Abstract
The purpose of this study was to evaluate the radiopacity of 5 root-end filling materials (white MTA-Angelus, grey MTA-Angelus, IRM, Super EBA and Sealer 26). Five specimens (10 mm diameter X 1 mm thickness) were made from each material and radiographed next to an aluminum stepwedge varying in thickness from 2 to 16 mm. Radiographs were digitized and the radiopacity of the materials was compared to that of the aluminum stepwedge using VIXWIN 2000 software in millimeters of aluminum (mm Al). Data were analyzed statistically by ANOVA and Tukey's test at 5% significance level. Radiopacity values varied from 3 mm Al to 5.9 mm Al. Sealer 26 and IRM presented the highest radiopacity values (p<0.05), while white/grey MTA and Super EBA presented the lowest radiopacity values (p<0.05). The tested root-end filling materials presented different radiopacities, white/grey MTA and Super EBA being the least radiopaque materials.
Keywords: Radiopacity, Retrograde obturation, Root canal filling materials, Radiology
INTRODUCTION
Retrograde filling is an endodontic surgical procedure frequently used to seal the root canal following root-end resection22,24. The root-end filling material should present sufficient radiopacity to be distinguished from adjacent anatomical structures16,18, such as bone and teeth.
In recent years, materials used in root-end fillings have greatly evolved. Silver amalgam, previously used, is no longer recommended due to clinical failure, poor marginal adaptation and inadequate sealing10. Other materials currently in use include root canal sealers11,17, zinc oxideeugenol-based materials4,7,26 and mineral trioxide aggregate (MTA)24,25.
Since their introduction by Grossman in 1936, zinc oxide-eugenol-based materials have been widely used in dentistry. IRM (Dentsply Caulk, Milford, DE, USA) is a polymethylmethacrylate-reinforced zinc oxide-eugenol cement that is indicated for use as a root-end filling material12,26. Super EBA (Harry J Bosworth Co, IL, USA) is another modified zinc oxide-eugenol cement used for filling of retrograde cavities. Its liquid contains 68% ethoxybenzoic acid and 32% eugenol, presenting as advantages a good sealing, low leakage levels2 and good tissue tolerance4,15.
Various materials have been studied for use as root-end filling materials. Gerhards and Wagner11 used Diaket, an epoxy resin-based sealer, in retrograde fillings, and reported a satisfactory apical seal. Sealer 26 (Denstply Indústria e Comércio Ltda., Petrópolis, RJ, Brazil) is an epoxy resin-based endodontic sealer that presents bismuth oxide and calcium hydroxide in its formulation. A greater powder-to-resin ratio is used to obtain a thicker consistency for use in retrograde fillings. Sealer 26 is known for its excellent sealing properties when used for either root canal filling or retrograde obturation17. Tanomaru-Filho, et al.22 have observed good periapical healing in dogs after retrograde filling with Sealer 26, similar to that obtained with MTA.
MTA has been considered as the ideal root-end filling material because of its low solubility, low cytotoxicity, good tissue tolerance and possible induction of mineralized tissue formation25. MTA-Angelus (Angelus, Londrina, PR, Brazil) is produced from Portland cement with addition of bismuth oxide to increase radiopacity. Its properties, in terms of increasing pH and releasing calcium ions, are similar to those of Pro Root™ MTA (Dentsply Tulsa Dental, Tulsa, OK), as previously demonstrated by Duarte, et al.8.
Eliasson and Haaskel9 have established a comparison standard for radiopacity studies using optical density values for impression materials and calculating the equivalent thickness of aluminum required to result in similar radiographic density. Tagger and Katz19 developed a method to measure radiopacity that includes obtaining radiographic images of materials next to an aluminum stepwedge. This method also involves digitization of the radiographs and use of specific software to determine the grey pixel values.
The purpose of this study was to evaluate the radiopacity of 5 root-end filling materials by comparing the radiopacity of samples to that of an aluminum stepwedge, according to the ISO 6876:2001 standard13.
MATERIAL AND METHODS
Five root-end filling materials were evaluated in this study: white MTA-Angelus, grey MTA-Angelus, IRM, Super EBA and Sealer 26 (Table 1).
