carolina were ineligible for this study because they did not even stock HPV vaccine (despite anecdotal reports from school health center experts indicating that all centers in North Carolina offered HPV vaccine). Indeed, as of spring 2012, most of the participating school health centers (14 out of 28 school-located health centers who we obtained data for) had stopped stocking HPV vaccine. Future research is needed to address what prevents school health centers from providing HPV vaccine.
School health centers also reported difficulties with the centralized North Carolina Immunization Registry. All of the centers used the Registry to record vaccination, but many respondents noted barriers with using this resource in addition to internal tracking procedures as well as with obtaining students’ vaccine histories. These complexities may reflect the need for improved tracking systems or additional NCIR user training. More specifically, adolescent vaccine efforts could be greatly improved by systems that link the records of school health centers with those of other providers. Ideally, these infrastructure changes would support school health centers in their vaccination efforts and improve the health of student populations.
Several of these barriers could generalize to school health centers’ provision of other recommended adolescent vaccines (tetanus, diphtheria, and pertussis booster and meningococcal conjugate4), particularly the difficulties with tracking or recordkeeping. Previous research has demonstrated that parents report similarly high levels of consent for vaccination in school health centers for all three adolescent vaccines.38
Limitations
Our study did not gather data on parents’ beliefs and attitudes about interventions to increase HPV vaccine uptake in school health centers, a topic that merits further investigation.19,24,36,39 We also did not collect data on some contextual factors that might influence intervention success, such as the school health center enrollment rate and whether the centers call students out of class for vaccine-only visits or offer the vaccine only when students come into the clinic for other health needs. In addition, future studies should investigate further the impact of out-of-pocket costs, for both privately- and publicly-purchased vaccines, especially given the many uncertainties surrounding the implementation of the Affordable Care Act. At the time of this study, North Carolina’s VFC funding only supported vaccination for under- and uninsured children (ie, not universal coverage of all children regardless of insurance status), which could limit the generalizability of these findings to states with public funding for vaccination for VFC-only individuals. Finally, our sample was limited to school health centers stocking HPV vaccine in North Carolina, and the generalizability of our results to centers in other states will depend on the respective healthcare and policy environments.
Conclusions
We viewed school health centers as an opportunity to better understand how to deliver HPV vaccine in schools, and lessons learned from these existing programs may be applicable to mass vaccination clinics and other school-based efforts to vaccinate adolescents. If schools are to be viable as alternative sites for HPV vaccination, developing a multi-pronged approach is critical because at present, relatively few schools have school-located health centers. North Carolina has 2,524 schools, including 1,835 schools that serve students in pre-kindergarten through eighth grade,40 capturing the targeted age range for HPV vaccine, 11 to 12 years. Only 2.9% (53/1,835) of these schools had access to a school-located or school-linked health center, and only 1.8% (33/1,835) had a health center that stocked HPV vaccine. Across the country, only 6% of schools have affiliated health centers.27 Improving access to school-located health centers may help increase adolescent vaccination, but mass vaccination programs in schools without these health centers will remain a necessity for school-located vaccination to have a broad impact.
Our study used quantitative and qualitative data to investigate currently existing policies and procedures in all of the school health centers in North Carolina that stocked HPV vaccine. In addition, we measured their interest in and perceptions of potential new activities to increase students’ uptake of HPV vaccine. These results provide evidence that school health centers face significant challenges to delivering HPV vaccine, particularly around parental consent and vaccine costs. However, the school health center administrators reported a high level of interest in activities to increase vaccination, including strategies that they implemented themselves or that involved outside partners.
