Abstract
This in vitro study evaluated the tensile bond strength of glass fiber posts (Reforpost – Angelus-Brazil) cemented to root dentin with a resin cement (RelyX ARC – 3M/ESPE) associated with two different adhesive systems (Adper Single Bond - 3M/ESPE and Adper Scotchbond Multi Purpose (MP) Plus – 3M/ESPE), using the pull-out test. Twenty single-rooted human teeth with standardized root canals were randomly assigned to 2 groups (n=10): G1- etching with 37% phosphoric acid gel (3M/ESPE) + Adper Single Bond + #1 post (Reforpost – Angelus) + four #1 accessory posts (Reforpin – Angelus) + resin cement; G2- etching with 37% phosphoric acid gel + Adper Scotchbond MP Plus + #1 post + four #1 accessory posts + resin cement. The specimens were stored in distilled water at 37°C for 7 days and submitted to the pull-out test in a universal testing machine (EMIC) at a crosshead speed of 0.5 mm/min. The mean values of bond strength (kgf) and standard deviation were: G1- 29.163 ± 7.123; G2- 37.752 ±13.054. Statistical analysis (Student's t-test; α=0.05 showed no statistically significant difference (p<0.05) between the groups. Adhesive bonding failures between resin cement and root canal dentin surface were observed in both groups, with non-polymerized resin cement in the apical portion of the post space when Single Bond was used (G1). The type of adhesive system employed on the fiber post cementation did not influence the pull-out bond strength.
Keywords: Dental dowels, Dentin-bonding agents, Tensile strength
INTRODUCTION
The maintenance of teeth in the mouth is a primary goal of dentistry. In cases of large destruction, due to caries or accidental fracture, preservation of tooth remainder is a major concern, even if the pulp tissue has been affected. Endodontics is a specialty that aims to provide, under certain conditions, the maintenance of teeth whose pulp vitality has been irreversibly compromised13.
Endodontically treated teeth can be restored either directly or indirectly, and usually require the use of an intracanal retainer, such as metallic post and core. One of the main reasons for the use of intracanal metallic post and core, though mistaken, is reinforce the root structure13. In addition to being unaesthetic, metallic posts present low resilience and do not accompany the modulus of elasticity of dentin. The development of resin posts reinforced with glass or carbon fiber came to minimize the difference between the modulus of elasticity of the restorative material and that of root remnant, thus avoiding root fractures. Fiber posts are considered an alternative to metallic post and core in the restoration of endodontically treated teeth12.
Posts are usually cemented with resin cements associated with adhesive systems, which has increased the interest in studying bonding to root canal dentin7. The association of adhesive systems to resin cements promotes a more effective union to root dentin, being thus a relevant factor in adhesive cementation. Proper selection of the adhesive system might directly influence the retention of intracanal posts6,9.
It is known that autopolymerizing resins are not compatible with most conventional 2-step etch-and-rinse adhesive systems. This is due to the fact that these adhesive systems have in their composition an acidic monomer that, when in contact with autopolymerizing resins, react with tertiary amines and inhibit the activation of the polymerization reaction14. Such incompatibility also occurs with dual or chemically cured resin cements, and is also very common during fiber post cementation with resin cements. In the apical region, the adhesive system is not completely polymerized by light activation, and residual unreacted acidic monomers might interfere with the union with the cement. The durability of adhesive cementation depends on the interaction between the adhesive system and the root dentin, the resin cement and the post8.
This in vitro study evaluated the tensile bond strength of glass fiber posts cemented to root dentin with a resin cement associated with two different adhesive systems, using the pull-out test.
MATERIAL AND METHODS
Twenty extracted single-rooted human teeth were used in this study, after approval by the Ethics in Research Committee of Hospital for Rehabilitation of Craniofacial Anomalies of University of São Paulo (HRAC/USP) (#022/ 2005-UEO-CEP).
The root canals were prepared and obturated with guttapercha cones and Sealer AH 26 endodontic sealer (Dentsply Ind. e Com. Ltda., Rio Janeiro, RJ, Brazil). The crowns were sectioned coronally 2 mm from the cementoenamel junction with a #3203 diamond bur (KG Sorensen, São Paulo, SP, Brazil) positioned perpendicularly to the long axis of the tooth under copious water cooling. Roots were then prepared for post insertion. The canal space of each root was standardized and enlarged with diamond burs #4138 and #4137 (KG Sorensen) to a final depth of 13 mm from the cervical surface. The specimens were randomly assigned to 2 groups (n=10) based on the types of adhesive system used in association with Rely X ARC (3M/ESPE, St. Paul, MN, USA) dual cured resin cement: Group 1 - Adper Single Bond (3M/ESPE); Group 2 - Adper Scotchbond Multi Purpose (MP) Plus (3M/ESPE).