TABLE 1. Tested materials and compositions.
| Material | Composition |
|---|---|
| White MTA-Angelus | 80% Portland cement and 20% bismuth oxide |
| Grey MTA-Angelus | 80% Portland cement and 20% bismuth oxide |
| IRM | Powder: 75% zinc oxide and 15% polymethylmethacrylate |
| Liquid: 99% eugenol and 1% acetic acid | |
| Super EBA | Powder: zinc oxide |
| Liquid: 68% ethoxybenzoic and 32% eugenol | |
| Sealer 26 | Powder: 43% bismuth oxide, 37% calcium hydroxide, 14% hexamethylenetetramine and 5% titanium dioxide Paste B: bisphenol epoxy resin |
All materials were prepared according to the manufacturers' instructions, except for Sealer 26. As this material is a resin-based root canal sealer, a thicker consistency is necessary for filling of retrograde cavities and thus a 4:1 powder-to-resin weight ratio was used22. For specimen preparation, impressions were taken from metallic matrices using a light-bodied silicone-based impression material. The moulds were filled with the tested materials and stored in a moist incubator at 37°C until complete set of the cements. Five specimens measuring 10 mm diameter and 1 mm thickness were fabricated from each material.
Thereafter, the specimens were placed on 5 occlusal radiographic films (Insight; Kodak Comp, Rochester, NY, USA) next to a graduated aluminum stepwedge with thickness ranging from 2 to 16 mm (in 2 mm-increments) and exposed using a GE-1000 x-ray unit (General Electric, Milwaukee, WI, USA) operating at 50 kv, 10 mA, 18 pulses/s, and focus-film distance of 33.5 cm. The radiographs were digitized using a desktop scanner (SnapScan 1236; Agfa, Deutschland) and the digitized images were imported into the VIXWIN 2000 software (Gendex, Deplanes, IL, USA). The equal-density tool of this software was used to identify areas of equal density, allowing comparison between the radiographic density of the materials and the radiopacity of different thicknesses of the aluminum stepwedge. By double-clicking the left mouse button, the area corresponding to the specimen was selected in each radiographic image and the software determined which thickness of the aluminum stepwedge was equivalent to the specimen's radiographic density. This assessment determined the radiopacity of the selected material compared to a particular thickness of aluminum, measured in millimeters. Results were analyzed by calculating the means of 5 measurements per sample (one point in the central area and 4 points in the different quadrants). Data were submitted to statistical analysis using one-way analysis of variance (ANOVA) and Tukey's HSD post-hoc test (á=0.05).
RESULTS
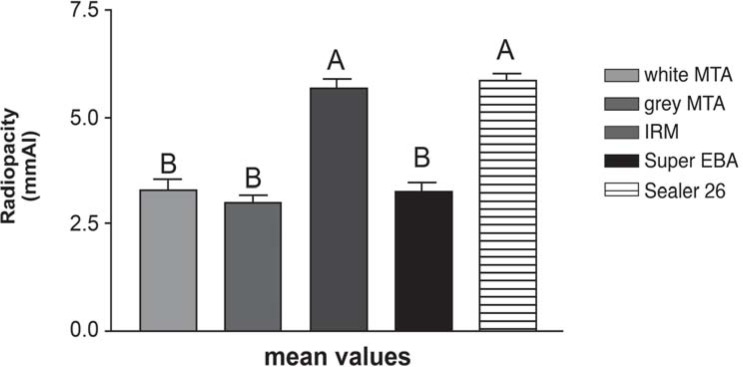
The radiopacity values are presented in Figure 1. Sealer 26 and IRM presented the highest radiopacity values among the tested materials (p<0.05), equivalent to 5.9 mm Al and 5.7 mm Al, respectively. White/grey MTA and Super EBA presented the lowest radiopacity values (p<0.05), ranging from 3 to 3.3 mm Al.
FIGURE 1. Radiopacity means and standard deviation of the tested materials and results of Tukey's HSD post-hoc test (α=0.05). Different letters indicate statistically significant difference at 5% significance level.
DISCUSSION
Tagger and Katz19 developed a method for analysis of the radiopacity of endodontic sealers using standardized samples radiographed next to an aluminum stepwedge. The radiographs are digitized and the specimens' radiopacity is compared to that of the aluminum stepwedge using computer software. The comparative evaluation of digitized radiographic images using an image-analysis software has been shown to determine the radiopacity of the materials in a simple and easily reproducible manner with reliable outcomes18,20,21.
Several radiopacity studies have included comparison to an aluminum stepwedge with varying thickness. Katz, et al.14 compared the radiopacity of gutta-percha cones to an aluminum stepwedge and observed a mean radiopacity of 7.4 mm Al. Tanomaru, et al.20 evaluated the radiopacity of root canal sealers using a similar methodology. Beyer-Olsen and Orstavik5 evaluated the radiopacity of several root canal sealers using an aluminum stepwedge with 2-mm increments in thickness and found that most analyzed materials were more radiopaque than dentin. The ISO 6876:2001 standard13 establishes 3 mm Al as the minimum radiopacity for root canal sealers. According to the ANSI/ADA specification No. 571, root canal sealers should be at least 2 mm Al more radiopaque than bone or dentin.
