Abstract
Objective:
The objective of this study was to demonstrate the sensitivity and specificity of multislice computed tomography (CT) for diagnosis of orbital fractures following different protocols, using an independent workstation.
Materials and methods:
CT images of 36 patients with maxillofacial fractures (symptomatic to orbit region) who were submitted to multislice CT scanning were analyzed, retrospectively. The images were interpreted based on 5 protocols, using an independent workstation: 1) axial (original images); 2) multiplanar reconstruction (MPR); 3) 3D images; 4) association of axial/MPR/3D images and 5) coronal images. The evaluated anatomical sites were divided according to the orbital walls: lateral (with or without zygomatic frontal process fracture); medial; superior (roof) and inferior (anterior, medial). The collected data were analyzed statistically using a validity test (Youden's J index; p<0.05). The clinical and/or surgical findings (medical records) were considered as the gold standard to corroborate the diagnosis of the anatomical localization of the orbital fracture.
Results:
3D-CT scanning presented sensitivity of 78.9%, which was not superior to that of MPR (84.0%), axial/MPR/3D (90.5%) and coronal images (86.1%). On the other hand, the diagnostic value of axial images was considered limited for orbital fractures region, with sensitivity of 44.2%.
Conclusions:
Except for the axial images, which presented a low sensitivity, all methods evaluated in this study showed high specificity and sensitivity for the diagnosis of orbital fractures according to the proposed methodology. This protocol can add valuable information to the diagnosis of fractures using the association of axial/MPR/3D with multislice CT.
Keywords: Orbital fractures, X-ray computed tomography, Computer-assisted diagnosis
INTRODUCTION
In trauma, therapeutic decisions about the best operative approach and the urgency and extension of the surgery are more difficult because there is not always information about the real range of the fracture20. Plain films have inadequate contrast between bone and soft tissue components to detect, describe and classify all types of fractures that may be present. Reliable imaging information is necessary to elucidate emergent injuries, to preoperatively plan reconstruction of functional areas and to guide the physical, psychological and social rehabilitation process10,14,16,21.
Multislice computed tomography (CT) represents a significant advance in the x-ray CT technology, with rapid table speeds and the real opportunity of shortening the time of data acquisition19.
The 64-slice CT scanner was launched during RSNA Meeting in 2004. This system is capable of doubling the amount of image data collected without increasing radiation dose and with a gantry rotation speed of 0.37 seconds. It has been demonstrated that multislice CT can provide a larger range of anatomic coverage during scanning7,9,12,25. It is possible to scan rapidly a large volume of interest, with high image quality, thin sections and a low artifact rating within a short time, thereby dramatically reducing respiratory motion problems7,9,12,19,25. The latest technology in computed tomography, with post-processing of CT scans to form multiplanar reconstruction (MPR) and 3D reconstruction images has increased the sensitivity and accuracy with which craniofacial fractures can be detected, allowing a more detailed analysis and interpretation. Three-dimensional imaging is intended to bridge the gap between radiology and surgery. Post processing of digital data acquired by CT scan imaging into 3D volumetric reformatted images or life-sized model has made quantitative preoperative surgical planning possible6,8. It has been shown to be useful for evaluation of maxillofacial fractures, especially when the surgeons can easily receive the 3D data from a workstation to the operation room simultaneously by a network connection, and developing a 3D real time model. 3D-CT reconstructions have been proved to be helpful in the evaluation of fracture comminution, displaced components and complex fractures involving multiple planes6.
The goal of this study was to assess the sensitivity and specificity of multislice computed tomography (CT) for diagnosis of orbital fractures following different protocols using an independent workstation
MATERIAL AND METHODS
CT images of 36 patients with maxillofacial fractures (symptomatic to orbit region) who were submitted to multislice CT scanning (Aquilion, Toshiba Medical Inc., Tustin, CA) were analyzed, retrospectively. CT data acquisition was performed by the following protocol: 1-mm thick slices, with 0.5-mm reconstruction interval in 8 slices by 0.5-second time, using 120 kVp and 150 mA, 512 X 512 matrix with FOV (field of view) 18, and standard filter for bone tissues.
