Abstract
Objective:
Emergence agitation (EA), a short-lived, self-limiting phenomenon, arises frequently after the use of inhalational agents and hampers the implementation of pediatric ambulatory surgery in spite of using so many drugs with variable efficacy.
Methods:
In this prospective, double-blinded, parallel group study (2008–2009), 80 children of both sex aged 3–7 years, with American Society of Anesthesiologists (ASA) physical status grade I-II, undergoing sevoflurane-based general anesthesia for elective day care surgery were randomly assigned into groups C or D. Group C received 4 μg/kg intranasal clonidine, whereas group D received 1 μg/kg intranasal dexmedetomidine, 45 min before induction of anesthesia. In postanesthesia care unit (PACU), the incidence of EA was assessed with Aonos four-point scale and the severity of EA was assessed with pediatric anesthesia emergence delirium scale upon admission (T0), after 5 min (T5), 15 min (T15), and 25 min (T25). Extubation time, emergence time, duration of PACU stay, dose and incidence of fentanyl use for pain control were noted.
Findings:
Based on comparable demographic profiles, the incidence and severity of EA were significantly lower in group D as compared to group C at T0, T5, T15, and T25. But time of regular breathing, awakening, extubation, and emergence were significantly delayed in group D than C. The number and dose of fentanyl used in group C were significantly higher than group D. PACU and hospital stay were quite comparable between groups.
Conclusion:
Intranasal dexmedetomidine 1 μg/kg was more effective than clonidine 4 μg/kg in decreasing the incidence and severity of EA, when administered 45 min before the induction of anesthesia with sevoflurane for pediatric day care surgery. Dexmedetomidine also significantly reduced fentanyl consumption in PACU.
Keywords: Clonidine, Dexmedetomidine, emergence agitation, postanesthesia care unit
INTRODUCTION
Emergence agitation (EA), also called as emergence delirium (ED) during recovery from inhalational agent based general anesthesia has been identified as a frequent problem in the pediatric population. In children, EA has been described as a mental disturbance that consists of confusion, hallucinations, and delusions manifested by inconsolable crying, disorientation, nonpurposeful restlessness, involuntary physical activity, and thrashing about in bed.[1] Among all inhalational anesthetics, sevoflurane is considered an agent of choice for induction and maintenance of day care anesthesia in children and enjoys wide acceptance among pediatric anesthesiologists.[2] The occurrence of EA in children after sevoflurane anesthesia is common, with an incidence ranging between 10% and 80%.[3]
Though EA is generally short-lived with no after-effect, it may not only cause injury to the child or bleeding from the surgical site, but also lead to the accidental removal of the surgical dressings, IV access, and drains. EA also leads to dissatisfaction and anxiety for the parents about the quality of child's recovery and requires extra nursing care with associated enhanced costs.[1,4] Supplemental sedative and/or analgesic medications may often be necessary to control the symptoms leading to delayed discharge from postanesthesia care unit (PACU). Parents who witness EA in their child may worry about a permanent sequel.[5]
Various pre-, intra-, and immediate postoperative pharmacological agents like-analgesics,[6] Dexa- methasone,[7] opioids,[8] propofol,[9] benzo- diazepines,[10] alpha-2 (α2) agonists,[10,11] were used with the aim of reducing the occurrence of EA after sevoflurane-based anesthesia, with variable results.
Alpha-2 agonists have sedative and analgesic properties without significant respiratory depression at clinical dosages. Kulka et al.[12] and Bock et al.[13] in their study with 2 μg/kg and 3 μg/kg clonidine, respectively; reported a decrease in EA and no delay in patient discharge. Again, Ibacache et al.[14] reported that another α2 adrenoreceptor agonist, dexmedetomidine had effectively reduced EA after sevoflurane anesthesia in children. Dexmedetomidine, is a more highly specific α2 adrenoreceptor agonist (α2/α1= 1620/1) than clonidine (α2/α1= 220/1), has significantly reduced EA frequency after sevoflurane anesthesia in pediatric surgery and nonsurgical procedures in inpatient[14,15] and outpatient settings.[16,17]
The aim of this double-blinded randomized prospective parallel group study was to compare the effect of these two α2 agonists (dexmedetomidine and clonidine) when administered intranasally 45 min prior to the induction of sevoflurane-based anesthesia on the incidence and severity of EA as well as emergence and discharge time in children undergoing day care surgery.