Shah, et al.16 have stated that root-end filling materials should be distinguishable from the adjacent bone and root dentin, and that materials with radiopacity values smaller than 3 mm Al are indistinguishable. According to these authors16, an international standardization establishing the minimum acceptable radiopacity of root-end filling materials is urgently needed. Likewise, Tagger and Katz18 have emphasized that the establishment of international guidelines is strongly recommended to standardize the minimum radiopacity for retrograde filling materials, due to the great variability observed in the currently used materials.
In the present study, Sealer 26 and IRM had the highest radiopacity values. This may be explained by the fact that Sealer 26 powder has bismuth oxide, which is responsible for its radiopacity, while 75% of IRM composition is zinc oxide, which confers radiopacity to this material.
Super EBA and both types of MTA were the least radiopaque materials. White/grey MTA-Angelus presented radiopacity between 3 to 3.3 mm Al. Bismuth oxide is added to the formulation of these materials to provide radiopacity. Despite the addition of bismuth oxide to its composition (Table 1), the value of radiopacity observed is close to the minimum required by ISO 6876/2001 standard ANSI/ADA Specification No.57 for root canal filling materials.
In the present study, there was no statistically significant difference between both types of MTA regarding their radiopacity. According to Asgary, et al.3, the major difference seems to be in FeO concentration, with considerably lower values in the white compared to the grey MTA. Differences in FeO concentration are thought to be primarily responsible for color variation of the white MTA compared to the grey MTA. Camilleri, et al.6 have verified a similar chemical composition for grey and white MTA. Both materials were found to be nontoxic, and both induced cell proliferation when hydrated.
Super EBA presented radiopacity similar to that of white/grey MTA. This result differs from those of Torabinejad, et al.23, who evaluated several retrofilling materials and concluded that amalgam was the most radiopaque material and that MTA had higher radiopacity values than Super EBA and IRM.
CONCLUSIONS
Under the tested conditions and according to the results of the present study, it may be concluded that the tested root-end filling materials had different radiopacities. White/grey MTA and Super EBA were the least radiopaque materials.
REFERENCES
- 1.American Dental Association. Specification No. 57 for endodontic filling materials. J Am Dent Assoc. 1984;108:88–88. [Google Scholar]
- 2.Aqrabawi J. Sealing ability of a amalgam, super EBA cement and MTA when used as retrograde filling materials. Br Dent J. 2000;188:266–268. doi: 10.1038/sj.bdj.4800450. [DOI] [PubMed] [Google Scholar]
- 3.Asgary S, Parirokh M, Eghbal MJ, Brink F. Chemical differences between white and grey mineral trioxide aggregate. J Endod. 2005;31:101–103. doi: 10.1097/01.don.0000133156.85164.b2. [DOI] [PubMed] [Google Scholar]
- 4.Bernabé PFE, Holland R, Morandi R, Souza V, Nery MJ, Otoboni JA, Filho, et al. Comparative study od MT and other materials in retrofilling of pulpless dog's teeth. Braz Dent J. 2005;16:149–145. doi: 10.1590/s0103-64402005000200012. [DOI] [PubMed] [Google Scholar]
- 5.Beyer-Olsen EM, Orstavik D. Radiopacity of root canal sealers. Oral Surg Oral Med Oral Pathol. 1981;51:320–328. doi: 10.1016/0030-4220(81)90062-1. [DOI] [PubMed] [Google Scholar]
- 6.Camilleri J, Montesin FE, Di Silvio L, Pitt Ford TR. The chemical constitution and biocompatibility of accelerated Portland cement for endodontic use. Int Endod J. 2005;38:834–842. doi: 10.1111/j.1365-2591.2005.01028.x. [DOI] [PubMed] [Google Scholar]
- 7.Chong BS, Pitt Ford TR, Hudson MB. A prospective clinical study of Mineral Troxide Aggregate and IRM when used as root-end filling materials in endodontic surgery. Int Endod J. 2003;36:520–526. doi: 10.1046/j.1365-2591.2003.00682.x. [DOI] [PubMed] [Google Scholar]
- 8.Duarte MAH, Demarchi ACCO, Yamashita JC, Kuga MC, Fraga SC. pH and calcium ion release of 2 root-end filling materials. Oral Surg Oral Med Oral Pathol. 2003;95:345–347. doi: 10.1067/moe.2003.12. [DOI] [PubMed] [Google Scholar]
