Abstract
Objective:
The aim of this study was to assess the knowledge, attitude and practice of B.Sc. Pharmacy students about usage and resistance of antibiotics in Trinidad and Tobago.
Methods:
This was a cross-sectional questionnaire-based study involving B.Sc. Pharmacy students. The questionnaire was divided into five components including Demographics data, knowledge about antibiotic use, attitude toward antibiotic use and resistance, self-antibiotic usage and possible causes of antibiotic resistance. Data were analyzed by employing Mann–Whitney and Chi-square tests using SPSS version 20.
Findings:
The response rate was 83.07%. The results showed good knowledge of antibiotic use among students. The overall attitude of pharmacy students was poor. About 75% of participants rarely use antibiotics, whereas self-decision was the major reason of antibiotic use (40.7%) and main source of information was retail pharmacist (42.6%). Common cold and flu is a major problem for which antibiotics were mainly utilized by pharmacy students (35.2%).
Conclusion:
The study showed good knowledge of pharmacy students regarding antibiotic usage. However, students' attitude towards antibiotic use was poor. The study recommends future studies to be conducted with interventional design to improve knowledge and attitude of pharmacy students about antibiotic use and resistance.
Keywords: Antibiotics, knowledge, pharmacy students, resistance, Trinidad and Tobago
INTRODUCTION
World Health Organization (WHO) has reported the increase antibiotic resistance worldwide.[1] Drug resistance consequences in increased hospital stay, costs, morbidity, and mortality.[2] Antibiotic resistance crisis is difficult in developing countries because of high burden of infectious diseases, irrational practice of antibiotics, availability of antibiotics without prescription and lack of laboratories for antibiotics susceptibility testing.[3] Expansion of antibiotic resistance is accelerated by increased use of antibiotics[4] and previous reports claim that >50% of antibiotics are sell or purchased without a valid prescription.[5] The main reasons of self-antibiotics practice in developing countries over-the-counter availability, prescribing on demand, high cost of the hospitals or healthcare consultation and dissatisfaction with medical practitioners.[6]
A noteworthy area was highlighted by many researchers regarding the inadequate training of healthcare professionals in their undergraduation in an area of antibiotic use and resistance.[7] Competence in understanding of resistance patterns is a valuable guide to devise antibiotic guidelines and directing the antibiotic practices toward a right path. In view of this, many studies have emphasized on revising the curriculum of junior healthcare professionals to promote an appropriate use of antibiotics.[8] Recently, WHO has also embraced the role of undergraduate training in prudent prescribing.[1]
The role of pharmacists is unequivocal in this war against antibiotic resistance. They are viewed as a more knowledgeable and resourceful healthcare professional to assist in infection control campaign. More importantly, community pharmacists are blessed to be called as a Gateway Practitioner. They have the significant opportunity to portray a prestigious role of promoting public health by their active participation in antibiotic stewardship program. The objective of this study was to assess the knowledge, attitude and practice (KAP) of BSc Pharmacy students toward antibiotic use and resistance. Our goal was to identify the knowledge gaps among pharmacy students to form the basis of effective interventions regarding their understanding of pharmacist's directed antibiotic stewardship program.
METHODS
A cross-sectional study was conducted for a period of 2 months in one of the major public sector university of Trinidad and Tobago. The data were collected with the approval of Head of the Department. Furthermore, the participation of students in this study was voluntary, and it was informed to the students that completion and submission of the questionnaire would be taken as their consent to participate in this study. High level of confidentiality and anonymity was maintained throughout the study.
The year three- and four-pharmacy students were selected for this study. All the participants were briefed about the objectives of the study before requesting them to voluntary participate in this study. A total of 130 students were enrolled in the pharmacy school of studied University, and all the students were approached to participate in this study.
A self-administered questionnaire was designed and used as a tool to collect the data from the participants. The questionnaire was designed by a thorough literature review of the related published studies,[9,10] after which the questions were short-listed to be included in the final questionnaire.
The questionnaire consisted of five sections. The first section explored the demographic information such as gender, living status, and family residence. The second section, comprised of eight questions, evaluated the knowledge of participants about the use of antibiotics. The knowledge of participants was evaluated by asking questions regarding the effectiveness, adverse effects, resistance and economical concerns, policy issues and implication of antibiotic use. The third section assessed the attitude of respondents regarding antibiotic use and resistance. This section included five questions. The fourth part explored the self-antibiotic practices of pharmacy students such as frequency, reason, source, indication and type of antibiotic use. The last part of the questionnaire evaluated the students regarding their knowledge of possible causes of antibiotic resistance.
