Abstract
Objective:
The objective of this study was to compare the pain levels on opposite sides of the maxilla at needle insertion during delivery of local anesthetic solution and tooth preparation for both conventional and anterior middle superior alveolar (AMSA) technique with the Wand computer-controlled local anesthesia application.
Material and methods:
Pain scores of 16 patients were evaluated with a 5-point verbal rating scale (VRS) and data were analyzed nonparametrically. Pain differences at needle insertion, during delivery of local anesthetic, and at tooth preparation, for conventional versus the Wand technique, were analyzed using the Mann-Whitney U test (p=0.01).
Results:
The Wand technique had a lower pain level compared to conventional injection for needle insertion (p<0.01). In the anesthetic delivery phase, pain level for the Wand technique was lower (p<0.01). However, there was no difference between the Wand and conventional technique for pain level during tooth preparation (p>0.05).
Conclusions;
The AMSA technique using the Wand is recommended for prosthodontic treatment because it reduces pain during needle insertion and during delivery of local anaesthetic. However, these two techniques have the same pain levels for tooth preparation.
Keywords: Maxillary local anesthesia, AMSA, Wand
INTRODUCTION
Local anesthesia and pain control is one of the most important elements of dentistry, and particularly prosthetic dentistry. According to the American Dental Association, fear of pain is the most important factor preventing patients from visiting their dentists. Different kinds of fear related to previous clinical experience affect patients' attitudes to local anesthesia or dentist20. Although local anesthesia techniques do not provide pain-free treatment, this pain is generally tolerable. Pain can result from the mechanical trauma of needle introduction into the site of injection, or from the sudden distension of the tissues, resulting from a rapid discharge of the contents of the syringe. Pain can also be caused by the stimulation of the first few drops of the local anaesthetic3,14. Contrary to prevalent ideas, needle penetration of tissue is not the primary reason for discomfort. Volume and pressure of the local anesthetic being injected causes more distress and/or pain. Administering local anesthetic injection may not only provoke anxiety in patients, but also in the dentist29. Despite that, administering local anesthesia by injection for pain relief is still the most common method used in dentistry. However, there are several ways to alleviate pain before dental procedures begin, or the often painful nature of the injection in local anesthesia. Transcutaneous electrical nerve stimulation (TENS)24, use of intraoral lidocaine patch11 and computerized local anesthesia7 (the Wand) are newly developed methods to alleviate the pain and anxiety of dental patients, as alternatives to conventional local anesthesia.
The Wand (Milestone Scientific, Livingston, NJ) is a computer-controlled local anesthesia delivery system that drives local anesthetic from a conventional local anesthetic cartridge through plastic microtubing into a plastic handle to which a luer-lok needle is attached. The computer-controlled flow is initiated by exerting pressure on a foot pedal. The pump allows administration of local anesthetic at two slow but constant rates, and the computer compensates for variation in resistance to flow4. During needle insertion, continuous positive pressure delivers an anesthetic drip that precedes the needle. The combination of an anesthetic pathway and controlled flow rate results in a virtually imperceptible injection and rapid onset of profound anesthesia. The Wand System offers several advantages over conventional syringes, including excellent tactile sensation afforded by a lightweight plastic handle and the ability to rotate the needle as it is introduced into tissues, producing a coring penetration that minimizes needle deflection. Wand devices automatically deliver the anesthetic more slowly and precisely than a conventional syringe, thereby reducing patient discomfort5,15. Anesthetic solution gently pumped into the soft tissue can be absorbed at the same rate by soft tissue in the Wand system. The theory is that when the needle is advanced slowly, the drops of solution anesthetize the tissue ahead of the needle. All techniques of local anesthesia, such as maxillary and mandibular infiltration, mandibular block22, intraligamentary26, and anterior middle superior alveolar (AMSA) injection8, and anterior superior alveolar (ASA) injection25 can be performed with the Wand system.