METHODS
After obtaining permission from Institutional Ethics Committee, written informed consent was taken from the parents/guardians. Total 80 children of either sex, aged 3-7 years, American Society of Anesthesiologists (ASA) physical status classification system,[18] grade I-II, scheduled for elective day care surgery under general anesthesia with expected operation time duration <60 min were enrolled in this prospective, randomized, double-blinded study.
Exclusion criteria included: Children with a developmental, psychological, and cognitive disorders; active airway disease, cerebral palsy, history of sleep apnea or epileptic fits; patients on chronic or acute intake of any sedative or analgesic medications; inborn errors of metabolism, body weight <10 kg or frank obese; patients with known allergy to any of the medications used for procedures; and children with cardiovascular or neurological abnormality.
All patients underwent thorough preoperative evaluation, which included the history, physical examination and relevant laboratory investigations. During the preoperative visit, each enrolled child was asked to choose a sealed envelope with his code number inside. The name, admission registration number, and body weight were recorded on the sealed envelope after been chosen.
The patients were randomly assigned to two equal groups to receive either 4 μg/kg intranasal clonidine (group C) or 1 μg/kg intranasal dexmedetomidine (group D) as premedication, via computer-generated random numbers which matched with the sealed envelope. Prior to arrival of the child, a resident doctor in anesthesiology who did not participate in clinical assessment, drew up the study drug (either clonidine or dexmedetomidine) into a tuberculin syringe that was labeled study drug. To ensure blinding, the volume of the study medication was standardized at 0.04 ml/kg. Intranasal dexmedetomidine and clonidine were prepared from the parenteral preparation (100 μg/ml and 150 μg/ml, respectively). The drugs were administered 45 min prior to induction of anesthesia.
The intranasal premedication was administered by on-duty resident doctor not knowing the composition of the prefilled syringe. On premedicating and shifting the child to preoperative room, hemodynamic parameters (heart rate, blood pressure, and oxygen saturation [SpO2]) were studied continuously. If the fall in (SpO2 < 90%) detected, then O2 were delivered by oxygen mask.
About 45 min after premedication, children were brought to the operating room where anesthesia was induced with sevoflurane in 100% oxygen (6 L/min) through a face mask.
At the end of surgery, once hemostasis was achieved, the anesthetic agents were discontinued and replaced with O2100% (6 L/min).
Time to regular breathing is the time period from discontinuation of anesthesia to time of deep, regular breathing. Time to awakening is the time period from discontinuation of anesthesia to time of initial arousal (eye opening, child showing purposeful movements). From discontinuation of anesthesia to tracheal extubation was defined as the time to extubation. First response to command or eye opening on command after extubation was the emergence time.
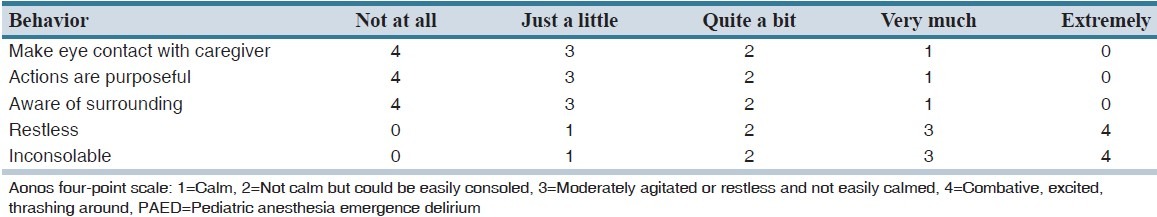
In the PACU, the incidence of EA was assessed with Aonos four-point scale and the severity of EA was assessed with pediatric anesthesia ED (PAED) scale [Table 1] upon admission and 5,15 and 25 min (T0, T5, T15, T25), respectively. One parent who was very close to the child was allowed to be with the child at PACU. Twenty-five minutes after entry into PACU, the agitated children were managed by giving intravenous increments of fentanyl 1 μg/kg with at least a 10 min time interval between each dose, during which time the children were monitored for any signs of respiratory depression. Resident anesthesiologists who were observers blinded to study groups recorded all the scores and observations at PACU and operation theater. The time for PACU stay (admission-discharge from PACU) and hospital discharge (eye opening-discharge), and the incidence of adverse events (bradycardia, desaturation (SpO2 < 95%), vomiting, shivering, coughing, breath holding, laryngospasm) were also recorded. Children were considered ready for discharge from the PACU when the modified Aldrete postanesthesia score was ≥9.[19] Patients were transferred to ward after being discharged from PACU. For nausea and vomiting, ondansetron 0.15 mg/kg IV was administered.
