Abstract
Processes to ensure world-wide best-practice for critical care delivery are likely to minimize preventable death, disability and costly complications for any healthcare system’s sickest patients, but no large-scale efforts have so far been undertaken towards these goals. The advances in medical informatics and human factors engineering have provided possibility for novel and user-friendly clinical decision support tools that can be applied in a complex and busy hospital setting. To facilitate timely and accurate best-practice delivery in critically ill patients international group of intensive care unit (ICU) physicians and researchers developed a simple decision support tool: Checklist for Early Recognition and Treatment of Acute Illness (CERTAIN). The tool has been refined and tested in high fidelity simulated clinical environment and has been shown to improve performance of clinical providers faced with simulated emergencies. The aim of this international educational intervention is to implement CERTAIN into clinical practice in hospital settings with variable resources (included those in low income countries) and evaluate the impact of the tool on the care processes and patient outcomes. To accomplish our aims, CERTAIN will be uniformly available on either mobile or fixed computing devices (as well as a backup paper version) and applied in a standardized manner in the ICUs of diverse hospitals. To ensure the effectiveness of the proposed intervention, access to CERTAIN is coupled with structured training of bedside ICU providers.
Keywords: Decision support systems, Critical care, Education, Checklists, Medical informatics
Core tip: Important barriers including limited access to educational resources, geographical distance, cost and lack of efficient global infrastructure greatly limit the feasibility of on site educational interventions. To overcome these barriers the international group of intensive care unit (ICU) physicians and researchers developed a simple decision support tool: Checklist for Early Recognition and Treatment of Acute Illness (CERTAIN). CERTAIN is a systematic approach to error prevention with the use of checklists and electronic decision support algorithms. The effectiveness of CERTAIN to improve outcomes and reduce costs will be tested in a stepped wedge cluster before-after trial in ICUs with variable resources across five continents.
INTRODUCTION
Incomplete knowledge of best practices by front-line health care providers and delayed, error-prone delivery processes can offset the potential benefits of critical care support. This is particularly important early in the course of critical illness, when errors and delays in appropriate care often lead to costly complications and poor outcomes, even in advanced hospitals[1,2]. Three major barriers prevent adequate delivery of care for critically ill patients: (1) provider (rather than patient)-oriented care delivery; (2) lack of access to standardized decision support; and (3) lack of an efficient global infrastructure. To overcome these barriers there is a need for standardized approach to evaluation and treatment of critically ill patients[3,4]. The systematic approach to error prevention with the use of checklists has been proposed to improve patient safety in surgical settings and in intensive care units (ICUs) in developed countries with encouraging results[5-9]. The expected benefit from a checklist approach to quality improvement process in various hospital settings including low-and middle-income countries is likely to be high. Indeed, the impact of surgical safety checklist was even more pronounced in the low-income country hospitals[5,10]. Our recent survey on critical care practices in resource limited settings showed that majority of these ICUs do not use any kind of checklist for acute resuscitation or rounding[11]. To address the third barrier, there is a need to establish an efficient interdisciplinary collaboration and robust infrastructure.
The advances in medical informatics and human factors engineering have provided possibility for novel and user friendly clinical decision support (CDS) tools that can be applied in a complex and busy hospital setting[12-14]. To facilitate timely and improved best-practice delivery and a reduction in preventable death and complications in critically ill patients compared to current practice international group of ICU physician and researchers developed a simple electronic decision support tool: Checklist for Early Recognition and Treatment of Acute Illness (CERTAIN)[15,16]. The central hypothesis is that health care provider access and training in CERTAIN will facilitate timely and accurate best-practice delivery and improve outcomes of critically ill patients.
OVERVIEW OF STUDY DESIGN
The Primary Objectives of the CERTAIN Study are: (1) to iteratively refine electronic decision support tool (CERTAIN); and (2) to implement CERTAIN into clinical practice in variable hospital settings and evaluate the impact of the tool on the care processes and patient outcomes.
The Secondary objective is to implement CERTAIN into educational settings as an interactive electronic educational tool.