Conventionally, maxillary teeth have been anesthetized by administering an infiltration injection on the buccal or labial aspects of the target tooth. Palatal injections have also been administered by plastic syringe for this objective, but can be painful5,7. The AMSA anesthesia technique was first described by Friedman and Hochman5. The AMSA injection technique anesthetizes maxillary teeth6,8,18. The AMSA derives its name from the injection's ability to anesthetize both the anterior and middle superior alveolar nerves5–7. The middle superior alveolar (MSA) and ASA nerves branch from the infraorbital nerve before they exit from the infraorbital foramen. The MSA nerve is thought to innervate the maxillary premolars and plays some role in pulpal innervation of the mesiobuccal root of the first molar. The anterior, superior alveolar nerve supplies pulpal innervation to the central and lateral incisors and canines18. The plexus where the 2 nerves join is the target site for the AMSA injection. The 10 maxillary teeth extending from the second premolar to contralateral second premolar, and the associated palatal tissue, can be anesthetised with bilateral AMSA injection5–7.
Wand research is largely attributable to pediatric dentistry1,2,9, restorative dentistry7, endodontics14, periodontology17,26,27, maxillofacial surgery16, comparison of pain perception to the Wand and a traditional syringe21,28, influence of anesthetic flow rate delivered by the Wand on pain response to the palatal injection23. There is limited research about the prosthetic dentistry-Wand combination in the literature. The hypothesis of the present study was that the Wand anesthesia technique reduces the pain at different phases (needle insertion, delivery of local anesthetic and tooth preparation) versus conventional buccal anesthesia with conventional plastic syringe. Therefore, the study compared pain levels at needle insertion, during delivery of local anesthetic solution and during tooth preparation, for the conventional syringe technique on the buccal or labial aspect on one side, and the AMSA technique with Wand local anesthesia application on the other side of the maxilla. A 5-point verbal pain rating scale (VRS)12,17 was used on 16 patients who were under prosthodontic treatment in the Ondokuz Mayis University clinic.
MATERIAL AND METHODS
Sixteen adult patients who had partially edentulous states of both left and right maxillary arch, and were to undergo fixed prosthodontic treatment, participated in this study. They ranged in age from 27 to 64, were predominantly women (12 women and 4 men), and were in a good health. Patients were not taking any medication that would alter their pain perception, as determined by a written medical health form and oral questioning. Allergy to lidocaine, mepivacaine, sulphides or articaine, history of significant medical problems, taking central nervous system depressants within 48 hours, pregnancy, or inability to give informed consent, were the exclusion criteria. The Human Subjects Review Committee of Ondokuz Mayis University approved this study (28.11.2005 dated, and 328 numbered), and written, informed consent was obtained from each patient.
The patients were informed that computer controlled and conventional injection techniques were being studied. All patients had previously experienced a conventional syringe, no patients had previously received the Wand injection, and all patients had at least one tooth absent both on the left and right maxillary arch.
Patients served as their own controls. The AMSA technique with the Wand for half the maxillary arch and conventional plastic syringe anesthesia on mucobuccal fold (control group) for opposite maxillary arch were administered by the same operator. The order of anesthesia techniques was randomly selected, and anesthesia procedures and tooth preparations were completed in the same session (Table 1).
TABLE 1. Prepared teeth of the patients in FDI (Federation of Dental International) notation system and VRS* pain data from conventional and the Wand® anesthesia techniques.
