Abstract
Chiari-like malformation (CLM) with syringomyelia (SM) in dogs is particularly prominent in the Cavalier King Charles spaniel breed, but has also been reported in several other small breed dogs. Over a period of 3 years, 23 canine patients were treated surgically for CLM-SM. Surgery consisted of foramen magnum decompression, durotomy, duraplasty, and free autogenous adipose tissue grafting (fat graft). All patients were re-evaluated clinically at least 1 month after surgery and some up to 3 years after surgery. Improvement was noted on all clinical evaluations. A questionnaire was mailed to all 23 owners after a period of at least 1 year after surgery. Seventeen surveys were returned. No patient has required additional surgery to date, 94% (16/17) had some improvement in quality of life after surgery, and none were judged to deteriorate to less than the pre-surgical status. The authors conclude that this surgical procedure, combined with medical therapy, resulted in favorable long-term outcomes.
Résumé
Chirurgie de décompression du trou occipital chez 23 patients atteints de malformation semblable à celle du syndrome de Chiari 2007–2010 : résultats et données du sondage auprès des propriétaires. Une malformation semblable à celle du syndrome de Chiari (MSC) avec syringomyélie (SM) chez les chiens est particulièrement prépondérante chez la race d’épagneuls Cavalier King Charles, mais elle a aussi été signalée chez plusieurs autres races de petits chiens. Pendant une période de trois ans, 23 patients canins ont été traités par chirurgie pour le MSC-SM. La chirurgie consistait à faire une décompression du trou occipital, une durotomie, une duraplastie et une greffe de tissu adipeux autogène (greffe de graisse). Tous les patients ont été réévalués cliniquement au moins 1 mois après la chirurgie, puis environ 3 ans après la chirurgie. Une amélioration a été notée dans toutes les évaluations cliniques. Un questionnaire a été envoyé par la poste aux 23 propriétaires après une période d’au moins un an suite à la chirurgie. Dix-sept sondages ont été retournés. Aucun patient n’a eu besoin de chirurgie additionnelle jusqu’à maintenant, 94 % (16/17) ont eu une certaine amélioration de la qualité de vie après la chirurgie et aucun n’a été jugé comme ayant subi une détérioration de son état avant la chirurgie. Les auteurs concluent que cette intervention chirurgicale, combinée avec un traitement médical, a produit des résultats favorables à long terme.
(Traduit par Isabelle Vallières)
Introduction
Numerous publications have described Chiari-like malformation (CLM) with syringomyelia (SM) in dogs, with the Cavalier King Charles spaniel (CKCS) being the most commonly affected breed (1–3). Surgical procedures for treatment of this disorder consist of foramen magnum decompression (FMD) and durotomy (4), FMD with a titanium-mesh cranioplasty and durotomy (5); and FMD with a durotomy and duraplasty with lyophilized swine submucosa (intestinal or bladder) coupled with a free adipose tissue autograft implanted over the duroplasty (6). While all of these surgical methods of treatment appear to have been mostly successful, long-term follow-up information is not available in the literature. In addition, specific criteria for surgical treatment are lacking.
Materials and methods
A total of 23 foramen magnum decompression (FMD) surgeries were performed on 18 CKCS, 1 Yorkshire terrier, and 4 Chihuahuas between 2007 and 2010. Dogs were considered surgical candidates if they met all the criteria shown in Table 1 and received oral medications [gabapentin, 5 mg/kg body weight (BW), q8h, and omeprazole, 1 mg/kg BW, q24h] for 2 wk prior to surgery. In all patients, surgery consisted of a FMD, a partial dorsal laminectomy of C1, an I-shaped incision through the meninges from the dorsal region of the vermis to the cranial one-third of C1, marsupialization of the dura using 5-0 monofilament absorbable suture (Figure 1), removal of adhesions using a lint free sponge, duroplasty using lyophilized swine sub-mucosa (Figures 2A, B), and placement of a free autogenous adipose tissue graft (obtained from the gluteal region) over the duroplasty (Figures 3A, B). All surgeries were performed by a team consisting of the faculty neurosurgeon (AS) and at least 1 neurology/neurosurgery resident.
