Abstract
AIM: To determine the efficacy and safety benefits of performing intraoperative cholangiography (IOC) during laparoscopic cholecystectomy (LC) to treat symptomatic cholelithiasis.
METHODS: Patients admitted to the Minimally Invasive Surgery Center of Tianjin Nankai Hospital between January 2012 and January 2014 for management of symptomatic cholelithiasis were recruited for this prospective randomized trial. Study enrollment was offered to patients with clinical presentation of biliary colic symptoms, radiological findings suggestive of gallstones, and normal serum biochemistry results. Study participants were randomized to receive either routine LC treatment or LC + IOC treatment. The routine LC procedure was carried out using the standard four-port technique; the LC + IOC procedure was carried out with the addition of meglumine diatrizoate (1:1 dilution with normal saline) injection via a catheter introduced through a small incision in the cystic duct made by laparoscopic scissors. Operative data and postoperative outcomes, including operative time, retained common bile duct (CBD) stones, CBD injury, other complications and length of hospital stay, were recorded for comparative analysis. Inter-group differences were statistically assessed by the χ2 test (categorical variables) and Fisher’s exact test (binary variables), with the threshold for statistical significance set at P < 0.05.
RESULTS: A total of 371 patients were enrolled in the trial (late-adolescent to adult, age range: 16-70 years), with 185 assigned to the routine LC group and 186 to the LC + IOC group. The two treatment groups were similar in age, sex, body mass index, duration of symptomology, number and size of gallstones, and clinical symptoms. The two treatment groups also showed no significant differences in the rates of successful LC (98.38% vs 97.85%), CBD stone retainment (0.54% vs 0.00%), CBD injury (0.54% vs 0.53%) and other complications (2.16% vs 2.15%), as well as in duration of hospital stay (5.10 ± 1.41 d vs 4.99 ± 1.53 d). However, the LC + IOC treatment group showed significantly longer mean operative time (routine LC group: 43.00 ± 4.15 min vs 52.86 ± 4.47 min, P < 0.01). There were no cases of fatal complications in either group. At the one-year follow-up assessment, one patient in the routine LC group reported experiencing diarrhea for three months after the LC and one patient in the LC + IOC group reported on-going intermittent epigastric discomfort, but radiological examination provided no abnormal findings.
CONCLUSION: IOC addition to the routine LC treatment of symptomatic cholelithiasis does not improve rates of CBD stone retainment or bile duct injury but lengthens operative time.
Keywords: Cholelithiasis, Cholecystectomy, Cholangiography, Laparoscopic, Gallstones
Core tip: The clinical benefits, in terms of efficacy and safety, of performing the additional intraoperative cholangiography (IOC) procedure during laparoscopic cholecystectomy (LC) treatment in patients with symptomatic cholelithiasis are not definitively established. This prospective randomized trial was designed to compare the operative and outcome features of patients treated by routine LC or LC + IOC. No statistically significant benefits were found for rates of common bile duct (CBD) stone retainment, CBD injury or other complications, or length of hospital stay, but the LC + IOC treatment required significantly longer operative time.
INTRODUCTION
Since its clinical introduction approximately 25 years ago, the laparoscopic cholecystectomy (LC) procedure has replaced open surgery as the gold standard treatment for symptomatic cholelithiasis[1-5]. Unfortunately, the more restricted working area and finer manipulation of tools required by the LC procedure increase the risk of bile duct injury[6-10]. The intraoperative cholangiography (IOC) procedure, in which a catheter is introduced into the common bile duct (CBD) for drainage of bile and injection of dye, can improve visualization of the bile duct anatomy and help the laparoscopist to avoid LC-induced damage. While the combination of LC + IOC is frequently used in medical centers worldwide, no systematic study has conclusively defined the precise benefits to patients, in terms of efficacy and safety, as compared to the routine LC procedure alone.
This prospective randomized trial was designed to determine whether patients who received LC + IOC to treat symptomatic cholelithiasis had better operative and outcome features than those treated by routine LC alone.
MATERIALS AND METHODS
Ethics statement
The study protocol was approved by the Research Ethics Committee of Tianjin Nankai Hospital (Tianjin, China).