| Prepared maxillary teeth in FDI notation and applied anesthesia technique | Conventional | The Wand® | |||||
|---|---|---|---|---|---|---|---|
| Conventional | The Wand | Cins | Cdel | Cpre | Wins | Wdel | Wpre |
| 16, 13, 12, 11 | 22, 23, 24 | 2 | 2 | 0 | 2 | 0 | 0 |
| 16, 14, 11 | 21, 25 | 2 | 2 | 2 | 0 | 0 | 1 |
| 15, 14, 13 | 23, 24, 25 | 0 | 0 | 0 | 0 | 0 | 0 |
| 13, 11 | 21, 23 | 2 | 0 | 0 | 0 | 0 | 1 |
| 16, 11 | 21, 22 | 2 | 0 | 0 | 0 | 0 | 0 |
| 16, 13, 12, 11 | 21, 22, 23, 24, 25 | 2 | 2 | 0 | 0 | 0 | 0 |
| 13, 11 | 21, 22, 23, 25 | 3 | 2 | 0 | 2 | 0 | 0 |
| 16, 14, 12, 11 | 21, 22 | 2 | 2 | 0 | 0 | 0 | 0 |
| 16, 15, 13 | 23, 25 | 2 | 0 | 0 | 0 | 0 | 0 |
| 16, 15, 13, 11 | 21, 23, 25 | 3 | 2 | 0 | 0 | 2 | 0 |
| 16, 15, 13, 12, 11 | 21, 22, 25 | 3 | 2 | 0 | 2 | 0 | 0 |
| 16, 14, 13, 11 | 21, 23, 25 | 3 | 2 | 0 | 0 | 0 | 0 |
| 15, 14, 13, 11 | 21, 24, 25 | 2 | 2 | 0 | 0 | 0 | 0 |
| 15, 14, 13, 12, 11 | 21, 22, 23 | 3 | 2 | 0 | 1 | 0 | 0 |
| 16, 13, 12, 11 | 21, 22, 23, 24, 25 | 2 | 2 | 0 | 0 | 0 | 0 |
| 16, 14, 13 | 22, 23, 25 | 3 | 2 | 0 | 0 | 0 | 0 |
VRS (0 no pain, 1 minimal pain, 2 slight pain, 3 moderate pain and 4 severe pain).
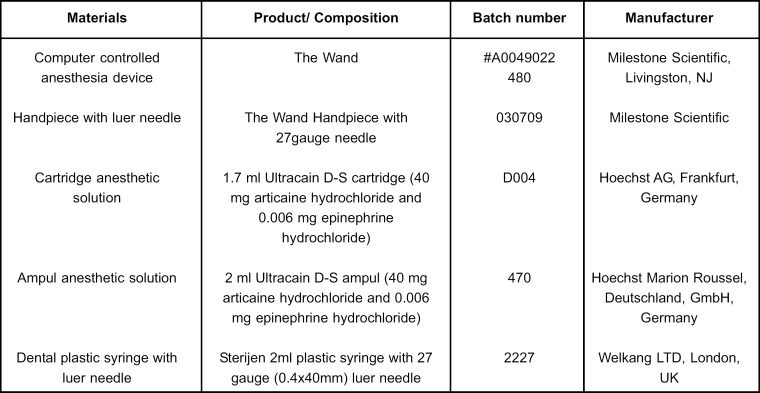
The pain ratings were explained to the patients before injection. The pain level descriptions were as follows: no pain, minimal pain, slight pain, moderate pain and severe pain (0, 1, 2, 3, 4). Patients were blindfolded with a commonly used sleeping mask so they would not distinguish which anesthetic delivery system was used. The Wand produces audible beeps as the injection is administered. Because the beeping tones cannot be turned off with a switch, the sound were produced during both injection methods (The Wand or conventional-control) so the patients were not aware of the method being used. Immediately after needle insertion, delivery of local anesthetic and tooth preparation, patients were asked to remove mask and rate the pain for both conventional and Wand injection techniques. No topical anesthetic was used because the Wand manufacturer's instructions suggest that topical application is optional. This study was conducted according to a split- mouth design, with both injections given to all patients. For each patient, the AMSA technique with single Wand injection was used on one side for central incisors, lateral incisors, upper canine, first and second premolars, and the traditional plastic aspirating syringe injection was used on the mucobuccal fold of the related tooth on the opposite side. The AMSA injection site is located at a point that bisects the maxillary first and second premolars, and midway between the crest of the free gingival margin and mid-palatine suture. The needle is orientated at a 45 degree angle with the bevel facing the palatal tissue, while rotating the Wand needle. All injections were given by the same operator who had had two months experience using the Wand at the Department of Prosthodontics, Faculty of Dentistry, Ondokuz Mayis University, Turkey. The products used in this study are presented in Figure 1.
FIGURE 1. Materials used in this study.