In both groups, one main #1 fiber-post (Reforpost; Angelus, Londrina, PR, Brazil) (1.1 mm diameter) and four accessory #1 fiber-posts (Reforpin; Angelus) were prepared following the manufacturer's instructions. They were cleaned with alcohol and then silanated (Silano Angelus) for 1 min. The adhesive systems of each group were applied on the posts and light-cured for 20 s with a halogen light (Optilight Plus; Gnatus, Ribeirão Preto, SP, Brazil).
Root dentin were etched with 37% phosphoric acid (3M/ESPE) for 15 s, rinsed with water for 30 s and dried with absorbent paper points, for both groups. Adhesive systems were applied with a microbrush according the manufacturers' instructions.
After preparation of root dentin, the resin cement was mixed following the manufacturer's recommendations and placed with a lentulo spiral drill into the canal. Finally, the main post was inserted in the canal followed by four accessory posts and light-cured for 40 s through the fiber posts. Once the posts were placed, the coronal portion was reconstructed with composite resin (Filtek Z-250; 3M/ESPE), using a cylindrical stainless steel mold, in such a way to allow the performance of the pull-out test (Figure 1). Tooth surface was neither etched nor treated with adhesive, before coronal reconstruction with composite resin.
FIGURE 1. Specimen after post cementation and coronal reconstruction.
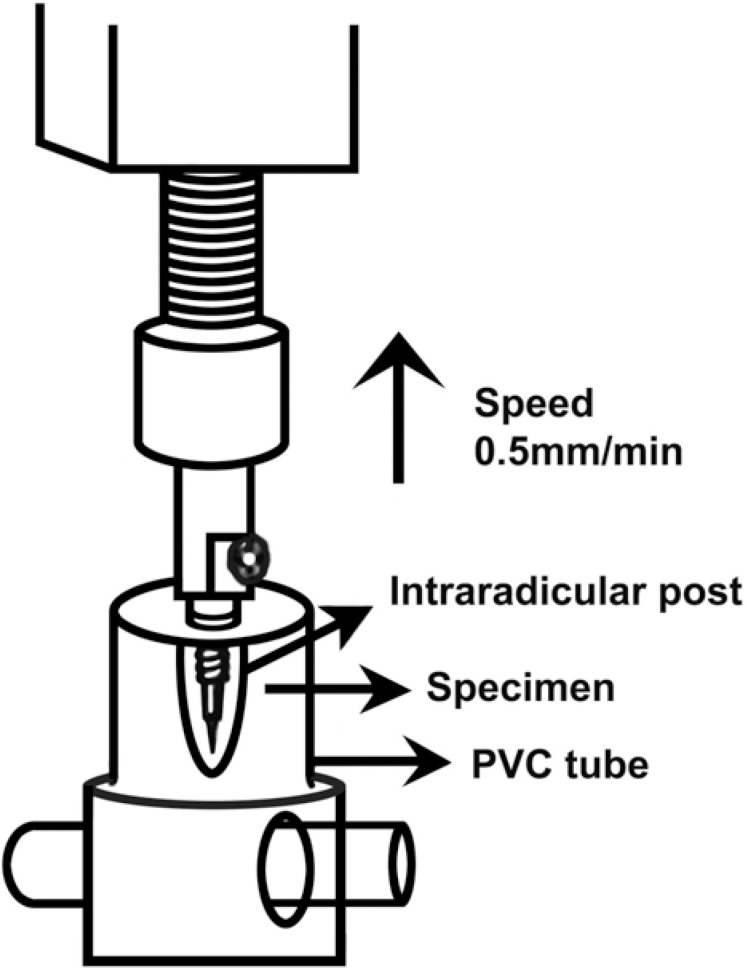
Teeth were stored in distilled water at 37°C for 24 h, and then embedded in epoxy resin using PVC cylinders as molds. After 1 week, the specimens were submitted to a pull-out test in a universal testing machine (Emic DL500; Emic Equipamentos e Sistemas de Ensaios, São José dos Pinhais, PR, Brazil) at a cross-head speed of 0.5 mm/min (Figure 2).
FIGURE 2. Schematic presentation of the pull-out test, showing the machine and the specimen.
Data were analyzed statistically by Student's t-test at 5% significance level.
