Abstract
Background A triangular fibrocartilage complex (TFCC) injury can produce distal radioulnar joint (DRUJ) instability. If the foveal attachment is avulsed, it translates distally. The footprint is separated from its origin and will become covered in synovitis, preventing healing. The authors describe a surgical technique for the treatment of instability of the DRUJ due to chronic foveal detachment of the TFCC.
Technique The procedure utilizes a loop of autologous palmaris longus tendon graft passed through the ulnar aspect of the TFCC and through an osseous tunnel in the distal ulna to reconstruct the fovel attachment.
Patients and Methods We report on nine patients with a mean age of 42. Median follow-up was 13 months.
Results The median pain scores measured were reduced from 8 to 3 postoperatively, and all had a stable DRUJ.
Conclusions This technique provides stability of the distal ulna to the radius and carpus, with potential for biologic healing through osseous integration. It is a robust, anatomically based reconstruction of the TFCC to the fovea that stabilizes the DRUJ and the ulnar-carpal sag.
Keywords: triangular fibrocartilage complex, foveal tear, DRUJ instability
The triangular fibrocartilage complex (TFCC) contains three components: the articular disc, the superficial and deep radioulnar ligaments, and the ulnolunate and ulnotriquetral ligaments. Secondary stabilizers include the sheath of the extensor carpi ulnaris (ECU), the distal interosseous membrane or distal oblique bundle (if present) and the pronator quadratus.1 2 As the palmar and dorsal radioulnar ligaments extend toward the ulna, each divides into two limbs: the deep limb attaches to the fovea on the ulna, and the superficial limb attaches to the base and mid-portion of the ulnar styloid. The deep palmar limb attaches to the fovea together with the ulnocapitate ligament, and the superficial palmar limb attaches to the styloid together with the ulnotriquetral ligament.3 4 5 6 The foveal insertion of the TFCC contributes more to DRUJ stability because of its closer relationship to the rotational axis of the forearm. In fractures of the tip of the ulnar styloid with disruption of only the distal components of the TFCC, patients will not experience DRUJ instability if the foveal attachment is intact.7
Palmer proposed a classification system for TFCC tears that divided them into traumatic and degenerative.8 Atzei and Luchetti recently subclassified the Palmer 1B tear into a distal component, proximal component, or both (complete) to guide treatment. Anatomic TFCC repair into the fovea is recommended for proximal or complete tears.2
Conventional repair techniques for peripheral TFCC tears involve repair to the dorsal or ulnar joint capsule. They do not reconstitute the foveal origin, and instability may persist if this is the site of primary pathology. Estrella et al reported results of a capsular repair of peripheral TFCC tears, with unsatisfactory results in 26%, of which 45% were related to persistent DRUJ instability.9 Many authors have now suggested foveal repair of the TFCC to restore DRUJ stability. The aim should be an anatomic repair to restore isometry and prevent a loss of forearm rotation due to overconstraint.
We present our foveal repair technique using an autologous palmaris longus graft. We recommend its use in chronic tears, where a repair is less likely to be successful using more conventional techniques. The procedure uses the palmaris longus tendon to secure the TFCC into the fovea through an osseous tunnel. Most current techniques described involve suture repair of the TFCC into the fovea.1 6 10 Our technique offers a theoretical advantage of osseous-tendon integration in the ulna tunnel. It stabilizes the DRUJ and the ulnar-carpal sling (Figs. 1a, b).
Fig. 1a, b.