Table 1.
PAED scale
This study was powered on the basis of preliminary results showing 50% incidence of ED in the control group. A sample size of 32 in each group was calculated to detect a decrease in the incidence of agitation down to 15% with α = 0.05 and β = 0.2. Continuous data were reported as mean ± standard deviation and were analyzed using an independent sample t-test or analysis of variance for multiple comparisons with least significant difference test for post hoc analysis. Categorical data were reported as percentages and were analyzed using the Chi-square test or Fisher exact test as appropriate. Nonparametric data such as pain scores were reported as median and inter-quartile range and were analyzed using the Mann–Whitney U-test. A P < 0.05 was considered statistically significant.
RESULTS
There were no significant differences (P > 0.05) between the two groups with regard to demographic data such as age, sex, weight, ASA status, duration of surgery and anesthesia. Also, the durations of sevoflurane administration among two groups were similarly comparable [Table 2]. Indications for different day care pediatric surgeries (data not shown) and perioperative hemodynamic parameters [Table 3] among two groups were similar among two groups. Time for regular breathing, awakening, extubation, and emergence were all delayed in patients of dexmedetomidine (D) group when compared with clonidine (C) group and the differences were all statistically significant [Table 4].
Table 2.
Comparison of demographic data between the two study groups (N=40)

Table 3.
Comparison of (pre, intra, post) operative clinical variables between the study groups (N=40)

Table 4.
Comparison of postoperative profile between the study groups (N=40)

Incidences of EA were significantly lower in group D in comparison with group C, up to the first 15 min; although, after then, the difference was both statistically and clinically comparable [Table 5]. Total number of patients suffering from ED after sevoflurane-based general anesthesia was both statistically and clinically significant in clonidine than dexmedetomidine group [Table 5]. Severity of emergence reaction as measured by PAED score was also significantly less in group D at all the time intervals (0, 5, 15, 25 min) while the results were statistically significant throughout the whole PACU stay [Table 5]. In group D, only one patient whereas, in group C, four patients had PAED score >15 and this difference was also statistically significant.
Table 5.
Comparison of emergence agitation between the study groups (N=40)

Frequency of children treated with fentanyl for pain and mean dose of fentanyl consumption were significantly less in group D than group C. Nausea, vomiting, and the use of ondansetron for controlling it were comparable among two groups. Duration of PACU stay and time for hospital discharge were also comparable among two groups [Table 6].
Table 6.
Comparison of PACU management parameters and discharge from hospital (N=40)

DISCUSSION
In pediatric day care surgery, EA still remains a big headache and nuisance for the surgeons and pediatric anesthesiologists as well as an irritating discomfort for the parents accompanying the children. Since 1961, the discontinued or decreased use of ether, cyclopropane, ketamine, scopolamine like older anesthetics and the increased use of short-acting opioids, sedatives, and regional techniques rendered this problem one of mere historical interest. With the introduction of a new, relatively insoluble volatile anesthetics, desflurane and sevoflurane, ED and agitation have reappeared, particularly in children.[20,21]
In pediatric ambulatory surgery, EA is a difficult problem, because EA itself and its treatment using sedative or analgesics may delay discharge and patient's home return. Extended hospital stay discourages both patients and their caregivers from undergoing ambulatory surgery. Therefore, ambulatory pediatric anesthesiologists have been trying to prevent EA in order to provide efficient and high-quality care that is a positive experience for children and their parents.[22]
Among several medications,[6,7,8,9,10,11] tried for prevention of EA after sevoflurane-based anesthesia α2 agonists has shown promising results.
