Abstract
Nasoendoscopy is an important tool for assessing velopharyngeal function. The purpose of this study was to analyze velar and pharyngeal wall movement and velopharyngeal gap during nasoendoscopic evaluation of the velopharynx before and during diagnostic therapy. Nasoendoscopic recordings of 10 children with operated cleft lip and palate were analyzed according to the International Working Group Guidelines. Ratings of movement of velum and pharyngeal walls, and size, location and shape of gaps were analyzed by 3 speech-language pathologists (SLPs). Imaging was obtained during repetitions of the syllable/pa/during a single nasoendoscopic evaluation: (a) before diagnostic therapy, and (b) after the children were instructed to impound and increase intraoral air pressure (diagnostic therapy). Once the patients impounded and directed air pressure orally, the displacement of the velum, right, left and posterior pharyngeal walls increased 40, 70, 80, and 10%, respectively. Statistical significance for displacement was found only for right and left lateral pharyngeal walls. Reduction in gap size was observed for 30% of the patients and other 40% of the gaps disappeared. Changes in gap size were found to be statistically significant between the two conditions. In nasoendoscopic assessment, the full potential of velopharyngeal displacement may not be completely elicited when the patient is asked only to repeat a speech stimulus. Optimization of information can be done with the use of diagnostic therapy's strategies to manipulate VP function. Assuring the participation of the SLP to conduct diagnostic therapy is essential for management of velopharyngeal dysfunction.
Keywords: Nasoendoscopy, Diagnostic therapy, Velar displacement, Pharyngeal walls displacement, Gap size
INTRODUCTION
An analysis of velopharyngeal performance may require the use of procedures such as nasopharyngoscopy and videofluoroscopy1. More specifically, during nasoendoscopic assessment one can observe velopharyngeal patterns of closure (or best attempt to closure) having the possibility of determining the factors that contribute to velopharyngeal dysfunction (VPD). Because many procedures are available to correct VPD, an adequate treatment decision may require the identification of the pattern of velopharyngeal functioning for speech with specific ratings of movement of the velum as well as the pharyngeal walls9. While the optimization of information obtained during the decision making process is possible when nasoendoscopy and videofluoroscopy are used as complementary procedures10,12, nasoendoscopic assessment does not involve radiation allowing for an extended time of examination during which one can attempt to modify velopharyngeal function.
The use of visual biofeedback of the velopharynx with nasoendoscopy has been described as a strategy for behavioral modification of velopharyngeal functioning during speech therapy2,4,7,8,13. Usually, during speech therapy with endoscopic biofeedback, the subjects are initially asked to observe their VP mechanism during function with attention called on both, movements and sensations. The therapist then guides the speaker targeting voluntary control of the movements and progressively increasing the complexity of the tasks. While improved velopharyngeal function during speech therapy with endoscopic feedback has been reported by several authors2,4,7,8,13 manipulation of velopharyngeal functioning with diagnostic therapy in the nasoendoscopic assessment during the decision making process for management of VPD has not been described.
In the management of VPD, the development of the most appropriate speech stimuli for each patient is the role of the speech-language pathologist11,12. In order to elicit the best performance of the VP mechanism, the speech stimuli for nasoendoscopic or videofluoroscopic diagnostic assessments involve the use of oral pressure phonemes, both as isolated sounds (including a sustained sibilant or fricative) and in a sample of connected speech including nasal to oral transitions10,12. The SLP (speech-language pathologist) must adequate the stimuli according to the speech performance and the stimulability of each patient taking into consideration both organic and functional conditions. Williams, et al.12 (2004) suggest that developmental delay leading to immature articulatory pattern, use of atypical articulatory patterns (glottal or pharyngeal stops or fricatives, for example), fistula, and even enlarged palatine tonsils, may affect velar and walls displacement.