The ampul form of articaine hydrochloride with adrenalin (Hoechst Marion Roussel, Deutschland, GmbH, Germany) was injected with conventional plastic syringe and 27gauge dental needle. The cartridge form of articaine hydrochloride with adrenaline (Hoechst AG, Frankfurt, Germany) was administered with the computer-controlled anesthesia device (The Wand, Milestone Scientific, Livingston, NJ, USA), with 27gauge handpiece and needle (Milestone Scientific). Approximately 0.9 to 1.0 mL local anesthetic was used both for AMSA with The Wand on one side and control group for each tooth on the other side. Groups were labelled as follows: Group (Cins), pain perception scores at needle insertion for the conventional technique; Group (Cdel), pain perception scores for local anesthetic delivery by the conventional technique; Group (Cpre), pain perception scores at tooth preparation for the conventional technique; Group (Wms), pain perception scores at needle insertion by the Wand technique; Group (Wdel), pain perception scores for local anesthetic delivery for the Wand technique; and Group (Wpre), pain perception scores at tooth preparation for the Wand technique.
Power analysis were performed to detect adequate sample size using statistical software (PASS 2008, NCSS, Kaysville, UT, USA). Group sample sizes of 16 and 16 achieve 100% power to detect statistical differences. Since our variable was an ordinal level, the Mann-Whitney U test was used to determine the number of times a score from the conventional method is ranked than a score from the Wand techniques at 1% significance level. Statistical tests were performed with the statistical software (SPSS version 12.0; SPSS Inc, Chicago, IL, USA). Differences in pain rating were analyzed at needle insertion, delivery of local anesthetic and during tooth preparation for conventional versus the Wand techniques.
RESULTS
Sixteen adult patients aged from 27 to 64 (12 women and 4 men) participated in this study. The VRS data are shown in Table 2. Median scores, minimum and maximum pain rating values after needle insertion, and delivery of anesthetic and tooth preparation time for both conventional and Wand techniques, are shown in Table 3.
TABLE 2. VRS pain data from conventional and Wand anesthesia techniques.
| Conventional technique Cins Cdel Cpre | The Wand | ||||
|---|---|---|---|---|---|
| Cins | Cdel | Cpre | Wins | Wdel | Wpre |
| 2 | 2 | 0 | 2 | 0 | 0 |
| 2 | 2 | 2 | 0 | 0 | 1 |
| 0 | 0 | 0 | 0 | 0 | 0 |
| 2 | 0 | 0 | 0 | 0 | 1 |
| 2 | 0 | 0 | 0 | 0 | 0 |
| 2 | 2 | 0 | 0 | 0 | 0 |
| 3 | 2 | 0 | 2 | 0 | 0 |
| 2 | 2 | 0 | 0 | 0 | 0 |
| 2 | 0 | 0 | 0 | 0 | 0 |
| 3 | 2 | 0 | 0 | 2 | 0 |
| 3 | 2 | 0 | 2 | 0 | 0 |
| 3 | 2 | 0 | 0 | 0 | 0 |
| 2 | 2 | 0 | 0 | 0 | 0 |
| 3 | 2 | 0 | 1 | 0 | 0 |
| 2 | 2 | 0 | 0 | 0 | 0 |
| 3 | 2 | 0 | 0 | 0 | 0 |
TABLE 3. Descriptive statistics for the two anesthesia techniques during 3 phases.
| Anesthesia techniques | Groups | Median scores | Minimum | Maximum |
|---|---|---|---|---|
| Conventional | Cins | 2 | 0 | 3 |
| Cdel | 2 | 0 | 2 | |
| Cpre | 0 | 0 | 2 | |
| The Wand | Wins | 0 | 0 | 2 |
| Wdel | 0 | 0 | 2 | |
| Wpre | 0 | 0 | 1 |
The results of the Mann-Whitney U test are presented in Table 4. The Wand technique registered a highly significantly lower pain level during the needle insertion phase (z = - 4.064, p<0.01), with the Wand technique having a lower pain level compared to the conventional. During the anesthetic solution delivery phase, the pain level for the Wand technique was again highly significantly lower than for the conventional technique (z = - 3.897, p<0.01). However, there was no difference between the Wand and conventional techniques for pain level during tooth preparation (z = - 0.671, p>0.05).
