Abstract
Objectives:
The purpose of this study was to evaluate the Vickers hardness number (VHN) and the in vitro marginal adaptation of inlay restorations of three hybrid composite resins (Filtek Z250, Opallis and Esthet-X) subjected to two post-cure treatments.
Material and Methods:
For the microhardness test, three different groups were prepared in accordance with the post-cure treatments: control group (only light cure for 40 s), autoclave group (light cure for 40 s + autoclave for 15 min at 130°C); and microwave group (light cure for 40 s + microwave for 3 min at 450 W). To assess the marginal adaptation, the composite resin was inserted incrementally into a mesial-occlusal-distal cavity brass mold and each increment light-cured for 40 s. A previous reading in micrometers was taken at the cervical wall, using a stereomicroscope magnifying glass equipped with a digital video camera and image-analysis software. Subsequently, the specimens were subjected to the post-cure treatments (autoclave and microwave) and a reading was taken again at the cervical wall. Data were compared using ANOVA for the hardness test, split-plot ANOVA for the adaptation assessment and Tukey's test for multiple comparisons. A significance level of 5% was adopted for all analyses.
Results:
The post-cure treatments increased the hardness of conventional composites (p<0.001) and the gap values of inlay restorations (p<0.01). Filtek Z250 showed higher hardness (p<0.001) and lower gap values than Opallis and Esthet-X (p<0.05). Gap values did not exceed 90 μm for any of the experimental conditions.
Conclusion:
The post-cure treatments increased the VHN and the gap values on the cervical floor of composite resin inlays. Moreover, Filtek Z250 showed the best results, with higher hardness and lower gap values.
Keywords: Composite resins, Inlays, Cure, Hardness, Marginal adaptation
INTRODUCTION
The great demand of patients for tooth-colored restorations or metal-free restorations and the improvements in the physical properties of composite resins have increased the indications of these materials for esthetic restorations. Nowadays, indirect composite resin inlay and onlay restorations are extensively used in esthetic treatments as a less expensive and less technique-sensitive alternative to ceramic crowns3. Moreover, the indirect technique improves the control of marginal adaptation, proximal contacts, anatomic form and polymerization shrinkage, compared to the direct composite resin technique30. Consequently, indirect composite resin restorations have shown less microleakage at the tooth-restoration interface than direct composite resins25.
The direct composite resin inlay/onlay technique was introduced to improve the adaptation in Class II cavities1, being less expensive than indirect ones and easily built up clinically. In this technique, the composite resin is first light-cured directly in the inlay cavity and then the inlay is removed from the cavity and post-cured. Extra-oral cure, which may occur under light, heat and/or pressure, increases the degree of conversion of dental composites, producing significant improvements in their mechanical and physical properties, such as hardness, elastic modulus, flexural strength, stiffness, hygroscopic expansion and solubility10,18,20,27. However, Peutzfeldt and Asmussen17 (1991) did not find these results for all composite resins evaluated in their study.
When direct inlays are fabricated, direct composite resins are used instead of ceromer materials, reducing the final treatment costs7. The mechanical properties of composites are comparable or superior to those of ceromers26. The higher degree of conversion caused by the secondary cure in the direct inlay technique can lead to greater polymerization shrinkage2 and, consequently, the marginal adaptation could be compromised28. Directly fabricated inlays have demonstrated good marginal integrity29 and are more accurate as regards gap formation than indirectly fabricated inlays16, particularly when the cervical margin is in dentin25.
After secondary cure, the inlay/onlay restoration is luted into place with composite resin luting materials. Therefore, the shrinkage is limited to the cement layer. However, the resin luting agents have some limitations, such as high shrinkage and low resistance to wear22. If the adaptation is poor, the resin cement layer will not be thin enough, and the longevity of the indirect restoration could be influenced19,22.
The purpose of this study was to evaluate the effects of two different post-cure treatments on the Vickers hardness number (VHN) and marginal adaptation of composite resin inlay restorations.