In our practice (Hospital for Rehabilitation of Craniofacial Anomalies of the University of São Paulo, HRAC/USP), we have observed that patients who use reduced subglottic pressure and/or weak intraoral pressure during production of oral speech sounds may not elicit all velopharyngeal potential even when they achieve adequate place of articulation. We also have seen patients who already presented Passavant's pad, to improve the pad's excursion reducing or even eliminating the velopharyngeal gap after being instructed to increase and direct air pressure orally. That is, even in the presence of which seems to be "the best attempt to close the VP", we may be able to further improve VP functioning, thus leading to a change in treatment recommendation. Behavioral manipulation of velopharyngeal function during diagnostic procedure, however, still needs further investigation since effortful and/or compensatory maneuvers (such as tongue anchor, for example) may compromise the interpretation of findings.
In this study, patients were guided to increase and direct air pressure orally during production of the syllable /pa/, a strategy that we called diagnostic therapy. It is hypothesized that the use of increased oral-pressure could elicit or improve movement of the velopharyngeal structures during a single nasoendoscopic diagnostic evaluation. The purpose of this study was therefore to compare ratings of velum and pharyngeal wall movements and velopharyngeal gap size before and during diagnostic therapy during a single nasoendoscopic evaluation of the velopharynx.
MATERIAL AND METHODS
Participants
Ten non-syndromic Brazilian children with operated unilateral cleft lip and palate of both gender (4 girls and 6 boys) aged between 5 and 8 years (mean age 5y7m) participated in this study. All children had undergone lip repair (3 with Spina and 7 with Millard techniques, respectively) at 3 to 6 months of age as well as primary palatal repair (4 with Furlow and 6 with Van Longenback techniques, respectively) at 9 months to 1 year and 4 months of age. All children presented with consistent hypernasality and nasal air emission as perceptually judged by a single SLP with extensive experience in rating speech disorders associated with velopharyngeal dysfunction. None of the children presented compensatory articulation with the exception of one child who presented posterior nasal fricative for /s/ and /z/ sounds. All children present normal language development.
The children underwent a videonasendoscopic evaluation of VP function at HRAC/USP. Nasoendoscopic films obtained from these evaluations were analyzed following the International Working Group Guidelines proposed by Golding-Kushner, et al.3 (1990). The HRAC/USP Institutional Review Board approved this study, which was conducted in compliance with the principles outlined in the Declaration of Helsinki.
Examiner and Equipment
A SLP with 15 years of experience performing instrumental evaluation of VP function conducted the videonasendoscopic assessment of each child. All nasoendoscopic films were obtained using a pediatric Olympus (ENF Type P4) flexible fiberoptic scope. The procedures were video-taped for further analysis.
Procedures
The children's VP structures were examined after the described procedures for nasoendoscopic evaluation10. Although some children were quite reluctant to undergo the procedure at the beginning of the exam, compliance was obtained for all children during VP examination. Each child was instructed to seat comfortably in a dentist's chair while the SLP inserted the scope into the most permeable nare. Once the scope was in position, the examiner performed the VP examination under both conditions (before and during diagnostic therapy) without removing the scope from the child's nose.
For the diagnostic therapy condition, it was demonstrated to each child how to generate a flow of air orally and how to interrupt this flow with bilabial closure. The syllable /pa/ was selected for this study because the voiceless plosive sound (/p/) requires the patients to generate a flow of air orally and interrupt this flow with bilabial closure by impounding and maintaining considerable amount of air pressure, in order to elicit maximal potential of displacement of the VP structures. Additionally, the vowel /a/ was used to control to any influence of the tongue height for the vowel that followed on the target sound (/p/). Although the vowel /a/ was used, the SLP targeted the elicitation of the maximal potential of displacement of the VP structures carefully attending to the use of unwanted compensatory maneuvers. The syllable /pa/ was selected because it is easy and quickly learned by children, allowing compliance during the instrumental assessment of velopharyngeal function. Children were guided, step by step, looking and imitating the SLP until they succeeded impounding enough air orally. The SLP also demonstrated a /pa/ produced with the inflated cheeks following with the plosion for the consonant, requesting the child to do the same. The SLP targeted the elicitation of the maximal potential of displacement of the VP structures carefully attending to the use of unwanted compensatory maneuvers. Once the patient produced the syllable as instructed, the SLP asked he/she to maintain the production protruding slightly the tongue tip while holding the air with inflated cheeks. The coordination between generating and directing the air orally, impounding air pressure behind the closed lips and timing the plosion of /pa/ with the production of the vowel was practiced with the SLP who used the visual feedback of the VP structures to guide the instructions to the patient. Only the SLP faced the monitor in order to visualize VP function during the child's speech, with the child receiving no visual biofeedback other then the model of the therapist. During the evaluation, production of the syllable and changes in VP displacement were monitored by the SLP, who used a TV screen and patient observation (auditory output and visual observation of mouth, face, neck and shoulders) to guide the diagnostic therapy. The whole diagnostic therapy session lasted 5 min on average of for each studied patient.