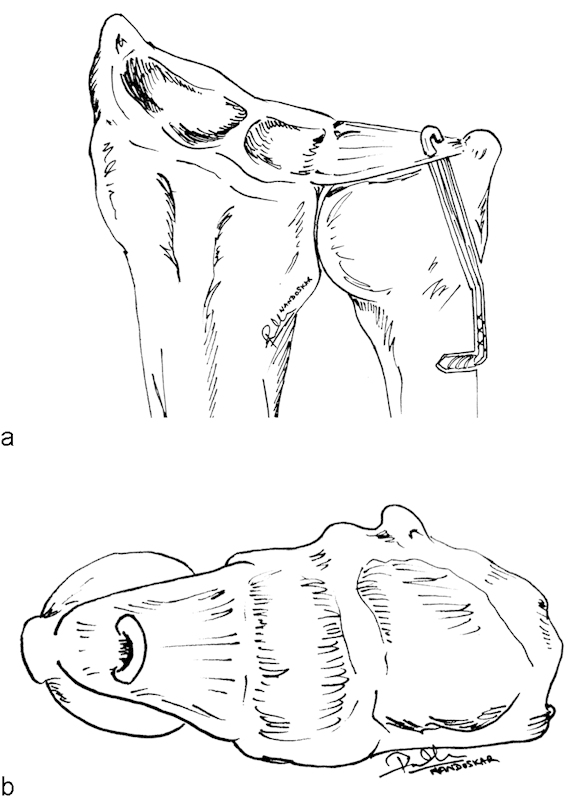
(a, b) Drawings illustrating our technique of foveal reconstruction of the TFCC. The palmaris longus tendon is passed through an osseous tunnel in the ulna, woven through the TFCC, and secured proximally to the ulna shaft with a tensionable anchor.
Anatomical Basis for Procedure
The ulnar attachment holds the TFCC down onto the fovea. The senior author proposes that the pathological/anatomical reason for the persistent instability with a foveal tear is that the entire TFCC is translated distally by the intact attachment to the carpus and radius. The foveal footprint becomes bathed in synovial fluid from the DRUJ, and synovitis forms. The persistent DRUJ instability is because the TFCC does not heal to the fovea. The authors believe that some of the published failures occur when (a) the surgeon performs a peripheral repair and fails to address the foveal attachment or (b) performs a foveal repair with a suture or suture anchor but fails to maintain the reduction of the TFCC to the footprint. The foveal reconstruction described in this paper is aimed at avoiding these two scenarios.
A foveal reconstruction can be performed in chronic cases where the TFCC is still attached to the distal radius and the carpus. If there is a small radial-sided tear of the TFCC, but the stability between the TFCC and the distal radius is maintained, then we would still proceed using this technique. A radial-sided instability of the TFCC is identified by probing the tear, utilizing the arthroscopic drawer test, and performing a “reverse hook test,” where the hook is used to translate the TFCC in the ulnar (reverse) direction. If there is an extensive unstable tear of the TFCC, then our technique of a foveal reconstruction is contraindicated. In that case a reconstruction that stabilizes the radial and ulnar aspects of the TFCC, as described by Mansat et al and by Adams and Berger would be our preferred technique.11 12
Surgical Technique
The patient is anesthetized, a tourniquet applied, and the hand suspended from finger traps from a shoulder arthroscopy frame.13 The stability of the DRUJ is assessed, and the direction of instability determined.
Arthroscopy and Examination of the TFCC
A standard wrist arthroscopy is performed through the 3/4 and the 6R portal. The TFCC is examined to obtain a detailed understanding of the tear configuration. This includes the following:
Visualization and Probing of the TFCC
A “trampoline test” will demonstrate loss of the normal tension with a TFCC tear. A hook test (where a probe is placed into the ulnar aspect of the TFCC and an attempt is made to translate the TFCC toward the radial side) will confirm an avulsion of the foveal attachment. In the normal wrist the TFCC will not translate significantly but will tend to just buckle.14
Ballottement under Arthroscopic Vision
This test includes ballottement of the DRUJ in neutral, supination, and pronation and the lunotriquetral joint.15 In the normal wrist the TFCC will be seen to ripple with a filling defect of the ulnar head below it. If the DRUJ is unstable, the translation can be seen to be much greater and extend beyond the rim of the sigmoid notch. In addition, the test may unmask a concealed tear. For example, a dorsal tear will open on volar translation of the distal ulna.
Radial-sided tears of the TFCC need to be assessed by probing and ballottement.
We use a reverse hook test, and if it is positive, there is no functional stability between the TFCC and the radius. This assessment is important because if there is a significant radial-sided tear, our technique of a foveal reconstruction is contraindicated.