RESULTS
The mean values of tensile bond strength (kgf) and standard deviation were: G1-29.163 ±7.123; G2-37.752 ±13.054. No statistically significant difference (p>0.05) was observed between the groups.
Fiber posts cemented with resin cement RelyX ARC and Adper Scotchbond MP Plus (3M ESPE) (G2) and Adper Single Bond (3M ESPE) (G1) showed similar tensile bond strength.
DISCUSSION
The bonding characteristics of prepared root dentin may vary in terms of the optimal moisture content required for application of some etch-and-rinse adhesive systems, the peculiar hydration conditions of root canal dentin due to pulp removal, the type of agent used for surface conditioning, the ability to achieve a reasonable degree of conversion when light-cured adhesive systems are polymerized at the entrance of post spaces, and potential for relief of polymerization shrinkage stresses during the setting of resin cements. There is also the action of endodontic irrigants, such as sodium hypochlorite and hydrogen peroxide, eugenol-containing sealers, and the heat generated from warm gutta-percha compaction techniques, which may influence the quality of intraradicular dentin hybridization. The chemical and physical properties of posts are variables that can also be included7,11.
In order to evaluate the retention of fiber posts cemented with resin cement, the main focus of this study was directed to the application of adhesive systems with different characteristics to the root dentin walls. The tested materials were a two-step etch-and-rinse adhesive system with acid pH, which could influence negatively the polymerization of the dual-cured resin cement, and a three-step etch-and-rinse adhesive system that, as found in literature, would not influence the polymerization. Except for distilled water, no irrigant was used to avoid any interference in the bonding process.
Cavity configuration factor (C-factor) is defined as the ratio of the bonded surface area in a cavity to the unbonded surface area4. In root canals, the C-factor is highly unfavorable and contributes to maximize the polymerization stress of resin cements along the root canal walls. With light-cured materials, the curing stress generated in areas of high C-factors may be so intense that the composite resin layer detaches from the dentin walls, thus creating interfacial gaps7·9. The volumetric shrinkage ranges from 1.5 to 5%, resulting on internal stresses that are transferred to the dentin/resin interface as pull-out forces5. In high C-factors areas, self- and slow-curing materials can reduce stresses on the bonding interface by allowing better flow of the resin cement and relief of polymerization shrinkage2,15. Alster, et al.1 (1997) showed that the difficulty in resin cement setting within the canal space generates stresses at the bonding interface.
In this study, root canal diameter was standardized before post cementation. Accessory posts of the same manufacturer were used to minimize the quantity of resin cement and C-factor and to promote a better frictional retention with dentin walls, which mitigates the influence of volumetric shrinkage and C-factor.
According to Pirani, et al.11 (2005), it is most likely that the clinical success of bonded fiber posts is predominantly due to frictional retention to post space walls, rather than to adhesive bonding. This frictional retention may occur due to water sorption that induces expanding of resin cement10.
Although no significant difference was observed between the pull-out bond strengths of the groups, Group 1 specimens (Adper Single Bond) presented non-polymerized resin cement in apical portion, in agreement with Tay, et al.14 (2003), who showed an incompatibility between acidic monomers present in the outer surface of oxygen-inhibited layer of the adhesive system and tertiary amines of the resin cement that was not completely polymerized. In addition, the post space depth usually exceeds the depth of cure achieved by most light-curing units, which is an issue of concern when a light-cured adhesive system is used for bonding to radicular dentin11.
Hybridization of intraradicular dentin, as shown by Pirani, et al.11 (2005), is a phenomenological manifestation of resin infiltration following smear layer dissolution and partial root dentin demineralization. This hybridization is not essential for the integrity of coronal sealing or resistance to dislodgement of restorations, which may be one of the reasons for the lack of statistically significant difference between the groups evaluated in the present study.
The non-uniform adaptation of the adhesive material or its incomplete polymerization, both related to the difficult access to root canal space, may account for the lower bond strengths of the adhesive cements to the middle and apical root dentin7.
The use of adhesive systems associated with resin cements and pre-fabricated posts is limited by factors inherent to the contemporary materials as well as to the characteristics of the substrates to which they are applied2. In the present study, two different light-cured adhesive systems used for adhesive cementation of glass fiber posts to root canal walls presented similar behavior under pull-out testing.
CONCLUSIONS
The type of adhesive system employed on the fiber post cementation did not influence the pull-out bond strength.
