Abstract
Objective
Low socioeconomic status (SES) is associated with many adverse health outcomes, including childhood overweight and obesity. However, little is understood about why some children defy this trend by maintaining a healthy weight despite living in obesogenic environments. The objective of this study is to test the hypothesis that the psychological strategy of “shift-and-persist” protects low-SES children from overweight and obesity. Shift-and-persist involves dealing with stressors by reframing them more positively while at the same time persisting in optimistic thoughts about the future.
Design and Methods
Middle school children (N = 1,523, ages 9–15) enrolled in a school-based obesity prevention trial completed health surveys and physical assessments. Multiple linear regression analysis was used to examine the role of SES, shift-and-persist strategies, and their interaction on BMI z-scores, while controlling for student race/ethnicity, gender, and reported diet and physical activity.
Results
Among children reporting engaging in less frequent shift-and-persist strategies, lower SES was associated with significantly higher BMI z-scores (P < 0.05). However, among children reporting engaging in more frequent shift-and-persist strategies, there was no association of SES with BMI z-score (P = 0.16), suggesting that shift-and-persist strategies may be protective against the association between SES and BMI.
Conclusions
Interventions aimed at improving psychological resilience among children of low SES may provide a complementary approach to prevent childhood overweight and obesity among at-risk populations.
Nearly one-third of US children ages 2–19 are overweight (BMI ≥85th and <95th percentile) or obese (BMI ≥ 95th percentile), with higher prevalence among Black and Latino children (1) and those of low socioeconomic status (SES) (2–5). Children from low-SES and disadvantaged backgrounds are more likely to live in “obesogenic environments” that promote sedentary lifestyles and consumption of energy-dense foods (6). For example, those living in obesogenic environments tend to lack access to safe outdoor recreational facilities and full supermarkets that sell a variety of foods (as opposed to small grocery stores) (6,7). Additionally, living in a low-SES environment is associated with experiencing more psychosocial stressors, for example, crowding and violence (8), which are in turn linked to the development of childhood obesity (9).
Despite its elevation as a national priority, interventions aimed at preventing and treating childhood obesity have had only modest success (7,10–12). Many of the strategies to prevent and treat childhood obesity have focused on elucidating behavioral risk factors for becoming overweight/obese (e.g. screen time, sugar-sweetened beverage consumption, sedentary behavior) (11) and implementing interventions to reduce these risks (12). A complementary or alternative approach may be to leverage protective factors some children inherently possess that allow them to maintain a healthy weight despite living in low-SES, obesogenic environments.
Chen and colleagues have documented one such protective psychological factor, “shift-and-persist,” in their exploration of protective factors among low-SES individuals (13–15). They posit that low-SES individuals who are able to develop an approach to life that prioritizes shifting, accepting stress and adapting the self through reappraisals, in combination with persisting, sustaining meaning and optimism about the future, may be protected from some of the negative health effects of low SES and therefore are likely to have better health outcomes than low-SES individuals who do not have these strategies. In a study of over 100 children diagnosed with asthma, engaging in more shift-and-persist strategies was associated with better asthma outcomes for low-SES children. Among low-SES children with asthma, those who reported engaging in more shift-and-persist strategies had fewer baseline biological markers of inflammation and less asthma impairment (reduced rescue inhaler use and fewer school absences) at 6 months, compared to low-SES children who did not report engaging in shift-and-persist strategies. Furthermore, the asthma profiles of low-SES children who were high in shift-and-persist resembled those of high-SES children, indicating that these resilience strategies were able to buffer the negative effects of low SES on asthma (13). Chen and colleagues found a similar protective health effect of shift-and-persist strategies for low-SES individuals in a study of allostatic load and SES (14). Allostatic load refers to the physiologic wear and tear that results from exposure to chronic stressors (16). Using a national sample of 1,207 adults, Chen and colleagues found that among adults from a low-SES background, those who reported the highest levels of shift-and-persist strategies had the lowest allostatic load scores (14). In contrast, there was no benefit of shift-and-persist among adults who came from high childhood socioeconomic backgrounds.