DRUJ arthroscopy can be performed to visualize the foveal attachment of the TFCC directly. This is easier to perform with a foveal disruption, as it creates more space.
Surgical Approach
On different occasions we have performed this technique with a volar or a dorsal approach and an arthroscopic procedure; however, the advancement of the tendon graft through the portals and the TFCC is quite technical. We prefer the dorsal open approach, as it provides good exposure of the TFCC and fovea. In addition, if for some reason we needed to revert to the radioulnar reconstruction,15 we could do so. With advances in arthroscopic techniques for passing the tendon through the TFCC, we expect that this will become the preferred technique.
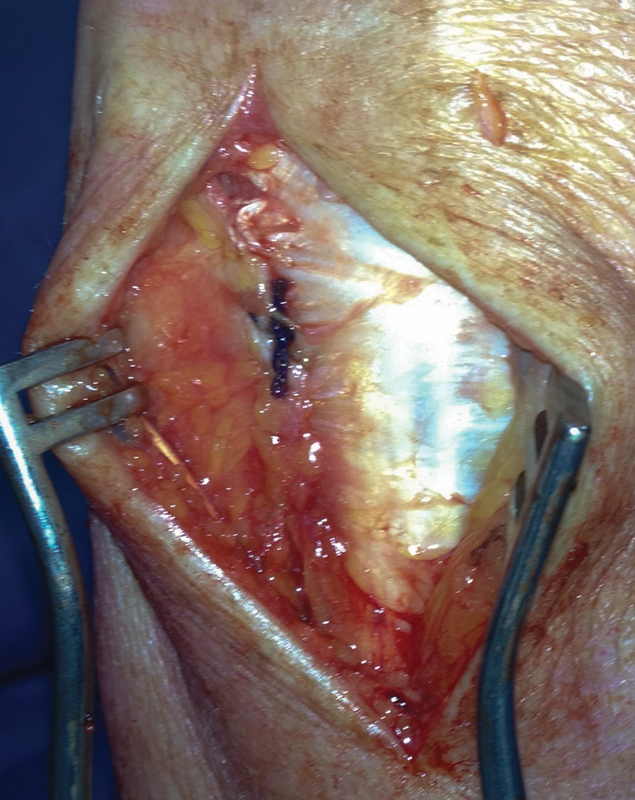
The dorsal approach is via the fifth dorsal extensor compartment. The dorsal branch of the ulnar nerve must be protected. The roof of the fifth extensor compartment is released, and the extensor digiti minimi (EDM) tendon retracted. The floor of the fifth compartment is incised longitudinally and the dorsal capsule is reflected ulnarly, to expose the proximal and distal aspects of the TFCC (Fig. 2).
Fig. 2.
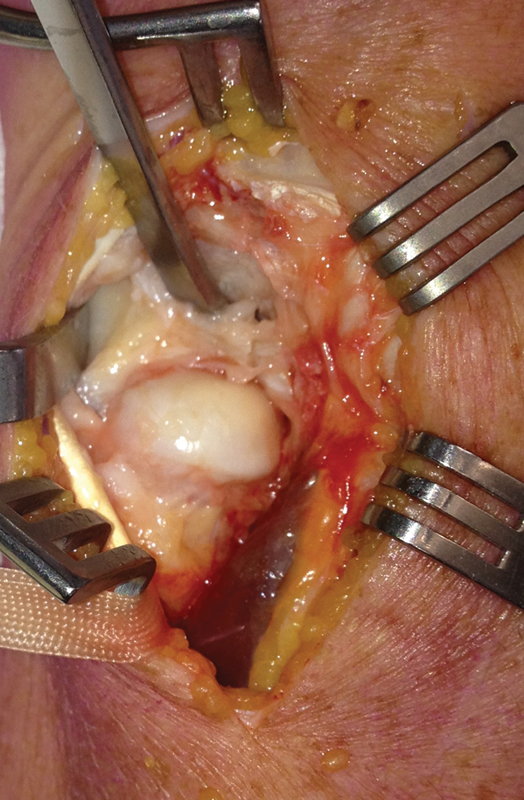
Dorsal approach to the DRUJ through the bed of the fifth extensor compartment. The Freer elevator has been placed in the ulnocarpal joint with the TFCC below it.