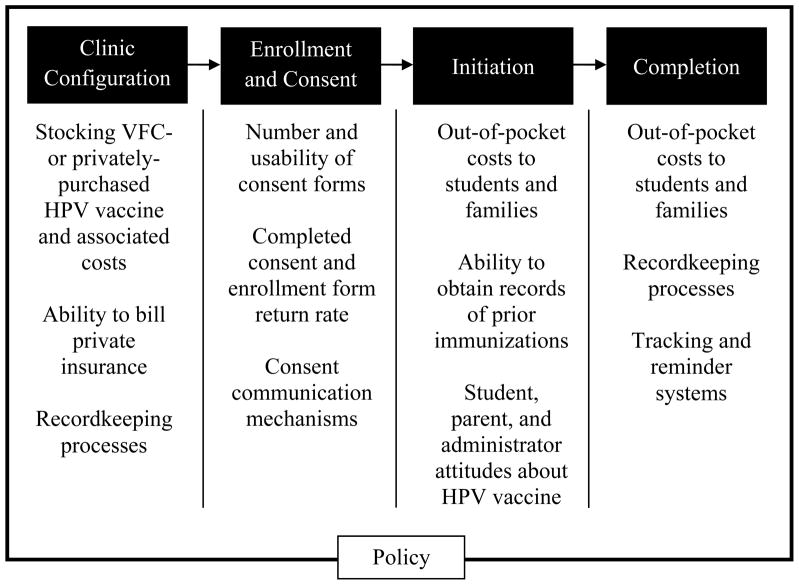
Public health professionals identifying intervention strategies to implement in school health centers should consider multiple, interacting points of intervention. Figure 2 indicates several potential interventions to address barriers to HPV vaccination in school health centers, from the configuration of the clinic, through enrollment and consent processes, to initiation and completion of the vaccine series. All of these interventions exist in the context of local and national policies and priorities that enable or hinder the efforts of school health centers to improve HPV vaccination.28 While we have identified several specific intervention strategies, we recognize that these interventions address barriers that exist in complex medical and social environments and are not independent of each other. For example, a school health center intervention to improve adolescent vaccine consent rates will not dramatically increase uptake of HPV vaccine at a school where few students have enrolled in the school health center. Likewise, an intervention targeting improved consent rates will not necessarily translate into increased uptake of HPV vaccine if a school health center does not have the resources to collect students’ immunization histories or schedule vaccine visits.
Figure 2.
Considerations at Different Points of Intervention
IMPLICATIONS FOR SCHOOL HEALTH
Our study illustrates the potential of school health centers as natural sites for interventions to increase HPV vaccination, based on the centers’ current vaccine promotion activities and barriers to providing HPV vaccine. Our findings indicate that cost, parental consent, and recordkeeping demands limit the ability of school health centers to offer HPV vaccine. Nevertheless, school health centers are willing to lead and to partner on interventions to boost uptake of HPV vaccine. Given the low rate of HPV vaccination in the United States and the success of school-based vaccination programs in other countries, interventions at school health centers represent important, underutilized tools that could have valuable public health impact.
Acknowledgments
We thank our participants and their school health centers, the North Carolina School Health Center Alliance, our Advisory Group (Amanda Dayton, Cathy DeMason, Anne Derouin, Dan Garsen-Angert, Chris Minard, Connie Parker, Rebecca Reeve, and Carol Tyson), and additional UNC researchers (Eric Geers, Kim Hayes, and Paul Reiter).
Funding
This study was supported in part by an unrestricted educational grant from GlaxoSmithKline. Additional support provided by the American Cancer Society (MSRG-06-259-01-CPPB) and the Cancer Control Education Program at UNC Lineberger Comprehensive Cancer Center (R25 CA57726).
Footnotes
Human Subjects Approval Statement
The institutional review board of the University of North Carolina reviewed and approved the study protocol.
Conflict of Interest
GlaxoSmithKline played no role in the manuscript design, planning, implementation, analysis, or reporting of the findings. NTB and JSS have received grants, honoraria or consulting fees from GlaxoSmithKline and Merck.
References
- 1.Centers for Disease Control and Prevention (CDC) [Accessed March 8, 2013];HPV and cancer. Available at: http://www.cdc.gov/hpv/cancer.html.
- 2.Villa LL, Costa RL, Petta CA, Andrade RP, Paavonen J, Iversen OE, et al. High sustained efficacy of a prophylactic quadrivalent human papillomavirus types 6/11/16/18 L1 virus-like particle vaccine through 5 years of follow-up. Br J Cancer. 2006;95(11):1459–1466. doi: 10.1038/sj.bjc.6603469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) [Accessed March 8, 2013];HPV vaccines. Available at: http://www.cdc.gov/hpv/vaccine.html.
- 4.Centers for Disease Control and Prevention (CDC) [Accessed March 8, 2013];Recommendations and guidelines: Advisory Committee on Immunization Practices. Available at: http://www.cdc.gov/vaccines/acip/index.html.