Chen and Miller proposed that shift-and-persist strategies are protective for health because they alter stress-physiology pathways. That is, shift-and-persist strategies mitigate perceptions of stress, thereby reducing acute activation of the hypothalamic–pituitary–adrenal (HPA) axis and the sympathetic nervous system (SNS) (15). Over time, diminished stress reactivity leads to reductions in longer term pathogenic processes, such as systemic inflammation, high blood pressure, and insulin resistance. Shift-and-persist strategies may be particularly adaptive in low-SES contexts where limited resources may make alternative approaches, such as proactive efforts to eliminate stressors, challenging and frustrating. Since chronic activation of the HPA axis has been linked with dysregulation of metabolism and the development of obesity (8,15), shift-and-persist strategies that decrease the stress response may also protect against obesity.
The objective of the present study was to test whether shift-and-persist strategies are protective against the association between low-SES and overweight and obesity among children. We hypothesized that low-SES (measured by eligibility for free or reduced-price lunch) would be associated with higher BMI z-scores for children low in shift-and-persist strategies, but would have no association with BMI-z scores for children high in shift-in-persist strategies.
Methods
Study participants
Data came from a study conducted by CARE – Community Alliance for Research and Engagement at the Yale School of Public Health in partnership with the Rudd Center on Food Policy and Obesity, and the New Haven Public Schools (17). Participants included 1,655 students from grades 5, 7, and 8 from twelve K-8 (kindergarten through grade 8) schools that were randomly selected from the 27 K-8 schools in the district. For the fifth grade cohort, baseline data were collected as part of a larger longitudinal study and for the seventh and eighth grade cohort, follow-up data were collected as part of a separate study. All data collection methods and procedures were identical in the two cohorts of students. Participants represent 85.5% of all eligible children. Those not included were either absent from school during study administration (6.8%) or had parents who requested that they not participate (7.7%). The analytic sample for this study included 1,523 students. Students were excluded if they were missing measures of height and weight (n=4), or missing sociodemographic data from school records (n=128). All procedures were approved by the Yale University Human Subjects Committee and the Board of Education. Parental consent and child assent were obtained for all participants in English or Spanish.
Data collection and measurement
Protocol
Physical measurements were obtained by trained research assistants and were based on the World Health Organization Expanded STEPS protocol (18). Measures were taken privately and recorded with only school-assigned identification numbers to enable data linkage. A standardized stadiometer (Charder Electronic Co., LTD, Taichung City, Taiwan) and digital scale (Seca Corp., Hamburg, Germany) were used to measure height and weight, respectively. Student surveys were administered online (Surveymonkey.-com, LLC; Palo Alto, CA, USA) via desktop computers during regularly scheduled computer classes. To take into account participants’ differing levels of literacy, trained research staff read all questions and responses aloud to the class while students read the survey and entered responses on their computer. Survey administration took approximately 30 min, and a water bottle was given to each child who participated as compensation.
Measures
Primary Outcome: Physical Assessments
Body mass index was calculated using height and weight. Age- and gender-adjusted BMI z-scores were determined for each student based on guidelines established by the Centers for Disease Control and Prevention (19).
Primary Independent Variables: Shift and Persist Strategies
Given limitations in survey duration to comply with the time available during a classroom period, a shortened five-item version of the shift-and-persist measurement (13,14) was used. The three “shift” items were selected from the Responses to Stress questionnaire (20), a validated measure of coping for use in children ages 11–18. Items were taken from the subscales of cognitive restructuring (“I think about the things I can learn from a situation, or about some thing good that can come from it”), positive thinking (“I tell myself that everything will be all right”), and emotion regulation (“I do something to calm myself down”). Two “persist” questions were used: one from the Resilience Inventory (21), a validated measure for children that taps optimism (“I think that things will get better in the future”), and one from the Purpose in Life Scale (22), a version of the commonly used Purpose in Life Test that has been validated in adolescents (“I feel my life has a sense of purpose”). Responses were on a 4-point Likert-type scale (ranging from “not at all” to “a lot”). Responses to the shift-and-persist measures were summed to create a total shift-and-persist score ranging from 0 to 20. Higher scores indicate reporting the use of more shift-and-persist strategies.