Clonidine is an α2 agonist that have been used for premedication in adult and pediatric patients. Clonidine is effective by the stimulation of pre- and post-synaptic α2 agonists in many areas of the central nervous system leading to sedation, analgesia, and reduction of sympathetic tone.[23] In adult intensive care patients, clonidine is used in the treatment of agitation associated with withdrawal syndromes.[24,25] We, therefore, assumed that clonidine to be a promising drug for the treatment of agitation after sevoflurane anesthesia. We had chosen 4 μg/kg intranasal clonidine as used by Almenrader et al.[26]
Dexmedetomidine is a highly selective α2 adrenoceptor agonist with sedative, analgesic, and anesthetic sparing properties and has been approved by Food and Drug Administration as a short-term sedative for mechanically ventilated intensive care unit (ICU) patients.[27] Dexmedetomidine has recently been used successfully with reduced EA frequency after sevoflurane anesthesia for pediatric surgery in- and outpatient settings.[16,28] Intranasal dose of dexmedetomidine was kept 1 μg/kg as per study by Isik et al.[16]
In this prospective, double-blinded trial we had compared the effect of intranasal premedication; with 4 μg/kg clonidine and 1 μg/kg dexmedetomidine administered 45 min before induction of anesthesia; on incidence, severity of EA, amount of fentanyl consumption, duration of PACU as well as hospital stay.
The indications for operations and demographic profile of patients, which were statistically insignificant between two groups, were quite similar with other research investigations,[29] and provided us the uniform platform to evenly compare the results obtained. The study was conducted by Srivastava et al.[29] on the comparative role of clonidine and dexmedetomidine for short-term sedation in ICU in a total of 70 patients yielded similar results.
In our study, the incidence and severity of EA were significantly lower in group D compared to group C. Di et al.[30] similarly found a single dose dexmedetomidine administered 30 min prior to end of surgery had reduced the incidence of sevoflurane induced EA significantly compared to control group (13.3% vs. 30%). But Ham et al.[31] when compared single dose dexmedetomidine with remifentanil found it did not attenuate EA in intubated adult patients. Again Zhang et al.[32] and Sun et al.[33] found from two different meta-analyses consisting 12 and 15 clinical trials, respectively that the dexmedetomidinehad significantly decreased the incidence of EA in children under sevoflurane anesthesia. Similarly, Heinmiller et al.[34] also found that Clonidine reduced EA after strabismus surgery when compared with placebo.
Time of regular breathing, awakening, extubation, and emergence all were delayed in group D than C, and the difference was both clinically and statistically significant. Di et al.[30] in their study found that the dexmedetomidine did not produce delay in extubation when compared with placebo. Ham et al.[31] found delayed awakening of patients in the dexmedetomidine group undergoing orthognathic surgery. Prolonged extubation time and emergence time was found by dexmedetomidine while doing a meta-analysis by Zhang et al.[32] Again in the study for prevention of sevoflurane induced EA, Malviya et al.[35] found that clonidine produced significant delay in awakening when compared with placebo. Though the awakening, extubation, and emergence were delayed in group D but the delay did not produce any clinical problem.
It is often difficult to distinguish between postoperative pain and EA in younger children as symptoms of both might be similar so that different assessments tools have been used by different investigators to differentiate between the two. Number of patients treated with fentanyl and the mean dose of fentanyl used at PACU was significantly higher in group C than group D both clinically and statistically. These observations were supported by Di et al.[30] who observed that dexmedetomidine significantly reduced fentanyl consumption in the postoperative period after cleft leap and palate repair (56.7% vs. 66.7%) when compared with placebo. Zhang et al.[32] also observed less pain in the dexmedetomidine-treated groups in their meta-analysis study.