Table 1.
Mississippi State University CVM Neurosurgery/Neurology Section’s Chiari-like Malformation/Syringomyelia Surgical Candidate Criteria
|
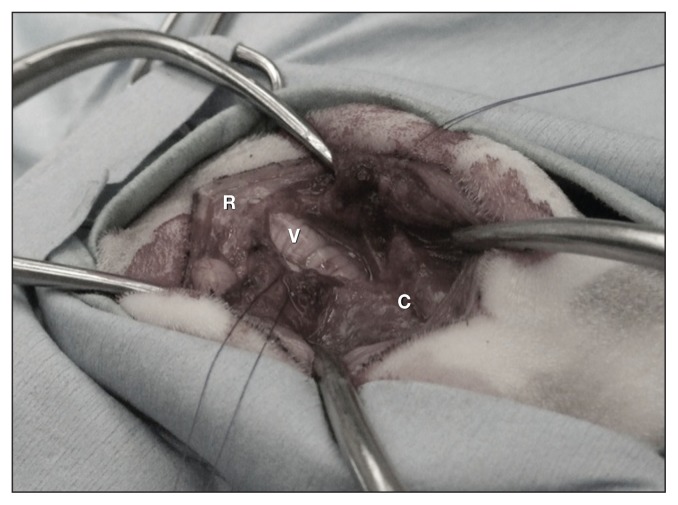
Figure 1.
The meninges have been incised with a number 12 scalpel blade and marsupialization is performed using 5-0 synthetic absorbable sutures. R — rostral; C — caudal; V — vermis of the cerebellum extending underneath the dorsal lamina of C1 vertebra.
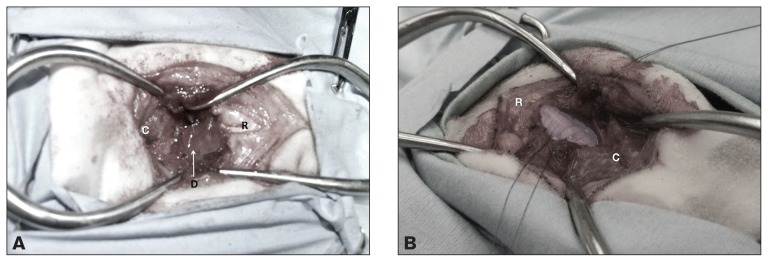
Figure 2.
A — Intraoperative photograph showing placement of lyophilized swine submucosa to create the duraplasty. This material is designed to provide scaffolding for growth of the meninges over the top of the exposed cerebellum and cervical spinal cord. R — rostral; C — caudal; D — duraplasty. B — Computer generated image (CGI) demonstrating placement of the lyophilized swine submucosa over the marsupialized and decompressed CNS tissues.
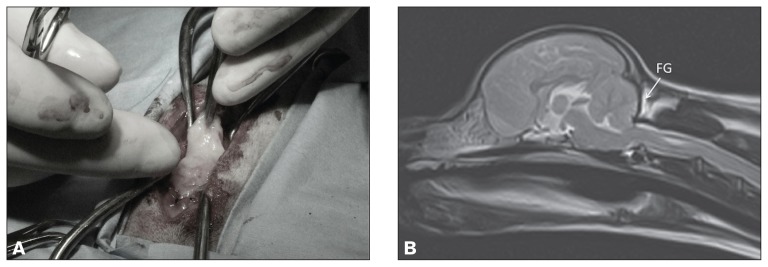
Figure 3.
A — Placement of the free autogenous adipose tissue (fat graft) over the FMD and duraplasty. B — MRI 1 y after surgery, demonstrating the location and the viability of the free autogenous adipose tissue graft. FG — fat graft.