Socioeconomic status
Data from school district records on students’ qualification for the free and reduced-price school lunch program were used as the indicator of SES. Low SES was defined as eligibility for free or reduced-price lunch, while higher SES was defined as being ineligible for these programs.
Control variables
Healthy and unhealthy eating
Students were asked questions regarding whether they ate certain foods yesterday. We summed responses to three healthy food items (fruit, vegetables, salad) into an additive “healthy eating index” ranging from 0 to 3, with three representing the healthiest eating. Similarly, we summed responses to five unhealthy food items (french fries, fried chicken, candy, ice cream, sweets) into an additive “unhealthy eating index” ranging from 0 to 5, with five representing the unhealthiest eating.
Physical activity
Based on CDC physical activity recommendations that children exercise for at least 60 minutes a day, students reported the number of days in the past week that they did physical activity for 60 minutes or more (23,24).
Statistical analysis
Descriptive statistics were calculated for all study variables. To test a priori hypotheses regarding the potential differential association of SES with BMI by level of shift-and-persist, multiple linear regression analyses were conducted. BMI z-score was the primary outcome. Primary independent variables included the main effect of shift-and-persist strategies, main effect of SES, and the interaction between shift-and-persist and SES. Including the interaction term allowed us to test the hypothesis that low-SES would be associated with higher BMI z-scores for those low in shift-and-persist strategies, but not those high in shift-and-persist strategies. Tests of interactions were conducted according to the recommendations of Aiken and West (25), whereby variables are first centered and then the interaction is calculated as the product of the two variables. The model adjusted for sex, race/ethnicity, healthy and unhealthy eating indices and physical activity. The latter two measures of diet and physical activity behaviors were included as additional covariates in order to determine whether the relationship between shift and persist and BMI z-scores existed even after accounting for variations in health behaviors. Statistical analyses were performed using SPSS Version 20.0.0.
Results
Description of study participants
The final sample included 1,523 children ages 9–15 years (Table 1). Reflecting school district demographics, Black and Latino students were well represented, making up over 85% of the sample. There was a high prevalence of overweight (20.2%) and an even higher prevalence of obesity (27.4%), together accounting for nearly one-half of the entire sample.
TABLE 1.
Characteristics of study sample (n = 1523)
| Characteristic | N (%) | Mean ± SD |
|---|---|---|
| Age | 12.4 ± 1.3 | |
| Gender | ||
| Female | 819 (53.8%) | |
| Male | 704 (46.2%) | |
| BMI status | ||
| Healthy weight (<85% BMI) | 798 (52.4%) | |
| Overweight (85% ≥ BMI ≤95%) | 307 (20.2%) | |
| Obese (BMI > 95%) | 418 (27.4%) | |
| BMI unadjusted | 22.6 ± 5.6 | |
| Race/ethnicity | ||
| Hispanic | 728 (47.8%) | |
| Black | 583 (38.3%) | |
| White/other | 212 (13.9%) | |
| Socioeconomic status | ||
| Low SES (free/reduced lunch) | 1335 (87.7%) | |
| Higher SES (ineligible) | 188 (12.3%) | |
| Shift-and-Persist Score | 14.97 ± 3.13 | |
Linear regression analysis
Table 2 presents the results of the multiple regression analysis for BMI z-score. After adjusting for sex, race/ethnicity, healthy and unhealthy eating indices, and physical activity, there were no statistically significant main effects for either SES or shift-and-persist strategies on BMI z-score. There was, however, a significant interaction of SES with the shift-and-persist score (P < 0.05). We then conducted follow-up regression analyses with all the same controls, examining the association between SES and BMI z-scores for those high and low in shift-and-persist strategies separately (split at the mean score). In these analyses, low SES was significantly associated with higher BMI z-score among those low in shift-and-persist strategies (β = .09, P = .036), but not for those high in shift-and-persist strategies (β = −.05, P = .158). Figure 1 depicts this interaction graphically.