In our study, duration of PACU stay and time for hospital discharge were slightly delayed in group D than C but the results were statistically and clinically insignificant. But on the contrary, Di et al.[30] found that dexmedetomidine produced significantly shorter PACU stay than a placebo group. Again in the study by Heinmiller et al.[34] found clonidine-treated group spent insignificantly longer time at PACU than the placebo group. Malviya et al.[35] also found that clonidine produced significantly longer PACU stay when compared with placebo.
Nausea and vomiting were seen in our both study groups, but there was no clinical or statistical difference among two groups. This finding was quite similar with other research investigators.[30,31,32,33,34,35]
One of the limitations of the current study is the absence of a placebo-controlled group. Though it was initially planned, but rejected by the Hospital Ethics Committee as administering no premedication may lead to severe ED and day care anesthesia may not be feasible due to parental anxiety arising from their children's unfamiliar behavior after operations. Second, we had to allow parental presence during recovery at PACU, which was not accordance to our hospital policy. Another limitation is that we compared clonidine and dexmedetomidine based on their known optimal as well as safe doses for day care setting without the knowledge of their equipotent doses.
In conclusion, the intranasal administration of dexmedetomidine (1 μg/kg) prevents incidence and severity of ED more effectively than intranasal clonidine (4 μg/kg) when administered 45 min prior to induction. Dexmedetomidine also reduces fentanyl consumption than clonidine, but PACU as well as a hospital stay were slightly delayed in the dexmedetomidine group without producing any appreciable side effect in children undergoing ambulatory surgery under sevoflurane-based general anesthesia.
AUTHORS' CONTRIBUTION
A. Mukherjee: Planning and study design, A. Das: Manuscript writing and editing, S.R. Basunia: Data collection and analysis, S. Chattopadhyay: Statistical analysis, R. Kundu: Study design, data collection, R. Bhattacharyya: Data collection and reference gathering.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sikich N, Lerman J. Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology. 2004;100:1138–45. doi: 10.1097/00000542-200405000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Tomal CR, Silva AG, Yamashita AM, Andrade PV, Hirano MT, Tardelli MA, et al. Assessment of induction, recovery, agitation upon awakening, and consumption with the use of two brands of sevoflurane for ambulatory anesthesia. Rev Bras Anestesiol. 2012;62:154–72. doi: 10.1016/S0034-7094(12)70115-0. [DOI] [PubMed] [Google Scholar]
- 3.Welborn LG, Hannallah RS, Norden JM, Ruttimann UE, Callan CM. Comparison of emergence and recovery characteristics of sevoflurane, desflurane, and halothane in pediatric ambulatory patients. Anesth Analg. 1996;83:917–20. doi: 10.1097/00000539-199611000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Silva LM, Braz LG, Módolo NS. Emergence agitation in pediatric anesthesia: Current features. J Pediatr (Rio J) 2008;84:107–13. doi: 10.2223/JPED.1763. [DOI] [PubMed] [Google Scholar]
- 5.Veyckemans F. Excitation phenomena during sevoflurane anaesthesia in children. Curr Opin Anaesthesiol. 2001;14:339–43. doi: 10.1097/00001503-200106000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Kim D, Doo AR, Lim H, Son JS, Lee JR, Han YJ, et al. Effect of ketorolac on the prevention of emergence agitation in children after sevoflurane anesthesia. Korean J Anesthesiol. 2013;64:240–5. doi: 10.4097/kjae.2013.64.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sajedi P, Baghery K, Hagibabie E, Mehr AM. Prophylactic use of oral acetaminophen or IV dexamethasone and combination of them on prevention emergence agitation in pediatric after adenotonsillectomy. Int J Prev Med. 2014;5:721–7. [PMC free article] [PubMed] [Google Scholar]