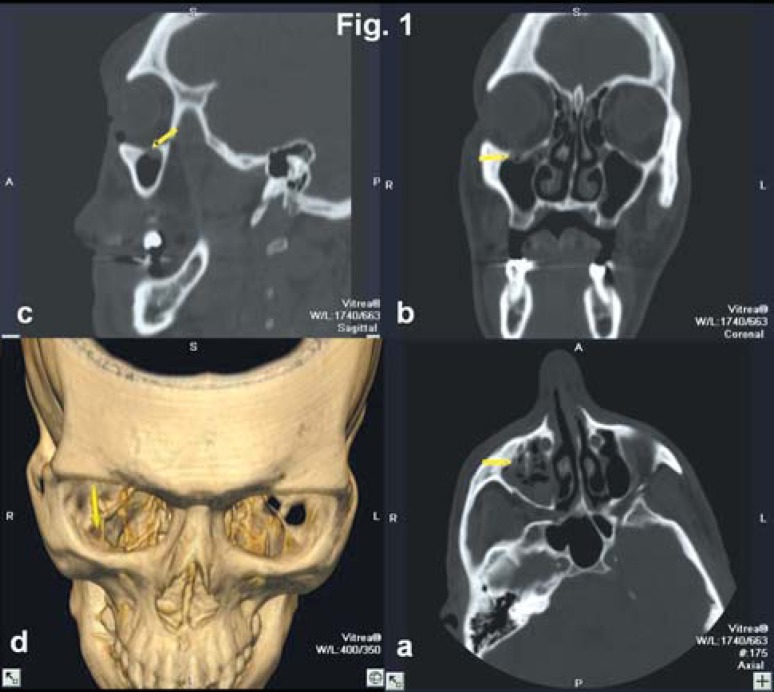
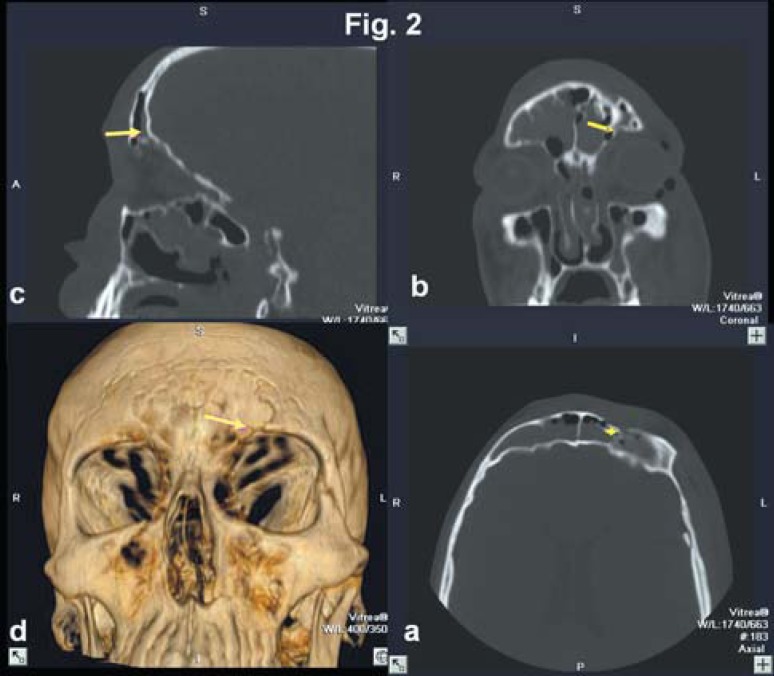
The original data were transferred to an independent workstation (Dell Precision 420 hardware, Windows NT) using Vitrea® software version 3.5.3 (Vital Images Inc., Plymouth, MN, USA) to generate an automatic and simultaneous multiplanar and 3D volume rendering reconstructed images (Figures 1 and 2). Subsequently, the images were processed, manipulated and interpreted in the workstation using the 3D software tools, such as bone protocol and transparency function that allowed the segmentation of the region of interest. Also, the "fly through" mode was used, which permitted visualization of the fractures in relationship to relevant anatomical points. The same parameters were used for all images, following the bone protocol for 3D image and bone window to axial and MPR images.
