Abstract
Schwannomas are rarely observed in the gastrointestinal tract. The most common symptoms of a gastric schwannoma are abdominal pain or dyspepsia, gastrointestinal bleeding, and an abdominal mass. Many gastric schwannomas are asymptomatic and are discovered incidentally or at postmortem. The diagnosis of a schwannoma is based on immunohistochemical positivity for S-100 protein. We present a case report of a rare complication of gastric schwannoma causing gastroduodenal intussusception that was successfully managed by a Billroth II distal gastrectomy. In this rare case, the patient had intermittent, colicky abdominal pain, nausea, and vomiting for over 4 wk accompanied by a weight loss. A diagnosis of gastric intussusception was made by computed tomography. A Billroth II distal gastrectomy was then performed, and complete en bloc removal (R0 resection) was achieved. Pathology confirmed a gastric schwannoma through positive immunohistochemical staining for S-100 protein.
Keywords: Gastroduodenal intussusception, Gastric schwannoma
Core tip: Schwannomas are rarely observed in the gastrointestinal tract. We present a case report of a rare complication of gastric schwannoma causing gastroduodenal intussusception that was successfully managed by a Billroth II distal gastrectomy.
INTRODUCTION
Schwannomas, also known as neurinomas, are tumors originating from any nerve that has a Schwann cell sheath[1]. Schwannomas are rarely observed in the gastrointestinal tract; when they do occur there, the most common site is the stomach. The most common symptoms of a gastric schwannoma are abdominal pain or dyspepsia, gastrointestinal bleeding, and an abdominal mass[2]. Imaging modalities, such as computed tomography (CT), magnetic resonance imaging (MRI), esophagogastroduodenoscopy (EGD), and endoscopic ultrasound (EUS), might offer useful preliminary diagnostic information. Pre-operative investigation is not pathognomonic; therefore, many schwannomas are diagnosed as gastrointestinal stromal tumors (GISTs). The diagnosis of a schwannoma is based on immunohistochemical positivity for S-100 protein, a calcium-binding protein found within cell lines of neural crest origin[3]. Gastric schwannomas are almost uniformly benign, and surgery is regarded as the curative treatment of choice.
We present a case report of a gastric schwannoma causing gastroduodenal intussusception that was treated by Billroth II distal gastrectomy, which resulted in complete en bloc removal (R0 resection).
CASE REPORT
A 69-year-old man was admitted due to intermittent, colicky abdominal pain, nausea, and vomiting for over 4 wk, accompanied by a weight loss (5 kg in 4 wk). A clinical examination revealed succession splash. CT showed that a pedunculated soft tissue tumor mass at the gastric antrum, including the stomach wall and its outer mesentery, had telescoped into the duodenum through the gastric pylorus (Figure 1). We diagnosed that the gastric intussusception was likely induced by an antrum gastrointestinal stromal tumor. A conventional laparotomy was then performed, which showed an indentation of the inferior aspect of the gastric antrum with no evidence of metastasis, as seen below (Figures 2 and 3). A Billroth II distal gastrectomy was then performed, and complete en bloc removal (R0 resection) was achieved. Pathological analysis of the gastric mass confirmed a gastric schwannoma through positive immunohistochemical staining for S-100 protein and vimentin, whereas CD117, CD34, β-catenin, smooth muscle actin, synaptophysin, chromogranin and desmin were negative (Figure 4). The patient had an uneventful recovery and was discharged on his tenth day of hospitalization.
Figure 1.
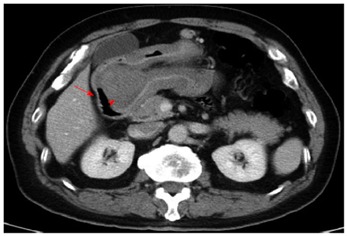
Computed tomography scan revealed a gastroduodenal intussusception of the gastric tumor. The red arrow marks the duodenum. The red arrowhead marks the tumor in the duodenum.
Figure 2.

Indentation at the antrum, the origin of intussusception.
Figure 3.

Macroscopic view of the resected specimen shows a lobulated polypoid gastric tumor measuring 50 mm × 50 mm × 48 mm, located at the gastric antrum, which did not infiltrate the mucosa.
Figure 4.