The key outcomes of interest are related to better care, and better health at a lower cost (see below).
To ensure the effectiveness of the proposed intervention, access to the easy to use electronic checklist/decision support (CERTAIN) will be coupled with structured training of bedside ICU providers. CERTAIN will be uniformly available on either mobile or fixed computing devices (as well as a backup paper version). The proposed project consists of two phases.
PHASE 1 (TOOL REFINEMENT)
Description of the novel technology
CERTAIN is a web-based decision support tool displaying relevant clinical information incorporated with the knowledge about evidence-based best clinical practices, which are organized according to a systematic review of end user data needs and ergonomic workflow[17].
CERTAIN is a web based application suite hosting in a secured Platform as a Service (PaaS) environment with on-demanding scalability up to multiple Linux servers. Current main version graphical user interface (GUI) is developed by using Adobe ActionScript 3 which could be viewed through any web browser including flash player either from regular computer (desktop/laptop) or from mobile devices (tablet pc, smartphone). A mobile app version which is developed by HTML5 is also provided as a complementary part to extend CERTAIN availability and better user experience on the mobile device. A backup paper version is available in a case of problems with internet connection.
CERTAIN modules
CERTAIN consists of two modules, stabilization (admission/resuscitation) module [CERTAIN evaluation of life threatening emergencies (ELITE)] and rounding module (CERTAIN Rounds), to help the clinicians with the routine recommended care processes which need to be assessed daily for every patient.
Stabilization (Admission/resuscitation) module
CERTAIN-ELITE (Figure 1) is designed as an electronic choreography for evaluation of life-threatening emergencies with embedded timer, checklist and decision support cards to facilitate error-free care of acutely deteriorating patient (ICU admission and subsequent emergencies).
Figure 1.
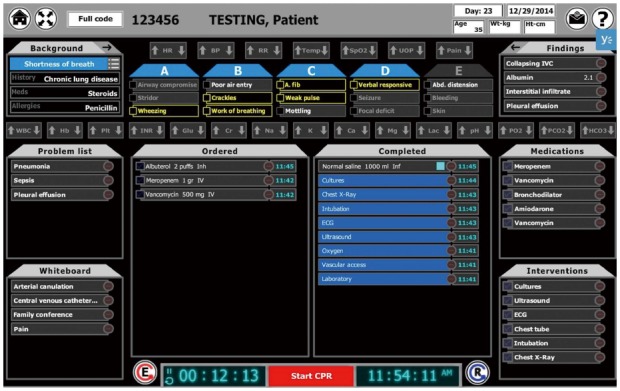
CERTAIN-ELITE (Evaluation of Life Threatening Emergencies) admission/resuscitation module. CERTAIN: Checklist for Early Recognition and Treatment of Acute Illness; ELITE: Evaluation of life threatening emergencies.
In CERTAIN data elements are organized by considering how experts incorporate information into decision making mental models. Reading from up to bottom organizational elements are (1) primary (ABCDE) survey; and (2) secondary patient survey, and from left to right the key organizational elements are: (1) clinical context -reason for admission/patient problem list; (2) provider actions tracked in the status central panel; and (3) proposed medications and interventions.
Optimization (Rounding) module
CERTAIN Rounding module (Figure 2) is designed as a simple and efficient ICU rounding tool with embedded checklist and decision support cards to facilitate error-free day-to-day care in the ICU.
Figure 2.
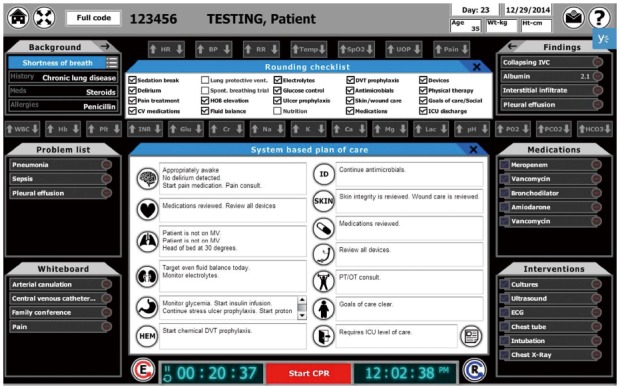
Rounding module with system based plan of care and rounding checklists.