Distal Ulna Preparation
The foveal footprint is débrided with either a motorized resector or a curette.
A drill hole is placed into the distal ulna. Under fluoroscopic control, a guide wire is advanced from 1.5–2 cm proximal to the tip of the ulnar styloid and angled up into the fovea (Fig. 3). A 3.5-mm drill hole is made in the ulnar metaphysis. The guide wire is then advanced into this drill hole and up into the fovea.11 This makes it easier to direct the guide wire and prevents it skiving off the ulna shaft. A jig (e.g., from the Herbert screw set) can be used to ensure the correct exit point of the guide wire. A cannulated drill is advanced over the guide wire. The size of the drill hole is dependent upon the size of the palmaris longus graft when doubled upon itself (usually a 3.5-mm or 4-mm drill).
Fig. 3.
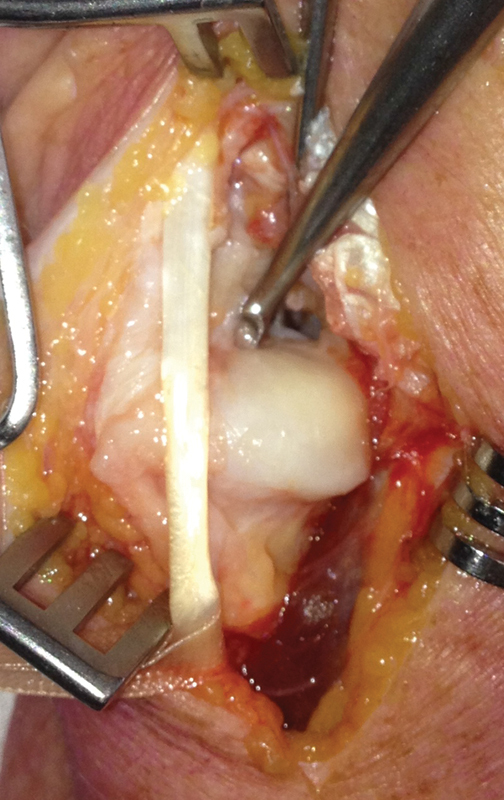
A wire is advanced from the fovea to the subcutaneous border of the ulna under direct vision. A cannulated drill is then advanced over the wire.
Placement of the Palmaris Longus Tendon Graft
The palmaris longus tendon is harvested from the volar aspect of the wrist, and grasping sutures are placed in each end of the tendon. The sutures from each end of the tendon will each be passed through the TFCC in two separate holes from distal to proximal, and through the ulnar drill hole using a suture grasper or loop (Fig. 4).
Fig. 4.
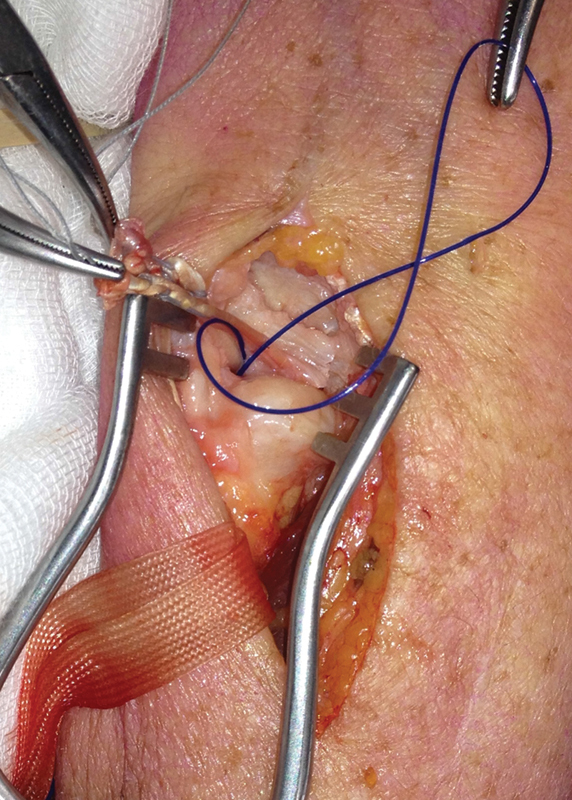
The palmaris longus graft has been passed through the TFCC. A loop of suture is passed through the ulna drill hole and is used to retrieve the suture ends, after which the graft is pulled down into the bone tunnel.