TABLE 4. Differences between the two anesthesia techniques for pain level.
| Anesthesia techniques | Mean rank | ||
|---|---|---|---|
| Needle insertion (Cins- Wins) | Delivery of anesthesic solution (Cdel- Wdel) | Tooth preparation (Cpre- Wpre) | |
| Conventional | 23.13b | 22.00b | 16.00a |
| The Wand | 9.88a | 11.00a | 17.30a |
Different letters in same column indicate statistically significant difference at 1% level.
DISCUSSION
The research hypothesis stated that the Wand anesthesia technique reduces the pain at different phases (needle insertion, delivery of local anesthetic and tooth preparation) versus conventional buccal anesthesia with conventional plastic syringe. The results of the study partially support this hypothesis. The Wand anesthesia technique reduces the pain compared the conventional anesthesia for needle insertion and anesthetic solution delivery phases (p<0.01), with the exception of tooth preparation phase (p>0.05).
The majority of literature on the computer-controlled injection system (the Wand) has dealt with the pain of injection with the computer-assisted injection system, compared to injection using a conventional syringe1,2,8–l0,l6,2l,27,28. in general, the results have been favorable1,8,9,16,23,27 for the computer-assisted injection system, with only 2 studies showing no difference2,28, and 1 study showing higher pain ratings10.
Palatal injections are generally considered the most painful injections13; Wahl, et al.30 showed that palatal injections caused significantly more pain than other intraoral injections. The authors of18,30 speculated that palatal injection pain might be mainly the result of pressure.
The traditional route for administration of anesthesia to the maxillary teeth is supraperiosteal infiltration delivered in the mucobuccal fold near the apex of the tooth to be anesthetized. Although effective in achieving pulpal anesthesia of the neurovascular bundle by diffusion of anesthetic through the porous maxilla, this approach routinely anesthetizes the surrounding tissues (lips, surface of the face), and also affects muscle activity. The patient's natural repose, as well as active facial expressions are temporarily affected, including an distortion of the smile. The patient also experiences the annoying sensation of facial numbness, and the smile line is temporarily invalidated as an esthetic reference for restorative and prosthetic dentistry. An alternative to maxillary infiltration is the infraorbital nerve block injection which, if properly performed, achieves anesthesia of the anterior superior alveolar branch of the trigeminal nerve. This injection site, however, is also close to muscles of expression, and anesthesia of cutaneous fibers of the infraorbital nerve results in a corresponding loss of sensation in the face and the upper lip29.
The palatal approach AMSA nerve block can be attempted with a traditional manual syringe, but the precise pressure and volume ratios of the Wand are virtually impossible to reproduce5,6. The clinician can anesthetize several teeth in the maxillary arch, extending from the mesiobuccal root of the first molar to the central incisor, by means of a single palatal infiltration. In addition to profound pulpal anesthesia, palatal soft tissue anesthesia is realized, which also extends from the maxillary first molar to the central incisor and the associated palatal tissues, without numbness to the lips and face, and without interference with the muscles of facial expression for at least 60 min16,25. During needle insertion with a coring motion, continuous positive pressure delivers an anesthetic drip that precedes the needle. The drops of solution anesthetize the tissue ahead of the needle when the needle is advanced slowly7,15. The combination of an anesthetic pathway and controlled flow rate results in virtually imperceptible needle insertion and injection, and rapid onset of profound anesthesia28.
The same efficacy of anesthesia was achieved with conventional buccal anesthesia and the palatal approach AMSA technique with the Wand device25. The current study was in agreement for tooth preparation, but contradictory for needle insertion and delivery of local anesthetic. Numbness of the lips and face was not observed in the current study for the palatal approach when using the AMSA technique with the Wand.