Data were statistically analyzed using SPSS 20 for Windows (IBM Corporation, Armonk, New York). Descriptive analysis was employed, and the results were expressed in frequency and percentages. Nonparametric tests (Mann–Whitney U-test) were performed to inter-relate mean knowledge score and demographic variables. Chi-squares test was also used to assess the association between dependent and independent variables. P < 0.05 was considered as a significant association.
RESULTS
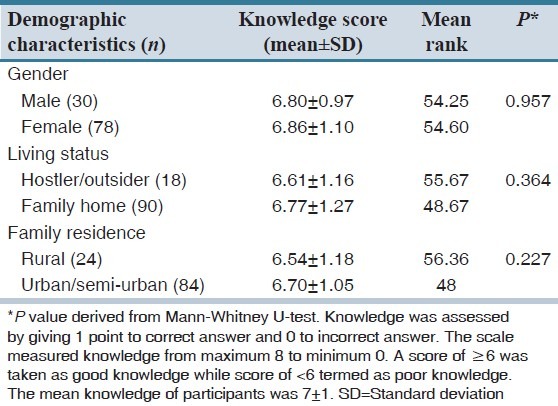
A total of 108 students participated in this study. The results showed good knowledge of antibiotic use among pharmacy students. Female participants showed slightly higher knowledge as compared to their male counterpart; however, the difference was not supported by the statistical analysis. Those living with family and in urban/semi-urban areas appeared to be more knowledgeable as compared to their respective groups, though the difference was not statistically significant. The inter-relation of knowledge of antibiotic use and demographic variables is presented in Table 1.
Table 1.
Inter-relation of knowledge of antibiotic use and score with demographic characteristics of participants (n=108)
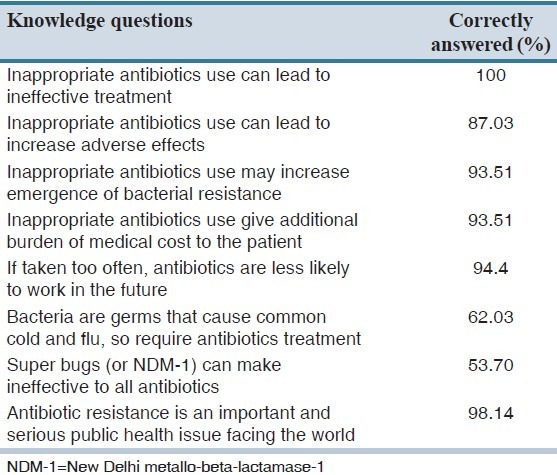
The knowledge of pharmacy students was remarkably high for most of the questions. All the participants correctly answered that inappropriate antibiotics lead to ineffective treatment. Similarly, 98.14% correctly identified antibiotic resistance as a serious public health issue. However, the proportion of students who correctly answered the question was quite low when asked about superbugs and their relation with antibiotics (53.7%). Likewise, only 62.03% correctly answered bacteria are not responsible for common cold and flu. The complete description of students' knowledge of antibiotic use is tabularized in Table 2.
Table 2.