MATERIAL AND METHODS
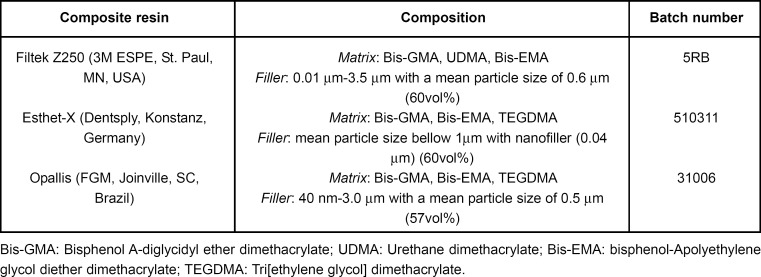
The main characteristics of the three composites evaluated in this study (Esthet-X/Dentsply, Filtek Z250/3M and Opallis/FGM) are presented in Figure 1.
FIGURE 1. Composition of the composite resins evaluated in the study.
For the Vickers hardness test, two 2-mm-thick composite resin increments were inserted into a conical brass mold (3 and 4 mm diameter and 4 mm high), each one being light-cured for 40 s with a halogen light-curing unit (Optilux 501; Demetron/Kerr, Danbury, CT, USA, output 490 mw/cm2). Light unit irradiance was monitored using a radiometer (model 100, Demetron/Kerr). Fifteen specimens were made for each composite resin and divided into three experimental groups, in accordance with the post-cure treatments: control group (no post-cure treatment); autoclave group: the specimens were maintained during 15 min under 2.0 kgf / cm2 and 130 ± 1°C in an autoclave (BIOS 19L; Dabi Atlante, Ribeirão Preto, SP, Brazil); microwave group: the specimens were treated for 3 min under medium power of 450 W in a domestic microwave oven (MB6544W, Samsung, Korea). The specimens were embedded in PVC tubes using epoxy resin (Trok-Dente, Prodens, RJ, Brazil) and were polished with 220-, 400-, 600- and 1200-grit abrasive papers and felt discs using diamond paste (Arotec, SP, Brazil) in a polishing machine (DPU-10, Struers, Copenhagen, Denmark). After 24 h of storage in distilled water, three indentations for VHN assessment (2003, Büehler, Lake Bluff, IL, USA) were performed in each specimen, under 50 g load and 15 s dwell time. The mean of the three measurements for each specimen was calculated and subjected to statistical analysis by two-way ANOVA and Tukey's test at 5% significance level.
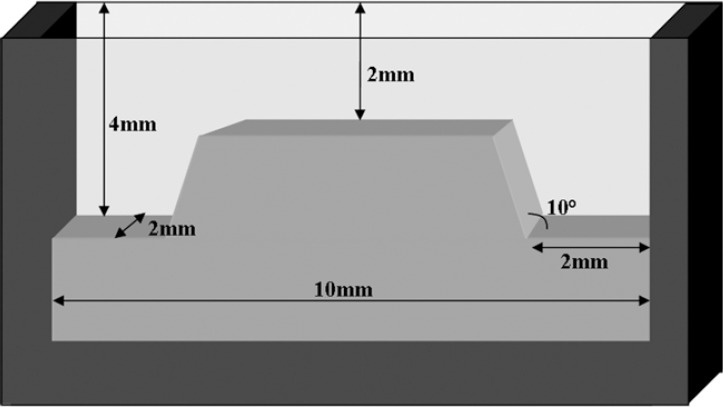
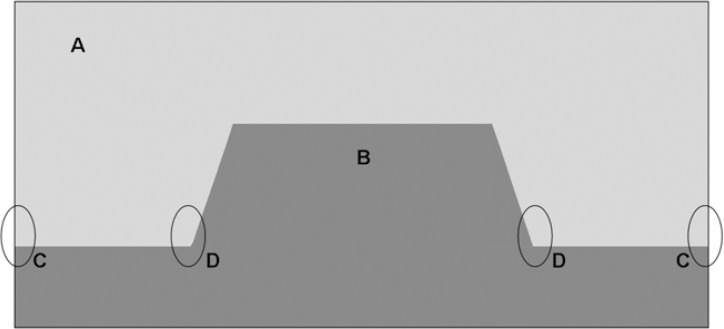
For marginal adaptation assessment, 2-mm-thick composite resin increments were inserted into a brass mold that simulated a mesial-occlusal-distal cavity. The dimensions and shape of the mold are shown in Figure 2. Each increment was light-cured for 40 s with the halogen light-curing unit (Optilux 501; Demetron/Kerr) and light unit irradiance was also monitored, as mentioned before. Ten specimens were made for each composite. After replacing the specimens in the brass mold, a monochrome charge-coupled device (CCD) video camera (TA-0123 Opton, Hexasystems, SP, Brazil) captured the images of the inlay restorations under a stereomicroscope magnifying glass (PZO, Metrimpex, Hungary) at ×10 magnification. These images were transferred to an IBM-compatible personal computer for quantitative assessment in micrometers of marginal adaptation at four points (Figure 3), using Image1.36 image-analysis software (National Institute of Health, Bethesda, MD, USA). Two points were located at the cervical margin (mesial and distal) and two points at the internal angles (mesial-cervical-axial and distal-cervical-axial). After removing the specimens from the mold, they were divided into two experimental groups, in accordance with the post-cure treatments: autoclave group and microwave group, which were described previously. The specimens were replaced again into the brass mold and the cervical adaptation was measured again, using the stereomicroscope, as mentioned above. The mean of the four measurements was calculated for each specimen. Data were analyzed by split-plot ANOVA and Tukey's test at 5% significance level.