Another study using the VRS (verbal rating scale) compared computer-controlled and conventional local anesthesia delivery systems for performing scaling and root planing on patients with moderate periodontal disease; AMSA injections with the Wand were considered less painful than the conventional syringe17. Two further benefits of the AMSA injection technique are that it also eliminates the potential for an intravascular injection because no major vessels are encountered in this region of the palate5, and the palatal bone is porous enough to permit the anesthetic solution to diffuse through the tissues and anesthetize both the anterior and middle branches of the superior alveolar nerve when the injection is deliberately slow and steady. For this reason, the successful deposition of the anesthetic solution through the fibrous tissue is said to be accomplished more easily with the computer-controlled delivery device that regulates the pressure and volume ratio of solution delivered5,7.
The Wand System offers several advantages over conventional syringes, including excellent tactile sensation afforded by the lightweight plastic handle and the ability to rotate the needle as it is introduced into tissues, producing a coring penetration that minimizes needle deflection. Presumably, the slow rate of anesthetic flow reduces patient discomfort compared with palatal injections administered with a traditional syringe4. Decreasing the total amount of anesthetic and vasoconstrictor necessary for maxillary anesthesia, shorthening the total anesthesia time, and diminishing patient-operator anxiety are other advantages of the Wand19. However, the Wand's beeping sounds make the injection seem longer and may make the patient feel uncomfortable. Other negative aspects of the Wand are frequent breakage of the anesthetic cartridge on activation of the unit, and a separate instrument is required for removing the cartridge from the unit10. Additionally, 1.4 mL anesthetic solution can be delivered in about 1 min in rapid injection mode, and in 4 min 45 s in slow injection mode9.
Fukayama, et al.8 examined the efficacy of the AMSA anesthesia technique using the Wand system to assist with the electrical pulp test. Electrical pulp stimulation indicated that the lateral incisors, canines, and first and second premolars were more anesthetized than the central incisors and first molars. They also stated that anesthetic applied via AMSA with the Wand has a slow onset and further studies are required to evaluate its effectiveness for this reason. However, AMSA injection using the Wand method seems to both preclude severe injection pain and be very effective for pulpal anesthesia of lateral incisors, canines, and premolars. Pain scores were higher for AMSA technique in the central tooth than in other teeth (p<0.05) in another related study16.
In the present study, in two cases of AMSA using the Wand, pain was at the minimum level (VRS score 1) during tooth preparation of central incisors. The reason for this pain rating could be that the central incisors were innervated from the opposite arch, or alternatively, Fukayama, et al.8 and Lee, et al.16 stated that the effectiveness of the Wand is lower in the central incisors and first molar teeth than lateral incisors, canines, and premolars.
Friedman and Hochman5–7 stated that careful needle insertion and slow anesthetic delivery could reduce the sensation of needle insertion. Anesthetic flow rate is independent of applied pressure in the Wand system12. Primosch and Brooks23 showed that slow anesthetic delivery produces significantly lower pain scores than fast anesthetic delivery, and the Wand decreases the pain for both slow or fast anesthetic delivery rate, but contrary to the manufacturer's claims, it did not eliminate pain elicited by palatal injections in some patients34.
In the present study, a highly significant (p<0.01) difference for pain rating was obtained between conventional buccal and AMSA using the Wand injection for needle insertion and anesthetic solution delivery. However, contrary to the manufacturer's claims, pain was not eliminated at slow anesthetic flow rate in this study
There have been limited prosthodontic or restorative studies for AMSA using Wand injection. In one study, AMSA was bilaterally applied with the Wand and 6 anterior maxillary teeth were prepared. Incisal reduction of these teeth was achieved with reference to the lip, which is not affected by AMSA. Porcelain restoration was also fabricated using the lip contour for ideal incisal shape. Bilaterally, the AMSA technique using the Wand was repeated for tooth sensitivity during the cementation procedure5,6. As in previous studies, AMSA using the Wand was also of benefit for lip guidance in the present study.
Another benefit of palatal AMSA injection using the Wand is that it reduces the number of injections, and also the amount of anesthetic solution compared to conventional buccal infiltration anesthesia that applies multiple injections to each tooth. In addition, more teeth can be anesthetized with a single injection, without numbness of lips and face, compared to the conventional technique.