Students who answered correctly to the knowledge questions regarding antibiotic use (n=108)
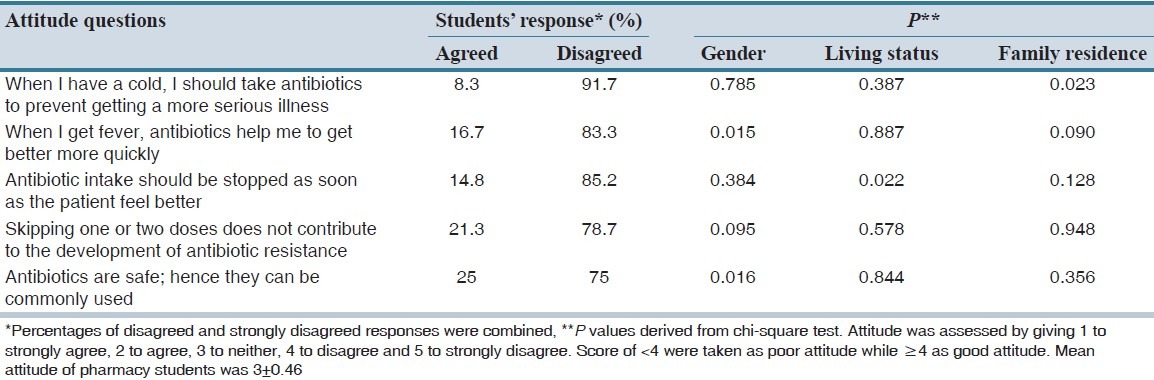
The overall attitude of pharmacy student was poor. A significant difference was observed between rural and urban respondents when asked whether antibiotics help in the prevention of illness during common cold and flu. Urban population agreed more to this statement as compared to rural respondent; however, overall, only 8.3% respondents agreed to this statement. One-fourth of the participants believed that antibiotics are safe and can be commonly used. Male respondents tend to agree more to this statement as compared to their female counterpart. Students' responses to various attitude questions are mentioned in Table 3.
Table 3.
Students' attitude towards antibiotic use (n=108)
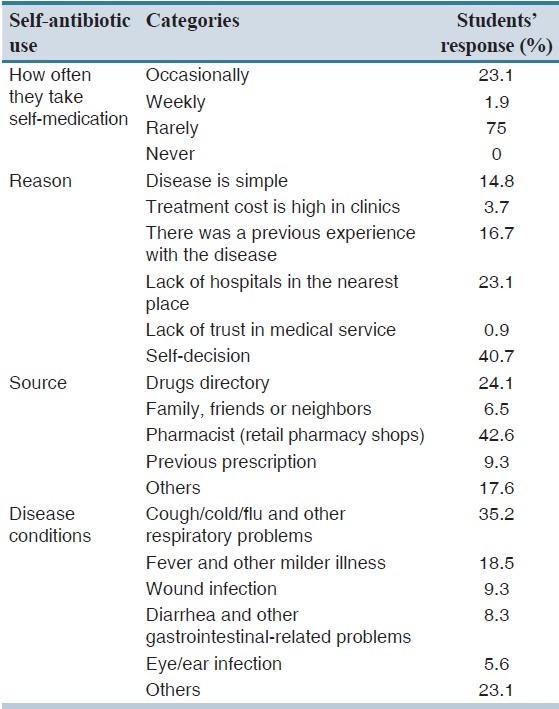
The results showed that three-fourths of pharmacy students rarely use antibiotics while self-decision was the major reason of antibiotic use (40.7%). The main source of information about antibiotics was pharmacist available on retail shop (42.6%). Common cold and flu is a major problem for which antibiotics were mainly utilized by pharmacy students (35.2%). The results of self-antibiotic practice are presented in Table 4. Penicillins were the commonly used drugs reported by pharmacy students (34%).
Table 4.
Self-antibiotics practice among the participated students (n=108)
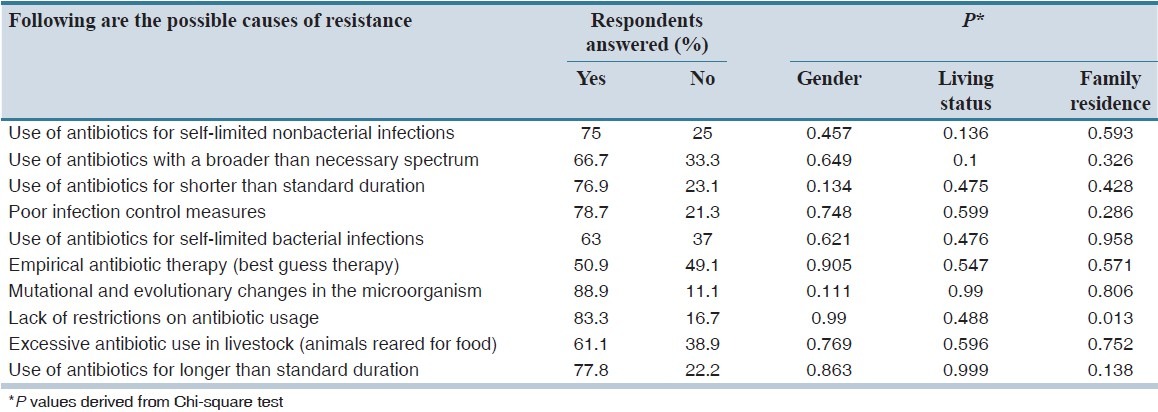
Another aspect of this study highlighted the students' response on the possible causes of antibiotic resistance. A remarkable variation in the responses was noted when asked whether empirical therapy could be a possible cause of antibiotic resistance, as 50% of students agreed to this statement. Similarly, 61.1% of students identified excessive antibiotic use in livestock as a likely cause of antibiotic resistance. Moreover, majority of students agreed that mutational and evolutionary changes in the micro-organism (88.9%) and Lack of restrictions on antibiotic usage (83.3%) are the potential causes of antibiotic resistance [Table 5].