TABLE 2.
Multiple regression analysis predicting BMI z-score
| Predictor | β | P-value |
|---|---|---|
| SES | 0.01 | 0.78 |
| Shift-and-persist score | 0.09 | 0.23 |
| SES × shift-and-persist score | −0.15 | 0.03 |
Adjusted for sex, race/ethnicity, health and unhealthy eating scales, and physical activity. SES, socioeconomic status (1 = qualifies for free/reduced price lunch, 0 = ineligible for free/reduced price lunch).
FIGURE 1.
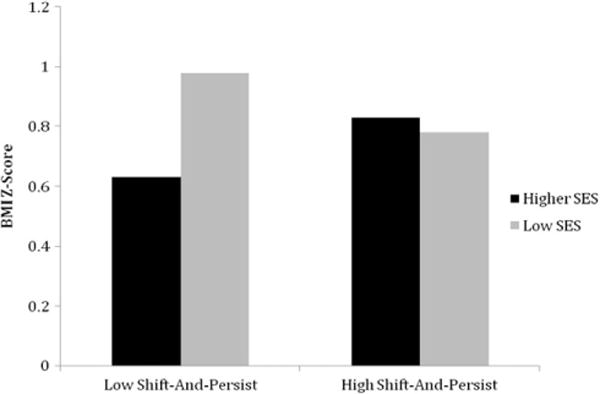
Mean BMI z-scores by SES and level of shift-and-persist. Shift-and-persist level was split at the mean. Low SES was significantly associated with higher BMI z-score for those low in shift-and-persist, but not for those high in shift-and-persist.
Discussion
The results confirmed our hypothesis that low-SES children with psychological resilience, as defined by reporting more frequent shift-and-persist strategies, were protected against the association of low-SES with higher BMI. Low SES was significantly associated with higher BMI z-scores among children reporting lower shift-and-persist strategies. However, low SES had no association with BMI z-scores among those who had higher shift-and-persist strategies. As proposed by Chen et al (15), shifting (working to reinterpret stressors in a more positive light) and persisting (maintaining optimism about the future) may be protective against the negative health impact of low-SES settings where, on average, individuals experience more frequent uncontrollable stressors (26). Findings are consistent with prior research on shift-and-persist strategies by Chen et al. which found that shift-and-persist strategies were protective against severity of asthma in low-SES children (13) and allostatic load in low-SES adults (14). This study is the first to show such a relationship between shift-and-persist strategies and BMI.
We hypothesize that shift-and-persist strategies influence BMI by enabling children to be less reactive to stressors, which in turn decreases the activation of their HPA axis and sympathetic nervous system. Since chronic activation of the HPA axis and SNS has been linked to the accumulation of visceral fat, insulin resistance, and dysregulation of metabolism, decreasing their activation will be beneficial in preventing the development of many chronic diseases, including obesity (15,27). The strategies of shift-and-persist may be particularly adaptive in low-SES settings where limited resources may prevent children from taking active steps to eliminate stressors. Instead, strategies such as shift-and-persist, which involve reframing one’s perception of stressors, may be more beneficial. Alternatively, shift-and-persist may affect BMI by decreasing perception of stress and therefore reducing children’s stress-eating.
Our work has important implications for efforts to reduce the prevalence of overweight and obesity among children of low SES. We identified psychological qualities of resilience that seem to protect children from the adverse impact of low-SES on BMI. It is important to determine whether shift-and-persist strategies can be learned. If so, they may be taught to low-SES children to protect them against weight gain and other negative health outcomes. The beneficial effects of shift-and-persist strategies may be helpful to children of all weight categories because children’s risk of most co-morbidities of overweight and obesity increase continuously with BMI z-score even if they are considered to be at a healthy weight (28). Interventions that promote psychological resiliency have been successful in diverse settings, including preventing depression (29,30) and improving coping skills when being bullied (31). Future studies should examine if such interventions are effective in the prevention of overweight and obesity among low-SES children.