FIGURE 2. Dimensions and shape of the standard inlay cavity.
FIGURE 3. Gap measurement points: (A) composite resin; (B) brass mold; (C) cervical margin (mesial and distal); (D) internal angles (cervical-axial, mesial and distal).
RESULTS
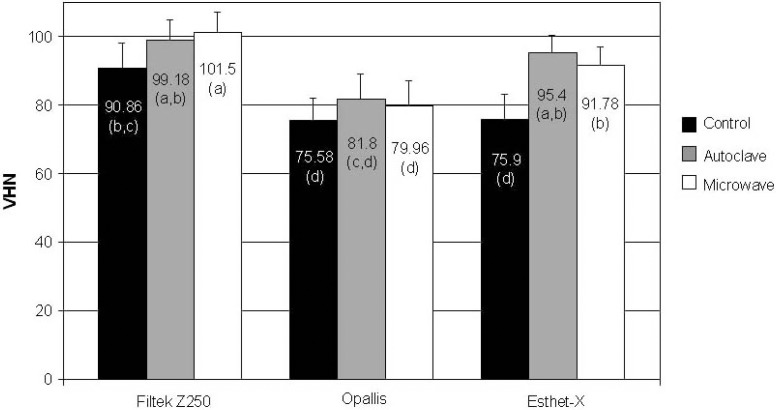
Figure 4 and Table 1 present the means and standard deviation of the VHN and gap width values as a function of the post-cure treatments.
FIGURE 4. Mean and standard deviation of the VHN for each material and post-cure treatment. Different lower case letters show statistically significant diferences.
TABLE 1. Mean, standard deviation, minimum and maximum of gap values (μm).
| Composite resin | Post-cure treatment | |||
|---|---|---|---|---|
| Before | After | Minimum | Maximum | |
| Filtek Z250 | 13.02 [11.64]a,A | 19.69 [15.87]b,A | 0 | 61.36 |
| Opallis | 23.95 [11.19]a,B | 32.68 [13.31]b,B | 5.48 | 64.85 |
| Esthet-X | 22.56 [15.50]a,B | 32.74 [18.07]b,B | 0 | 81.46 |
Different lowercase letters in the rows and uppercase letter in the columns indicate statistically significant difference.
Regarding Vickers hardness analysis, ANOVA showed that the VHN was significantly affected by the composite materials (p<0.001) and the post-cure treatments (p<0.001). The highest VHN was found for Filtek Z250, followed by the Esthet-X and Opallis. Moreover, all post-cure treatments increased the VHN when compared to the control group, though without statistically significant difference (p>0.05) between them. For Opallis, neither autoclave nor microwave was able to increase the VHN (Figure 4). For Esthet-X, both post-cure treatments, increased the VHN (p<0.01), whereas for Filtek Z250, only the microwave group showed higher VHN, when compared with the control group (p<0.01).
Regarding the adaptation assessment, split-plot ANOVA showed that the composite materials and the post-cure treatments influenced the gap width values. The lowest width gap values (Table 1) were found for the inlay restorations that were not subjected to any post-cure treatment (p<0.001). No statistically significant difference was found between the two experimental groups (autoclave or microwave). Filtek Z250 showed significantly (p<0.05) lower gap values (Table 1) than Opallis and Esthet-X.