Table 5.
Students perception of possible causes of antibiotic resistance (n=108)
DISCUSSION
The study examined the KAP of antibiotic use and resistance among senior pharmacy students in Trinidad and Tobago. To the best of our knowledge, this is the first study which has examined KAP among pharmacy students in Trinidad and Tobago.
The results suggested that the knowledge of pharmacy students regarding antibiotic use and resistance was above par. This finding is in line with other published studies which also reported good understanding of antibiotics among healthcare students.[9] Our results were also similar to another study which reported good knowledge of medical students with respect to antibiotic use and resistance.[10] However, it was noted that this increased knowledge of healthcare professionals in West Indies could not be translated into practice as inappropriateness of antibiotic prescribing was observed in primary healthcare facilities in North Trinidad.[11] The likely reasons of this discrepancy could be lack of resources and training opportunities and excessive workload. This gap in execution of knowledge could be bridged by effective interventions and promoting rational antibiotic use.[12] Although, 100% participants believed that irrational use of antibiotic can lead to ineffective treatment, it is also noteworthy to mention that only 62% students correctly answered when asked whether antibiotics are required in common cold and flu. This result is relatively poor in accordance to other study in which 95% students correctly answered the question.[9]
The findings of the current study showed a negative attitude of pharmacy students towards antibiotic use and resistance. 25% students believed that antibiotics are safe enough to be used in common practice. In contrast, researchers reported that 15% participants perceived antibiotics as safe drugs. Similarly, the results were also not much different when it was revealed that students did not have clear concepts of medication adherence as a reasonable number of students believed skipping of doses would not contribute to resistance.[10]
A large proportion of pharmacy students in this study rarely used nonprescribed antibiotics. The results are in line with other published study which also reported the same.[13] Cough, cold, and flu were the major problems for which antibiotics were used commonly by the students. The results are in accordance to a study where common cold was the major cause of antibiotics self-practices. In contrast, the results were more discouraging when a study reported that 60% of their participants recommended antibiotics for viral infections.[14] Outcome based education could be an effective approach to bridge the gap between from knowledge to practice.
When asked about the causes of antibiotic resistance, it was observed that Mutational and evolutionary changes in the micro-organism and Lack of restrictions on antibiotic usage were the major causes identified by the participants, while fewer participants perceived empirical therapy as the potential cause of antibiotics. Similar results were found in another study.[9] The results highlight the need to educate pharmacy students' regarding the potential causes of antibiotic resistance, and more importantly the significance the following guidelines for the empirical therapy.[15]
The strength of this study is that it addresses the major issue of antibiotic use and resistance in Trinidad. The other potential feature of this study is that it selected senior pharmacy students as a sample population on which not much research has been done in the past. The findings of this study would urge the researchers to explore this area by recruiting more students from other schools of faculty of medical sciences. However, like any other study, this research also has some limitations. The convenience sampling approach of recruitment of one pharmacy school may limit the generalizability of the results. However, it is pertinent to mention that this is the only school offering pharmacy education in small islands of Trinidad and Tobago. As a general limitation to knowledge and attitude research, we cannot ignore the tendency of participants to provide more socially desirable results.
The study showed good knowledge of pharmacy students regarding antibiotic use. However, students' attitude towards antibiotic use was poor. Self-decision was the major reason which persuaded pharmacy students for self-antibiotic use most commonly in common cold and other upper respiratory problems. The findings showed mutational and evolutionary changes in microorganism as the most important, and empirical therapy as the least important cause of antibiotic resistance. The study recommends future researchers to design effective interventions to improve the knowledge and attitude of pharmacy students about antibiotic usage and resistance in Trinidad and Tobago.