The key characteristics of CERTAIN are: (1) task specific, concept-oriented views of patient data -CERTAIN serves to organize appropriate data determined by a systematic review of end user data needs; (2) knowledge translation - evidence based checklists are incorporated; (3) collaborative workspace - real time plan of care with patient specific tasks, status checks and reminders which provide a location to communicate clearly the goals of care and their status to all members of the multidisciplinary team; (4) reports - scheduled and on demand unit/hospital level reports of quality metrics can be designed for local reporting; and (5) user interface - providers will interact with the system through secure fixed and mobile computer interfaces.
Supporting evidence base
Components of the evidence-informed ICU care practices incorporated in CERTAIN decision support cards are informed by a systematic, comprehensive search for published guidelines, clinical trials and cohort studies in multiple databases such as Medline, EMBASE, National Guideline Clearing House, and Cochrane Library. The guidelines and clinical studies are critically appraised to identify practices with the best evidence.
Utility of CERTAIN has been evaluated in high fidelity clinical simulation setting and has been shown to improve performance of clinical providers faced with simulated emergencies. Among 18 providers there was 14% absolute reduction in omissions of critical tasks with CERTAIN. Most providers (72%) felt better prepared during an emergency scenario when using the CERTAIN model[18].
Following initial development and alpha testing at Mayo Clinic simulation center the tool has been further refined by: (1) web-based survey of decision support needs in an international convenience sample of critical care practitioners from various backgrounds and settings. By directly requesting acute care providers to rank the importance of guidelines and information detailed in literature (from high to low priority), we defined and developed a card template. The detailed description of the development of card template can be found elsewhere[19]; and (2) a decision support card was made for each clinical problem, medication or intervention and was then validated through a modified Delphi process by multidisciplinary, international European Society of Critical Care Medicine/American Thoracic Society/The United States Critical Illness and Injury Trials Group (ESICM/ATS/USCIITG) (ESICM/ATS/USCIITG) expert panel. Once the card was validated, each card is assigned expiration date for ensuring up to date medical knowledge.
PHASE 2 IMPLEMENTATION OF CERTAIN
Participant recruitment and enrollment
Settings: Following IRB approval the effectiveness of CERTAIN to improve outcomes and reduce costs will be tested in a stepped wedge cluster before-after trial of a total of 25-40 ICUs in hospitals with variable resources from five continents (Asia, Africa, Europe, America, Australia) (Figure 3). Total of 12000-15000 patients will be included in the study (Figure 4).
Figure 3.
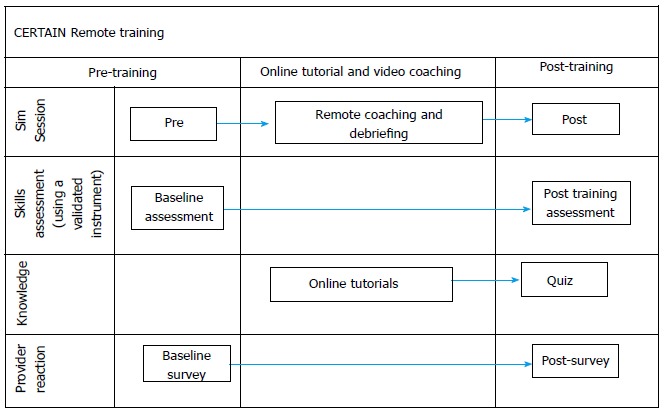
CERTAIN remote simulation training flow. CERTAIN: Checklist for Early Recognition and Treatment of Acute Illness.
Figure 4.