CONCLUSIONS
The AMSA technique administered using the Wand in a prosthodontic treatment reduced pain highly significantly more than conventional buccal anesthesia, both in inserting the needle and in the of delivery of local anesthetic. When comparing the anesthesia efficiency of AMSA using the Wand injection and conventional buccal infiltration techniques, no statistical difference was found. Although the slow anesthetic flow rate proved superior in pain control, the pain score was not zero for the Wand, contrary to the manufacturer's claim. Computer-controlled anesthesia using the Wand appears advantageous for restorative procedures because more teeth are anesthetized with one palatal injection, and without numbness of lips and face, in contrast to multiple conventional buccal anesthetic injections for each tooth.
REFERENCES
- 1.Allen KD, Kotil D, Larzelere RE, Hutfless S, Beiraghi S. Comparison of a computerized anesthesia device with a traditional syringe in preschool children. Pediatr Dent. 2002;24:315–320. [PubMed] [Google Scholar]
- 2.Asarch T, Allen K, Petersen B, Beiraghi S. Efficacy of a computerized local anesthesia device in pediatric dentistry. Pediatr Dent. 1999;21:421–424. [PubMed] [Google Scholar]
- 3.Ballard BE. Biopharmaceutical considerations in subcutaneus and intramuscular drug administration. J Pharm Sci. 1968;57:357–378. doi: 10.1002/jps.2600570301. [DOI] [PubMed] [Google Scholar]
- 4.Blanton PL, Jeske AH. Dental local anesthetics: alternative delivery methods. J Am Dent Assoc. 2003;134:228–234. doi: 10.14219/jada.archive.2003.0140. [DOI] [PubMed] [Google Scholar]
- 5.Friedman MJ, Hochman MN. A 21st century computerized injection system for local pain control. Compend Contin Educ Dent. 1997;18:995–1003. [PubMed] [Google Scholar]
- 6.Friedman MJ, Hochman MN. The AMSA injection: a new concept for local anesthesia of maxillary tooth using a computer-controlled injection system. Quintessence Int. 1998;29:297–303. [PubMed] [Google Scholar]
- 7.Friedman MJ, Hochman MN. Using AMSA and P-ASA nerve blocks for esthetic restorative dentistry. Gen Dent. 2001;49:506–511. [PubMed] [Google Scholar]
- 8.Fukayama H, Yoshikawa F, Kohase H, Umino M, Suzuki N. Efficacy of anterior and middle superior alveolar (AMSA) anesthesia using a new injection system: the Wand. Quintessence Int. 2003;34:537–541. [PubMed] [Google Scholar]
- 9.Gibson RS, Allen K, Hutfless S, Beiraghi S. The Wand vs. traditional injection: a comparison of pain related behaviors. Pediatr Dent. 2000;22:458–462. [PubMed] [Google Scholar]
- 10.Goodell GG, Gallagher FJ, Nicoll BK. Comparison of a controlled injection pressure system with a conventional technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:88–94. doi: 10.1067/moe.2000.107365. [DOI] [PubMed] [Google Scholar]
- 11.Hersh EV, Houpt MI, Cooper SA, Feldman RS, Wolf MS, Levin LM. Analgesic efficacy and safety of an intraoral lidocaine patch. J Am Dent Assoc. 1996;12(7):1626–1634. doi: 10.14219/jada.archive.1996.0098. [DOI] [PubMed] [Google Scholar]
- 12.Hochman M, Chiarello D, Hochman CB, Lopatkin R, Pergola S. Computerized local anesthetic delivery vs. traditional syringe technique: subjective pain response. N Y State Dent J. 1997;63:24–29. [PubMed] [Google Scholar]
- 13.Hutchins HS, Young FA, Lackland DT, Fishburne CP. The effectiveness of topical anesthesia and vibration in alleviating the pain of oral injections. Anesth Prog. 1997;44:87–89. [PMC free article] [PubMed] [Google Scholar]