ACKNOWLEDGEMENTS
We are grateful to Dr. Maria Teresa Atta for advice and assistance with data analysis. We thank ANGELUS Produtos Odontológicos (Brasil) and 3M/ESPE (Brasil) for supplying the products used in this study.
REFERENCES
- 1.Alster D, Feilzer AJ, Gee AJ, Davidson CL. Polymerization contraction stress in thin resin composite layers as a function of layer thickness. Dent Mater. 1997;13(3):146–150. doi: 10.1016/S0109-5641(97)80115-7. [DOI] [PubMed] [Google Scholar]
- 2.Bouillaguet S, Troesch S, Wataha JC, Krejci I, Meyer JM, Pashley DH. Microtensile bond strength between adhesive cements and root canal dentin. Dent Mater. 2003;19(3):199–205. doi: 10.1016/s0109-5641(02)00030-1. [DOI] [PubMed] [Google Scholar]
- 3.Carvalho RM, Pereira JC, Yoshiyama M, Pashley DH. A review of polymerization contraction: the influence of stress development versus stress relief. Oper Dent. 1996;21(1):17–24. [PubMed] [Google Scholar]
- 4.Feilzer AJ, Gee AJ, Davidson CL. Setting stresses in composite resin in relation to configuration of the restoration. J Dent Res. 1987;66(11):1636–1639. doi: 10.1177/00220345870660110601. [DOI] [PubMed] [Google Scholar]
- 5.Ferracane JL. Developing a more complete understanding of stresses produced in dental composites during polymerization. Dent Mater. 2005;21(1):36–42. doi: 10.1016/j.dental.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 6.Ferrari M, Mannocci F. A "one-bottle" adhesive system for bonding a fibre post into a root canal: a SEM evaluation of the post-resin interface. Int Endod J. 2000;33(4):397–400. doi: 10.1046/j.1365-2591.2000.00310.x. [DOI] [PubMed] [Google Scholar]
- 7.Goracci C, Tavares AU, Fabianelli A, Monticelli F, Raffaelli O, Cardoso PC, et al. The adhesion between fiber posts and root canal walls: comparison between microtensile and push-out bond strength measurements. Eur J Oral Sci. 2004;112(4):353–361. doi: 10.1111/j.1600-0722.2004.00146.x. [DOI] [PubMed] [Google Scholar]
- 8.Hofmann N, Papsthart G, Hugo B, Klaiber B. Comparison of photo-activation versus chemical or dual-curing of resin-based luting cements regarding flexural strength, modulus and surface hardness. J Oral Rehab. 2001;28:1022–1028. doi: 10.1046/j.1365-2842.2001.00809.x. [DOI] [PubMed] [Google Scholar]
- 9.Mannocci F, Bertelli E, Watson TF, Ford TP. Resin-dentin interfaces of endodontically-treated restored teeth. Am J Dent. 2003;16(1):28–32. [PubMed] [Google Scholar]
- 10.Ortengren U, Wellendorf H, Karlsson S, Ruyter IE. Water sorption and solubility of dental composites and identification of monomers released in an aqueous environment. J Oral Rehabil. 2001;28(12):1106–1115. doi: 10.1046/j.1365-2842.2001.00802.x. [DOI] [PubMed] [Google Scholar]
- 11.Pirani C, Chersoni S, Foschi F, Piana G, Loushine RJ, Tay FR, et al. Does hybridization of intraradicular dentin really improve fiber post retention in endodontically treated teeth? J Endod. 2005;31(12):891–894. doi: 10.1097/01.don.0000164853.92310.e7. [DOI] [PubMed] [Google Scholar]
- 12.Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: a literature review. J Endod. 2004;30(5):289–301. doi: 10.1097/00004770-200405000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Shillinburg HT, Hobo S, Whitsett LD, Jacobi R, Bracket SE. Fundamentals of fixed prosthodontics. Ilinois: Quintessence Publishing Company; 1997. Carol Stream. [Google Scholar]
- 14.Tay FR, Pashley DH, Yiu CK, Sanares AM, Wei SH. Factors contributing to the incompatibility between simplified-step adhesives and chemically-cured or dual-cured composites. Part I. Single-step self-etching adhesive. J Adhes Dent. 2003;5(1):27–40. [PubMed] [Google Scholar]
- 15.Tay FR, Loushine RJ, Lambrechts P, Weller RN, Pashley DH. Geometric factors affecting dentin bonding in root canals: a theoretical modeling approach. J Endod. 2005;31(8):584–589. doi: 10.1097/01.don.0000168891.23486.de. [DOI] [PubMed] [Google Scholar]