Once the sutures and graft are advanced, the graft will pull a segment of the TFCC down onto the foveal footprint, thereby stabilizing the DRUJ. In withdrawing the suture passer from the TFCC, if the grasping suture is held taut up against the aperture of the suture passer, it will deliver the tendon through the TFCC.
Our preferred technique to stabilize the graft is to secure the ends through a tensionable anchor inserted into the subcutaneous border of the ulna proximal to the drill hole. The anchor is tightened, and then the wrist and forearm are taken through a range of motion. The anchor is then further tightened, so that the viscoelastic “creep” of the tendon graft are taken up, which ensures that the graft is taut (Fig. 5a, b).
Fig. 5a, b.
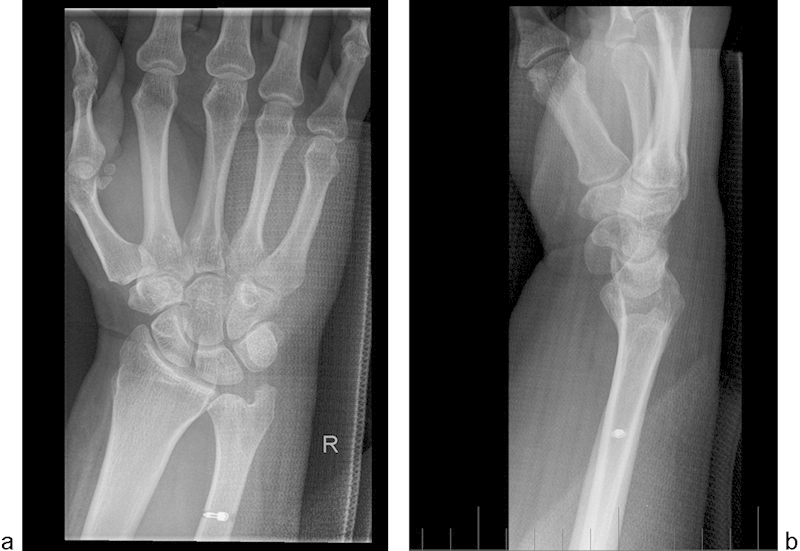
(a) AP and (b) lateral postoperative radiographs following TFCC reconstruction using a palmaris longus tendon graft secured using a tensionable suture anchor in the ulna diaphysis.
We have also used interference fit screws and Endobuttons (Smith & Nephew, Andover, MA, USA), but we no longer use these. The interference fit screws are technically the simplest; however, there is a fracture risk. The Endobutton migrates distally because of the obliquity of the ulnar hole and can be palpable.
The capsule is closed, and the patient is placed into an above-elbow cast postoperatively in neutral rotation (Fig. 6).
Fig. 6.
The dorsal capsule is plicated, which further adds stability to the DRUJ.
At the 4-week visit the above-elbow cast is removed and the patient is provided with a removable below-elbow wrist splint for a further 4 weeks. A hand therapist supervises gentle range of motion exercises. At 8 weeks the splint is discarded and full active range of motion is encouraged as well as strengthening exercises. The patient is advised not to perform any heavy lifting for 3 months.
The dorsal cutaneous branch of the ulnar nerve is at risk. There is risk of fracture to the ulnar styloid or distal ulna due to a small bone bridge. It is important to ensure that there is a bone bridge of at least 1.5 cm from the ulnar styloid to the drill hole, and considerable care is required if an interference fit screw is used to secure the tendon graft. Persistent instability would occur if the tendon graft were to cut through the TFCC, so care is required to ensure the correct placement of the graft through the TFCC and that it is adequately secured.