- 8.Inomata S, Maeda T, Shimizu T, Satsumae T, Tanaka M. Effects of fentanyl infusion on tracheal intubation and emergence agitation in preschool children anaesthetized with sevoflurane. Br J Anaesth. 2010;105:361–7. doi: 10.1093/bja/aeq168. [DOI] [PubMed] [Google Scholar]
- 9.Lee JR, Kim MS, Moon BE, Kim H. Comparison of propofol and fentanyl for preventing emergence agitation in children. Br J Anaesth. 2013;111:121–2. doi: 10.1093/bja/aet182. [DOI] [PubMed] [Google Scholar]
- 10.Tazeroualti N, De Groote F, De Hert S, De Villé A, Dierick A, Van der Linden P. Oral clonidine vs midazolam in the prevention of sevoflurane-induced agitation in children. A prospective, randomized, controlled trial. Br J Anaesth. 2007;98:667–71. doi: 10.1093/bja/aem071. [DOI] [PubMed] [Google Scholar]
- 11.Ali MA, Abdellatif AA. Prevention of sevoflurane related emergence agitation in children undergoing adenotonsillectomy: A comparison of dexmedetomidine and propofol. Saudi J Anaesth. 2013;7:296–300. doi: 10.4103/1658-354X.115363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kulka PJ, Bressem M, Tryba M. Clonidine prevents sevoflurane-induced agitation in children. Anesth Analg. 2001;93:335–8. [PubMed] [Google Scholar]
- 13.Bock M, Kunz P, Schreckenberger R, Graf BM, Martin E, Motsch J. Comparison of caudal and intravenous clonidine in the prevention of agitation after sevoflurane in children. Br J Anaesth. 2002;88:790–6. doi: 10.1093/bja/88.6.790. [DOI] [PubMed] [Google Scholar]
- 14.Ibacache ME, Muñoz HR, Brandes V, Morales AL. Single-dose dexmedetomidine reduces agitation after sevoflurane anesthesia in children. Anesth Analg. 2004;98:60–3. doi: 10.1213/01.ANE.0000094947.20838.8E. [DOI] [PubMed] [Google Scholar]
- 15.Guler G, Akin A, Tosun Z, Ors S, Esmaoglu A, Boyaci A. Single-dose dexmedetomidine reduces agitation and provides smooth extubation after pediatric adenotonsillectomy. Paediatr Anaesth. 2005;15:762–6. doi: 10.1111/j.1460-9592.2004.01541.x. [DOI] [PubMed] [Google Scholar]
- 16.Isik B, Arslan M, Tunga AD, Kurtipek O. Dexmedetomidine decreases emergence agitation in pediatric patients after sevoflurane anesthesia without surgery. Paediatr Anaesth. 2006;16:748–53. doi: 10.1111/j.1460-9592.2006.01845.x. [DOI] [PubMed] [Google Scholar]
- 17.Shukry M, Clyde MC, Kalarickal PL, Ramadhyani U. Does dexmedetomidine prevent emergence delirium in children after sevoflurane-based general anesthesia? Paediatr Anaesth. 2005;15:1098–104. doi: 10.1111/j.1460-9592.2005.01660.x. [DOI] [PubMed] [Google Scholar]
- 18.Saklad M. Grading of patients for surgical procedures. Anesthesiology. 1941;2:281–4. [Google Scholar]
- 19.Aldrete JA. The post-anesthesia recovery score revisited. J Clin Anesth. 1995;7:89–91. doi: 10.1016/0952-8180(94)00001-k. [DOI] [PubMed] [Google Scholar]
- 20.Davis PJ, Cohen IT, McGowan FX, Jr, Latta K. Recovery characteristics of desflurane versus halothane for maintenance of anesthesia in pediatric ambulatory patients. Anesthesiology. 1994;80:298–302. doi: 10.1097/00000542-199402000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Aono J, Ueda W, Mamiya K, Takimoto E, Manabe M. Greater incidence of delirium during recovery from sevoflurane anesthesia in preschool boys. Anesthesiology. 1997;87:1298–300. doi: 10.1097/00000542-199712000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Dahmani S, Stany I, Brasher C, Lejeune C, Bruneau B, Wood C, et al. Pharmacological prevention of sevoflurane- and desflurane-related emergence agitation in children: A meta-analysis of published studies. Br J Anaesth. 2010;104:216–23. doi: 10.1093/bja/aep376. [DOI] [PubMed] [Google Scholar]