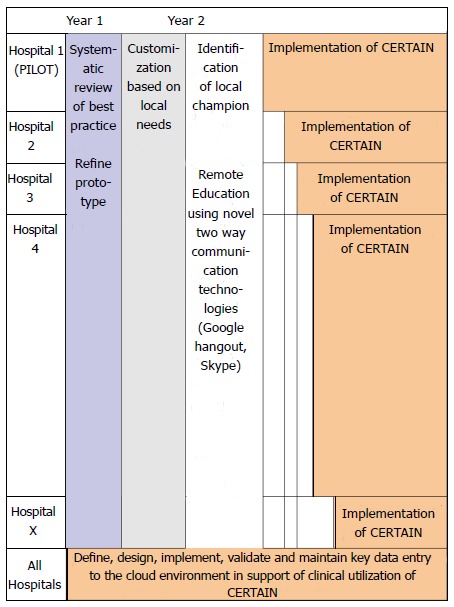
Overview of the proposed intervention. CERTAIN: Checklist for Early Recognition and Treatment of Acute Illness.
Study subjects: All adult (≥ 18 years) patients admitted for the first time to the participating ICUs will be included.
Not critically Ill, admitted for low risk monitoring, planned ICU admissions for routine postoperative surveillance for less than 24 h after uncomplicated surgery, readmission and transferred from outside ICU.
Data collection for outcome assessment: The pre-implementation phase consists of 3 mo full dataset, prospectively and 9 previous months of minimal outcome data, retrospectively baseline data collection (up to 250 patients per ICU). Data collection will include epidemiological data and daily assessment of processes of care, organ function and support. Length of ICU and hospital stay and outcome will be collected. The site research coordinators are instructed in the study protocol, outcome measures, and data collection process as soon as IRB approval is obtained.
Following pre-implementation phase and prior to the clinical implementation and testing, local champions resuscitation skills will be evaluated by remote online video simulation assessment (in a simulated acute care environment of all participating centers) (Figure 3). Each center has a baseline assesment with three physicians (Implementation team) who are given three admission and one rounding scenarios. Following baseline session, the participating centers will be given access to online CERTAIN tool and training materials. After 2-4 wk a follow up training session is performed during which we will test competency of the participants to use the CERTAIN tool. Again, the physicians are given 3 admission and one rounding scenario similar to the baseline session, but this time the physicians will use CERTAIN during all scenarios. These practice scenarios will be followed with remote debriefing to provide structured feedback to enhance learning experience. Following successful second skill assessment, the Implementation team will be certified and use the similar simulation procedure on site to train local staff with local languages. Once local physicians and nurses complete the training program the participating center will have a permission to proceed to clinical implementation and testing.
Bedside ICU providers (physicians and nurses) will be given access to and training in CERTAIN starting with the single ICU bed in a PILOT ICU with subsequent expansion to the whole unit followed by the step-wedge implementation in a similar manner across international ICUs. The participating site clinicians will be trained in the use of CERTAIN by the local Implementation teams. During the process, adoption feedback and suggestion will be collected by design team and make necessary customization for local hospitals. The local implementation experience will also be shared with whole CERTAIN investigators to facilitate subsequent implementation efforts in other centers.
Data collection on outcomes measures and compliance with each element of best practices will be done daily during the control period by trained research coordinators. It consists of 6 mo full dataset, and 6 more months of minimal outcome data; up to 250 patients per ICU. After implementation of CERTAIN during the post-intervention period, enrollment tracking, data cleaning, outcome assignment, outcome validation, and outcome tracking will be performed electronically. The site research coordinators will be trained in the study protocol, outcome measures, and data collection process via webinars conducted by the Outcomes group.
OUTCOME ASSESSMENT
We will track relevant outcomes to demonstrate better care, better health and lower costs in the objectives as outlined below: (1) with regards to better care: we expect to see an improvement in the processes of care, safety culture and patient and family satisfaction. Specifically we will measure: Compliance with timely and adequate antimicrobial therapy; Compliance with ventilator bundle (DVT prophylaxis, GI prophylaxis, sedation holidays, assessment of readiness to extubate); Compliance with lung-protective mechanical ventilation; Conservative blood product usage; (2) better health: we will examine the health outcomes of patients in a number of ways. Measures include: ICU, hospital and 28 d mortality, and discharge disposition (home vs other institution); and (3) lower costs - Resource utilization: ICU and hospital length of stay.
