Abstract
Objective:
Etomidate is an imidazole derivative and formulated in 35% propylene glycol. When given without a rapid lidocaine injection, etomidate is associated with pain after injection. Magnesium (Mg) is a calcium channel blocker and influences the N-methyl-D-aspartate receptor ion channel. The aim of the study is to evaluate the efficiency of preemptive injection of magnesium sulfate and lidocaine on pain alleviation on etomidate intravenous injection.
Methods:
In a randomized, double-blinded trial study, 135 adult patients scheduled for elective outpatient or inpatient surgery were divided into three groups. Group M received 620 mg magnesium sulfate, Group L received 3 ml lidocaine 1% and Group S received normal saline, all in a volume of 5 mL followed by a maximal dose of 0.3 mg/kg of 1% etomidate. Pain was assessed on a four-point scale: 0 = no pain, 1 = mild pain, 2 = moderate pain and 3 = severe pain at the time of pretreatment and etomidate injection.
Findings:
About 60% of patients in the control group had pain during etomidate injection as compared to 22.2% and 40% in the lidocaine and magnesium sulfate groups, respectively. There was difference in induction pain score between three treatment groups, significantly (P = 0.01) and observed differences in pain scores between “normal saline and lidocaine group” (P < 0.001) and “normal saline and magnesium sulfate groups” were statistically meaningful (P = 0.044).
Conclusion:
Intravenous magnesium sulfate and lidocaine injection are comparably effective in reducing etomidate-induced pain.
Keywords: Etomidate, Lidocaine, Magnesium sulfate, pain, pretreatment, prevention
INTRODUCTION
Several intravenous (IV) agents used in present-day anesthesia practice often produce pain after IV injection. When given without an adjuvant, etomidate (formulated in 35% propylene glycol) is associated with inflammation and pain after injection.[1,2]
Etomidate (Amidate, Hynomidate) is an imidazole derivative[3] that its properties include hemodynamic stability, minimal respiratory depression, cerebral protection, pharmacokinetics enabling rapid recovery and maintenance of anesthesia after either a single dose or a continuous infusion.[4]
Etomidate has the disadvantage of pain on injection that a rapid lidocaine injection is effective in the alleviation of pain during the injection of etomidate. Pain on injection is reduced further using a large vein. The lipid formulation of etomidate also is associated with a much lower incidence of pain on injection, thrombophlebitis, and histamine release on injection.[1] The hyperosmolality of the propylene glycol formulation may cause direct injury to vascular endothelium, resulting in local physical damage and release histamine into the circulation.[5]
Magnesium sulfate has been used for many years for the management of preeclampsia, cardiac arrhythmias and postoperative pain.[6,7] Magnesium is an antagonist of the N-methyl-D-aspartate (NMDA) receptor ion channel, and this may explain part of its analgesic activity.[8]
There are no advantages for using magnesium sulfate in comparison with lidocaine in the term of adverse effects. It was not investigated before which drug was better for control of pain following etomidate injection. So the present study was conducted to compare the efficacy of magnesium sulfate with lidocaine on the incidence and severity of pain after induction of anesthesia with etomidate.
METHODS
This double-blinded, randomized study was conducted in 2011-2012 at Kashani Hospital. We studied 135 patients, (American Society of Anesthesiologists [ASA]) physical status I and II, aged 18–65 years and who were scheduled for elective outpatient or inpatient (orthopedic and neurosurgical surgeries). Inclusion criteria were patients without neuromuscular disease and difficulty in communication, patients without ischemic heart disease, cardiac rhythm other than sinus rhythm, recent convulsions, history of endocrine or metabolic disease, severe neurological deficits and psychiatric disorders, those without thin dorsal hand veins, nonsuspected or unknown pregnancy, nonlactating women, patients without disorders of pancreas or liver, renal problems, thrombophlebitis, or chronic pain for which they were taking sedative or analgesic medication, received an analgesic within 24 h before surgery, and those without a history of difficult intubation. Exclusion criteria were patients with allergy to etomidate, magnesium sulfate and lidocaine and patients with cardiac arrest. Also, if there was any change in technique of anesthesia, the patient was excluded from the study. If the patient condition was not suitable for general anesthesia, the technique of anesthesia was changed to the regional anesthesia.