There are several limitations of the present study. Our measure of SES was whether students qualified for free or reduced price lunch. Although this measure is often used in the education literature, it has also come under criticism as a restricted way to assess family SES (32). Unfortunately, the school district collects only limited family demographic information and young children could not reasonably be expected to accurately answer questions regarding parent’s educational attainment or income. Second, our study was cross-sectional in design; therefore, temporal order cannot be determined. In contrast, this study was strengthened by its large sample size and the objective measure of BMI. Furthermore, we take a novel approach of examining a protective rather than risk factor for obesity among low-SES children, and this factor may be amenable to future intervention.
In sum, shift-and-persist strategies protect children from the negative association of low SES with higher BMI. Interventions aimed at promoting psychological resilience and shift-and-persist strategies in low-SES children represent a novel approach that should be added to the arsenal of interventions used to prevent childhood overweight and obesity.
Acknowledgments
This research was conducted in affiliation with Community Interventions for Health, Oxford Health Alliance, Oxford England.
Funding agencies: Funding for this study came from the Patrick and Catherine Weldon Donaghue Medical Research Foundation; The Kresge Foundation, Emerging and Promising Practices; and an R01 from the National Institute for Child and Human Development (1R01 HD070740).
Footnotes
Disclosure: The authors declared no conflict of interest.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shrewsbury V, Wardle J. Socioeconomic status and adiposity in childhood: a systematic review of cross-sectional studies 1990–2005. Obesity. 2008;16:275–284. doi: 10.1038/oby.2007.35. [DOI] [PubMed] [Google Scholar]
- 3.Singh GK, Kogan MD, Van Dyck PC, Siahpush M. Racial/ethnic, socioeconomic, and behavioral determinants of childhood and adolescent obesity in the United States: analyzing independent and joint associations. Ann Epidemiol. 2008;18:682–695. doi: 10.1016/j.annepidem.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Ruijsbroek A, Wijga AH, Kerkhof M, Koppelman GH, Smit HA, Droomers M. The development of socio-economic health differences in childhood: results of the Dutch longitudinal PIAMA birth cohort. BMC Public Health. 2011;11:225. doi: 10.1186/1471-2458-11-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Howe LD, Tilling K, Galobardes B, Smith GD, Ness AR, Lawlor DA. Socioeconomic disparities in trajectories of adiposity across childhood. Int J Pediatr Obes. 2011;6:e144–e153. doi: 10.3109/17477166.2010.500387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev. 2009;31:7–20. doi: 10.1093/epirev/mxp005. [DOI] [PubMed] [Google Scholar]
- 7.Singh GK, Siahpush M, Kogan MD. Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health Aff. 2010;29:503–512. doi: 10.1377/hlthaff.2009.0730. [DOI] [PubMed] [Google Scholar]
- 8.Evans GW. The environment of childhood poverty. American Psychologist. 2004;59:77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- 9.Gundersen C, Mahatmya D, Garasky S, Lohman B. Linking psychosocial stressors and childhood obesity. Obes Rev. 2011;12:e54–63. doi: 10.1111/j.1467-789X.2010.00813.x. [DOI] [PubMed] [Google Scholar]
- 10.Rosenkranz RR, Dzewaltowski DA. Model of the home food environment pertaining to childhood obesity. Nutr Rev. 2008;66:123–40. doi: 10.1111/j.1753-4887.2008.00017.x. [DOI] [PubMed] [Google Scholar]