DISCUSSION
It is well known that, at room temperature, the conversion of composite resin C=C bonds is not complete23, ranging between 48 and 60%8,24. For indirect resin restorations, additional cure procedures have been used to increase the degree of conversion, improving the mechanical properties18. With secondary cure the chain vibration amplitude is increased allowing free radicals and methacrylate groups to collide and establish covalent links, increasing the degree of conversion21. It has been shown that the hardness of composites correlates well with degree of conversion6. In the present study, the post-cure treatments improved the VHN. This result is in agreement with those of other authors10,27.
If the VHN had increased, the degree of conversion might be higher, leading to greater cure shrinkage and, consequently, poor marginal adaptation. In the present study, the gap values on the cervical floor increased with the postcure treatments, also indicating a higher degree of conversion. Gap values under 90 μm were found for all experimental conditions (Table 1). Schmalz, et al.22 found that with a luting space of up to 100 μm, the width of the luting space has no influence on the marginal integrity.
The adaptation was evaluated directly in the brass mold, mimicking the clinical conditions for the direct composite resin inlay/onlay technique, since no impression was taken. When the marginal and overall adaptation of inlays was observed by using the silicon replica technique, gap values over 100 μm were found15. For this technique, the impression material, the stone and the silicone fitness-checking could have some influence on the gap formation between cavity walls and inlays. The use of silicon impression has never been considered adequate to exactly replicate the behavior of dental cement in the clinical situation19.
Although Opallis and Esthet-X had shown similar VHN for the control group, they showed lower VHN than Filtek Z250, corroborating finding of Correr, et al.4 (2005) for Esthet-X composite. As their manufacturers propose a longer working time, it can be speculated that a diminished content of photoinitiators might be present, leading to a lower degree of conversion and a lower VHN with the cure protocol used in the present study. Therefore, with the secondary cure by microwave or autoclave, the network would have higher mobility, improving the cure and, consequently, the VHN. This factor was statistically significant for Esthet-X, which showed an increase of 20.9% to 25% with both post-cure treatments (microwave and autoclave), but not for Opallis. However, the VHN for Opallis increased about 8.2% for the autoclave group and 5.8% for the microwave group, indicating an improvement in VHN with the post-cure treatments. In a previous study5, after 1-week storage, an additional light exposure also increased the VHN for Esthet-X.
For Filtek Z250, VHN also tended to increase (9.8%) when the samples were autoclaved and there was a significant difference (11.7% increase) between the control and microwave groups (Figure 3). Other authors have suggested that the faster cure rate of the Z100 might be caused by its high content of photoinitiators9,12. Although the technical profiles of 3M ESPE do not specify the content of photoinitiators in their composites and neither the aforementioned studies nor the present study made this evaluation in the tested materials, it can be hypothesize that, since Filtek Z250 was developed from Filtek Z100 (Technical Product Profile, 3M ESPE), a higher level of photoinitiators might be present in both materials, explaining the higher degree of conversion and, consequently, the higher VHN shown for Filtek Z250 (Figure 3). Supporting this statement, Hofmann, et al.13 (2002) attributed the faster cure reaction of Filtek Z250 to the high efficiency of the photoactivation system of this material.
Still following the same thought, if the degree of conversion before the post-cure treatments was very high for Filtek Z250, the mobility of the network would be more difficult11 during the post-cure treatments, leading to a lower extent of post-cure (9.8-11.7%), when compared to Esthet-X. These speculations could also explain the best adaptation on the cervical floor for Z250 (p<0.05). If its conversion with the post-cure treatment were lower, its polymerization shrinkage would also be lower, leading to the formation of smaller gaps. The very low content of TEGDMA in Filtek Z2508, a smaller molecular size monomer, might also explain the best adaptation for this material, as it could be expected a lower shrinkage than that for Opallis and Esthet-X.
Since there was no significant difference between autoclave and microwave groups, it can be emphasized that both treatments were efficient for enhancing the VHN, which is in agreement with Soares, et al.26 (2005) Furthermore, after the secondary cure, the gap values were higher but similar for both groups. Others studies also verified an improvement in the degree of conversion when light was used in conjunction with heat and pressure8,14,24.
Within the limitations of this in vitro study, the postcure treatments for the tested composites were efficient in increasing the VHN, without significantly compromising the marginal adaptation of the inlay restorations, as gap values did not exceed 90 μm. Therefore, in wide Class II cavities, the lower cost of the direct composite resin inlay/onlay, as well as being less time-consuming technique, would be an advantage. Additional clinical studies are necessary to analyze the cervical adaptation, marginal leakage and wear resistance, confirming the efficiency of this technique.