FIGURE 1. This sequence of images (axial (a), coronal (b), sagittal (c) and 3D-CT (d)), it may be observed an anterior inferior orbit wall fracture (arrows). An arrow is simultaneously pointed by the software in all the images. This fracture cannot be detect in axial image.
FIGURE 2. A case of fracture in the roof orbit in the anterior portion (arrows). The images are in sequence, as described in the protocol (axial (a), coronal (b), sagittal (c) and 3D-CT (d)). The site of fracture cannot be accurately distinguished in the axial image. The transparency feature and bone protocol were applied to the 3D-CT image, in order to facilitate the analysis.
The images were interpreted by two experienced examiners in 5 protocols, using an independent workstation: a) axial (original images), b) multiplanar reconstruction (MPR) (with analysis of coronal and sagittal views simultaneously), c) 3D images, d) association ofaxial/MPR/3D images (Figures 1 and 2) and e) coronal images. The analyses of the images were performed in a random order, in different sessions, in order to reach an agreement. The examiners were asked to judge whether they correctly identified different conditions, such as the sites of orbital fractures and their localization in each protocol. These sites were divided according to the orbital walls, as follows: lateral (with or without zygomatic frontal process fracture); medial; superior (roof) and inferior (anterior, medial). The clinical and/or surgical findings (medical records) were considered the gold standard corroborating the diagnosis of the anatomical localization in the orbital region.
Data were analyzed statistically using validity test. The sensitivity and specificity were quantified by checking the concordance of results with the gold standard, distinguishing false positives and false negatives for the orbital region.
In the application of Youden's J index, the sensitivity and specificity values of each method were combined, giving a score of validity by a mathematic calculation using the following equation: J (Youden's) = S (sensitivity) + E (specificity) – 100%24. The numeric values (Youden's J) were interpreted in order to help comparing the methods.
RESULTS
The validity (sensitivity and specificity) of the methods considering the specific sites of orbit: lateral with or without zygomatic frontal process, medial wall, superior (roof) and inferior (anterior and medial) walls are described on Table 1. Additionally, the reliability of the methods is demonstrated (positive and negative predictive values).
TABLE 1. Site-specific validity assessment of CT methods for the diagnosis of orbital fractures.
| AXIAL | Sensitivity | Specificity | Youden's J Statistic | Positive Predictive Value | Negative Predictive Value |
|---|---|---|---|---|---|
| Roof | 0.389 | 1.000 | 0.389 | 1.000 | 0.800 |
| Lateral | 0.886 | 0.722 | 0.609 | 0.886 | 0.722 |
| Zygomatic frontal process | 0.688 | 1.000 | 0.688 | 1.000 | 0.750 |
| Medial | 0.757 | 0.840 | 0.597 | 0.875 | 0.700 |
| Inferior Anterior | 0.029 | 1.000 | 0.029 | 1.000 | 0.443 |
| Inferior Medial | 0.088 | 0.964 | 0.053 | 0.750 | 0.466 |
| RMP | Sensitivity | Specificity | Youden's J Statistic | Positive Predictive Value | Negative Predictive Value |
| Roof | 0.667 | 0.977 | 0.644 | 0.923 | 0.878 |
| Lateral | 0.773 | 0.889 | 0.662 | 0.944 | 0.615 |
| Zygomatic frontal process | 0.750 | 0.933 | 0.683 | 0.923 | 0.778 |
| Medial | 0.811 | 0.880 | 0.691 | 0.909 | 0.759 |
| Inferior Ant | 0.914 | 0.963 | 0.877 | 0.970 | 0.897 |
| Inferior Med | 0.971 | 0.893 | 0.863 | 0.917 | 0.962 |
| 3D | Sensitivity | Specificity | Youden's J Statistic | Positive Predictive Value | Negative Predictive Value |
| Roof | 0.778 | 1.000 | 0.778 | 1.000 | 0.917 |