In the preoperative holding area, informed consent was obtained, fasting status was confirmed, and a 20-gauge peripheral IV catheter was placed in the dorsum of the hand without subcutaneous local anesthesia. Lactated Ringer's solution was infused, and a premedication dose of IV midazolam (1–2 mg) was administered. Monitoring including electrocardiogram lead II, noninvasive arterial blood pressure, and pulse oximetry was instituted.
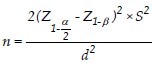
The sample size was calculated with an alpha level equal to 5% and the study power equal 80% and using the following formula about 45 samples in each group and the total 135 samples.[7]
Patients were randomly assigned to one of three groups by computer-generated randomization. Patients in the magnesium group (Group M, n = 45) received 620 mg of IV magnesium sulfate (2 ml) in 3 ml of normal saline, patients in the lidocaine group (Group L, n = 45) received IV lidocaine 1% (3 ml) in 2 ml of normal saline, whereas patients in the control group (Group S, n = 45) received 5 ml of saline over the same period. The anesthetist was unaware of which solution was administered. The drugs used in the study were prepared in identical syringes at room temperature by personnel blinded to the study group.
Preoxygenation via face mask was performed for 3 min. Then all groups were induced with etomidate over 1 min, up to a maximal dose of 0.3 mg/kg in 20 ml of normal saline.
Etomidate has onset effect time 30–60 s since injection till loss of consciousness.[4] It was administered over 30–60 s. Patients were evaluated for pain every 10 s until loss of consciousness. The severity of injection pain was explained using the four-point scale: 0 = no pain, 1 = mild pain (reported only in response to questioning and without behavioral signs), 2 = moderate pain (pain reported in response to questioning and accompanied by behavioral signs or pain reported spontaneously without questioning), or 3 = severe pain (strong vocal response or response accompanied by facial grimacing, arm withdrawal).[2] The absence or presence of erythema in the arm reaction was observed and recorded. Heart rate (HR) and systolic blood pressures (SBP) and diastolic blood pressures (DBP) were recorded before the administration of pretreatment solution and 1–3 min after etomidate injection. Hypotension was characterized as mean medium arterial pressure (MAP) reduction (computed comparing the baseline blood pressure with the minimal value calculated) and the total number of patients with MAP decrease >20 mmHg. During the first postoperative 24 h, the injection site was assessed for pain, oedema, or allergic reactions by an anesthesiologist who was unaware which drug had been administered. Statistical analysis was carried out with the SPSS 22 software (SPSS, Inc., Chicago, IL). One-way analysis of variance and post-hoc comparisons at various points in time using Bonferroni's type I error rate correction was used to compare differences in mean values between groups. Chi-square test and Mann-Whitney test was used for analysis of qualitative variables. The P < 0.05 was considered statistically significant.
RESULTS
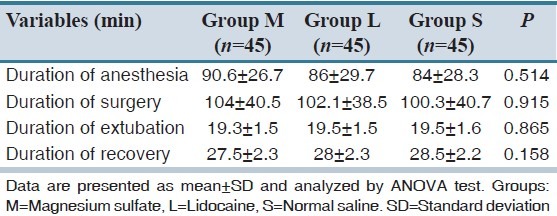
For this study, 135 patients were randomly assigned to three treatment groups. Demographic data (age, gender, ASA, weight and height) were similar in three groups [Table 1]. There were no differences in duration of anesthesia (the time from injection of anesthetic drug till its discontinuation), duration of surgery (the time from beginning of surgery till its termination), extubation time (the time from discontinuation of anesthetic drug till extubation) and recovery stay time (the time since from arrival of patient to the recovery room till its leaving) between three groups [Table 2].
Table 1.
Demographic data of patients in three treatment groups
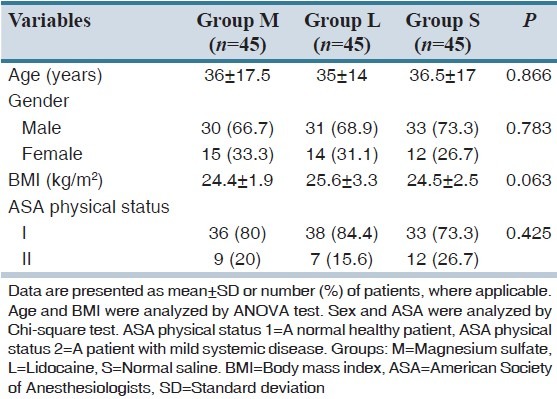
Table 2.