Study design
Patients admitted to the Minimally Invasive Surgery Center of Tianjin Nankai Hospital for management of symptomatic cholelithiasis between January 2012 and January 2014 were recruited for the trial. Study enrollment was offered to late-adolescent (≥ 16 years) and adult patients with clinical presentation of biliary colic symptoms, radiological findings suggestive of gallstones, and serum biochemistry results in the normal range (such as bilirubin, alkaline phosphatase and alanine aminotransferase levels). Patients were denied enrollment if any of the following conditions were present[11,12]: current suspicion or diagnosis of CBD stones or history of CBD stones; active acute pancreatitis; pregnancy; septic shock; intrahepatic gallstones or intrahepatic duct dilatation; malignant pancreatic or biliary tumors; prior sphincterotomy; unfit for anesthesia and surgery; contraindications to meglumine diatrizoate; liver cirrhosis; history of abdominal surgery; history of jaundice; dilated CBD (diameter > 8 mm); primary sclerosing cholangitis; inability to give informed consent for study participation.
All study participants provided informed consent and were randomly assigned to undergo routine LC treatment or LC + IOC treatment by using the sealed envelope protocol. All surgical operations were performed by a single laparoscopist who has LC experience with > 2000 cases.
LC and IOC procedures
The routine LC procedure was conducted using the standard four-port technique[13,14]. The IOC procedure was carried out first using laparoscopic scissors to make a small hole in the cystic duct and then inserting a catheter and injecting a 1:1 dilution of normal saline:meglumine diatrizoate (Melamine Diatrizoate Injection; Hansen Pharmaceuticals Company, Yiyang, China). The biliary anatomy was visualized dynamically using a mobile C-arm machine equipped with an image intensifier (SIEMENS AG, Siremobile Compact L, Germany). The laparoscopic CBD exploration or laparotomy procedure was initiated only after it had been verified that no filling defects or injury was present in the CBD.
The operative time was measured as the duration of pneumoperitoneum. LC success was defined as successful removal of the gallbladder by laparoscopic surgery.
All patients, regardless of treatment group, were administered pre-operative antibiotics, and the antibiotic course was not continued postoperatively. All patients attended a 12-mo follow-up in the outpatient clinic.
Statistical analysis
Quantitative data are presented as mean ± SD. Inter-group differences were assessed using the χ2 test (for categorical variables) and Fisher’s exact test (for binary variables). The threshold for a statistically significant difference was set as a P-value < 0.05. All statistical analyses were performed using SPSS for Windows, Version 16.0 (SPSS Inc., Chicago, IL, United States).
RESULTS
Study population and treatment groups
As shown in Figure 1, a total of 544 patients met the initial inclusion criteria. Of those, 119 patients declined the offer of enrollment and 21 were denied enrollment due to the presence of CBD stones or B-ultrasound-verified CBD dilation > 8 mm (n = 21). Thus, the initial study population consisted of 404 patients, which were divided equally into the routine LC group and the LC + IOC group (n = 202 each). However, only 371 of these patients were included in the final analysis as a result of loss to follow-up (n = 17, routine LC group; n = 10, LC + IOC group) and failure to complete the attempted IOC procedure due to severe adhesions in the cystohepatic triangle (n = 6).
Figure 1.
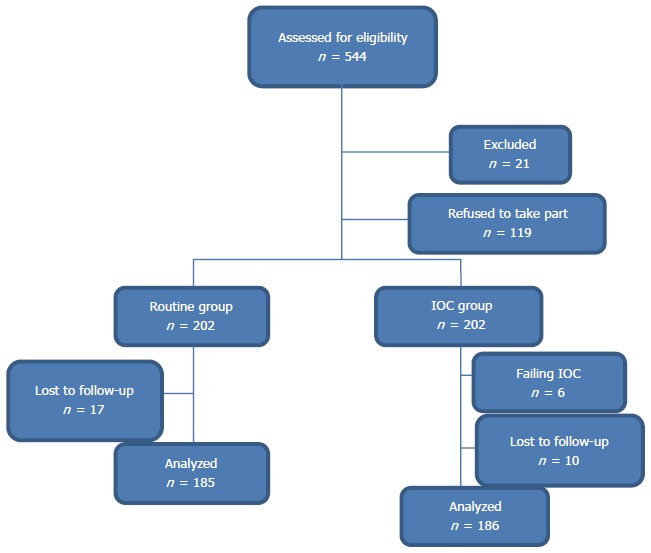
Flow chart of selection process for study participants. IOC: Intraoperative cholangiography.
The subjects in the two treatment groups were not significantly different in regards to patient characteristics (age, sex, and body mass index) and disease characteristics (duration of symptoms, number and size of gallstones, and clinical symptoms) (Table 1).
Table 1.