| Lateral | 0.727 | 1.000 | 0.727 | 1.000 | 0.600 |
| Zygomatic frontal process | 0.757 | 0.920 | 0.677 | 0.933 | 0.714 |
| Medial | 0.625 | 1.000 | 0.625 | 1.000 | 0.719 |
| Inferior Anterior | 0.943 | 0.926 | 0.869 | 0.943 | 0.926 |
| Inferior Medial | 0.853 | 0.964 | 0.817 | 0.967 | 0.844 |
| ASSOCIATION | Sensitivity | Specificity | Youden's J Statistic | Positive Predictive Value | Negative Predictive Value |
| Roof | 0.889 | 1.000 | 0.889 | 1.000 | 0.957 |
| Lateral | 0.932 | 0.944 | 0.876 | 0.976 | 0.850 |
| Zygomatic frontal process | 0.813 | 1.000 | 0.813 | 1.000 | 0.833 |
| Medial | 0.919 | 0.960 | 0.879 | 0.971 | 0.889 |
| Inferior Anterior | 0.943 | 0.963 | 0.906 | 0.971 | 0.929 |
| Inferior Medial | 0.912 | 0.929 | 0.840 | 0.939 | 0.897 |
| CORONAL | Sensitivity | Specificity | Youden's J Statistic | Positive Predictive Value | Negative Predictive Value |
| Roof | 0.667 | 1.000 | 0.667 | 1.000 | 0.880 |
| Lateral | 0.773 | 0.833 | 0.606 | 0.919 | 0.600 |
| Zygomatic frontal process | 0.813 | 1.000 | 0.813 | 1.000 | 0.833 |
| Medial | 0.892 | 0.960 | 0.852 | 0.971 | 0.857 |
| Inferior Anterior | 0.943 | 0.963 | 0.906 | 0.971 | 0.929 |
| Inferior Medial | 0.941 | 0.964 | 0.905 | 0.970 | 0.931 |
In each method, a variance (95% confidence interval) of sensibility was found according to the anatomic site of fracture. The values of specificity were almost constant and the differences were not significant statistically (p<0.05). In the axial method, a high value of sensitivity (0.886) was observed in lateral wall, while low sensitivity was observed in the inferior anterior wall (0.029). In the MPR method, high sensitivity was observed, for the inferior middle wall (0.971) while low sensibility was recorded for the roof (0.667). In the 3D method, the values were 0.943 for the inferior anterior wall and 0.625 for the medial wall (high and low sensitivity respectively). The best method was considered the association of axial/MPR/3D images, with high sensitivity values for all sites (0.813 to 0.943). The coronal method provided high sensitivity for the inferior anterior wall (0.943) and low sensitivity for the orbital roof (0.667).
We found the worst results of validity for the axial imaging with Youden's J statistical test (38.2%), while MPR and 3D methods showed 77.10% and 75.8%, respectively. The association of axial/MPR/3D images and the coronal method showed the best results (87.0% and 82.2% of validity, respectively) (Table 2).
TABLE 2. Validity assessment of CT methods for the diagnosis of fractures affecting all anatomic sites of the orbit.
| METHOD | Youden's J Statistic | Positive Predictive Value | Negative Predictive Value |
|---|---|---|---|
| Axial | 38.2% | 0.895 | 0.597 |
| MPR | 77.1% | 0.933 | 0.836 |
| 3D | 75.8% | 0.968 | 0.801 |
| Association | 87.0% | 0.968 | 0.899 |
| Coronal | 82.2% | 0.961 | 0.859 |
DISCUSSION
Nowadays, the capability of the modern scanners to acquire several slices simultaneously offers the decisive advantage of being able to achieve high volume scan speeds coupled with thin slice acquisition8,13. In this study with multislice CT, several aspects, such as resolution, speed, volume and power were improved. Comparisons of the preoperative condition with the postoperative outcomes were easier appreciated with axial/MPR/3D-CT protocol. Using an independent workstation, we were able to store, retrieve and review the images. In addition, at the same time that the exam was done, the images could be sent via Intranet to the members of the treatment team. With a powerful native toolset and a variety of automated distribution options, the interpretation process was simplified. MPR and 3D-CT reconstructed images were acquired from axial images, without exposing the patient to additional radiation dose.