CONCLUSIONS
Based on the methodology of the present study, it may be conclude that: 1. The post-cure treatment with autoclave or microwave increased the VHN and the gap values on the gingival floor of composite resin inlays; 2. Filtek Z250 showed the highest VHN and the best marginal adaptation of all composites.
ACKNOWLEDGEMENTS
The authors would like to thank the PIBIC/CNPq for finacial support.
REFERENCES
- 1.Blankenau RJ, Kelsey WP, 3rd, Cavel WT. A direct posterior restorative resin inlay technique. Quintessence Int Dent Dig. 1984;15(5):515–516. [PubMed] [Google Scholar]
- 2.Calheiros FC, Braga R, Kawano Y, Ballester RY. Relationship between contraction stress and degree of conversion in restorative composites. Dent Mater. 2004;20(10):939–946. doi: 10.1016/j.dental.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 3.Chalifoux PR. Restoration of endodontically treated teeth: review, classification and post design. Pract Periodontics Aesthet Dent. 1998;109(2):247–254. [PubMed] [Google Scholar]
- 4.Correr AB, Sinhoreti MA, Correr L, Sobrinho, Tango RN, Schneider LF, Consani S. Effect of increase of energy density on Knoop hardness of dental composites light-cured by conventional QTH, LED and xenon plasma arc. Braz Dent J. 2005;16(3):218–224. doi: 10.1590/s0103-64402005000300009. [DOI] [PubMed] [Google Scholar]
- 5.De Jong LC, Opdam NJ, Bronkhorst EM, Roeters JJ, Wolke JG, Geitenbeek B. The effectiveness of different polymerization protocols for class II composite resin restorations. J Dent. 2007;35(6):513–520. doi: 10.1016/j.jdent.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 6.DeWald JP, Ferracane JL. A comparison of four modes of evaluating depth of cure light activated composites. J Dent Res. 1987;66(3):727–730. doi: 10.1177/00220345870660030401. [DOI] [PubMed] [Google Scholar]
- 7.Duke ES. The introduction of a new class of composite resins ceromers. Compend Contin Educat Dent. 1999;20(3):246–247. [PubMed] [Google Scholar]
- 8.Emami N, Soderholm KJ. How light irradiance and curing time affect monomer conversion in light-cured resin composites. Eur J Oral Sci. 2003;111(6):536–542. doi: 10.1111/j.0909-8836.2003.00082.x. [DOI] [PubMed] [Google Scholar]
- 9.Ernst CP, Kürschner R, Rippin G, Willershausen B. Stress reduction in resin-based composites cured with a two-step light-curing unit. Am J Dent. 2000;13(2):69–72. [PubMed] [Google Scholar]
- 10.Ferracane JL, Condon JR. Post-cure heat treatments for composites: properties and fractography. Dent Mater. 1992;8(5):290–295. doi: 10.1016/0109-5641(92)90102-i. [DOI] [PubMed] [Google Scholar]
- 11.Halvorson RH, Erickson RL, Davidson CL. Energy dependent polymerization of resin-based composite. Dent Mater. 2002;18(6):463–469. doi: 10.1016/s0109-5641(01)00069-0. [DOI] [PubMed] [Google Scholar]
- 12.Hasegawa T, Itoh K, Yukitani W, Wakumoto S, Hisamitsu H. Effects of soft-start irradiation on the depth of cure and marginal adaptation to dentin. Oper Dent. 2001;26(4):389–395. [PubMed] [Google Scholar]
- 13.Hofmann N, Hugo B, Klaiber B. Effect of irradiation type (LED or QTH) on photo-activated composite shrinkage strain kinects, temperature rise and hardness. Eur J Oral Sci. 2002;110(6):471–479. doi: 10.1034/j.1600-0722.2002.21359.x. [DOI] [PubMed] [Google Scholar]
- 14.Kakaboura A, Rahiotis C, Zinelis S, Al-Dhamadi YA, Silikas N, Watts DC. In vitro characterization of two laboratory-processed resin composites. Dent Mater. 2003;19(5):393–398. doi: 10.1016/s0109-5641(02)00082-9. [DOI] [PubMed] [Google Scholar]