Rating of the VP Structures Displacement
Nasoendoscopic films were analyzed using the International Working Group (IWG) Guidelines for standardizing reporting of information about the VP functioning3. IWG guidelines are based on relative ratings and measurements, with the ratings of the displacement of the structures done after contrasting the position of the structure at rest to the position during displacement. Following the guidelines, displacement and gap of velopharyngeal structures were rated by three SLPs and reported on a nasoendoscopic analysis form. Ratings of velar movement (presence/absence and velar maximum displacement); lateral pharyngeal wall movements (presence/absence, maximum displacement, direction of movement, symmetry) and posterior pharyngeal wall movement (presence/absence and maximum displacement) were firstly reported. Then, information regarding size, location and shape of the VP gap were presented.
Inter-examiner Agreement
The 3 SLPs, experienced in analyzing VP function findings obtained instrumentally, rated the films together, discussing each finding until 100% agreement was reached. There was no problem reaching 100% agreement for most rated aspects, except for lateral wall displacement. In this case, instead of establishing a rating for wall displacement varying from 0.0 to 1.0, the three SLPs reached 100% agreement rating the displacement of the lateral walls into quarters: 0-25%, 26-50%, 51-75% or 76-100%.
Data Analysis
Percent changes in displacement of velar, lateral and posterior pharyngeal walls as well as the gap size, location and shape observed before and during diagnostic therapy are presented in Tables 1 and 2. The Wilcoxon Matched Pairs test was used for comparison of the measurements under both conditions, testing the hypothesis that increased movement of VP structures, and consequently changes in gap size, shape and location, would be observed once patient impounded and directed air orally during the production of the oral pressure syllable /pa/.
TABLE 1. Summary of the displacement of the velopharyngeal structures before and during diagnostic therapy (N=10).
| Maximal Displacement | Rating Before Therapy | Rating During Therapy | Observation During Diagnostic Therapy | Before vs. During |
|---|---|---|---|---|
| Velar | Mean: 0.6 SD: 0.3 | Mean: 0.7 SD: 0.3 | 60% remained the same, 40% increased displacement | Wilcoxon Matched Pairs p=0.067898 |
| Right Lateral Pharyngeal Wall | 0%-25%** | 26%-50%** | 30% remained the same, 70% increased displacement | Wilcoxon Matched Pairs p=0.017966* |
| Left Lateral Pharyngeal Wall | 0%-25%** | 26%-50%** | 20% remained the same, 80% increased displacement | Wilcoxon Matched Pairs p=0.011724* |
| Posterior Pharyngeal Wall | Mean: 0.3 SD: 0.3 | Mean: 0.3 SD: 0.3 | 70% remained the same, 10% increased displacement, 20% could not be seen | Wilcoxon Matched Pairs p=1.0 |
Significant difference between displacement before and during diagnostic therapy
Displacement rated in quarters (0%-25%, 26%-50%, 51%-75%, 76%-100%) instead the scale 0.0 to 1.0
SD= Standard Deviation
TABLE 2. Summary of changes in gap size, shape and location during diagnostic therapy.