Patient and pre-operative disease characteristics of the study participants randomly assigned to the routine laparoscopic cholecystectomy or laparoscopic cholecystectomy + intraoperative cholangiography treatment groups n (%)
| Characteristic | Routine LC group, | LC + IOC group, | P value |
| n = 185 | n = 186 | ||
| Age1 (yr) | 58.22 ± 8.41 | 57.43 ± 7.15 | 0.33 |
| Female sex | 97 (52.43) | 101 (54.30) | 0.72 |
| BMI1, | 24.14 ± 1.12 | 23.96 ± 1.89 | 0.27 |
| Clinical symptoms | |||
| Intermittent abdominal pain | 176 (95.14) | 179 (96.24) | 0.60 |
| Fever | 46 (24.86) | 49 (26.34) | 0.74 |
| Nausea/vomiting | 28 (15.14) | 31 (16.67) | 0.69 |
| Symptom duration1 (d) | 3.46 ± 1.82 | 3.50 ± 2.22 | 0.48 |
| Gallstone maximum size1 (cm) | 1.42 ± 0.23 | 1.39 ± 0.21 | 0.19 |
| Multiple gallstones, ≥ 3 | 46 (24.86) | 48 (25.81) | 0.84 |
Data are presented as mean ± SD. BMI: body mass index; LC: Laparoscopic cholecystectomy; IOC: Intraoperative cholangiography.
LC and LC + IOC operative characteristics
The LC success rates were similar between the two treatment groups (routine LC group: 98.38% vs LC + IOC: 97.85%). The rates of conversion to open surgery for structural complications were also similar between the two treatment groups (routine LC group: 1.62% vs IL + IOC: 2.15%), with patients in the routine LC group requiring conversion due to adhesions and fibrosis around the gallbladder caused by recurrent cholecystitis, and patients in the LC + IOC group requiring conversion due to extensive fibrosis of Calot’s triangle caused by recurrent cholecystitis. In addition, the rates of CBD injury were similar between the two groups (routine LC group: 0.54% vs LC + IOC group: 0.54%), with the injured condition in the routine LC group patient necessitating conversion to open surgery and the injured condition in the LC + IOC group necessitating conversion to laparoscopic CBD exploration and T tube drainage. The operative time was significantly different between the two groups, with the LC + IOC surgery requiring approximately 10 more minutes, but the duration of postoperative hospital stay was similar for the two groups. The data are presented in Table 2.
Table 2.
Operative characteristics of laparoscopic cholecystectomy and laparoscopic cholecystectomy + intraoperative cholangiography
| Characteristic | Routine LC group, | LC + IOC group, | P value |
| n = 185 | n = 186 | ||
| Successful LC completion | 182 | 182 | 0.71 |
| Conversion to open surgery | 3 | 4 | 0.71 |
| CBD injury | 1 | 1 | 0.75 |
| Operative time1 (min) | 43.00 ± 4.15 | 52.86 ± 4.47 | < 0.01 |
| Hospital stay1 (d) | 5.10 ± 1.41 | 4.99 ± 1.53 | 0.47 |
Data are presented as mean ± SD. LC: Laparoscopic cholecystectomy; IOC: Intraoperative cholangiography; CBD: Common bile duct.
Outcomes and complications of LC and LC + IOC
During the in-hospital recovery period, one patient in the routine LC group complained of continuous epigastric discomfort, and evaluation by B-ultrasound scanning showed residual CBD stones. There was a similar rate of postoperative complications in the two groups (routine LC group: 1.08% vs LC + IOC group: 1.08%); the complications in the LC group were bile leakage (n = 1) and wound infection (n = 1), while those in the LC + IOC group were postoperative pneumonitis (n = 1) and hydrops in the gallbladder bed (n = 1). There were no fatal complications in either group.
At the 12-mo follow-up, only one patient in each group made complaints of symptoms possibly related to the disease or treatment procedure. The patient in the routine LC group reported experiencing diarrhea for three months after the LC, which was self-limiting. The patient in the IOC group reported experiencing on-going intermittent epigastric discomfort; however, imaging evaluation, including magnetic resonance cholangiopancreatography and computed tomography, found no abnormalities. These data are presented in Table 3.
Table 3.
Outcomes and complications of laparoscopic cholecystectomy and laparoscopic cholecystectomy + intraoperative cholangiography
| Characteristic | Routine LC group, | LC + IOC group, | P value |
| n = 185 | n = 186 | ||
| CBD stone retainment | 1 | 0 | 0.50 |
| Other complications | 2 | 2 | 0.64 |
LC: Laparoscopic cholecystectomy; IOC: Intraoperative cholangiography; CBD: Common bile duct.
DISCUSSION
The addition of IOC during LC treatment of gallstone disease is routinely practiced and considered beneficial for delineating biliary anatomy and identifying stones in the CBD. However, the efficacy and safety of this combined approach, as opposed to the LC procedure alone, remain to be definitively established. Advocates of the combined approach argue that IOC may help laparoscopists to avoid inducing bile duct injury and may lower the risk of CBD stone retainment. Meanwhile, opponents argue that this additional procedure may provide minimal or no benefit while complicating the operative conditions.