CONFIDENTIALITY OF SUBJECTS’ DATA AND DATA SECURITY
All the cloud servers and database services used in CERTAIN project are secured by adopting Server Name Indication (SNI) based Secure Sockets Layer (SSL) protocol. Every request to the server required to be authenticated by our SSL certificate. The data stored in the Database are encrypted based on security requirements and every hospital has its own separated logical space. Data backup is also planned and implemented by setting up scheduled jobs in the server side.
Each study subject will be assigned a unique study identification number linked to his or her medical record number at the respective home site. We will use existing procedures to ensure that individual patient identifiers are kept separate from analysis files and are available only to project personnel on a need-to-know basis. All identified patient data necessary to complete this research will be created and stored in secure computers to which only project team members will have access. Only project personnel directly involved in the study will have access to identified patient data and medical charts at their respective site. All project personnel with access to patient data will be trained in the proper handling of such data.
LIMITATIONS
Restricted availability of some medications and equipment in resource-limited settings may preclude delivery of best care practices and limit generalizibility of the study results. Nevertheless, we expect to see improvement in all proposed outcomes with the implementation of the CERTAIN tool. We overcame possible lack of internet access by providing paper version of the tool.
CONCLUSION
CERTAIN initiative directly addresses the major barriers to the consistent and timely delivery of error-free, evidence-informed clinical care to critically ill patients by: (1) organizing clinical information into vital components specific to the patient’s condition and task at hand; (2) incorporating centralized CDS tools informed by evidence-based guidelines that are both patient and context appropriate to ensure that interventions are implemented at the right time for the right patients for the right conditions; (3) coupling the intervention with an interactive educational initiative to decrease the gap between knowledge and translation to clinical practice; and (4) providing centralized, timely and regular compliance and quality metrics feedback and auditing to empower institutions to implement and enact change. By providing ready solutions for major barriers - lack of collaboration, early recognition, prompting and support tools - we propose to be able to increase access to critical care knowledge at the point of care thereby minimizing diagnostic error, therapeutic harm and resulting preventable death, disability and cost.
Footnotes
Conflict-of-interest: This research has been reviewed by the Mayo Clinic Conflict of Interest Review Board and is being conducted in compliance with Mayo Clinic conflict of interest policies. Mayo Clinic and Dr Gajic hold intellectual property rights and financial conflict of interest in critical care related software tools.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: August 24, 2014
First decision: November 27, 2014
Article in press: January 20, 2015
P- Reviewer: John J, Yao YM S- Editor: Tian YL L- Editor: A E- Editor: Wu HL
References
- 1.Moreno RP, Rhodes A, Donchin Y. Patient safety in intensive care medicine: the Declaration of Vienna. Intensive Care Med. 2009;35:1667–1672. doi: 10.1007/s00134-009-1621-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bracco D, Favre JB, Bissonnette B, Wasserfallen JB, Revelly JP, Ravussin P, Chioléro R. Human errors in a multidisciplinary intensive care unit: a 1-year prospective study. Intensive Care Med. 2001;27:137–145. doi: 10.1007/s001340000751. [DOI] [PubMed] [Google Scholar]