- 14.Keller BJ. Comparison of the effectiveness of two topical anesthetics and placebo in reducing injection pain. Hawaii Dent J. 1985;16:10–11. [PubMed] [Google Scholar]
- 15.Krochak M, Friedman N. Using a precision metered injection system to minimize dental injection anxiety. Compend Contin Educ Dent. 1998;19:137–148. [PubMed] [Google Scholar]
- 16.Lee S, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of the anterior middle superior alveolar (AMSA) injection. Anesth Prog. 2004;51:80–89. [PMC free article] [PubMed] [Google Scholar]
- 17.Loomer PM, Perry DA. Computer-controlled delivery versus syringe delivery of local anesthetic injections for theurapeutic scaling and root planing. J Am Dent Assoc. 2004;135:358–365. doi: 10.14219/jada.archive.2004.0188. [DOI] [PubMed] [Google Scholar]
- 18.Malamed SF. Handbook of local anesthesia. 4th ed. St. Louis: Mosby; 1997. [Google Scholar]
- 19.Matthews DC, Rocchi A, Gafni A. Factors affecting patients 'and potential patients' choices among anaesthetics for periodontal recall visits. J Dent. 2001;29:173–179. doi: 10.1016/s0300-5712(01)00009-4. [DOI] [PubMed] [Google Scholar]
- 20.Milgrom P, Coldwell SE, Getz T, Weinstein P, Ramsey DS. Four dimensions of fear of dental injections. J Am Dent Assoc. 1997;128:756–766. doi: 10.14219/jada.archive.1997.0301. [DOI] [PubMed] [Google Scholar]
- 21.Nicholson JW, Berry TG, Summitt JB, Yuan CH, Witten TM. Pain perception and utility: a comparison of the syringe and computerized local injection techniques. Gen Dent. 2001;49:167–173. [PubMed] [Google Scholar]
- 22.Öztas N, Ulusu T, Bodur H, Dogan C. The Wand in pulp therapy: an alternative to inferior alveolar nerve block. Quintessence Int. 2005;36:559–564. [PubMed] [Google Scholar]
- 23.Primosch RE, Brooks R. Influence of anesthetic flow rate delivered by the Wand local anesthetic system on pain response to palatal injection. Am J Dent. 2002;15:15–20. [PubMed] [Google Scholar]
- 24.Quarnstrom F, Libed EN. Electronic anesthesia versus topical anesthesia for the control of injection pain. Quintessence Int. 1994;25:713–716. [PubMed] [Google Scholar]
- 25.Ram D, Kassirer J. Assessment of a palatal approach- anterior superior alveolar (P-ASA) nerve block with the Wand in pediatric dental patients. Int J Paediatr Dent. 2006;16:348–351. doi: 10.1111/j.1365-263X.2006.00752.x. [DOI] [PubMed] [Google Scholar]
- 26.Ram D, Peretz B. Assessing the pain reaction of children receiving periodontal ligament anesthesia using a computerized device (Wand) J Clin Pediatr Dent. 2003;27:247–250. [PubMed] [Google Scholar]
- 27.Rosenberg ES. A computer-controlled anaesthetic delivery system in a periodontal practice: patient satisfaction and acceptance. J Esthet Restor Dent. 2002;14:39–46. doi: 10.1111/j.1708-8240.2002.tb00146.x. [DOI] [PubMed] [Google Scholar]
- 28.Saloum FS, Baumgartner JC, Marshall G, Tinkle J. A clinical comparison of pain perception to the Wand and a traditional syringe. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:691–695. doi: 10.1067/moe.2000.106333. [DOI] [PubMed] [Google Scholar]
- 29.Simon JF, Peltier B, Chambers D, Dower J. Dentists troubled by the administration of anaesthetic injections: long-term stresses and effects. Quintessence Int. 1994;25:641–646. [PubMed] [Google Scholar]
- 30.Wahl MJ, Schmitt MM, Overton DA, Gordon MK. Injection pain of bupivacaine with epinephrine vs. prilocaine plain. J Am Dent Assoc. 2002;133:1652–1656. doi: 10.14219/jada.archive.2002.0115. [DOI] [PubMed] [Google Scholar]