Follow-up clinical examinations were performed in all 23 patients at 1 month after surgery (Table 2). Some patients were examined multiple times as routine evaluations over a period of 1 to 3 y. A questionnaire was mailed to all 23 owners after a period of at least 1 y after surgery.
Table 2.
Results of pre-operative and 1 month post-operative neurologic examinations for 23 dogs with Chiari-like malformation with syringomyelia
| Patient number | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| Criteria | 1,9,10 22 |
3,6,13, 14,23 | 2,8,15, 17,20 | 4 | 5 | 7 | 11 | 16 | 18 | 19 | 21 |
| Cranial nerve examination | N | N | N | N | N | N | N | N | Def | N | N |
| N | N | N | N | N | N | N | N | N | N | N | |
| Postural reactions | N | N | N | N | N | N | APL | A | N | A | A |
| N | N | N | N | N | N | APL | APL | N | A | APL | |
| Segmental reflexes | N | N | N | N | N | N | N | N | N | N | N |
| N | N | N | N | N | N | N | N | N | N | N | |
| Head and neck hyperpathia | 2 | 3 | 2 | 3 | 2 | 3 | 1 | 3 | 2 | 3 | 2 |
| 1 | 1 | 0 | 2 | 0 | 1 | 0 | 2 | 1 | 1 | 1 | |
| Phantom scratching | L | L | L | S | S | S | S | S | L | L | L |
Results for preoperative examination are given above those for the post-operative examination.
N — normal; Def — spinal accessory and hypoglossal deficits; A — abnormal pelvic and thoracic limbs; APL — abnormal pelvic limbs. Head and neck hyperpathia: 0 = none; 1 = intermittent, mild, or only with very deep palpation; 2 = easily elicited on palpation of neck or head; 3 = spontaneous episodes of pain or muscle spasms of the neck plus vocalization with or without palpation. Phantom scratching (PS): L = owner perceived less PS at 1 month after surgery compared with before surgery; S = owner perceived no change in amount of PS 1 month after surgery compared with before surgery.
Results
There were no intraoperative complications or adverse events resulting from the surgery. The clinical re-evaluations at 1 month after surgery demonstrated clinical improvement in all 23 patients (Table 2). Routine clinical re-evaluations were performed several times in a few patients, with 3 patients returning at 1 y after surgery and 1 patient evaluated 3 y after surgery. All examinations revealed improvement over the pre-operative status as judged by history, physical examination, and neurologic examination. Five patients had follow-up magnetic resonance imaging (MRI) examinations (3 at 3 mo post-surgery, 1 at 6 mo post-surgery, and 1 at 3 y post-surgery). Results of the MRI examinations revealed the fat graft was viable and in the same position as placed at the time of surgery (Figure 3B); there was a slight reduction in the diameter of the syrinx in 1 patient.
The average age of the patients at the time of surgery was 42.8 mo, with a median age of 32.5 mo. The youngest patient in the group was 10 mo old and the oldest was 99 mo. The age ranges were: 10 to 24 mo (7 dogs); 25 to 48 mo (8 dogs); 49 to 99 mo (8 dogs).
Seventeen of 23 owners (74%) returned surveys. Outcome was determined from the survey using the following parameters: i) overall quality of life before surgery; ii) overall quality of life after surgery; iii) level of scratching after compared to before surgery; iv) level of apparent discomfort (pain) after compared to before surgery; v) medications required after surgery; vi) reoccurrence of clinical signs at some point after maximum improvement was seen; and vii) owner comments.