- 3.Pronovost PJ, Berenholtz SM, Ngo K, McDowell M, Holzmueller C, Haraden C, Resar R, Rainey T, Nolan T, Dorman T. Developing and pilot testing quality indicators in the intensive care unit. J Crit Care. 2003;18:145–155. doi: 10.1016/j.jcrc.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Ilan R, Fowler RA, Geerts R, Pinto R, Sibbald WJ, Martin CM. Knowledge translation in critical care: factors associated with prescription of commonly recommended best practices for critically ill patients. Crit Care Med. 2007;35:1696–1702. doi: 10.1097/01.CCM.0000269041.05527.80. [DOI] [PubMed] [Google Scholar]
- 5.Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, Herbosa T, Joseph S, Kibatala PL, Lapitan MC, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–499. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 6.Arriaga AF, Bader AM, Wong JM, Lipsitz SR, Berry WR, Ziewacz JE, Hepner DL, Boorman DJ, Pozner CN, Smink DS, et al. Simulation-based trial of surgical-crisis checklists. N Engl J Med. 2013;368:246–253. doi: 10.1056/NEJMsa1204720. [DOI] [PubMed] [Google Scholar]
- 7.de Vries EN, Dijkstra L, Smorenburg SM, Meijer RP, Boermeester MA. The SURgical PAtient Safety System (SURPASS) checklist optimizes timing of antibiotic prophylaxis. Patient Saf Surg. 2010;4:6. doi: 10.1186/1754-9493-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gawande A. The checklist manifesto: how to get things right. 1st ed. New York: Metropolitan Books; 2010. [Google Scholar]
- 9.Treadwell JR, Lucas S, Tsou AY. Surgical checklists: a systematic review of impacts and implementation. BMJ Qual Saf. 2014;23:299–318. doi: 10.1136/bmjqs-2012-001797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kwok AC, Funk LM, Baltaga R, Lipsitz SR, Merry AF, Dziekan G, Ciobanu G, Berry WR, Gawande AA. Implementation of the World Health Organization surgical safety checklist, including introduction of pulse oximetry, in a resource-limited setting. Ann Surg. 2013;257:633–639. doi: 10.1097/SLA.0b013e3182777fa4. [DOI] [PubMed] [Google Scholar]
- 11.Vukoja M, Riviello E, Gavrilovic S, Adhikari NKJ, Kashyap R, Bhagwanjee S, Gajic O, Kilickaya O. A Survey on Critical Care Resources and Practices in Low- and Middle-Income Countries. Global Heart. 2014;9:337–342.e5. doi: 10.1016/j.gheart.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Herasevich V, Pickering BW, Dong Y, Peters SG, Gajic O. Informatics infrastructure for syndrome surveillance, decision support, reporting, and modeling of critical illness. Mayo Clin Proc. 2010;85:247–254. doi: 10.4065/mcp.2009.0479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pickering BW, Herasevich V, Ahmed A, Gajic O. Novel Representation of Clinical Information in the ICU: Developing User Interfaces which Reduce Information Overload. Appl Clin Inform. 2010;1:116–131. doi: 10.4338/ACI-2009-12-CR-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pickering BW, Litell JM, Herasevich V, Gajic O. Clinical review: the hospital of the future - building intelligent environments to facilitate safe and effective acute care delivery. Crit Care. 2012;16:220. doi: 10.1186/cc11142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CERTAIN -Checklist for Early Recognition and Treatment of Acute Illness. Cited 2014. Available from: http://www.icertain.org/
- 16.Baker T. The Certain Project (2013) European Society of Critical Care Medicine (ESICM). Cited 2013-12. Available from: http://www.esicm.org/upload/530c4acfcfa7c-escim-globalintensivecareworkinggroup-projects-022014.pdf.
- 17.Pickering BW, Gajic O, Ahmed A, Herasevich V, Keegan MT. Data utilization for medical decision making at the time of patient admission to ICU. Crit Care Med. 2013;41:1502–1510. doi: 10.1097/CCM.0b013e318287f0c0. [DOI] [PubMed] [Google Scholar]
- 18.Sevilla-Berrios R, O’Horo J, Schmickl C, Erdogan A, Chen X, Garcia Arguello L, Dong Y, Gajic O. Prompting with Electronic Checklist Improves Clinician Performance in Medical Emergencies: High Fidelity Simulation Study. Critical Care Medicine. 2014;42:A1424. doi: 10.1186/s12245-018-0185-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonneton BA, Adhikari N, Schultz M, Kilickaya O, Senkal S, Gavrilovic Srdjan, Kashyap R, Pickering B. Development of bedside descision support cards based on the information needs of acute care providers. Critical Care Medicine. 2013;41:A30–A31. [Google Scholar]