Our medical center began performing LC surgery in 1992 and has subsequently accumulated substantial clinical experience in laparoscopic surgery treatment of cholelithiasis, applied to > 50000 cases to date. Recording and analysis of performance metrics in our hospital revealed an increase in cases of LC-related CBD injury and CBD stone retainment over the past two decades. We made the general observation that the increases in these unsatisfactory cases coincided with the introduction and more routine practice of IOC in LC. When a detailed audit of the hospital’s metric data proved inadequate to determine whether IOC is necessary during LC (improving efficacy while having a sufficient safety profile), we designed the current prospective randomized trial.
The results of this trial indicate that the addition of IOC to the LC procedure has no significant effect on rates of success for LC completion, CBD stone retainment, CBD injury, or treatment-related complications. However, the IOC procedure did lengthen the operative time. We also found a less than absolute rate of success for IOC completion, yet our rate (3.23%) was higher that those previously reported by others[15]. Our relatively high success rate for IOC may reflect the extensive experience of our laparoscopists and their surgical support teams and/or general advancements in instrumentation and imaging quality[11]. Nonetheless, it should be noted that in the single case of biliary duct injury that occurred in our LC + IOC case series, the IOC procedure did identify the very tiny injury that was not obvious to the naked eye. In addition, one patient in the routine LC group experienced bile leakage and it is possible that this condition would have been observed and avoided if the IOC had been performed.
In conclusion, our symptomatic cholelithiasis case series showed no statistically significant advantage for the use of IOC during LC; specifically, it did not improve the rates of CBD stone retainment or bile duct injury. Performance of the additional IOC procedure did, however, lengthen the operative time, complicating the surgery and possibly introducing more opportunities for detrimental outcomes. Therefore, the results from this trial do not support the routine use of IOC in LC for patients who have symptomatic cholelithiasis. Larger studies, using broader ranges of patient demographics, treating physicians, and hospitals, are required to confirm our findings and indicate their generalizability to other cholelithiasis patient populations.
COMMENTS
Background
Intraoperative cholangiography (IOC) may help laparoscopists visualize the biliary anatomy and common bile duct (CBD) stones during the laparoscopic cholecystectomy (LC) procedure to treat symptomatic cholelithiasis. Despite IOC being routinely practiced in LC, there is no evidence-based consensus on whether or not the IOC procedure provides sufficient efficacious and safe benefits to justify its routine application.
Research frontiers
This study was conducted with a case series treated in the Minimally Invasive Surgery Center of Tianjin Nankai Hospital, one of the earliest adopters of LC in China and having experience with > 50000 cases. The case series evaluated in this prospective randomized trial encompasses two decades of clinical experience.
Innovations and breakthroughs
Comparative analysis of symptomatic cholelithiasis patients treated by either LC alone or LC + IOC showed no benefits in improving operative outcome. The lack of efficacious advantage does not justify the complicating nature of performing IOC routinely in LC for this patient population.
Applications
Laparoscopy care teams and hospital policy teams should consider the risk-benefit ratio of routinely applying IOC in LC; this may be especially important in China, where surgeons face an overload of operations on a daily basis.
Terminology
Intraoperative cholangiography is a procedure that introduces a catheter into the common bile duct for drainage of bile and injection of dye, both of which can improve visualization of the bile duct anatomy and help avoid LC-induced damage.
Peer-review
The authors conducted the randomized prospective study to investigate the influence of IOC during laparoscopic cholecystectomy for cholelithiasis. They concluded that IOC does not prevent retained common bile duct stones and bile duct injury.