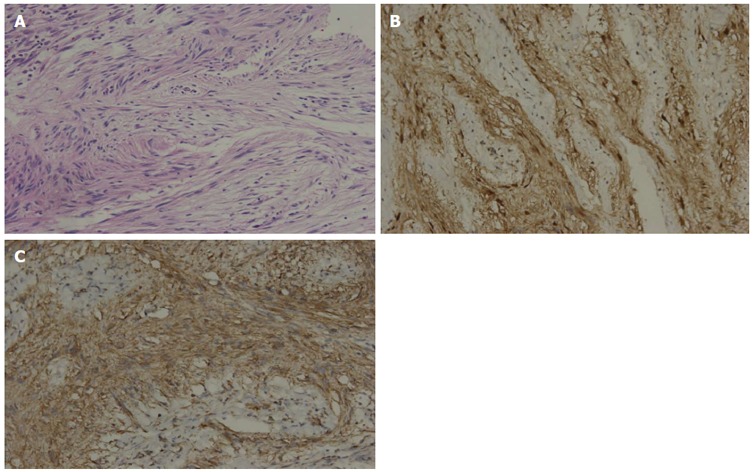
Pathological analysis of the gastric mass confirmed a gastric schwannoma through positive immunohistochemical staining for S-100 protein and vimentin, whereas CD117, CD34, β-catenin, smooth muscle actin, synaptophysin, chromogranin and desmin were negative. A: The tumor showed typical features of a spindle cell tumor with moderate nuclear pleomorphism but no mitotic activity (original magnification: × 200); B: S-100 protein immunostaining demonstrated strong nuclear and cytoplasmic immunoreactivity; C: Vimentin protein immunostaining demonstrated strong cytoplasmic immunoreactivity.
DISCUSSION
Gastroduodenal intussusception occurs in only 10% of adult intussusceptions[4]. Various gastric lesions, including adenocarcinoma, adenoma, GIST[5] and, as in our case, gastric schwannoma, can lead to intussusception. No previous case report has described gastroduodenal intussusception caused by gastric schwannoma, as was illustrated in our case.
A very rare complication of gastric schwannoma is gastroduodenal intussusception caused by the propulsion and prolapse of the tumor through the pylorus and into the duodenum[6]. The rarity of this condition is explained by the fact that the gastric cardia, the pylorus, and the duodenum are much more fixed than the rest of the alimentary tract. The intussusception presents as a partial or complete gastric outlet obstruction, resulting in severe, intractable pain, nausea, vomiting, and even shock[7]. The preoperative diagnosis of gastroduodenal intussusception is not difficult; however, imaging modalities, such as CT, MRI, EGD and EUS, only offer preliminary diagnostic etiologic information[8]. Schwannomas are easily misdiagnosed, frequently as GISTs, and their true nature is revealed only through accurate histological and immunohistochemical analysis. The diagnosis of schwannoma is based on immunohistochemical positivity for S-100 protein, a family of calcium-binding proteins found within cell lines of neural crest origin[9]. Digestive tract schwannomas never express CD117, CD34, c-kit, or DOG-1, in contrast to GISTs[10]. Our case was misdiagnosed as a GIST until these histological and immunohistochemical findings were revealed.
The definitive therapy for gastric schwannoma is surgical resection. Operations should follow the same principles as those for GISTs[11]. All tumors should be completely resected en bloc with the surrounding normal tissue, including the adjacent involved structures. Local extirpation, wedge resection, and partial, subtotal, or even total gastrectomy are all acceptable procedures[12]. Resection can be achieved via a laparoscopic or open approach. In our case, a symptomatic schwannoma of the gastric antrum approximately 5 cm in diameter was treated by a Billroth II distal gastrectomy, and the diagnosis was established microscopically and immunohistochemically after surgery.
Gastroduodenal intussusception is an uncommon complication of gastric schwannoma that typically presents as a gastric outlet obstruction. We report a patient with a gastric schwannoma who presented with a gastroduodenal intussusception. Moreover, we highlight how the tumor may be misdiagnosed pre-operatively despite both endoscopic and radiological assessments. The diagnosis of schwannoma is based on immunohistochemical positivity for S-100 protein. Resection surgery should be considered curative because such tumors are benign.
COMMENTS
Case characteristics
A 69-year-old man was admitted due to intermittent, colicky abdominal pain, nausea, and vomiting for over 4 wk, accompanied by a weight loss.
Clinical diagnosis
We diagnosed a likely gastric intussusception induced by a gastric tumor.
Differential diagnosis
Gastrointestinal stromal tumor, gastric cancer, and gastric adenoma.
Laboratory diagnosis
Routine blood test, metabolic panel, and liver function test were within normal limits.