Postoperative Evaluation
A retrospective review was completed of the nine patients who underwent a foveal reconstruction of the TFCC using a palmaris longus graft. The median follow-up was 13 months (range 7–49 months). The average age was 43 years at the time of injury (range 23–56).
All patients had failed nonoperative treatment prior to surgery. The median time from injury to surgery was 10 months (2–42 months). The primary indication for surgery was instability of the DRUJ due to a foveal tear diagnosed clinically with a positive foveal sign16 and DRUJ ballottement test and then confirmed on MRI. Some cases did have significant pain associated with instability, but cases with pain but no instability were not offered this operation.
All patients had a foveal tear of the TFCC confirmed on arthroscopy and had an abnormal trampoline test, hook test, and ballottement under arthroscopic vision. All had an intact radial side of the TFCC, as demonstrated by a normal reverse hook test. Tendon fixation methods included anchor fixation, interference screw, and Endobutton.
Patients were assessed using a satisfaction score (out of 10), and pain score using a 0–10 visual analog scale measured on a slide rule (Astra USA Inc., Westborough, MA, USA), range of motion and clinical assessment of DRUJ stability using the ballottement test in neutral, supination, and pronation.
Results
The median satisfaction score was 8/10 (range 6–10). The median pain scores measured were reduced from 8 to 3 postoperatively. Some of the patients with persistent pain had associated injuries of the articular cartilage, scapholunate, or lunotriquetral ligaments.
Postoperatively the median extension was 75°, flexion 70°, supination 75° and pronation 85°. All DRUJs were clinically stable.
One patient had a second operative procedure for pain. A sigmoid notch osteoplasty was performed. The patient still had ongoing pain, however.
Discussion
There are currently several studies that describe foveal reattachment of the TFCC with varying success.1 6 10 17 We feel our repair technique offers increased security and osseous integration in the setting of a chronic foveal TFCC tear.
Nakamura et al described open and arthroscopic transosseous repair techniques for foveal detachment of the TFCC using a custom targeting device and sutures secured on the ulnar cortex.6 Seven of the 24 patients (29%) in the arthroscopic group and 10 of the 66 (15%) patients in the open group had persistent instability. Our technique is similar; however, we have used a tendon graft in preference to a suture. Thin suture may cut through the TFCC or rupture, leading to failure. The tendon reconstruction is technically more difficult but is robust and provides a good tendon-to-bone interface within the ulna.
Results from other studies on TFCC repair have shown more positive results than Nakamura et al achieved. In a series of 37 patients who underwent arthroscopic foveal repair with a suture anchor by Atzei, 94% of patients had excellent or good outcomes.1 17 Iwasaki et al reported 92% excellent or good outcomes following arthroscopic-assisted foveal repair using a suture in a series of 12 patients reviewed at 24 months.10 There was no instability noted.Tse et al reported 10-year follow-up of arthroscopic foveal reconstruction with autografts, with good improvements in range of motion and wrist scores, although their technique involved a graft passing through the radius and then the fovea. There was no evidence of DRUJ arthritis.18 Our technique is technically simpler but relies on an intact radial attachment of the TFCC.
Our technique of reconstruction utilizes an autologous tendon graft to secure the avulsed TFCC into the ulnar fovea. This is potentially more durable, and it allows osseous-tendon integration. In our small series, we have no residual clinical instability of the DRUJ at latest follow-up. Nakamura et al observed better results when operating within 4 months and poorer results if operated on after 7 months.6 We would add that chronicity of the injury and mixed concurrent pathology make excellent results difficult to achieve.