| Observation before Diagnostic Therapy (N=10) | Observation During Diagnostic Therapy (N=10) | Before vs. During | ||
|---|---|---|---|---|
| Gap Shape | 60% of the patients presented circular gaps, 30% coronal and 10% sagittal | 30% remained circular and 20% coronal, 10% changed from coronal to circular, 40% disappeared | No statistical test applied | |
| Gap Location | 60% located centrally, 20% skewed to the right, and 20% skewed to the left | 50% remained the same, 10% changed from central to skewed to left, 40% gap disappeared | No statistical test applied | |
| Rating Before | Rating During | Observation During Diagnostic Therapy (N=10) | Before vs. During | |
| Gap Size* | Mean: 0.6 SD: 0.3 |
Mean: 0.8 SD: 0.2 |
30% remained the same, 30% reduced gap size, 40% gap disappeared | Wilcoxon Matched Pairs p=0.017966* |
Significant difference between displacement before and during diagnostic therapy
RESULTS
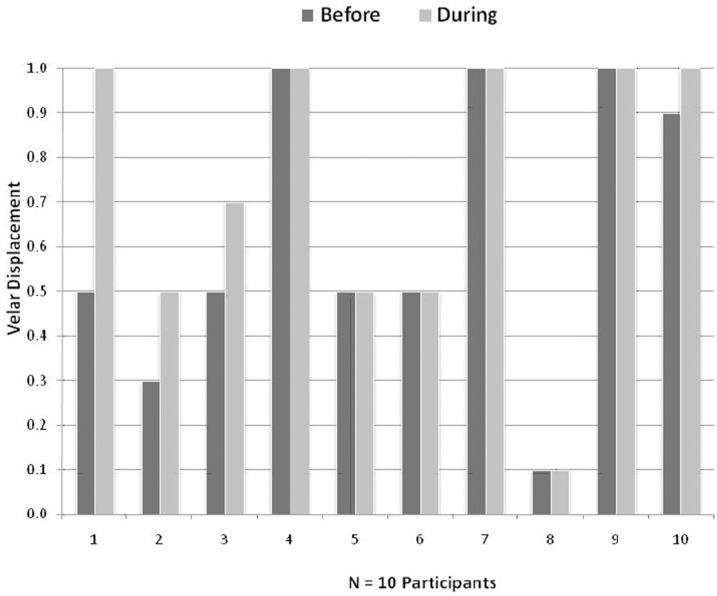
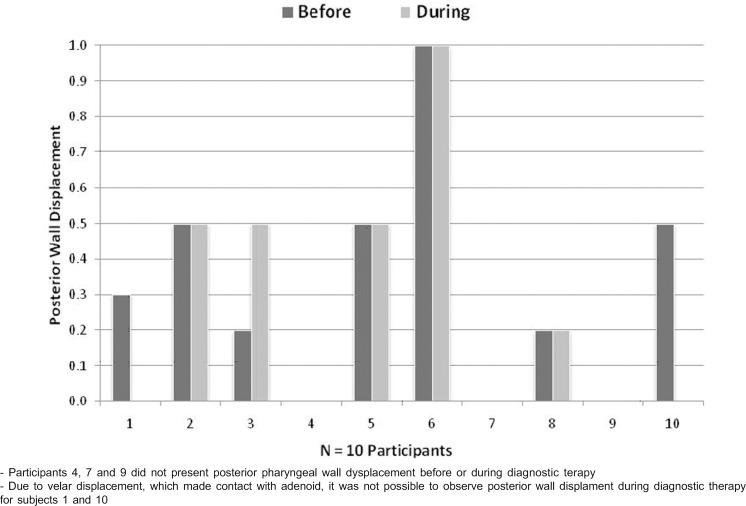
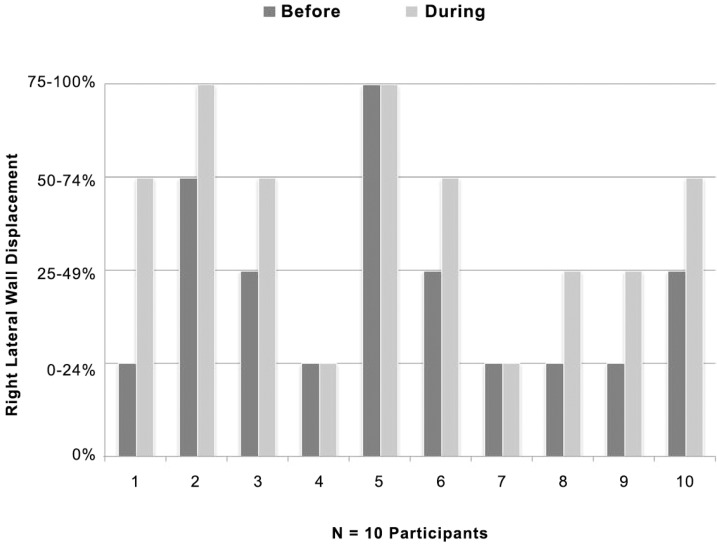
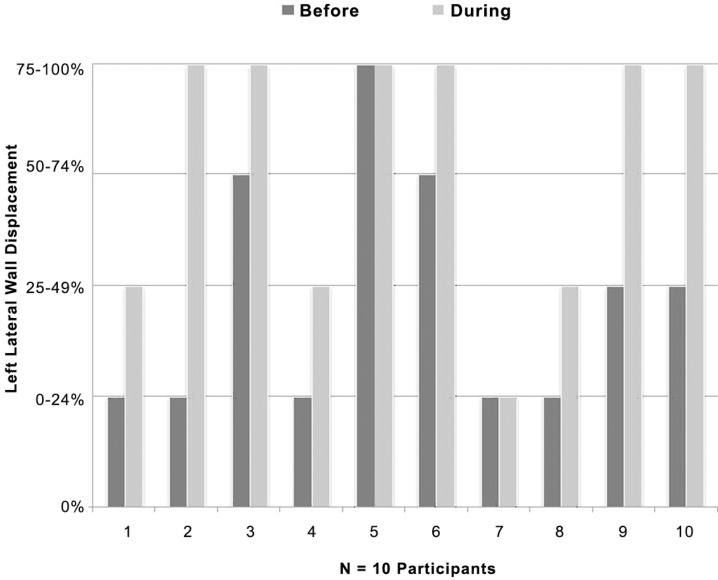
Table 1 and Figures 1–4 present the observations of velar and pharyngeal wall displacement for the syllable /pa/ during diagnostic therapy. When the patients impounded and directed air pressure orally, the displacement of the velum increased 40% (see