Imaging diagnosis
A computed tomography scan revealed a gastroduodenal intussusception secondary to a gastric tumor.
Pathological diagnosis
Immunohistochemical staining revealed S-100/vimentin positivity, whereas tests for CD117, CD34, β-catenin, smooth muscle actin, synaptophysin, chromogranin, and desmin were negative.
Treatment
A Billroth II distal gastrectomy was performed, and complete en bloc removal (R0 resection) was achieved.
Term explanation
Schwannomas, also known as neurinomas, are tumors originating from any nerve that has a Schwann cell sheath.
Experiences and lessons
This case report demonstrates that gastroduodenal intussusception is an uncommon complication of gastric schwannomas. Moreover, such tumors may be misdiagnosed pre-operatively despite both endoscopic and radiological assessments. The diagnosis of schwannoma is based on immunohistochemical positivity for S-100 protein.
Peer-review
The case report entitled ”gastroduodenal intussusception due to gastric schwannoma treated by Billroth II distal gastrectomy” is interesting and well written.
Footnotes
Supported by Department of General Surgery, Putuo Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai, China.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: July 8, 2014
First decision: August 6, 2014
Article in press: September 30, 2014
P- Reviewer: Fiori E, Luo JC S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Liu XM
References
- 1.Lin CS, Hsu HS, Tsai CH, Li WY, Huang MH. Gastric schwannoma. J Chin Med Assoc. 2004;67:583–586. [PubMed] [Google Scholar]
- 2.Alvarez JF, Ben-David K. Gastric schwannoma: a rare find. J Gastrointest Surg. 2013;17:2179–2181. doi: 10.1007/s11605-013-2387-y. [DOI] [PubMed] [Google Scholar]
- 3.Agaimy A, Märkl B, Kitz J, Wünsch PH, Arnholdt H, Füzesi L, Hartmann A, Chetty R. Peripheral nerve sheath tumors of the gastrointestinal tract: a multicenter study of 58 patients including NF1-associated gastric schwannoma and unusual morphologic variants. Virchows Arch. 2010;456:411–422. doi: 10.1007/s00428-010-0886-8. [DOI] [PubMed] [Google Scholar]
- 4.Stubenbord WT, Thorbjarnarson B. Intussusception in adults. Ann Surg. 1970;172:306–310. doi: 10.1097/00000658-197008000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rittenhouse DW, Lim PW, Shirley LA, Chojnacki KA. Gastroduodenal intussusception of a gastrointestinal stromal tumor (GIST): case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 2013;23:e70–e73. doi: 10.1097/SLE.0b013e31826d72d4. [DOI] [PubMed] [Google Scholar]
- 6.Crowther KS, Wyld L, Yamani Q, Jacob G. Case report: gastroduodenal intussusception of a gastrointestinal stromal tumour. Br J Radiol. 2002;75:987–989. doi: 10.1259/bjr.75.900.750987. [DOI] [PubMed] [Google Scholar]
- 7.Lin F, Setya V, Signor W. Gastroduodenal intussusception secondary to a gastric lipoma: a case report and review of the literature. Am Surg. 1992;58:772–774. [PubMed] [Google Scholar]
- 8.Atmatzidis S, Chatzimavroudis G, Dragoumis D, Tsiaousis P, Patsas A, Atmatzidis K. Gastric schwannoma: a case report and literature review. Hippokratia. 2012;16:280–282. [PMC free article] [PubMed] [Google Scholar]
- 9.Daimaru Y, Kido H, Hashimoto H, Enjoji M. Benign schwannoma of the gastrointestinal tract: a clinicopathologic and immunohistochemical study. Hum Pathol. 1988;19:257–264. doi: 10.1016/s0046-8177(88)80518-5. [DOI] [PubMed] [Google Scholar]
- 10.Miettinen M, Lasota J. Gastrointestinal stromal tumors--definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch. 2001;438:1–12. doi: 10.1007/s004280000338. [DOI] [PubMed] [Google Scholar]
- 11.Williamson JM, Wadley MS, Shepherd NA, Dwerryhouse S. Gastric schwannoma: a benign tumour often mistaken clinically, radiologically and histopathologically for a gastrointestinal stromal tumour--a case series. Ann R Coll Surg Engl. 2012;94:245–249. doi: 10.1308/003588412X13171221590935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bandoh T, Isoyama T, Toyoshima H. Submucosal tumors of the stomach: a study of 100 operative cases. Surgery. 1993;113:498–506. [PubMed] [Google Scholar]