Duration of anesthesia, surgery, extubation and recovery in three treatment groups
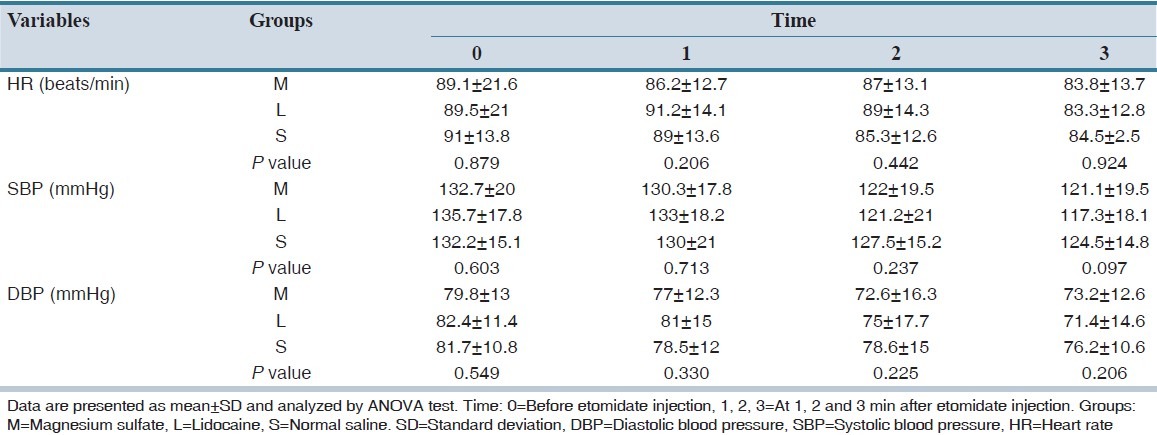
The mean HR was not different in the three groups at different time intervals, significantly [Table 3]. No difference was showed in all groups with regard to SBP and DBP, recorded at different time intervals [Table 3]. There were no patients with hypotension in any group.
Table 3.
Patient's mean SBP, DBP and HR values
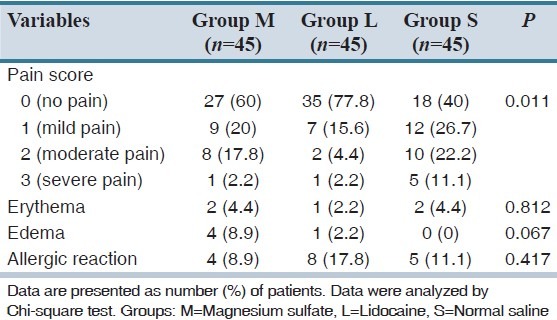
The incidence of pain during injection of etomidate in three groups is shown in Table 4. Duration of etomidate injection, in normal saline group 60% of the patients had pain as compared to 40% and 22.22% in the magnesium sulfate and lidocaine groups, respectively. There was a significant difference in the incidence of different severity of pain score between three treatment groups (P = 0.01) [Table 4] as analyzed with Chi-square test. The results showed that the observed differences in pain scores between “normal saline versus lidocaine group” (P < 0.001) and “normal saline versus magnesium sulfate groups” (P = 0.044) were statistically meaningful. But there was no significant difference in pain scores between lidocaine versus magnesium sulfate groups. The observed differences in erythema during the first postoperative 24 h at the injection site between normal saline, magnesium sulfate and lidocaine groups were not significant (P = 0.812). Similarly, there was no difference in oedema between the all groups (P = 0.067). Also, the allergic reaction between three groups showed that there were no comparative differences (P = 0.417).
Table 4.
The incidence of pain, erythema, edema and allergic reaction during etomidate injection in three groups
DISCUSSION
There was no difference in demographic data between three groups showing that they affected neither the presence nor the intensity of pain. The hemodynamic stability indices such as HR, SBP and DBP were recorded at 0–3 min after the etomidate injection in three groups. Result showed that there were not differences in mentioned hemodynamic stability indices between the groups. This demonstrated that lidocaine and magnesium pretreatments were equally safe in patients' hemodynamic stability during IV. Etomidate injection. There were no statistically significant differences in duration of anesthesia, surgery, extubation, and recovery between the groups.