subjects 1, 2, 3 and 10 in Figure 1). The displacement of the right lateral pharyngeal wall increased 70% (see subjects 1, 2, 3, 6, 8, 9 and 10 in Figure 2). The displacement of the left lateral pharyngeal wall increased 80% (see subjects 1, 2, 3, 4, 6, 8, 9 and 10 in Figure 3). The displacement of the posterior pharyngeal wall (Passavant's Pad) increased in 10% of the patients (see subject 3 in Figure 4) and was not observable in another 20% of the group (subjects 1 and 10 in Figure 4). That is, for two patients, the increase in the displacement of the velum lead to a contact with the adenoid not allowing for the visualization of the Passavant's Pad which were located at the lower end of the pharyngeal tonsil and below the palatal plane. Statistical significance for displacement between the two conditions was found only for right and left lateral pharyngeal walls.
FIGURE 1. Maximum velar displacement before and after diagnostic therapy for all 10 participants.
FIGURE 4. Maximum posterior pharyngeal wall displacement before and after diagnostic therapy for all 10 participants.
FIGURE 2. Maximum right lateral pharyngeal wall displacement before and after diagnostic therapy for all 10 participants.
FIGURE 3. Maximum left lateral pharyngeal wall displacement before and after diagnostic therapy for all 10 participants.