- 15.Karakaya S, Sengun A, Ozer F. Evaluation of internal adaptation in ceramic and composite resin inlays by silicon replica technique. J Oral Rehabil. 2005;32(6):448–453. doi: 10.1111/j.1365-2842.2005.01443.x. [DOI] [PubMed] [Google Scholar]
- 16.Peutzfeldt A, Asmussen E. A comparison of accuracy in seating and gap formation for three inlay/onlay techniques. Oper Dent. 1990;15(4):129–135. [PubMed] [Google Scholar]
- 17.Peutzfeldt A, Asmussen E. Mechanical properties of three composite resins for the inlay/onlay technique. J Prosthet Dent. 1991;66(3):322–324. doi: 10.1016/0022-3913(91)90257-w. [DOI] [PubMed] [Google Scholar]
- 18.Peutzfeldt A, Asmussen E. The effect of postcuring on quantity of remaining double bonds, mechanical properties and in vitro wear of two resin composites. J Dent. 2000;28(6):447–452. doi: 10.1016/s0300-5712(00)00021-x. [DOI] [PubMed] [Google Scholar]
- 19.Qualtrough AJ, Piddock V, Kypreou V. A comparison of two in vitro methods for assessing the fitting accuracy of composite inlays. Br Dent J. 1993;174(12):450–454. doi: 10.1038/sj.bdj.4808196. [DOI] [PubMed] [Google Scholar]
- 20.Reinhardt JW, Boyer DB, Stephens NH. Effects of secondary curing on indirect posterior composite resins. Oper Dent. 1994;19(6):217–220. [PubMed] [Google Scholar]
- 21.Rueggeberg FA, Ergle JW, Lockwood PE. Effect of photoinitiator level on properties of a light-cured and post-cure heated model resin system. Dent Mater. 1997;13(6):360–364. doi: 10.1016/s0109-5641(97)80107-8. [DOI] [PubMed] [Google Scholar]
- 22.Schmalz G, Federlin M, Reich E. Effect of dimension of luting space and luting composite on marginal adaptation of a class II ceramic inlay. J Prosthet Dent. 1995;73(4):392–399. doi: 10.1016/s0022-3913(05)80337-3. [DOI] [PubMed] [Google Scholar]
- 23.Sideridou I, Tserki V, Papanastasiou G. Effect of chemical structure on degree of conversion in light-cured dimethacrylate-based dental resins. Biomaterials. 2002;23(8):1819–1829. doi: 10.1016/s0142-9612(01)00308-8. [DOI] [PubMed] [Google Scholar]
- 24.Silva GRD, Simamoto PC, Jr, Mota AS. Mechanical properties of light-curing composites polymerized with different laboratory photo-curing units. Dent Mater J. 2007;26(2):217–223. doi: 10.4012/dmj.26.217. [DOI] [PubMed] [Google Scholar]
- 25.Soares CJ, Celiberto L, Dechichi P, Fonseca RB, Martins LRM. Marginal integrity and microleakage of direct and indirect composite inlays – SEM and stereomicroscopic evaluation. Braz Oral Res. 2005;19(4):295–301. doi: 10.1590/s1806-83242005000400011. [DOI] [PubMed] [Google Scholar]
- 26.Soares CJ, Pizi EC, Fonseca RB, Martins LRM. Mechanical properties of light cured composites polymerized with several additional post-curing methods. Oper Dent. 2005;30(3):389–394. [PubMed] [Google Scholar]
- 27.Takeshige F, Kinomoto Y, Torii M. Additional heat-curing of light-cured composite resin for inlay restoration. J Osaka Univ Dent Sch. 1995;35:59–66. [PubMed] [Google Scholar]
- 28.Tarle Z, Meniga A, Knezevic A, Sutalo J, Ristic M, Pichler G. Composite conversion and temperature rise using a conventional, plasma arc, and experimental blue LED curing unit. J Oral Rehabil. 2002;29(7):662–667. doi: 10.1046/j.1365-2842.2002.00866.x. [DOI] [PubMed] [Google Scholar]
- 29.Van DijKen JW, Hörstedt P. Marginal breakdown of 5-year-old direct composite inlays. J Dent. 1996;24(6):389–394. doi: 10.1016/0300-5712(95)00098-4. [DOI] [PubMed] [Google Scholar]
- 30.Wassel RW, Walls AW, McCabe JF. Direct composite inlays versus conventional composite restorations: three-year clinical results. Br Dent J. 1995;179(9):343–349. doi: 10.1038/sj.bdj.4808919. [DOI] [PubMed] [Google Scholar]