Axial and coronal CT are adequate for diagnosis of medial orbital wall fractures. The superiority of coronal CT in the diagnosis of fractures of the orbital floor, blow-out fractures was confirmed, especially in patients who may develop diplopia or enophtalmos26. Generally, the original coronal images may be better for diagnosing orbital floor fracture detection, for adequate assessment of the cribiform plate, orbital roof, orbital floor and planum sphenoidale11. However, it cannot be applied on polytraumatized patients, who usually present with associated intracranial pathology or cervical vertebra fractures, limiting the examination3,17. For this reason, the problems in positioning such patients for CT scanning have been emphasized and axial multislice CT is recommended as the safest method under these circumstances. As Luka, et al.17 stated, the spiral CT technique using 1-mm slice thickness by 1 mm reconstruction interval allowed high 2D coronal imaging quality and represents a clinically effective way for detection of orbital floor fractures. As described in this paper, multiple overlapping slices could be reconstructed from a single examination allowing higher quality reconstructed images and facilitating the management of trauma patients.
According to previous studies, the association of MPR-CT and 3D-CT reconstructed images, with recent developments in computer graphics, enabled the radiologist to improve the visualization and to manipulate volumetric data readily, permitting an accurate application to maxillofacial region6,8.
Other studies have demonstrated the importance of axial and MPR-CT images as effective imaging methods for maxillary fractures1,2,6,10,11. In acute trauma cases, 3D-CT aided recognizing the position and the direction of fractures, the number of bone pieces and the amount of dislodgement2,22. In orbital fractures, this information is important in determining the need for surgical intervention and for choosing the correct approach and osteosynthesis method13,15,23. In our comparative validation by anatomical study, we consider imaging protocols to be the principal concern5. Multislice CT imaging is useful for assessing the severity of mid-face injuries. The interpretation of these images has been studied and proposed to search many anatomic structures and to define criteria for planning treatment in patients with orbital fractures. Furthermore, 3D-CT was reported to faithfully reproduce osseous structures, providing complete inspection of the reproduced structure from any viewpoint (including internal inspection), to enable understanding of anatomy, and to aid the evaluation of the operative results for craniofacial surgery18.
In the present study, the comparison of the sensitivity of the methods to detect orbital fractures showed that 3D-CT presented sensitivity of 78.9%, which was not superior to MPR (84.0%), association of axial/MPR/3D methods (90.5%) or coronal images (86.1%). The diagnostic value of axial images was considered limited for orbital fractures in this study, with sensitivity of 44.2%.
Ohkawa, et al.22 (1997) reported that both 2D-CT and 3D-CT techniques presented a similar sensitivity for the diagnosis of fractures in the mandibular region, though 3D-CT imaging allowed a better visualization. Rhea, et al.23 (1999) and Carls, et al.4 (1994) also observed that 3D images provided an easy detection of specific characteristics of facial asymmetries, midface defects and skull vault defects, and a clear localization of fractures associated with extensive bone displacement. In the present study, we interpreted the images using a spiral CT from an independent workstation. Thus, it was possible to improve the validity of 2D-CT examinations using the association of methods (axial/MPR/3D). The analysis of our results showed that the association of images had a sensitivity of 90.5%.
According to Mayer, et al.18 (1988), multiple frontal and nasal bone fractures can be observed on axial images. However, the extent of comminutive fractures is better demonstrated on 3D-CT scans, where the size, shape, and displacement of individual fragments are clearly revealed2,15,19. In agreement with these authors, we found low sensitivity for the axial method for the analysis of fractures in the orbit region (44.2%). On the other hand, when we interpreted 3D images, the sensitivity was 78.9%. Also, the association of images presented high sensitivity (90.5%), demonstrating the validity of the combination of methods.
In conclusion, except for the axial images, which presented a low sensitivity, all methods evaluated in this study showed high specificity and sensitivity for the diagnosis of orbital fractures according to the proposed methodology. This protocol can add valuable information to the diagnosis of fractures using the association of axial/MPR/3D with multislice CT. However, we believe that improvements in advanced CT techniques might continue expanding the role of 3D imaging.