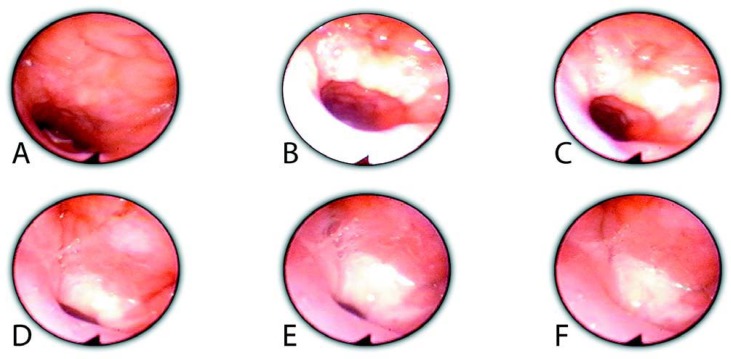
Table 2 presents the observations of VP gap size, shape and location for production of the syllable /pa/ before and during diagnostic therapy. It was observed that when the patients impounded and directed air pressure orally, 30% of the gaps reduced in size and 40% of the gaps disappeared. These changes in gap size were found to be statistically significant between the two conditions. Before diagnostic therapy, 60% of the patients presented circular gaps, 30% coronal and 10% sagittal. During diagnostic therapy, 30% of the gaps remained circular, 20% remained coronal, 10% changed from coronal to circular, while 40% of the gaps disappeared. Before diagnostic therapy, 60% of the patients presented gaps located centrally, 20% presented gaps skewed to the right, and 20% presented gaps skewed to the left. Once patients impounded and directed air orally, 50% of the gaps remained at the same location, 10% changed from central to skewed to left, and 40% disappeared. No changes were observed for direction of lateral pharyngeal walls displacement which continued to be medial for 80%, anteromedial for 10%, and posteromedial for 10% of the patients. Also, no changes were observed for symmetry of lateral pharyngeal walls movement which continued to be symmetric for 50% of the patients. Figure 5 displays changes in gap size for one participant before and during the diagnostic therapy.
FIGURE 5. Nasoendoscopic images of the velopharynx for one participant before and during diagnostic therapy. A: At rest; B: Production of /pa/ before diagnostic therapy; C: Production of /pa/ at the beginning of diagnostic therapy; D & E: Production of /pa/ showing reduction in the size of the velopharyngeal gap as the diagnostic therapy progressed; F: Production of /pa/ showing elimination of velopharyngeal gap during diagnostic therapy.
DISCUSSION
Looking historically while managing VPD, we can see that the decision-making process and treatment outcomes have changed significantly since clinicians began using procedures that allowed the visualization of the velopharynx during speech production. The role of the SLP in procedures for assessing VP function during speech has gone beyond the development of appropriate speech material. According to Williams, et al.11 (1999), Williams, et al.12 (2004) and Seagle, et al.9 (2002), for example, the SLP should also recommend the optimal method of treatment based on the interpretation of findings obtained during visualization of the VP mechanism.
Nasoendoscopic assessment of VP function, in particular, has been considered as an important tool for a careful evaluation of the velopharynx during speech5,6, especially when all velopharyngeal structures can be viewed during the speaker's best attempt of oral production. This study described the use of diagnostic therapy to elicit or modify displacement of velopharyngeal structures in a single nasoendoscopic diagnostic assessment. During the assessment, the SLP guided the speech task using the visual biofeedback of velopharyngeal displacement to orient her instructions to the patient. It was observed that the use of strategies for the manipulation of intraoral air pressure during the production of the syllable /pa/ did result in an increase of the displacement of velopharyngeal structures, even leading to the disappearance of the gap for 4 subjects. It is important to point out that while the speaker attempted his best production without any compensatory articulation, unwanted compensatory responses (such as tongue anchor, for example) were carefully monitored by the SLP. It is also important to point out that the disappearance of the gap for 4 subjects during diagnostic therapy lead us to initially select an intensive speech therapy program in order to attempt to achieve VP closure for speech before addressing a secondary surgical procedure for VPD correction for these cases. This strategy did not aim to correct VPD. Instead, it was used to lead the clinician only to improve the chances of success of a patient tailored treatment plan.
Although the present study dealt with a restrict amount of patients, the present findings as well as our clinical experience in the management of VPD using speech bulbs, lead us to believe that the full potential of VP displacement may not be completely elicited when the patient is only asked to repeat a speech stimulus. As observed in this study, optimization of information during the decision-making process to correct VPD can be done with the use of strategies of diagnostic therapy to manipulate VP function during the nasoendoscopic assessment.
Although results from this study demonstrated that the best VP function was obtained by visually monitoring the speaker's speech while producing the syllable /pa/, further research are needed to investigate whether there are differences in VP function while speakers produce different sounds in syllables as well as in longer speech samples. Additionally, even though changes in Passavant's pad displacement were observed, future studies on the role of the pad during speech production are still warranted.