- 11.Han JC, Lawlor DA, Kimm SY. Childhood obesity. Lancet. 2010;375:1737–1748. doi: 10.1016/S0140-6736(10)60171-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;12:CD001871. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- 13.Chen E, Strunk RC, Trethewey A, Schreier HMC, Maharaj N, Miller GE. Resilience in low-socioeconomic-status children with asthma: Adaptations to stress. J Allergy Clin Immunol. 2011;128:970–976. doi: 10.1016/j.jaci.2011.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen E, Miller GE, Lachman ME, Gruenewald TL, Seeman TE. Protective factors for adults from low-childhood socioeconomic circumstances: the benefits of shift-and-persist for allostatic load. Psychosom Med. 2012;74:178–186. doi: 10.1097/PSY.0b013e31824206fd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen E, Miller GE. “Shift-and-Persist” strategies. Perspect Psychol Sci. 2012;7:135–158. doi: 10.1177/1745691612436694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McEwen BS, Stellar E. Stress and the individual: mechanisms leading to disease. Arch Intern Med. 1993;153:2093–2101. [PubMed] [Google Scholar]
- 17.O’Connor Duffany K, Finegood D, Matthews D, et al. Community Interventions for Health (CIH): a novel approach to tackling the worldwide epidemic of chronic diseases. CVD Prevent Contr. 2011;6:47–56. [Google Scholar]
- 18.WHO. WHO STEPS Surveillance Manual. Geneva: World Health Organization; 2008. [Google Scholar]
- 19.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. 2002;1111:1–190. [PubMed] [Google Scholar]
- 20.Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. J Consult Clin Psychol. 2000;68:976. [PubMed] [Google Scholar]
- 21.Oberle E, Schonert-Reichl K, Zumbo B. Life satisfaction in early adolescence: personal, neighborhood, school, family, and peer influences. J Youth Adolescence. 2011;40:889–901. doi: 10.1007/s10964-010-9599-1. [DOI] [PubMed] [Google Scholar]
- 22.Robbins M, Francis LJ. Religion, personality, and well-being: the relationship between church attendance and purpose in life. J Res Christian Educ. 2000;9:223–238. [Google Scholar]
- 23.Physical Activity for Everyone: Guidelines. Children | DNPAO | CDC. Available at: http://www.cdc.gov/physicalactivity/everyone/guidelines/children.html. Accessed on December 14, 2012.
- 24.Patrick K, Sallis J, Long B. A new tool for encouraging activity: project PACE. Phys Sports Med. 1994;22:45–55. doi: 10.1080/00913847.1994.11947706. [DOI] [PubMed] [Google Scholar]
- 25.Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. London: Sage Publications, Inc; 1991. [Google Scholar]
- 26.Brady SS, Matthews KA. The influence of socioeconomic status and ethnicity on adolescents’ exposure to stressful life events. J Pediatr Psychol. 2002;27:575–583. doi: 10.1093/jpepsy/27.7.575. [DOI] [PubMed] [Google Scholar]
- 27.Nieuwenhuizen AG, Rutters F. The hypothalamic-pituitary-adrenal-axis in the regulation of energy balance. Physiol Behav. 2008;94:169–177. doi: 10.1016/j.physbeh.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 28.Bell LM, Byrne S, Thompson A, et al. Increasing body mass index z-score is continuously associated with complications of overweight in children, even in the healthy weight range. J Clin Endocrinol Metab. 2006;92:517–522. doi: 10.1210/jc.2006-1714. [DOI] [PubMed] [Google Scholar]
- 29.Cutuli JJ, Chaplin TM, Gillham JE, Reivich KJ, Seligman MEP. Preventing co-occurring depression symptoms in adolescents with conduct problems: the Penn Resiliency Program. Ann N Y Acad Sci. 2006;1094:282–286. doi: 10.1196/annals.1376.035. [DOI] [PubMed] [Google Scholar]
- 30.Brunwasser SM, Gillham JE, Kim ES. A meta-analytic review of the Penn Resiliency Program’s effect on depressive symptoms. J Consult Clin Psychol. 2009;77:1042–1054. doi: 10.1037/a0017671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vessey JA, O’Neill KM. Helping students with disabilities better address teasing and bullying situations: a MASNRN study. J Sch Nurs. 2011;27:139–148. doi: 10.1177/1059840510386490. [DOI] [PubMed] [Google Scholar]
- 32.Harwell M, LeBeau B. Student eligibility for a free lunch as an SES measure in education research. Educ Res. 2010;39:120–131. [Google Scholar]