AUTHORS' CONTRIBUTION
All authors contributed the idea of research, design of study, data analysis and manuscript preparation.
Footnotes
Source of Support: That the source of extra-institutional funding, particularly that provided by commercial sources, is indicated.
Conflict of Interest: None declared.
REFERENCES
- 1.WHO. The Evolving Threat of Antimicrobial Resistance: Options for Action. 2012. [Last cited on 2014 Aug 10]. Available from: http://www.whqlibdoc.who.int/publications/2012/9789241503181_eng.pdf .
- 2.Abera B, Kibret M, Mulu W. Knowledge and beliefs on antimicrobial resistance among physicians and nurses in hospitals in Amhara Region, Ethiopia. BMC Pharmacol Toxicol. 2014;15:26. doi: 10.1186/2050-6511-15-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vila J, Pal T. Update on antimicrobial resistance in low-income countries: Factors favoring the emergence of resistance. Open Infect Dis J. 2010;4:38–54. [Google Scholar]
- 4.World Health Organization. Global Strategy for the Containment of Antimicrobial Resistance. Geneva: WHO; 2001. [Last cited on 2014 Aug 10]. Available from: http://www.who.int/drugresistance/WHO_Global_Strategy_English.pdf . [Google Scholar]
- 5.Cars O, Nordberg P. Antibiotic resistance - The faceless threat. Int J Risk Saf Med. 2005;17:103–10. [Google Scholar]
- 6.Grigoryan L, Burgerhof JG, Degener JE, Deschepper R, Lundborg CS, Monnet DL, et al. Determinants of self-medication with antibiotics in Europe: The impact of beliefs, country wealth and the healthcare system. J Antimicrob Chemother. 2008;61:1172–9. doi: 10.1093/jac/dkn054. [DOI] [PubMed] [Google Scholar]
- 7.Wright EP, Jain P. Survey of antibiotic knowledge amongst final year medical students. J Antimicrob Chemother. 2004;53:550–1. doi: 10.1093/jac/dkh096. [DOI] [PubMed] [Google Scholar]
- 8.Steinberg I. Clinical choices of antibiotics: Judging judicious use. Am J Manag Care. 2000;6:S1178–88. [PubMed] [Google Scholar]
- 9.Jamshed SQ, Elkalmi R, Rajiah K, Al-Shami AK, Shamsudin SH, Siddiqui MJ, et al. Understanding of antibiotic use and resistance among final-year pharmacy and medical students: A pilot study. J Infect Dev Ctries. 2014;8:780–5. doi: 10.3855/jidc.3833. [DOI] [PubMed] [Google Scholar]
- 10.Khan AK, Banu G, Reshma KK. Antibiotic resistance and usage-A survey on the knowledge, attitude, perceptions and practices among the medical students of a Southern Indian teaching hospital. J Clin Diagn Res. 2013;7:1613–6. doi: 10.7860/JCDR/2013/6290.3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mungrue K, Brown T, Hayes I, Ramroop S, Thurston P, Pereira LP. Drugs in upper respiratory tract infections in paediatric patients in North Trinidad. Pharm Pract (Granada) 2009;7:29–33. doi: 10.4321/s1886-36552009000100004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kolluru S, Roesch DM, de la Fuente AA. A multi-instructor, team-based, active-learning exercise to integrate basic and clinical sciences content. Am J Pharm Educ. 2012;76:33. doi: 10.5688/ajpe76233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mitsi G, Jelastopulu E, Basiaris H, Skoutelis A, Gogos C. Patterns of antibiotic use among adults and parents in the community: A questionnaire-based survey in a Greek urban population. Int J Antimicrob Agents. 2005;25:439–43. doi: 10.1016/j.ijantimicag.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 14.Azevedo MM, Pinheiro C, Yaphe J, Baltazar F. Portuguese students' knowledge of antibiotics: A cross-sectional study of secondary school and university students in Braga. BMC Public Health. 2009;9:359. doi: 10.1186/1471-2458-9-359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chambless DL, Hollon SD. Defining empirically supported therapies. J Consult Clin Psychol. 1998;66:7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]