Footnotes
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: June 25, 2014
First decision: July 21, 2014
Article in press: October 15, 2014
P- Reviewer: Dasari BVM, Murata A, Singhal V S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Liu XM
References
- 1.Kim EY, You YK, Kim DG, Lee SH, Han JH, Park SK, Na GH, Hong TH. Is a drain necessary routinely after laparoscopic cholecystectomy for an acutely inflamed gallbladder? A retrospective analysis of 457 cases. J Gastrointest Surg. 2014;18:941–946. doi: 10.1007/s11605-014-2457-9. [DOI] [PubMed] [Google Scholar]
- 2.Randial Pérez LJ, Fernando Parra J, Aldana Dimas G. [The safety of early laparoscopic cholecystectomy (& lt; 48 hours) for patients with mild gallstone pancreatitis: a systematic review of the literature and meta-analysis] Cir Esp. 2014;92:107–113. doi: 10.1016/j.ciresp.2013.01.024. [DOI] [PubMed] [Google Scholar]
- 3.Dawe SR, Windsor JA, Broeders JA, Cregan PC, Hewett PJ, Maddern GJ. A systematic review of surgical skills transfer after simulation-based training: laparoscopic cholecystectomy and endoscopy. Ann Surg. 2014;259:236–248. doi: 10.1097/SLA.0000000000000245. [DOI] [PubMed] [Google Scholar]
- 4.Lee SC, Choi BJ, Kim SJ. Two-port cholecystectomy maintains safety and feasibility in benign gallbladder diseases: a comparative study. Int J Surg. 2014;12:1014–1019. doi: 10.1016/j.ijsu.2014.06.017. [DOI] [PubMed] [Google Scholar]
- 5.Agrusa A, Romano G, Frazzetta G, Chianetta D, Sorce V, Di Buono G, Gulotta G. Role and outcomes of laparoscopic cholecystectomy in the elderly. Int J Surg. 2014;12 Suppl 2:S37–S39. doi: 10.1016/j.ijsu.2014.08.385. [DOI] [PubMed] [Google Scholar]
- 6.Sugawara G, Ebata T, Yokoyama Y, Igami T, Mizuno T, Nagino M. Management strategy for biliary stricture following laparoscopic cholecystectomy. J Hepatobiliary Pancreat Sci. 2014;21:889–895. doi: 10.1002/jhbp.151. [DOI] [PubMed] [Google Scholar]
- 7.Williamson JM. Bile duct injury following laparoscopic cholecystectomy. Br J Hosp Med (Lond) 2014;75:325–330. doi: 10.12968/hmed.2014.75.6.325. [DOI] [PubMed] [Google Scholar]
- 8.Fullum TM, Downing SR, Ortega G, Chang DC, Oyetunji TA, Van Kirk K, Tran DD, Woods I, Cornwell EE, Turner PL. Is laparoscopy a risk factor for bile duct injury during cholecystectomy? JSLS. 2013;17:365–370. doi: 10.4293/108680813X13654754535638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lau WY, Lai EC, Lau SH. Management of bile duct injury after laparoscopic cholecystectomy: a review. ANZ J Surg. 2010;80:75–81. doi: 10.1111/j.1445-2197.2009.05205.x. [DOI] [PubMed] [Google Scholar]
- 10.Głuszek S, Kot M, Bałchanowski N, Matykiewicz J, Kuchinka J, Kozieł D, Wawrzycka I. Iatrogenic bile duct injuries--clinical problems. Pol Przegl Chir. 2014;86:17–25. doi: 10.2478/pjs-2014-0004. [DOI] [PubMed] [Google Scholar]
- 11.Khan OA, Balaji S, Branagan G, Bennett DH, Davies N. Randomized clinical trial of routine on-table cholangiography during laparoscopic cholecystectomy. Br J Surg. 2011;98:362–367. doi: 10.1002/bjs.7356. [DOI] [PubMed] [Google Scholar]
- 12.Prevot F, Rebibo L, Cosse C, Browet F, Sabbagh C, Regimbeau JM. Effectiveness of intraoperative cholangiography using indocyanine green (versus contrast fluid) for the correct assessment of extrahepatic bile ducts during day-case laparoscopic cholecystectomy. J Gastrointest Surg. 2014;18:1462–1468. doi: 10.1007/s11605-014-2560-y. [DOI] [PubMed] [Google Scholar]
- 13.Gurusamy KS, Vaughan J, Ramamoorthy R, Fusai G, Davidson BR. Miniports versus standard ports for laparoscopic cholecystectomy. Cochrane Database Syst Rev. 2013;8:CD006804. doi: 10.1002/14651858.CD006804.pub3. [DOI] [PubMed] [Google Scholar]
- 14.Iranmanesh P, Frossard JL, Mugnier-Konrad B, Morel P, Majno P, Nguyen-Tang T, Berney T, Mentha G, Toso C. Initial cholecystectomy vs sequential common duct endoscopic assessment and subsequent cholecystectomy for suspected gallstone migration: a randomized clinical trial. JAMA. 2014;312:137–144. doi: 10.1001/jama.2014.7587. [DOI] [PubMed] [Google Scholar]
- 15.Nieuwenhuijs VB. Impact of routine intraoperative cholangiography during laparoscopic cholecystectomy on bile duct injury (Br J Surg 2014; 101: 677-684) Br J Surg. 2014;101:685. doi: 10.1002/bjs.9524. [DOI] [PubMed] [Google Scholar]