Etomidate is an imidazole derivative (R-[+]- pentylethyl-1H-imidazole-5 carboxylate sulfate).[3] Despite all the advantages of using the etomidate for induction of anesthesia, rapid administration of etomidate is associated with pain. Therefore, considering the use of etomidate in clinical practice, the pain frequently reported on the induction of anesthesia cannot be neglected.[8,9] Many methods have been used to reduce the incidence of pain on etomidate injection with variable results. Injecting into a large forearm vein reduces the pain.[1,2] Lipid formulation of etomidate also is associated with a much lower incidence of pain on injection.[1] Also, using some medications such as thiopental sodium, opioids, and metoclopramide preemptively prevented the pain associated with etomidate injection. Altering temperature and PH of etomidate formulation is another technique used in this respect;[10] however, IV lidocaine is the most frequently used method to reduce pain associated with induction doses of etomidate.[9]
Lidocaine, a local anesthetic, reversibly blocks peripheral nerve pathways through the action on excitable membranes in the arm.[10] It blocks fast voltage-gated sodium channels in the cell membrane of nerve impulses.[10] Lidocaine pretreatment may modify vascular pain on etomidate injection because of its local analgesic effect of stabilizing the kinin cascade.[11,12] Brown and Moss[2] stated a significant reduction (from 37% to 10%) in the frequency of pain on etomidate injection of into veins on the dorsum of the hand by the addition of lidocaine. Melnick et al.[13] reported that lidocaine is an effective drug to reduce the etomidate-induced pain by allowing lidocaine to dwell prior to etomidate administration.
Magnesium is the calcium channel blocker, and it probably interferes with calcium channel and NMDA receptors. Calcium is required for the release of various neurotransmitters and substances, implicated in nociceptive pain and inflammation. Thus, the analgesic action of some calcium channel blockers is mediated by an increase in nociceptive threshold resulting from interference with calcium influx.[14,15] A second possible explanation for the analgesic action of magnesium is its antagonism of the NMDA receptor. The NMDA receptor is coupled to an ion channel permeable to K+and Ca2+. Magnesium blocks NMDA receptor currents in a voltage-dependent manner by blocking the receptor channel.[16,17,18,19] Guler et al. compared low-dose magnesium and ketamin in preventing the injection pain of etomidate and found ketamin to be superior.[17] In a study of magnesium sulfate pretreatment to alleviate pain on propofol injection, a comparison with ketamine or lidocaine, Honarmand and Safavi[18] noted that IV magnesium, ketamine, and lidocaine pretreatment are equally effective in attenuating propofol-induced pain. One previous study showed that MgSO4 620 mg was effective in reducing severity of myoclonic muscle movements induced by etomidate.[17]
Our study had some limitations. We didn't check the serum level of MgSO4 and lidocaine that alleviated etomidate induced pain. Also, we used the bolus doses of MgSO4 and lidocaine. We recommend designing another study to investigate the effect of infusing MgSO4 and lidocaine in this respect. Another recommendation is using a combination of MgSO4 and lidocaine in this regard.
It is concluded in the current study, after comparing the two methods, pretreatment with IV magnesium 620 mg and lidocaine 1% 3 ml was comparably effective in attenuating pain during IV injection of etomidate. Therefore, anesthesiologist based on the availability of magnesium sulfate or lidocaine can be used either of these drugs.
ACKNOWLEDGMENTS
The authors wish sincerely to thank the support of all the colleagues in Kashani Hospital Medical Center affiliated to Isfahan University of Medical Sciences in Isfahan, Iran. Furthermore, our special thanks go to the patients, who wholeheartedly and actively assisted us to carry out this research.
Footnotes
Source of Support: Anesthesiology and Critical Care Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
Conflict of Interest: None declared.