- 9.Eliasson ST, Haasken B. Radiopacity of impression materials. Oral Surg Oral Med Oral Pathol. 1979;47:485–491. doi: 10.1016/0030-4220(79)90136-1. [DOI] [PubMed] [Google Scholar]
- 10.Frank LA, Glick DH, Patterson SS, Weine FS. Long term evaluation of surgically placed amalgam fillings. J Endod. 1992;18:391–398. doi: 10.1016/s0099-2399(06)81226-4. [DOI] [PubMed] [Google Scholar]
- 11.Gerhards F, Wagner W. Sealing ability of five different retrograde filling materials. J Endod. 1996;22:463–466. doi: 10.1016/S0099-2399(96)80078-1. [DOI] [PubMed] [Google Scholar]
- 12.Harrison JW, Johnson SA. Excisional wound healing following the use of IRM as a root-end filling material. J Endod. 1997;23:19–27. doi: 10.1016/S0099-2399(97)80201-4. [DOI] [PubMed] [Google Scholar]
- 13.International Organization for Standardization. ISO 6876: dental root sealing materials. Geneva: The Organization; 2001. [Google Scholar]
- 14.Katz A, Kaffe I, Littner M, Tagger M, Tamse A. Densitometric measurement of radiopacity of gutta-percha cones and root dentin. J Endod. 1990;16:211–213. doi: 10.1016/S0099-2399(06)81671-7. [DOI] [PubMed] [Google Scholar]
- 15.Pitt Ford TR, Andreasen JO, Dorn SO, Kariyawasam SP. Effect of Super EBA as a root-end filling on healing after replantation. J Endod. 1995;21:13–15. doi: 10.1016/s0099-2399(06)80550-9. [DOI] [PubMed] [Google Scholar]
- 16.Shah PMM, Chong BS, Sidhu SK, Ford TRP. Radiopacity of potential root-end filling materials. Oral Surg Oral Med Oral Pathol. 1996;81:476–479. doi: 10.1016/s1079-2104(96)80028-x. [DOI] [PubMed] [Google Scholar]
- 17.Siqueira JF, Jr, Roças IN, Abad EC, Castro AJ, Gabyva SMM, Favieri A. Ability of three root-end filling materials to prevent bacterial leakage. J Endod. 2001;27:673–675. doi: 10.1097/00004770-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Tagger M, Katz A. A standard for radiopacity of root-end (retrograde) filling materials is urgently needed. Int Endod J. 2004;37:260–264. doi: 10.1111/j.0143-2885.2004.00787.x. [DOI] [PubMed] [Google Scholar]
- 19.Tagger M, Katz A. The radiopacity of endodontic sealers: development of a new method for direct measurement. J Endod. 2003;29:751–755. doi: 10.1097/00004770-200311000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Tanomaru JMG, Cezare L, Gonçalves M, Tanomaru M., Filho Evaluation of the radiopacity of root canal sealers by digitalization of radiographic images. J Appl Oral Sci. 2004;12:355–357. doi: 10.1590/s1678-77572004000400019. [DOI] [PubMed] [Google Scholar]
- 21.Tanomaru M, Filho, Jorge EG, Guerreiro-Tanomaru JM, Gonçalves M. Radiopacity evaluation of new root canal filling materials by digitalization of images. J Endod. 2007;33:249–251. doi: 10.1016/j.joen.2006.08.015. [DOI] [PubMed] [Google Scholar]
- 22.Tanomaru M, Filho, Luis MR, Leonardo MR, Tanomaru JMG, Silva LAB. Evaluation of periapical repair following retrograde filling with different root-end filling materials in dog teeth with periapical lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:127–132. doi: 10.1016/j.tripleo.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 23.Torabinejad M, Hong CU, McDonald F, Pitt Ford TR. Physical and chemical properties of a new a root-end filling material. J Endod. 1995;21:349–353. doi: 10.1016/S0099-2399(06)80967-2. [DOI] [PubMed] [Google Scholar]
- 24.Torabinejad M, Pitt Ford TR, McKendry DJ, Abedi HR, Miller DA, Kariyawasam SP. Histologic assessment of mineral trioxide aggregate as a root-end filling in monkeys. J Endod. 1997;23:225–228. doi: 10.1016/S0099-2399(97)80051-9. [DOI] [PubMed] [Google Scholar]
- 25.Torabinejad M, Pitt Ford TR. Root end filling materials: a review. Endod Dent Traumatol. 1996;12:161–178. doi: 10.1111/j.1600-9657.1996.tb00510.x. [DOI] [PubMed] [Google Scholar]
- 26.Walivaara DA, Abrahamsson P, Isakssom S, Blomqvist JE, Samfors KA. Prospective study of periapically infected teeth treated with periapical surgery including ultrasonic preparation and retrograde intermediate restorative material rot-end fillings. J Oral Maxillofac Surg. 2007;65:931–935. doi: 10.1016/j.joms.2005.12.077. [DOI] [PubMed] [Google Scholar]