- 5.Centers for Disease Control and Prevention (CDC). . National and state vaccination coverage among adolescents aged 13–17 years - United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61:671–677. [PubMed] [Google Scholar]
- 6.Brabin L, Roberts SA, Stretch R, Baxter D, Chambers G, Kitchener H, et al. Uptake of first two doses of human papillomavirus vaccine by adolescent schoolgirls in Manchester: prospective cohort study. BMJ. 2008;336(7652):1056–1058. doi: 10.1136/bmj.39541.534109.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brotherton JM, Deeks SL, Campbell-Lloyd S, Misrachi A, Passaris I, Peterson K, et al. Interim estimates of human papillomavirus vaccination coverage in the school-based program in Australia. Commun Dis Intell. 2008;32(4):457–461. doi: 10.33321/cdi.2008.32.45. [DOI] [PubMed] [Google Scholar]
- 8.Ogilvie G, Anderson M, Marra F, McNeil S, Pielak K, Dawar M, et al. A population-based evaluation of a publicly funded, school-based HPV vaccine program in British Columbia, Canada: parental factors associated with HPV vaccine receipt. PLoS Med. 2010;7(5):e1000270. doi: 10.1371/journal.pmed.1000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reeve C, De La Rue S, Pashen D, Culpan M, Cheffins T. School-based vaccinations delivered by general practice in rural North Queensland: an evaluation of a new human papilloma virus vaccination program. Commun Dis Intell. 2008;32(1):94–98. doi: 10.33321/cdi.2008.32.14. [DOI] [PubMed] [Google Scholar]
- 10.Stretch R. Implementing a school-based HPV vaccination programme. Nurs Times. 2008;104(48):30–33. [PubMed] [Google Scholar]
- 11.Watson M, Shaw D, Molchanoff L, McInnes C. Challenges, lessons learned and results following the implementation of a human papilloma virus school vaccination program in south Australia. Aust N Z J Public Health. 2009;33(4):365–370. doi: 10.1111/j.1753-6405.2009.00409.x. [DOI] [PubMed] [Google Scholar]
- 12.Tan W, Viera AJ, Rowe-West B, Grimshaw A, Quinn B, Walter EB. The HPV vaccine: are dosing recommendations being followed? Vaccine. 2011;29(14):2548–2554. doi: 10.1016/j.vaccine.2011.01.066. [DOI] [PubMed] [Google Scholar]
- 13.Cawley J, Hull HF, Rousculp MD. Strategies for implementing school-located influenza vaccination of children: a systematic literature review. J Sch Health. 2010;80(4):167–175. doi: 10.1111/j.1746-1561.2009.00482.x. [DOI] [PubMed] [Google Scholar]
- 14.Glezen WP, Gaglani MJ, Kozinetz CA, Piedra PA. Direct and indirect effectiveness of influenza vaccination delivered to children at school preceding an epidemic caused by 3 new influenza virus variants. J Infect Dis. 2010;202(11):1626–1633. doi: 10.1086/657089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.King JC, Jr, Stoddard JJ, Gaglani MJ, Moore KA, Magder L, McClure E, et al. Effectiveness of school-based influenza vaccination. N Engl J Med. 2006;355(24):2523–2532. doi: 10.1056/NEJMoa055414. [DOI] [PubMed] [Google Scholar]
- 16.Luthy KE, Thorpe A, Dymock LC, Connely S. Evaluation of an intervention program to increase immunization compliance among school children. J Sch Nurs. 2011;27(4):252–257. doi: 10.1177/1059840510393963. [DOI] [PubMed] [Google Scholar]
- 17.Hall S, Galil K, Watson B, Seward J. The use of school-based vaccination clinics to control varicella outbreaks in two schools. Pediatrics. 2000;105(1):e17. doi: 10.1542/peds.105.1.e17. [DOI] [PubMed] [Google Scholar]
- 18.Stubbs BW, Panozzo CA, Moss JL, Reiter PL, Whitesell DH, Brewer NT. Evaluation of an intervention providing HPV vaccine in schools. Am J Health Behav. doi: 10.5993/AJHB.38.1.10. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hayes KA, Entzel P, Berger W, Caskey RN, Shlay JC, Stubbs BW, et al. Early lessons learned from extramural school programs that offer HPV vaccine. J Sch Health. 2013;83(2):119–126. doi: 10.1111/josh.12007. [DOI] [PubMed] [Google Scholar]
- 20.Allison MA, Crane LA, Beaty BL, Davidson AJ, Melinkovich P, Kempe A. School-based health centers: improving access and quality of care for low-income adolescents. Pediatrics. 2007;120(4):e887–94. doi: 10.1542/peds.2006-2314. [DOI] [PubMed] [Google Scholar]
- 21.Kessels SJ, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: a systematic review. Vaccine. 2012;30(24):3546–3556. doi: 10.1016/j.vaccine.2012.03.063. [DOI] [PubMed] [Google Scholar]