Footnotes
Conflict of Interest None
References
- 1.Atzei A, Luchetti R. Philadelphia, PA: Saunders; 2010. Repair of the foveal insertion of the TFCC through the DF portal; pp. 559–568. [Google Scholar]
- 2.Atzei A, Luchetti R. Foveal TFCC tear classification and treatment. Hand Clin. 2011;27(3):263–272. doi: 10.1016/j.hcl.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 3.Haugstvedt J R, Berger R A, Nakamura T, Neale P, Berglund L, An K N. Relative contributions of the ulnar attachments of the triangular fibrocartilage complex to the dynamic stability of the distal radioulnar joint. J Hand Surg Am. 2006;31(3):445–451. doi: 10.1016/j.jhsa.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 4.Moritomo H. Advantages of open repair of a foveal tear of the triangular fibrocartilage complex via a palmar surgical approach. Tech Hand Up Extrem Surg. 2009;13(4):176–181. doi: 10.1097/BTH.0b013e3181bd8319. [DOI] [PubMed] [Google Scholar]
- 5.Nakamura T, Takayama S, Horiuchi Y, Yabe Y. Origins and insertions of the triangular fibrocartilage complex: a histological study. J Hand Surg [Br] 2001;26(5):446–454. doi: 10.1054/jhsb.2001.0562. [DOI] [PubMed] [Google Scholar]
- 6.Nakamura T, Sato K, Okazaki M, Toyama Y, Ikegami H. Repair of foveal detachment of the triangular fibrocartilage complex: open and arthroscopic transosseous techniques. Hand Clin. 2011;27(3):281–290. doi: 10.1016/j.hcl.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Slutsky D J. Arthroscopic evaluation of the foveal attachment of the triangular fibrocartilage. Hand Clin. 2011;27(3):255–261. doi: 10.1016/j.hcl.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 8.Palmer A K. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14(4):594–606. doi: 10.1016/0363-5023(89)90174-3. [DOI] [PubMed] [Google Scholar]
- 9.Estrella E P Hung L K Ho P C Tse W L Arthroscopic repair of triangular fibrocartilage complex tears Arthroscopy 2007237729–737., 737.e1 [DOI] [PubMed] [Google Scholar]
- 10.Iwasaki N, Nishida K, Motomiya M, Funakoshi T, Minami A. Arthroscopic-assisted repair of avulsed triangular fibrocartilage complex to the fovea of the ulnar head: a 2- to 4-year follow-up study. Arthroscopy. 2011;27(10):1371–1378. doi: 10.1016/j.arthro.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 11.Adams B D, Berger R A. An anatomic reconstruction of the distal radioulnar ligaments for posttraumatic distal radioulnar joint instability. J Hand Surg Am. 2002;27(2):243–251. doi: 10.1053/jhsu.2002.31731. [DOI] [PubMed] [Google Scholar]
- 12.Mansat M, Mansat C, Martinez C. Paris, France: Expansion Scientifique Française; 1998. L'articulation radio-cubitale inférieure. Pathologie traumatique; pp. 196–203. [Google Scholar]
- 13.Bain G I, Richards R, Roth J H. Philadelphia. PA: WB Saunders; 1997. Wrist arthroscopy; pp. 151–168. [Google Scholar]
- 14.Ruch D S, Yang C C, Smith B P. Results of acute arthroscopically repaired triangular fibrocartilage complex injuries associated with intra-articular distal radius fractures. Arthroscopy. 2003;19(5):511–516. doi: 10.1053/jars.2003.50154. [DOI] [PubMed] [Google Scholar]
- 15.Bain G I, Munt J, Turner P C. New advances in wrist arthroscopy. Arthroscopy. 2008;24(3):355–367. doi: 10.1016/j.arthro.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Tay S C, Tomita K, Berger R A. The “ulnar fovea sign” for defining ulnar wrist pain: an analysis of sensitivity and specificity. J Hand Surg Am. 2007;32(4):438–444. doi: 10.1016/j.jhsa.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 17.Atzei A. New trends in arthroscopic management of type 1-B TFCC injuries with DRUJ instability. J Hand Surg Eur Vol. 2009;34(5):582–591. doi: 10.1177/1753193409100120. [DOI] [PubMed] [Google Scholar]
- 18.Tse W L, Lau S W, Wong W Y. et al. Arthroscopic reconstruction of triangular fibrocartilage complex (TFCC) with tendon graft for chronic DRUJ instability. Injury. 2013;44(3):386–390. doi: 10.1016/j.injury.2013.01.009. [DOI] [PubMed] [Google Scholar]