ACKNOWLEDGEMENTS
We would like to thank Professor José Leopoldo Ferreira Antunes, PhD from the Department of Social Dentistry, University of São Paulo for performing the statistical analysis, and CAPES (Dr. Denise Santos) for providing the PhD fellowship, Brasilia, Brazil.
REFERENCES
- 1.Alder ME, Deahl ST, Matteson SR. Clinical usefulness of two-dimensional reformatted and three-dimensionally rendered computerized tomographic images: literature review and a survey of surgeons' opinions. J Oral Maxillofac Surg. 1995;53(4):375–386. doi: 10.1016/0278-2391(95)90707-6. [DOI] [PubMed] [Google Scholar]
- 2.Altobelli DE, Kikinis R, Mulliken JB, Cline H, Lorensen W, Jolesz F. Computer-assisted three-dimensional planning in craniofacial surgery. Plast Reconstr Surg. 1993;92(4):576–585. discussion 586-7. [PubMed] [Google Scholar]
- 3.Buitrago-Tellez CH, Schilli W, Bohnert M, Alt K, Kimmig M. A comprehensive classification of craniofacial fractures: postmortem and clinical studies with two- and three-dimensional computed tomography. Injury. 2002;33(8):651–668. doi: 10.1016/s0020-1383(02)00119-5. [DOI] [PubMed] [Google Scholar]
- 4.Carls FR, Schuknecht B, Sailer HF. Value of three-dimensional computed tomography in craniomaxillofacial surgery. J Craniofac Surg. 1994;5(5):282–288. doi: 10.1097/00001665-199411000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Cavalcanti MGP, Haller JW, Vannier MW. Three-dimensional computed tomography landmark measurement in craniofacial surgical planning: experimental validation in vitro. J Oral Maxillofac Surg. 1999;57(6):690–694. doi: 10.1016/s0278-2391(99)90434-2. [DOI] [PubMed] [Google Scholar]
- 6.Cavalcanti MGP, Panella J, Santos DT, Vannier MW, Costa e Silva APA. In: Interpretation of craniofacial fractures using multislice CT: establishing a protocol. Lemke H, Inamura K, Doi K, Vannier M, Farman A, Reiber J, editors. Chicago: Elsevier; 2004. pp. 1215–1219. [Google Scholar]
- 7.Donnelly LF, Frush DP, Nelson RC. Multislice helical CT to facilitate combined CT of the neck, chest, abdomen, and pelvis in children. AJR Am J Roentgenol. 2000;174(6):1620–1622. doi: 10.2214/ajr.174.6.1741620. [DOI] [PubMed] [Google Scholar]
- 8.Dos Santos DT, Costa e Silva AP, Vannier MW, Cavalcanti MGP. Validity of multislice computerized tomography for diagnosis of maxillofacial fractures using an independent workstation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98(6):715–720. doi: 10.1016/j.tripleo.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Flohr T, Stierstorfer K, Bruder H, Simon J, Polacin A, Schaller S. Image reconstruction and image quality evaluation for a 16-slice CT scanner. Med Phys. 2003;30(5):832–845. doi: 10.1118/1.1562168. [DOI] [PubMed] [Google Scholar]
- 10.Fox LA, Vannier MW, West OC, Wilson AJ, Baran GA, Pilgram TK. Diagnostic performance of CT, MPR and 3DCT imaging in maxillofacial trauma. Comput Med Imaging Graph. 1995;19(5):385–395. doi: 10.1016/0895-6111(95)00022-4. [DOI] [PubMed] [Google Scholar]
- 11.Hoeffner EG, Quint DJ, Peterson B, Rosenthal E, Goodsitt M. Development of a protocol for coronal reconstruction of the maxillofacial region from axial helical CT data. Br J Radiol. 2001;74(880):323–327. doi: 10.1259/bjr.74.880.740323. [DOI] [PubMed] [Google Scholar]