Quality of life was assessed by a scale from 1 to 5: 1 = Extremely poor, considering euthanasia; 2 = Poor, able to obtain some comfort with medical therapy; 3 = Fair overall, but has noticeable signs of disease; 4 = Good, minor signs of disease (occasional scratching, painful); 5 = Excellent, minimal signs of disease (rarely scratches). Of the 17 patients included in this study, the rankings for quality of life before surgery were as follows: 1 (n = 2), 2 (n = 2), 3 (n = 10), 4 (n = 3), 5 (n = 0); 94% of study participants (16/17) had some improvement in quality of life after surgery. One participant had an improvement in quality of life of 4 points. Two participants had improvement in quality of life of 3 points. Five participants had an improvement in quality of life of 2 points. Six participants had an improvement in quality of life of 1 point. Three participants’ owners did not note an improvement on this scale, but based on the client comments, it appeared that 2 out of the 3 did seem to improve. None of the patients were judged by owners to deteriorate to a level below that noted prior to surgery. One owner stated her pet showed improvement for 6 mo, and then regressed to a near pre-surgical state. One owner stated that her pet had several co-morbidities, including right front leg pain associated with a diagnosis of arthritis, unrelated to the CLM-SM. This owner reported that his scratching and pain would be “triggered” by petting near the right shoulder. That owner also explicitly stated in the comments that the patient’s quality of life had improved.
Survey participants were asked to evaluate improvements in scratching and pain by ranking the level of scratching and the perceived level of painful episodes after surgery compared to before surgery on a scale of 1 to 5 (1 = considerably more; 2 = somewhat more; 3 = about the same; 4 = somewhat less; 5 = considerably less). Of the 17 patients, 16 (94%) showed some improvement. Over 18% of patients (3/17) had a level of scratching approximately equal to the pre-surgical level. One owner (1/17) said that the level of scratching had worsened somewhat since surgery, but this pet also had ear and allergy issues. The comment associated with this response was that the patient had a significant improvement in quality of life with almost no pain and no regression as time progressed. The following responses were obtained regarding scratching: 2 (n = 1), 3 (n = 3), 4 (n = 5), 5 (n = 8). The owners perceived some degree of pain relief in 16/17 patients. In 1 patient (1/17) the level of pain seemed equal to that before surgery; however, the owners did not continue prescribed post-operative medications (gabapentin, omeprazole). The following responses were obtained regarding pain level: 3 (n = 1), 4 (n = 4), 5 (n = 12).
Survey participants were asked to list the medications their pet was taking after surgery. Heartworm, flea, and tick preventions are excluded from the following list, even if mentioned. All other relevant and irrelevant medications included: pregabalin (n = 1), levetiracetam (n = 1), tramadol (n = 1), omeprazole (n = 8), gabapentin (n = 8), acetaminophen (as needed: n = 1), carprofen (n = 1), hydroxyzine (n = 1), omega-3 supplements (n = 1), cetirizine (n = 1), “allergy shots” (n = 1), methylprednisolone acetate injections for allergies (n = 1), chlorpheniramine (n = 1), furosemide (n = 1), diphenhydramine HCl (n = 1). Our standard long-term post-operative medications were omeprazole and gabapentin in all 23 patients. Of the 17 patients in the survey responses, 6 had discontinued gabapentin and omeprazole; 2 were taking only omeprazole; 2 were taking only gabapentin; and 6 were taking both omeprazole and gabapentin.
Survey participants were asked to provide an estimation of the amount of time post-procedure it took for the patient to reach maximum improvement. Most clients reported maximum improvement within the first 2 mo. The shortest time recorded was immediately after surgery, and the longest time recorded was 8 mo. The participants were also asked whether their animal was noted to decline to any degree after this point; 53% of owners (9/17) reported some decline. In most instances, the decline was perceived as mild pain or scratching noted anywhere from 6 mo to 3 y after surgery. In 1 case, the decline correlated with a change in post-operative medications. In 1 case, the returning clinical signs resolved with medical management.
Several clients mentioned that episodes of scratching were triggered by certain factors, including exercise, going up and down stairs, stress, being petted in the neck region, other illness, and warm temperatures.
All 17 of the returned surveys expressed satisfaction that they had elected to have the foramen magnum decompression surgery for their pets.