CONCLUSIONS
In nasoendoscopic assessment, the full potential of velopharyngeal displacement may not be completely elicited when the patient is asked only to repeat a speech stimulus. Optimization of information can be done with the use of diagnostic therapy's strategies to manipulate VP function. Assuring the participation of the SLP to conduct diagnostic therapy is essential for management of velopharyngeal dysfunction.
REFERENCES
- 1.American Cleft Palate-Craniofacial Association. Parameters for evaluation and treatment of patients with cleft lip/palate or other craniofacial anomalies. Chapel Hill: American Cleft Palate-Craniofacial Association; Oct, 2004. Revised Edition. Available from: http://www.acpa-cpf.org/teamcare/Parameters04rev.pdf. [Google Scholar]
- 2.Brunner M, Stellzig-Eisenhauer A, Pröschel U, Verres R, Komposch G. The effect of nasopharyngoscopic biofeedback in patients with cleft palate and velopharyngeal dysfunction. Cleft Palate Craniofac J. 2005;42:649–657. doi: 10.1597/03-044.1. [DOI] [PubMed] [Google Scholar]
- 3.Golding-Kushner KJ, Argamaso RV, Cotton RT, Grames LM, Henningsson G, Jones DL, et al. Standardization for the reporting of nasopharyngoscopy and multiview videofluoroscopy: a report from an international working group. Cleft Palate Craniofac J. 1990;27:337–347. doi: 10.1597/1545-1569(1990)027<0337:sftron>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 4.Kummer AW. Cleft palate and craniofacial anomalies – effects on speech and resonance. San Diego: Singular; 2001. [Google Scholar]
- 5.Pannbacker MD, Lass NJ, Hansen GGR, Mussa AM, Robison KL. Survey of speech-language pathologists' training, experience, and opinions on nasopharyngoscopy. Cleft Palate Craniofac J. 1993;30:40–45. doi: 10.1597/1545-1569_1993_030_0040_soslpt_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 6.Pannbacker MD, Lass NJ, Scheuerle JF, English PJ. Survey of services and practices of cleft palate-craniofacial teams. Cleft Palate Craniofac J. 1992;29:164–167. doi: 10.1597/1545-1569_1992_029_0164_sosapo_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 7.Peterson-Falzone SJ, Hardin-Jones MA, Karnell MP. Cleft palate speech. 3rd ed. Mosby; St. Louis, MI: 2001. [Google Scholar]
- 8.Ruscello DM. Communicative disorders related to cleft lip and palate. In: Bzoch KR, editor. Considerations for behavioral treatment of velopharyngeal closure for speech. 5th ed. Boston: Little & Brown; 2004. [Google Scholar]
- 9.Seagle MB, Mazaheri MK, Dixon-Wood VL, Williams WN. Evaluation and treatment of velopharyngeal insufficiency: The University of Florida experience. Ann Plast Surg. 2002;48(5):464–470. doi: 10.1097/00000637-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Shprintzen RJ. Communicative disorders related to cleft lip and palate. In: Bzoch KR, editor. Nasopharyngoscopy. 5th ed. Boston: Little & Brown; 2004. [Google Scholar]
- 11.Williams WN, Pegoraro-Krook MI, Dutka J, Marino VCC, Wharton PW. Nasoendoscopy:the Role of the Speech-Language Pathologist. Braz J Dysmorphol Speech Hear Disord. 1999;2:23–36. [Google Scholar]
- 12.Williams WN, Henningsson G, Pegoraro-Krook MI. Communicative disorders related to cleft lip and palate. In: Bzoch KR, editor. Radiographic assessment of velopharyngeal function for speech. 5th ed. Boston: Little & Brown; 2004. [Google Scholar]
- 13.Ysunza A, Pamplona M, Femat T, Mayer I, Garcia-Velaso M. Videonasopharyngoscopy as an instrument for visual biofeedback during speech in cleft palate patients. Int J Pediatr Otorhinolaryngol. 1997;41(3):291–298. doi: 10.1016/s0165-5876(97)00096-7. [DOI] [PubMed] [Google Scholar]