- 12.Hu H, He HD, Foley WD, Fox SH. Four multidetector-row helical CT: image quality and volume coverage speed. Radiology. 2000;215(1):55–62. doi: 10.1148/radiology.215.1.r00ap3755. [DOI] [PubMed] [Google Scholar]
- 13.Kloppel R, Schreiter D, Dietrich J, Josten C, Kahn T. Early clinical management after polytrauma with 1 and 4 slice spiral CT. Radiologe. 2002;42(7):541–546. doi: 10.1007/s00117-002-0764-8. [DOI] [PubMed] [Google Scholar]
- 14.Laine JL, Conway WF, Laskin DM. Radiology of maxillofacial trauma. Curr Probl Diagn Radiol. 1993;22:145–188. doi: 10.1016/0363-0188(93)90019-p. [DOI] [PubMed] [Google Scholar]
- 15.Lakits A, Prokesch R, Scholda C, Bankier A. Orbital helical computed tomography in the diagnosis and management of eye trauma. Ophthalmology. 1999;106(12):2330–2335. doi: 10.1016/S0161-6420(99)90536-5. [DOI] [PubMed] [Google Scholar]
- 16.Lo LJ, Marsh JL, Vannier MW, Patel VV. Craniofacial computer-assisted surgical planning and simulation. Clin Plast Surg. 1994;21(4):501–516. [PubMed] [Google Scholar]
- 17.Luka B, Brechtelsbauer D, Gellrich NC, Konig M. 2D and 3D CT reconstructions of the facial skeleton: an unnecessary option or a diagnostic pearl? Pt 2Int J Oral Maxillofac Surg. 1995;24(1):76–83. doi: 10.1016/s0901-5027(05)80866-5. [DOI] [PubMed] [Google Scholar]
- 18.Mayer JS, Wainwright DJ, Yeakley JW, Lee KF, Harris JH, Jr, Kulkarni M. The role of three-dimensional computed tomography in the management of maxillofacial trauma. J Trauma. 1988;28(7):1043–1053. doi: 10.1097/00005373-198807000-00022. [DOI] [PubMed] [Google Scholar]
- 19.McCollough CH, Zink FE. Performance evaluation of a multi-slice CT system. Med Phys. 1999;26(11):2223–2230. doi: 10.1118/1.598777. [DOI] [PubMed] [Google Scholar]
- 20.Nortjé CJ, Farman AG, Wood RE. Traumatic Injuries. 1. ed. Saint Louis: Mosby; 1993. Oral and maxillofacial diagnostic imaging; pp. 158–180. [Google Scholar]
- 21.Novelline RA, Rhea JT, Rao PM, Stuk JL. Helical CT in emergency radiology. Radiology. 1999;213(2):321–339. doi: 10.1148/radiology.213.2.r99nv01321. [DOI] [PubMed] [Google Scholar]
- 22.Ohkawa M, Tanabe M, Toyama Y, Kimura N, Uematsu K, Satoh G. The role of three-dimensional computed tomography in the management of maxillofacial bone fractures. Acta Med Okayama. 1997;51(4):219–225. doi: 10.18926/AMO/30760. [DOI] [PubMed] [Google Scholar]
- 23.Rhea JT, Rao PM, Novelline RA. Helical CT and three-dimensional CT of facial and orbital injury. Radiol Clin North Am. 1999;37(3):489–513. doi: 10.1016/s0033-8389(05)70108-1. [DOI] [PubMed] [Google Scholar]
- 24.Szklo M, Javier-Nieto F. Epidemiology: beyond the basics. Gaithersburg: Aspen; 2000. [Google Scholar]
- 25.Taguchi K, Anno H. High temporal resolution for multislice helical computed tomography. Med Phys. 2000;27(5):861–872. doi: 10.1118/1.598951. [DOI] [PubMed] [Google Scholar]
- 26.Tanrikulu R, Erol B. Comparison of computed tomography with conventional radiography for midfacial fractures. Dentomaxillofac Radiol. 2001;30(3):141–146. doi: 10.1038/sj/dmfr/4600593. [DOI] [PubMed] [Google Scholar]