Discussion
The pathophysiology and the pathogenesis of CLM-SM continue to require more definition. Definitive studies to compare treatment modalities (medical versus surgical), to compare medical treatment regimens, to establish criteria for determining the indications for surgery, to establish the optimum timing of surgery (younger versus older patients), and to establish the most efficacious surgical technique are lacking. In this study, we prospectively established criteria for surgical indications which did not alter during the course of the study; we continue to use these today. These criteria were based on clinical impressions from examination and treatment of CLM-SM patients over several years and remain unproven. Severely affected patients with syrinxes < 3 mm in diameter that respond poorly to medical management might also benefit from surgery. Using these criteria, however, provided some consistency in our patient population. One study following 48 dogs with CLM-SM that were treated medically suggested the signs of neuropathic pain were progressive in these patients (7). The 17 owner survey responses reported no progression of neuropathic pain in any of the surgically managed patients.
Our primary goal was to evaluate the long-term outcome of the patients. While it does not represent a large number of patients, the study does provide long-term results on 17 patients treated with the same surgical technique. In addition, the clinical follow-up and the at least 1-year survey follow-up of 17 patients does indicate the surgical technique used (combined with some continued medical therapy in 10/17 patients) is effective, and to date has not resulted in a need for a revision procedure. This is a clinically based trial without the benefit of controls, as one author has proposed (8). Using a blinded study with controls for this condition may not be fair or ethical for the individual patient. However, a weakness of this study is a lack of a control population. Proof that this procedure was the best method of treatment for CLM-SM would require comparison with an equal number of similar patients treated medically.
It remains troubling that little or no reduction in the syrinx seems to occur with any of the results in the current literature. The authors are hopeful that others will publish similar studies and that a meta-analysis may result in additional insight into the most effective treatment for this condition.
Acknowledgments
The authors acknowledge the contributions of Dr. Michelle Carnes and Dr. Jill Narak, both participants in several of the surgeries during their residencies. CVJ
Footnotes
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.Wolfe KC, Poma R. Syringomyelia in the Cavalier King Charles spaniel (CKCS) dog. Can Vet J. 2010;51:95–102. [PMC free article] [PubMed] [Google Scholar]
- 2.Rusbridge C, Greitz D, Bermans, Iskandar J. Syringomyelia: Current concepts in pathogenesis, diagnosis, and treatment. J Vet Intern Med. 2006;20:469–479. doi: 10.1892/0891-6640(2006)20[469:sccipd]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 3.Rusbridge C. PhD dissertation. Utrecht University; Utrecht, The Netherlands: 2007. Chiari-like malformation and syringomyelia in the Cavalier King Charles Spaniel. [Google Scholar]
- 4.Rusbridge C. Chiari-like malformation with syringomyelia in the Cavalier King Charles Spaniel: Long-term outcome after surgical management. Vet Surg. 2007;36:396–405. doi: 10.1111/j.1532-950X.2007.00285.x. [DOI] [PubMed] [Google Scholar]
- 5.Dewey CW, Marino DJ, Bailey KS, et al. Foramen magnum decompression with cranioplasty for treatment of caudal occipital malformation syndrome in dogs. Vet Surg. 2007;36:406–415. doi: 10.1111/j.1532-950X.2007.00286.x. [DOI] [PubMed] [Google Scholar]
- 6.Akin EY, Ortinau NH, Shores A, Carnes MB, Narak J. Foramen magnum decompression with free autogenous adipose tissue graft for treatment of caudal occipital malformation syndrome in dogs. Proceedings ACVS Vet Symposium; Washington, DC, USA. 2009. p. E24. [Google Scholar]
- 7.Plessas IN, Rusbridge C, Driver CJ, et al. Long-term outcome of Cavalier King Charles spaniel dogs with clinical signs associated with Chiari-like malformation and syringomyelia. Vet Rec. 2012;171:501. doi: 10.1136/vr.100449. [DOI] [PubMed] [Google Scholar]
- 8.LeCouteur RA. It’s time. Vet Surg. 2007;36:390–395. doi: 10.1111/j.1532-950X.2007.00284.x. [DOI] [PubMed] [Google Scholar]