- 22.Daley MF, Curtis CR, Pyrzanowski J, Barrow J, Benton K, Abrams L, et al. Adolescent immunization delivery in school-based health centers: a national survey. J Adolesc Health. 2009;45(5):445–452. doi: 10.1016/j.jadohealth.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 23.Reiter PL, McRee AL, Pepper JK, Chantala K, Brewer NT. Improving human papillomavirus vaccine delivery: a national study of parents and their adolescent sons. J Adolesc Health. 2012;51(1):32–37. doi: 10.1016/j.jadohealth.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kadis JA, McRee AL, Gottlieb SL, Lee MR, Reiter PL, Dittus PJ, et al. Mothers’ support for voluntary provision of HPV vaccine in schools. Vaccine. 2011;29(14):2542–2547. doi: 10.1016/j.vaccine.2011.01.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schaffer SJ, Humiston SG, Shone LP, Averhoff FM, Szilagyi PG. Adolescent immunization practices: a national survey of US physicians. Arch Pediatr Adolesc Med. 2001;155(5):566–571. doi: 10.1001/archpedi.155.5.566. [DOI] [PubMed] [Google Scholar]
- 26.Skinner SR, Cooper Robbins SC. Voluntary school-based human papillomavirus vaccination: an efficient and acceptable model for achieving high vaccine coverage in adolescents. J Adolesc Health. 2010;47(3):215–218. doi: 10.1016/j.jadohealth.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 27.Brener ND, Wheeler L, Wolfe LC, Vernon-Smiley M, Caldart-Olson L. Health services: results from the School Health Policies and Programs study 2006. J Sch Health. 2007;77(8):464–485. doi: 10.1111/j.1746-1561.2007.00230.x. [DOI] [PubMed] [Google Scholar]
- 28.Lindley MC, Boyer-Chu L, Fishbein DB, Kolasa M, Middleman AB, Wilson T, et al. The role of schools in strengthening delivery of new adolescent vaccinations. Pediatrics. 2008;121 (Suppl 1):S46–54. doi: 10.1542/peds.2007-1115F. [DOI] [PubMed] [Google Scholar]
- 29.Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med. 2007;45(2–3):107–114. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 30.Brewer NT, Gottlieb SL, Reiter PL, McRee AL, Liddon N, Markowitz L, et al. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis. 2011;38(3):197–204. doi: 10.1097/OLQ.0b013e3181f12dbf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Keating KM, Brewer NT, Gottlieb SL, Liddon N, Ludema C, Smith JS. Potential barriers to HPV vaccine provision among medical practices in an area with high rates of cervical cancer. J Adolesc Health. 2008;43(4 Suppl):S61–7. doi: 10.1016/j.jadohealth.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 32.Gottlieb SL, Brewer NT, Smith JS, Keating KM, Markowitz LE. Availability of human papillomavirus vaccine at medical practices in an area with elevated rates of cervical cancer. J Adolesc Health. 2009;45(5):438–444. doi: 10.1016/j.jadohealth.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 33.Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100(4):590–595. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chapman GB, Li M, Colby H, Yoon H. Opting in vs opting out of influenza vaccination. JAMA. 2010;304(1):43–44. doi: 10.1001/jama.2010.892. [DOI] [PubMed] [Google Scholar]
- 35.Johnson EJ, Goldstein D. Medicine. Do defaults save lives? Science. 2003;302(5649):1338–1339. doi: 10.1126/science.1091721. [DOI] [PubMed] [Google Scholar]
- 36.Reiter PL, McRee AL, Pepper JK, Brewer NT. Default policies and parents’ consent for school-located HPV vaccination. J Behav Med. 2012 doi: 10.1007/s10865-012-9397-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.North Carolina General Assembly. Minor’s consent sufficient for certain medical health services. 2012. Practice of medicine: treatment of minors: 90-21.5. [Google Scholar]
- 38.Kelminson K, Saville A, Seewald L, Stokley S, Dickinson LM, Daley MF, et al. Parental views of school-located delivery of adolescent vaccines. J Adolesc Health. 2012;51(2):190–196. doi: 10.1016/j.jadohealth.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 39.Reiter PL, Stubbs B, Panozzo CA, Whitesell D, Brewer NT. HPV and HPV vaccine education intervention: effects on parents, healthcare staff, and school staff. Cancer Epidemiol Biomarkers Prev. 2011;20(11):2354–2361. doi: 10.1158/1055-9965.EPI-11-0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.NC State Department of Education. North Carolina public schools’ fast facts. 2011. p. 20110318. [Google Scholar]