REFERENCES
- 1.Doenicke AW, Roizen MF, Hoernecke R, Lorenz W, Ostwald P. Solvent for etomidate may cause pain and adverse effects. Br J Anaesth. 1999;83:464–6. doi: 10.1093/bja/83.3.464. [DOI] [PubMed] [Google Scholar]
- 2.Brown PM, Moss E. Reduction of pain on injection of etomidate. Anaesthesia. 1981;36:814–6. doi: 10.1111/j.1365-2044.1981.tb08823.x. [DOI] [PubMed] [Google Scholar]
- 3.Corssen G, Reves J, Stanley T. Intravenous Anesthesia and Analgesia. Philadelphia: Lea and Febiger; 1988. Dissociative anesthesia; p. 99. [Google Scholar]
- 4.Janssen P, Niemegeers J, Schellekens K. Etomidate, R-(+)-Ethyl-1-(alpha-methyl-benzyl) imidazole-carboxylate (R 16659): A potent, short-acting and relatively atoxic intravenous hypnotic agent in rats. Arzneimittelforschung. 1971;21:1234. [PubMed] [Google Scholar]
- 5.Ruo W, Shay J, Attele A, Doenicke A, Moss J. Propylene glycol damages vascular smooth muscle and endothelium. Anesthesiology. 1992;775:A1096. [Google Scholar]
- 6.Begum R, Begum A, Bullough CH, Johanson RB. Reducing maternal mortality from eclampsia, using magnesium sulphate. Eur J Obstet Gynecol Reprod Biol. 2000;92:223–4. doi: 10.1016/s0301-2115(99)00274-2. [DOI] [PubMed] [Google Scholar]
- 7.Koinig H, Wallner T, Marhofer P, Andel H, Hörauf K, Mayer N. Magnesium sulfate reduces intra-and postoperative analgesic requirements. Anesth Analg. 1998;87:206–10. doi: 10.1097/00000539-199807000-00042. [DOI] [PubMed] [Google Scholar]
- 8.Ascher P, Nowak L. Electrophysiology studies of NMDA receptors. Trends Neurosci. 1987;10:284–8. [Google Scholar]
- 9.Owen H, Spence AA. Etomidate. Br J Anaesth. 1984;56:555–7. doi: 10.1093/bja/56.6.555. [DOI] [PubMed] [Google Scholar]
- 10.Picard P, Tramèr MR. Prevention of pain on injection with propofol: A quantitative systematic review. Anesth Analg. 2000;90:963–9. doi: 10.1097/00000539-200004000-00035. [DOI] [PubMed] [Google Scholar]
- 11.Lai YY, Chang CL, Yeh FC. The site of action of lidocaine in intravenous regional anesthesia. Ma Zui Xue Za Zhi. 1993;31:31–4. [PubMed] [Google Scholar]
- 12.Scott RP, Saunders DA, Norman J. Propofol: Clinical strategies for preventing the pain of injection. Anaesthesia. 1988;43:492–4. doi: 10.1111/j.1365-2044.1988.tb06641.x. [DOI] [PubMed] [Google Scholar]
- 13.Melnick BM, Phitayakorn P, McKenzie R. Abolishing pain on injection of etomidate. Anesthesiology. 1987;66:444. doi: 10.1097/00000542-198703000-00048. [DOI] [PubMed] [Google Scholar]
- 14.Memis D, Turan A, Karamanlioglu B, Süt N, Pamukçu Z. The use of magnesium sulfate to prevent pain on injection of propofol. Anesth Analg. 2002;95:606–8. doi: 10.1097/00000539-200209000-00020. [DOI] [PubMed] [Google Scholar]
- 15.Wong CH, Dey P, Yarmush J, Wu WH, Zbuzek VK. Nifedipine-induced analgesia after epidural injection in rats. Anesth Analg. 1994;79:303–6. doi: 10.1213/00000539-199408000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Altura BT, Altura BM. Endothelium-dependent relaxation in coronary arteries requires magnesium ions. Br J Pharmacol. 1987;91:449–51. doi: 10.1111/j.1476-5381.1987.tb11235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guler A, Satilmis T, Akinci SB, Celebioglu B, Kanbak M. Magnesium sulfate pretreatment reduces myoclonus after etomidate. Anesth Analg. 2005;101:705–9. doi: 10.1213/01.ANE.0000160529.95019.E6. [DOI] [PubMed] [Google Scholar]
- 18.Honarmand A, Safavi M. Magnesium sulphate pretreatment to alleviate pain on propofol injection: A comparison withketamine or lidocaine. Acute Pain. 2008;10:23–9. [Google Scholar]
- 19.Isitemiz I, Uzman S, Toptas M, Vahapoglu A, Gül YG, Inal FY, et al. Prevention of etomidate-induced myoclonus: Which is superior: Fentanyl, midazolam, or a combination. A Retrospective comparative study? Med Sci Monit. 2014;20:262–7. doi: 10.12659/MSM.889833. [DOI] [PMC free article] [PubMed] [Google Scholar]