- 23.Maze M, Tranquilli W. Alpha-2 adrenoceptor agonists: Defining the role in clinical anesthesia. Anesthesiology. 1991;74:581–605. [PubMed] [Google Scholar]
- 24.Verner L, Hartmann M, Seitz W. Clonidine supplemented analgesia and sedation in prevention of postoperative delirium. Anasth Intensivther Notfallmed. 1990;25:274–80. [PubMed] [Google Scholar]
- 25.Ip Yam PC, Forbes A, Kox WJ. Clonidine in the treatment of alcohol withdrawal in the intensive care unit. Br J Anaesth. 1992;68:106–8. doi: 10.1093/bja/68.1.106. [DOI] [PubMed] [Google Scholar]
- 26.Almenrader N, Passariello M, Coccetti B, Haiberger R, Pietropaoli P. Steal-induction after clonidine premedication: A comparison of the oral and nasal route. Paediatr Anaesth. 2007;17:230–4. doi: 10.1111/j.1460-9592.2006.02080.x. [DOI] [PubMed] [Google Scholar]
- 27.Huang R, Hertz L. Receptor subtype and dose dependence of dexmedetomidine-induced accumulation of [14C] glutamine in astrocytes suggests glial involvement in its hypnotic-sedative and anesthetic-sparing effects. Brain Res. 2000;873:297–301. doi: 10.1016/s0006-8993(00)02525-7. [DOI] [PubMed] [Google Scholar]
- 28.Yuen VM, Irwin MG, Hui TW, Yuen MK, Lee LH. A double-blind, crossover assessment of the sedative and analgesic effects of intranasal dexmedetomidine. Anesth Analg. 2007;105:374–80. doi: 10.1213/01.ane.0000269488.06546.7c. [DOI] [PubMed] [Google Scholar]
- 29.Srivastava U, Sarkar ME, Kumar A, Gupta A, Agarwal A, Singh TK, et al. Comparison of clonidine and dexmedetomidine for short-term sedation of intensive care unit patients. Indian J Crit Care Med. 2014;18:431–6. doi: 10.4103/0972-5229.136071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Di M, Huang C, Chen F, Zeng R, Yu C, Shangguan W, et al. Effect of single-dose dexmedetomidine on recovery profiles after sevoflurane anesthesia with spontaneous respiration in pediatric patients undergoing cleft lip and palate repair. Zhonghua Yi Xue Za Zhi. 2014;94:1466–9. [PubMed] [Google Scholar]
- 31.Ham SY, Kim JE, Park C, Shin MJ, Shim YH. Dexmedetomidine does not reduce emergence agitation in adults following orthognathic surgery. Acta Anaesthesiol Scand. 2014;58:955–60. doi: 10.1111/aas.12379. [DOI] [PubMed] [Google Scholar]
- 32.Zhang C, Hu J, Liu X, Yan J. Effects of intravenous dexmedetomidine on emergence agitation in children under sevoflurane anesthesia: A meta-analysis of randomized controlled trials. PLoS One. 2014;9:e99718. doi: 10.1371/journal.pone.0099718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sun L, Guo R, Sun L. Dexmedetomidine for preventing sevoflurane-related emergence agitation in children: A meta-analysis of randomized controlled trials. Acta Anaesthesiol Scand. 2014;58:642–50. doi: 10.1111/aas.12292. [DOI] [PubMed] [Google Scholar]
- 34.Heinmiller LJ, Nelson LB, Goldberg MB, Thode AR. Clonidine premedication versus placebo: Effects on postoperative agitation and recovery time in children undergoing strabismus surgery. J Pediatr Ophthalmol Strabismus. 2013;50:150–4. doi: 10.3928/01913913-20130205-02. [DOI] [PubMed] [Google Scholar]
- 35.Malviya S, Voepel-Lewis T, Ramamurthi RJ, Burke C, Tait AR. Clonidine for the prevention of emergence agitation in young children: Efficacy and recovery profile. Paediatr Anaesth. 2006;16:554–9. doi: 10.1111/j.1460-9592.2006.01818.x. [DOI] [PubMed] [Google Scholar]


